
About Inseparable
Inseparable is a national nonprofit working to advance mental health
policy solutions that help people thrive, including by increasing access
to care, improving crisis response, and promoting youth mental health.
We use a unique, campaign-style approach to support lawmakers in
enacting mental health policies that will save lives and improve care for
millions of Americans. We believe that with the right leadership and
strategy, we can all take better care of ourselves, our loved ones,
and our communities.
Acknowledgements
Inseparable is grateful to the Milliman team, including Stoddard
Davenport, T.J. Gray, Bridget Darby, and Cole Spear, whose invaluable
data is featured in Improving Mental Health Care: The Access Report.
All opinions or views expressed in this report are those of the authors,
not Milliman. Milliman does not intend to benefit or create a legal duty
to any recipients of this report. As a matter of policy, Milliman does not
endorse any product, service, or initiative, and no such endorsement
is intended for Inseparable.
Authors
Angela Kimball, Caitlin Hochul, Benjamin Miller, PsyD., and Dania Lofton.
Inseparable extends a special thank you to
Tim Clement, Kathleen Daughety, Pamela Krikorian, David Lloyd,
Keris Myrick, and Betsey O’Brien for their helpful review of and
contributions to this report.
© December 2023 Inseparable, Inc.
www.inseparable.us
Improving
Mental
Health Care
THE ACCESS REPORT
DECEMBER
2023

ACCESS TO MENTAL HEALTH CARE IN AMERICA TODAY 4
U.S. mental health care by the numbers 4
The purpose of this report 5
Policies at-a-glance 6
STATE POLICIES THAT WORK 7
1 Expand coverage of care 7
Require coverage of all medically necessary treatment 8
Require coverage for out-of-network care 9
Mandate accurate provider directories 10
Insure more people through Medicaid 11
Ensure continuous Medicaid coverage 12
Extend Medicaid coverage to people in prison or jail 13
2 Leverage the mental health workforce 14
Expand the use of telemental health 15
Adjust state licensure requirements 16
Promote the use of peer and behavioral health support specialists 17
Provide competitive reimbursement rates for providers 18
3 Promote prevention and early intervention 19
Cover annual mental health screenings and wellness exams 20
Waive formal diagnosis requirements for mental health care 21
Address social determinants or drivers of health 22
Integrate mental health care with primary care 23
STATE PROGRESS: IMPROVING ACCESS TO CARE 24
Progress guide to state policies 24
State progress snapshots 26
Nationwide snapshot 128
CONTENTS
3
Improving Mental Health Care: The Access Report
inseparable.us

People in every state and every community
agree that America’s mental health care
system is falling short.
Poll after poll reveals that mental health is top of mind for Americans. They are
worried about their own health and the health of their loved ones. They need
better access to care. And they want their elected leaders to treat these issues
with urgency.
U.S. mental health care by the numbers
Access to mental health
care in America today
1
SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based Estimated Totals.
2, 3
Milliman, “Access Across America” (2023) Inseparable.us/accessacrossamerica.
1 in 5 people
had a mental health
condition in the past