
Kimberly Battle-Miller, MD, MS, MBA
System Medical Director- Palliative Care and Hospice,
An Overview of Hospice Care

Types of Care Available to Patients with
Serious Illness and Advance Disease
• Curative Care:
• Focused on a cure to an illness and the prolonging your life
• Palliative Care:
• Focused on comfort (treats symptoms related to the disease or resulting
from the treatment)and quality of life (what’s important to you)
• Focus on ensuring patient understand their disease, their doctors, and
treatment options
• May be provided with treatments that seek to cure patient’s disease or
prolong the patient’s life
• Hospice Care:
• When a cure of the disease is not possible
• When patient/family elects to forgo or discontinue curative treatment
• Focused on comfort and quality of life

From Diagnosis to Death
Disease-Modifying
Therapy
Palliative Care
CARE
Diagnosis Death &
Bereavement
Hospice
Non-hospice palliative care
Hospice care
Comfort care
Type of care
is matched to
prognosis and
goals of care
6 months

Hospice Eligibility
• Per CMS guidelines, patients must qualify for Hospice Care
• Two physicians, the attending physician and the hospice
medical director, must certify the patient
• Is a terminally ill or has a “life-limiting condition”
• Prognosis of 6 months or less, assuming the disease
process will run its usual course
• Patient and/or payer surrogate must elect hospice care by
signing Hospice consent forms

Common Hospice Diagnoses
• Cardiac – Cardiomyopathy, Heart Failure, MI, CAD, PVD,
Hypertensive heart disease, intractable arrhythmia
• Pulmonary – COPD, Pulm HTN, Pulm Fibrosis, Acute
pneumonia with respiratory failure, COVID-19 pneumonia
• Neurologic – Advanced stage: MS, ALS, Alzheimer’s &
Parkinson's diseases, Lewy body dementias, intracranial
hemorrhage, CVA (acute or late effect), cerebrovascular
disease (for unspecified dementia if CT/MRI consistent)
• Renal: Chronic kidney disease (w/Heart failure); ESRD
discontinuing dialysis
• Liver: End-stage cirrhosis, hepatorenal failure, liver failure
• Cancer – metastatic, end-stage unresponsive to treatment or
patient electing to stop treatment
• Autoimmune – HIV, Advanced stage Lupus & Sarcoidosis;
COVID-19 infection

Traditional Hospice Services
• Manages the patient’s pain and other symptoms
• Assists the patient and family members with the
emotional, psychosocial, and spiritual aspects of dying
• Provides medications and medical equipment
• Instructs the family on how to care for the patient
• Makes short-term inpatient care available when pain and
symptoms become too difficult to manage at home, or
the caregiver needs respite time
• Provides grief support and counseling to surviving family
and friends

Modern Hospice Care
Selected Non-curative Treatments including:
• IV Fluids/TPN
• SC Fluids
• BIPAP/Trilogy
• IV Antibiotics
• Limited Palliative Radiation Therapy
• Selective Dialysis (if not related to terminal diagnosis)
• Milrinone/Dobutamine infusions
• LVADs
• ICD/Pacemakers
• Extubation outside of the hospital (home, nursing facility,
Zelber)
• Aromatherapy

Hospice Response to COVID-19
• In-home COVID-19 testing & education by APN for:
• Persons Under Investigation:
• Due to exposure e.g. positive family member in the home
• Transferring from Nursing Facility or Rehab to home
• Acute change in symptoms, consistent with COVID-19 (for patient
education/planning, family and staff safety)
• Pre-procedure
• Prior to transfer from home to a nursing facility for Respite or Placement
• Virtual Visit (via secured Zoom)
• For hospice presentation
• For routine scheduled RN visits in home or facilities not allowing entry
• Physician visit for symptom management or family conference
• Chaplain and Social Worker routine scheduled visits
• COVID-19 exposed staff who are asymptomatic or awaiting test results

Hospice Services
Hospice
Physician
Attending Nursing Social Work
Chaplain
Home Health
Aide
Volunteer
Complimentary
Therapies
Medications
Medical
Supplies
Medical
Equipment
Bereavement

“Hospice”
• Hospice is NOT a place, it is a philosophy of care
• Hospice will be provided wherever the patient calls HOME: home, ALF, LTC
• Hospice is paid for by Medicare, Medicaid, some Insurances
• If activating Medicare hospice benefit and a patient is being discharged to a
nursing facility with hospice, room & board will either be private pay or
covered by Medicaid
• Just like hospice does NOT pay the mortgage, hospice does NOT cover room and board.

Caregiver
• Hospice care in the home requires a caregiver in the home (preferred)
• Hospice is NOT the caregiver
• Typically, a family member serves as the primary caregiver, but can be a
friend or hired caregiver
• Hospice team makes visits to assess the patient and work with the
family/caregiver
• Education on disease trajectory, daily care, and end-of-life care
• Hospice is on-call 24/7 (available by phone, staff visit if needed)

Levels of Hospice Care
Because a patient’s symptom needs may change during the course
of their disease process, hospice offers 4 different levels of care.
1. Routine Home Care
• Hospice care in patient’s place of residence (home)
2. General Inpatient Care
• Hospice care in the hospital or hospice facility
3. Continuous Care/Crisis Care
• Hospice care in the patient’s place of residence (home)
4. Respite Care
• Hospice care in a nursing facility or hospice facility

Rational
• Routine Home Care
• Provides hospice care and support to patient and family in the location the patient
calls home (house, apartment, assisted living, nursing home, homeless, group home)
• General Inpatient Hospice Care
• When patient’s symptoms/needs cannot be managed at home, the patient can be
transferred to the hospital or hospice unit for higher level of care with 24 hour nurse
availability until the symptoms are controlled/need is met and patient can return
home.
• Continuous Hospice Care (Crisis Care)
• Hospice care provided continuously for between 8 and 24 hours a day to manage any
uncontrollable symptoms
• CC is intended to maintain the patient's comfort at home during a pain or symptom
crisis
• Respite Care
• If/When the primary caregivers need to take a break (vacation/rest) the patient can
be transferred to a inpatient hospice facility or nursing facility for custodial level care
for a short time (usually 5 days)

•Inpatient Hospice Facility, CHAP accreditation*
•18 beds – 3 units (6 beds/unit)
•2019: 834 patients/687 total deaths
•Two staff stations
•LOC (GIP, Respite, Routine)
•Interdisciplinary Care, Bereavement for 13 months
•Meeting rooms
•Administrative Offices
• Also base for hospice home program
*CHAP – Community Health Accreditation Partners
Facility Purpose and Licensure

Specialized Care in a Serene Setting
• All ages
• IV/SQ pain and symptom management
• Terminal Sedation (Propofol, or Lorazepam/Propofol)
• Milrinone
• Wound Care
• Trach Care
• Drains
• Ventilator Withdrawals (terminal extubation)
• LVAD and Bi-Pap Discontinuation
• Aromatherapy (Lavender Nites or diffuser)
• Reiki, Guided Imagery, Massage therapy, music & art therapy, pet therapy, comforting companions
• Comfort Café
• Open access 24/7 for family/friends, private space avail for family, kitchen, visits by 4-legged
family members * modified visitor policy in place secondary to COVID-19

Honoring Special Life Events at AZFH
•Weddings
•Baptisms
•Couples room – sculptor donated a hand casting
•Milwaukee Brewers Racing Sausages
•MyLegacy – audio
•We Honor Vets
•Milwaukee Ballet
•Bucket List - Major motion picture
shown to patient prior to release

Palliative Care vs Hospice
• Focus: Comfort and quality of life
• Team: APN/MD, +/- CNA, SW, Chap
• Prognosis: curable, chronic, life-threating or terminal
disease
• Expected Outcome: relief from distressing
symptoms, ease pain and enhance quality of life
• Timing: no time restrictions, at any age, any time and
any stage of illness whether terminal or not; should
begin early in the disease process to identify goals of
care
• Treatment: comfort at any stage, no expectation that
life-prolonging or aggressive therapies will be
avoided; concurrent with treatment of primary disease
• Location: Hospital, outpatient, home, rehab/SNF,
ECF/NH
• Payment: Medicaid/Medicare/Private Insurance
• Focus: Comfort and quality at end-of-life
• Team: MD/APN, RN, CAN, SW, Chap, Vol
• Prognosis: life-limiting, terminal, incurable
• adults- life expectancy of 6 months or less,
• Expected Outcome: relief from distressing
symptoms, ease pain and enhance quality of life at
end-of-life
• Timing: end-of-life, considered terminal, with
prognosis of 6 months or less
• Treatment: typically elect to forego extensive life-
prolonging treatment for terminal diagnosis,
• non-curative treatment focused on symptom
relief for terminal illness
• may receive curative treatment for acute
illnesses
• Location: Hospital, outpatient, home, ECF/NH,
Hospice Facility
• Payment: Medicaid/Medicare/Private Insurance

Questions???
Thank you!!

Hospice Indicators
Aurora at Home Hospice

1
Admission Indicators
Admission Indicators
Admission criteria include:
• Patient has a life-limiting illness with a prognosis of
6 months or less
• Clinical progression of the terminal disease
• Two physicians confirm terminal condition
• Patient and family desire comfort-focused care
Admission indicators include a combination of the following:
• Life expectancy of 6 months or less if disease runs its
normal course
• Recent decline in functional status as determined by:
– Karnofsky Performance status less than 50%
(see scale on page 2)
– ECOG Performance Scale status of 3 or 4 (see scale on page 3)
– Palliative Performance status less than 50%
(see scale on page 4)
– FAST Scale (see page 10)
– Dependence in at least 3 of 6 ADLs (ie., personal hygiene, dressing,
eating, maintaining continence, transferring and ambulation)
(continued on the next page)
2
Karnofsky Performance Scale
General Category Index Specific Criteria
Unable to care
for self, requires
institutional or
hospital care or
equivalent, disease
may be rapidly
progressing
50
Requires considerable assistance from others and
frequent medical care
40 Disabled, requires special care and assistance
30
Severely disabled, hospitalization indicated,
death not imminent
20
Very sick, hospitalization necessary, active
supportive treatment necessary
10 Moribund, actively dying
• Impaired nutritional status evidenced by either:
– Weight loss of at least 10% over the past 6 months
– Serum albumin less than 2.5 gm/dl
• Repeated hospitalizations or emergency room visits
• Recurring infections, such as UTI, URI, sepsis
• Presence of decubitus ulcers
Admission Indicators (Continued)

3
ECOG Performance Status
*
Grade ECOG
0 Fully active, able to carry on all pre-disease performance without restriction
1 Restricted in physically strenuous activity but ambulatory and able to carry out
work of a light or sedentary nature, e.g., light house work, office work
2 Ambulatory and capable of all self-care but unable to carry out any work
activities. Up and about more than 50% of waking hours
3 Capable of only limited self-care, confined to bed or chair more than 50% of
waking hours
4 Completely disabled. Cannot carry on any self-care. Totally confined to bed or
chair
5 Dead
* As published in Am. J. Clin. Oncol.:
Oken, M.M., Creech, R.H., Tormey, D.C., Horton, J., Davis, T.E., McFadden, E.T., Carbone, P.P.: Toxicity
And Response Criteria Of The Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649-555, 1982.
Eastern Cooperative Oncology Group (ECOG)
Performance Status
These criteria are used by doctors and researchers to assess how a patient’s disease is
progressing, assess how the disease affects the daily living abilities of the patient, and
determine appropriate treatment and prognosis.

4
% Ambulation
Activity and Evidence
of Disease
Self-Care Intake
Consciousness
Level
100 Full
Normal Activity
No Evidence of Disease
Full Normal Full
90 Full
Normal Activity
Some Evidence of Disease
Full Normal Full
80 Full
Normal Activity with Effort
Some Evidence of Disease
Full
Normal or
Reduced
Full
70 Reduced
Unable to do Normal Work
Some Evidence of Disease
Full
Normal or
Reduced
Full
60 Reduced
Unable to do
Hobby/House Work
Significant Disease
Occasional
Assistance
Necessary
Normal or
Reduced
Full or Confusion
50
Mainly Sit/
Lie
Unable to do Any Work
Extensive Disease
Considerable
Assistance
Required
Normal or
Reduced
Full or Confusion
40
Mainly in
Bed
Unable to do Any Work
Extensive Disease
Mainly
Assistance
Normal or
Reduced
Full or Drowsy or
Confusion
30
Totally Bed-
Bound
Unable to do Any Work
Extensive Disease
Total Care Reduced
Full or Drowsy or
Confusion
20
Totally Bed-
Bound
Unable to do Any Work
Extensive Disease
Total Care
Minimal
Sips
Full or Drowsy or
Confusion
10
Totally Bed-
Bound
Unable to do Any Work
Extensive Disease
Total Care
Mouth Care
Only
Drowsy or Coma
0 Death – – – –
Palliative Performance Scale*
* This scale is a modification of the Karnofsky Performance Scale. It takes into account ambulation, activity,
self-care, intake and consciousness level.
5
Cancer
Hospice Indicators for Cancer
• Metastasis at presentation or progression
• Curative treatments are no longer effective
• Treatment is having negative impact on patient’s quality of life
• Increasing pain and/or symptoms
• Multiple trips to hospital for symptom management
• Toxicity outweighs benefits
• Poor performance status
– ECOG of 3 – 4 (see scale on page 3)
– Karnofsky or Palliative Performance Scale less than 50%
(see scales on page 2 and page 4)
• Exhausted patient and family/caregivers
• Patient/Family/Caregivers wants to stop curative or palliative radiation
and/or chemotherapy **
** Patients enrolled in hospice may qualify for palliative radiation and/or continuation chemotherapy
treatment on an individualized basis for cancer symptom management.
6
What is hospice? Hospice is a program designed specifically for people who have
chosen to change the plan of care for a life-limiting illness from aggressive medical
treatment, focused on curing an illness, to care that manages pain and symptoms so
patients can make the most of every day.
Did you know?

7
Cardiopulmonary Disease
• Disabling dyspnea at rest, poor
response to bronchodilators
• Persistent symptoms of recurrent
CHF at rest
• Optimally treated with diuretics
and vasodilators (ACE inhibitors) or
unable to tolerate
• New York Heart Class IV and/or
American Heart Association (AHA)
Stage D
• May have an impaired ejection
fraction
• History of unexplained syncope
• History of cardiac arrest or MI
• Brain embolism of cardiac origin
• Increasing visits to the ER
or hospitalizations for respiratory
infections and/or respiratory
failure
– pO
2
less than or equal to
55 mmHg
– Oxygen saturation less
than or equal to 88%
• Resting tachycardia greater
than 100/minute
• Presence of cor pulmonale
or right heart failure (RHF)
• Identification of functional
limitation, such as:
– Decline in functional status
Hospice Indicators for Cardiopulmonary Disease
Identification of specific structural/functional impairments, along with
relevant activity limitations such as:
Examples of secondary conditions: Delirium, pneumonia, stasis ulcers,
pressure ulcers, failure to thrive and debility
Example of co-morbid condition: End-stage renal disease (ESRD)

8
Class Patient Symptoms
I
II
III
IV
No limitation of physical activity. Ordinary physical activity does not cause undue
fatigue, palpitation, dyspnea (shortness of breath)
Slight limitation of physical activity. Comfortable at rest. Ordinary physical
activity results in fatigue, palpitation, dyspnea (shortness of breath).
Marked limitation of physical activity. Comfortable at rest. Less than ordinary
activity causes fatigue, palpitation, or dyspnea.
Unable to carry on any physical activity without discomfort. Symptoms of heart
failure at rest. If any physical activity is undertaken, discomfort increases.
American College Cardiology/American Heart Association Stages of Heart Failure:
Stage Patient Symptoms
A
B
C
D
No objective evidence of cardiovascular disease. No symptoms and no limitation
in ordinary physical activity.
Objective evidence of minimal cardiovascular disease. Mild symptoms
and slight limitation during ordinary activity. Comfort at rest.
Objective evidence of moderately severe cardiovasular disease. Marked limitation
in activity due to symptoms, even during less-than-ordinary activity. Comfortable
only at rest.
Objective evidence of severe cardiovascular disease. Severe limitations.
Experiences symptoms even while at rest.
New York Heart Association (NYHA) Functional
Clasification of Heart Failure:

9
Dementia
Hospice Indicators for Dementia
Includes diagnoses such as Alzheimer’s Disease, Parkinson’s Disease,
Lewy Body Dementia, frontal lobe dementia and *vascular dementia
* Note: Medicare does not accept vascular dementia or advanced dementia as a primary
hospice diagnoses. However, they may be used as secondary diagnoses.
1. Stage 7 on FAST Scale (loss of speech, locomotion and consciousness)
7a: Ability to speak is limited
(1 to 5 words a day)
7b: Speech is unintelligible
7c: Non-ambulatory
7d: Unable to sit up
independently
7e: Unable to smile
7f: Unable to hold head up
Co-morbidity, such as:
• CHD (Coronary Heart Disease)
• COPD
2. Should have one of the following in the past six months:
Secondary Conditions, such as:
• Decubitus ulcers, multiple Stage
III-IV
• Inability to maintain sufficient
fluid and calorie intake with 10%
weight loss during previous six
months or serum albumin less
than 2.5 gm/dl
• Aspiration pneumonia
• Septiciemia
• Pyelonephritis
• Fever, recurrent after antibiotics

10
Grade FAST
1
No difficulty either subjectively or objectively
2
Complains of forgetting location of objects. Subjective work difficulties
3
Decreased job functioning evident to co-workers. Difficulty in traveling to new locations.
Decreased organizational capacity*
4
Decreased ability to perform complex tasks (e.g., planning dinner for guests, handling
personal finances, such as forgetting to pay bills, etc.)
5
Requires assistance in choosing proper clothing to wear for the day, season or occasion
(e.g., pt may wear the same clothing repeatedly, unless supervised)*
6
Occasionally or more frequently over the past weeks* for the following
A) Improperly putting on clothes without assistance or cueing
B) Unable to bathe properly (not able to choose proper water temp)
C) Inability to handle mechanics of toileting (e.g., forget to flush the toilet, does
not wipe properly or properly dispose of toilet tissue)
D) Urinary incontinence
E) Fecal incontinence
7
A) Ability to speak limited to approximately </= 6 intelligible different words in
the course of an average day or in the course of an intensive interview
B) Speech ability is limited to the use of a single intelligible word in an average
day or in the course of an intensive interview
C) Ambulatory ability is lost (cannot walk without personal assistance)
D) Cannot sit up without assistance (e.g., the individual will fall over if there are
not lateral rests [arms] on the chair)
E) Loss of ability to smile
Functional Assessment STaging (FAST)
*Scored primarily on information obtained from knowledgeable informant. Psychopharmacology bulletin, 1988 24:653-659.
11
1. CD4 + count less than 25 cells/mcL
or persistent viral load greater than
100,000 copies/ml, plus ONE of the
following:
a. CNS Lymphoma
b. Untreated, or not responsive to
treatment, wasting (loss of 33%
lean body mass)
c. Mycobacterium avium complex
(MAC) bacteremia, untreated,
unresponsive to treatment, or
treatment refused
d. Progressive multifocal
leukoencephalopathy
e. Systemic lymphoma, with
advanced HIV disease and partial
response to chemotherapy
f. Visceral Kaposi’s Sarcoma
unresponsive to therapy
g. Renal failure in the absence
of dialysis
h. Cryptosporidium infection
i. Toxoplasmosis, unresponsive
to therapy
2. Decreased performance status,
as measured by the Karnofsky
Performance (KPS) Scale of less than
or equal to 50
3. Documentation of the following
factors support eligibility for hospice
care:
a. Chronic persistent diarrhea for
one year
b. Persistent serum albumin less
than 2.5
c. Concomitant, active substance
abuse
d. Age greater than 50 years
HIV Disease
Hospice Indicators for HIV Disease
1 and 2 must be present; factors from 3 will add supporting documentation:
Eligibility factors continued on reverse
12
e. Absence of antiretroviral, chemotherapeutic and prophylactic drug therapy
related specifically to HIV disease
f. Advanced AIDS dementia complex
g. Toxoplasmosis
h. Congestive heart failure, symptomatic at rest
i. Advanced liver disease
Hospice Indicators for HIV Disease (cont.)
Did you know?
Hospice is not a place. Rather, it is a comprehensive service that is provided in the
home 90 percent of the time. Sometimes, patients are temporarily moved to a hospital
if a patient’s pain or symptoms require skilled monitoring and plan of care changes.
The hospice team can also provide respite care so that caregivers can have a little
time away from the day-to-day requirements of caring for a loved one in hospice care.
The patient can be placed in a nursing home for a predetermined number of days
while continuing to receive care from the hospice team.

13
Liver Disease
Hospice Indicators for Liver Disease
Criteria in 1 and 2 should be present; factors from 3 will lend supporting
documentation:
1. INR greater than 1.5
(or Prothrombin time prolonged
more than 5 seconds over control);
Serum Albumin less than 2.5 gm/dl
2. Documentation of end-stage liver
disease, and patient shows at least
one of the following:
• Ascites, refractory to treatment,
or patient non-compliant
• Spontaneous bacterial peritonitis
• Hepatorenal Syndrome (elevated
creatinine and BUN with oliguria
[less than 400 ml/day] and urine
sodium concentration less than
10 mEq/l)
• Hepatic encephalopathy,
refractory to treatment, or
patient non-compliant
• Recurrent variceal bleeding
despite intensive therapy
3. The following support eligibility:
• Progressive malnutrition
• Muscle wasting with reduced
strength and endurance
• Continued active alcoholism
(greater than 80 gm ethanol/day)
• Hepatocellular carcinoma
• HBsAg (Hepatitis B) positivity
• Hepatitis C refractory to
interferon treatment
Patients awaiting liver transplant
who otherwise fit the above criteria
may be certified for the Medicare
hospice benefit. But if a donor organ
is procured, the patient must be
discharged from hospice.

14
Did you know?
A multi-disciplinary team cares for hospice patients. The team includes:
patient/caregivers; patient’s physician; hospice physician; registered nurse;
certified home health aide; social worker; chaplain; grief counselor; and
volunteers.

15
Neurological Conditions
Includes diagnoses such as CVA, Parkinson’s Disease, ALS and MS
• Neurological conditions are associated with impairments, activity
limitations and disability
• Identification of impaired function with increasing debility impacting
quality of life/functional impairments
• Palliative Performance Scale less than or equal to 50
• Recurrent hospitalizations
Secondary Conditions such as:
• Dysphagia/Aspiration
• Aspiration pneumonia
• Pressure ulcers
• Anorexia/Decreased appetite/
Failure to thrive
• Mental status decline and
confusion
• Generalized weakness and
frequent falls
• Recurrent urinary tract
infections
• Weight loss of greater than 10%
in the past 6 months or 7.5% in
the past 3 months
• Serum albumin less than
2.5 gm/dl
• Serum creatine greater than
1.5 mg/dl
• Pyelonephritis
Co-morbid conditions, such as COPD, heart failure or dementia.
Hospice Indicators for Other Neurological Conditions

16
Did you know?
Hospice is affordable. Medicare and Medicaid provide coverage at 100% for those
hospice services and medications which are used to manage the life-limiting
illness.
17
Protein Calorie Malnutrition
Hospice Indicators for Protein Calorie Malnutrition
Protein Calorie Malnutrition (Mild, Moderate or Severe)
• BMI less than or equal to 19
° Mild protein calorie malnutrition defined as BMI 17.00 – 18.49
° Moderate protein calorie malnutrition defined as BMI 16.00 – 16.99
° Severe protein calorie malnutrition defined as BMI less than 16.00
• PPS less than 40% mostly in bed (marked reduction in physical activity)
• Dependent on greater than 2 ADLs
• Serum albumin less than 2.5 g/dL
• Weight loss greater than 10% in 6 months; greater than 5% in 3 months;
visual fat loss, muscle wasting
° Unable to maintain/not responding to any nutritional support
° Unable to maintain sufficient calories or fluids
° Patient/Family/Durable Power of Attorney does not want/refusing enteral
or parenteral nutrition
• Stage 3 or 4 pressure ulcers
• Increase ER visits/multiple hospitalizations
18
Did you know?
After a patient dies, Aurora at Home Hospice offers family and loved ones a 13-month
bereavement program. Grief support can be provided in different ways: Bereavement
newsletter; individual grief support; grief support groups; workshops; and education.

19
Renal Care
Hospice Indicators for Renal Disease
The patient is not a candidate for dialysis or renal transplant or
wishes to discontinue dialysis
• Serum creatinine greater than 8.0 mg/dl (greater than 6.0 mg/dl
for diabetics)
• Creatinine clearance less than 10 cc/min (less than 15 cc/min for
diabetics); or less than 15 cc/min (less than 20 cc/min for diabetics)
with comorbidity of congestive heart failure
• Estimated glomerular filtration rate (GFR) less than 10 ml/min
Supplemental
Presence of co-morbid conditions in acute renal failure is helpful
• Coronary heart disease (CHD)
• Peripheral vascular disease (PVD)
• Vascular dementia
• Heart failure
• Advanced liver disease
Secondary conditions, directly related to the primary condition:
• Secondary hyperparathyroidism
• Calciphylaxis
• Electrolyte abnormalities
• Anorexia
• Fluid overload
Presence of signs and symptoms in chronic renal failure is helpful:
• Examples include uremia, oliguria (less than 400 cc/24 hours),
intractable hyperkalemia (greater than 7.0) not responsive to treatment,
hepatorenal syndrome, uremic pericarditis, Hepatorenal Syndrome,
intractable fluid overload not responsive to treatment

How Aurora at Home Hospice Helps Patients and Families
• Enhances quality of life
• Consultations available 24 hours a day, 7 days a week by professional
staff (ie., RN, MSW and physician)
• Pain evaluated on every visit
• Expertise in pain and symptom management
• Provides 4 Levels of Care (Routine, Respite, Crisis Care in an inpatient
setting or Continuous Care at the patient’s place of residence)
• Treats infections and wounds to promote patient comfort
• Provides medications, supplies and equipment related to symptom
management of the terminal illness, anxiety and depression
• Educates regarding nutrition and hydration issues, with a focus on
patient comfort and goals; evaluation for swallowing concerns can be
ordered if needed
• Provides a personalized plan of care
• Reduces physician office calls, 911 calls, ER visits and hospitalizations
(continued on page 21)
20
• Helps with end-of-life planning
• Assists with documenting advance directives, such as Health Care POA
• Assists with funeral planning arrangements
• Anticipates needs of patient and family; may refer to available
community resources
• Uses non-pharmacological therapy
• Visits provided by psychosocial and spiritual staff with ongoing
follow-up for patients, families and staff
• Communicates with families regarding patient’s condition
• Provides communication and patient updates as determined by the
referral source
• Attends and confirms deaths
• Provides 13 months of bereavement services
How Aurora at Home Hospice Helps Patients and Families
21

GAS 3/19 MC 1623
To learn more about Aurora at Home Hospice
or to make a referral, call:
1.833.268.1268

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
1
Inpatient Hospice
Inpatient to ADVOCATE Hospice in the Hospital Steps
End Users Affected: Inpatient Nurses, Hospice Nurses, Care Managers, Patient
Access/Registration, Unit Clerks, and Physicians
The following outlines the steps necessary to flip a patient to ADVOCATE Hospice in Epic from beginning to
end.
Entering Service to Hospice Order
I. Initial clinician steps [to be completed by a physician or anyone with
order entry access, including nurses in the event that the physician is
not available]
A. Navigate to the Discharge Navigator to open the Home Care Services Order Set
B. Click the Service to Home Care Option and then click on the blue hyperlink to open the order
composer
• Select Hospice for the Home care service needed
• Fill in required fields: “Terminal Diagnosis” and “Following/Attending provider for Hospice
Care”

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
2
Inpatient Hospice
C. Once the physician completes this order, click Accept.
• You will see a Discharge order automatically queued up in the sidebar on the right hand side of
screen. Remove this order at this point, as you do not know if the patient will be
accepted.
• Click “X” to the right of the order to remove it.
D. Select Sign. Associate a diagnosis if prompted.
After the patient has been evaluated by an Advocate at Home Nurse Liaison and has accepted
and consented to “Hospice in the Hospital” they will contact the attending physician to
collaborate on the entering of Hospice admission orders. Skip to Step III for details on that
process.
NOTE: For referrals during off hours, weekends, holidays, and those that are emergent, call Advocate at Home
directly after placing the order @ 630-963-6800.
Advocate Hospice Admission Nurse
II. Advocate Hospice Admission Nurse
A. Completes election visit per normal
B. Contacts hospice medical director to inform them that the patient has consented to hospice.

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
3
Inpatient Hospice
C. Contacts the physician covering the patient in the hospital to inform them that the patient has
consented to hospice.
i. Collaborate with inpatient physician to complete the Discharge/Readmit Process and
entering of Hospice orders (See Step III for details).
D. Call Admitting/Patient Access Dept. and let them know to set up a pre admission on the patient
(See Step IV for details).
• Remind them to add hospice as payer source and do not remove any payer sources.
• They will still need to enter information such as patient name, room, diagnosis, MD
following etc.
• Request they call you back when done.
E. Call the unit clerk and ask them to move patient up into room from the bottom of their screen via
Unit Manager (See Step V for details).
F. Call the patient’s RN and let them know that once the Unit Clerk does the step above, they can
release hospice orders from their Orders activity tab, Signed & Held tab (See step VI for
details).
“Discharge/Readmit” Steps
III. Discharge/Readmit Steps – to be completed by the physician or Hospice RN
if physician not available
A. PHYSICIAN STEPS:
i. Go to Discharge Tab
ii. Click on second tab called DISCHARGE READMIT navigator, click Discharge readmit
on the left side
iii. Reconcile Medications
These new medication orders will be signed and held! They will not be active on the MAR until the nurse
releases the med orders after the patient has been readmitted as a Hospice Patient!

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
4
Inpatient Hospice
✓ Review Current Orders: Decide which orders to continue or don’t order. Address each
medication – use buttons for Unselected options to expedite process.
✓ Enter New Orders: Click on Order Sets to locate the IP Hospice Admission Order Set
iv. Click ORDER SETS tab.
• Search “IP Hospice” in Order Set search field in the sidebar to locate IP Hospice Admission Order
Set
• Open the HOSP IP Hospice Admission Order Set (right click to make a favorite)
• Click on Admit to Hospice order – enter admitting dx
• Continue to enter appropriate orders for Hospice care. (Common orders are selected as default
checked - Click on blue hyperlinks to make changes to order details as needed.)

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
5
Inpatient Hospice
• Once you have the orders selected from the order set, look at your sidebar.
Click on the “Sign-Will be Released on New Admission.” The Discharge Patient order is
now active, but all other orders are signed and held for the nurse to release after the
following step below.
v. Fill out the Discharge Patient Order details.
In the Disposition field, enter “Hospice – Inpatient Medical Facility.” Find this using the magnifying
glass.
B. HOSPICE RN STEPS:
i. Log in to Hyperspace in a “HOSPICE ADVOCATE…” department (If you use Hospice
Scheduling department or an Inpatient Hospital department, you will not get the correct tools!!!)
ii. Navigate to the Patient List activity to open the patient’s hospital chart. Double click on
the patient to open their chart. (If you access the patient’s chart via any other method, you will not have the correct tools to
perform the discharge/readmit process)
iii. Navigate to the “Navigators” tab.
iv. Click on the “Discharge Readmit”
v. From here the process mimics the physician steps starting at step iv above

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
6
Inpatient Hospice
Patient Access: Creating New Pre-Admission
IV. Create New Pre-Admission
A. Navigate to the patient’s Patient Station and click “New Preadmission”.
B. Select Yes on the Encounter Creation warning that will populate.
C. In the New Admission Questionnaire complete the following fields:
➢ Expected Date: enter the expected date that the admission will occur
➢ Unit: select the appropriate unit
➢ Patient Class: Inpatient Hospice
➢ Admitting Provider: enter the appropriate provider
➢ Service: Hospice
D. Complete and Patient level registration that is needed if applicable
E. Enter the necessary information in the Admission Info folder
F. Move to the Hospital Accounts folder on the Form Navigator
G. Click the Create New Account Button
H. Click PreAdmission button at the bottom of the screen
I. Patient Station will open and the pending admission is listed as a current encounter – Look for
Patient Class to say Inpatient Hospice.

Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
7
Inpatient Hospice
J. Call the Hospice Nurse and let them know that the preadmission has been created.
Unit Clerk/Inpatient RN: Discharge Readmit Steps
V. Discharging patient and readmit with new Preadmission
1. From Unit Manager select the patient and click Discharge
2. From Admissions on bottom left, drag the patient and drop in the room they were just
discharged from.
3. The patient’s accommodation code should now say “Hospice”
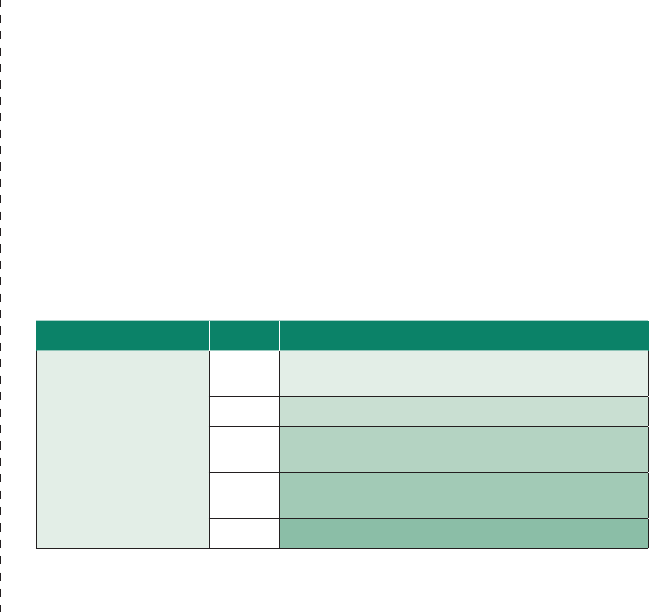
Inpatient Nurse: Releasing Orders
VI. Releasing Orders
1. Navigate to Orders activity tab
2. Select Sign & Held
3. Click the blue hyperlink Edit and Release Signed and Held Orders
4. Click on the symbol if you don’t see orders – they may be collapsed
5. Scroll down to the bottom and click Select All Orders Placed Prior to This Admission
and then click Release
Approved By: Post-Acute Clinical Informatics
Date: January 30, 2020
8
Inpatient Hospice
6. Complete all usual admission documentation
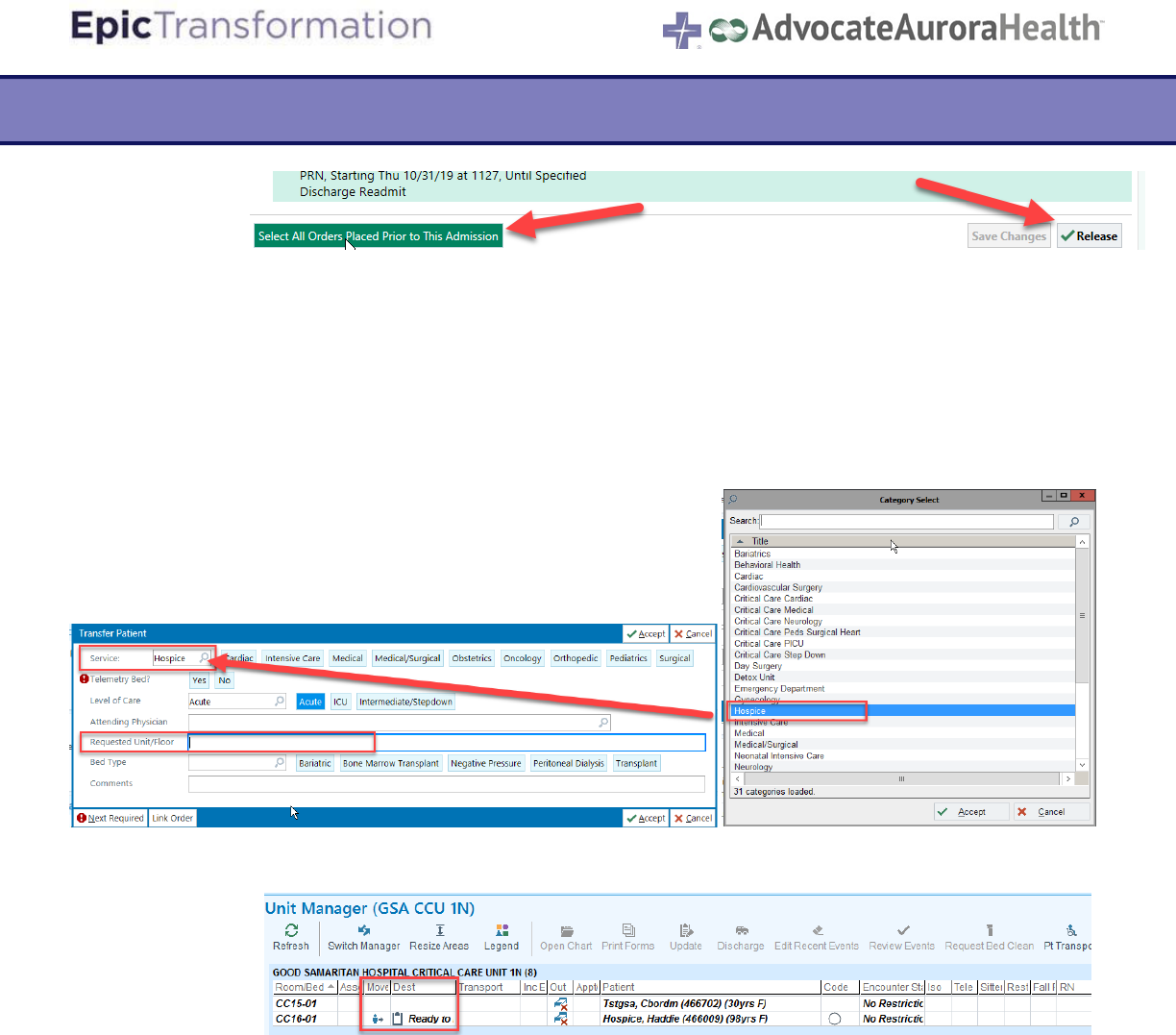
VII. Inpatient RN: Moving the patient to Another Unit or Bed
1. If the patient needs to be moved to another unit or bed, navigate to the Orders tab and
search “Transfer (ADT7)”Order
2. Fill in all required fields as well as which Unit/Floor the patient is transferring to.
3. In the Unit Manager, the patient will now appear with an Icon and “Ready to Plan” column.
4. Follow regular transfer patient workflows from here.

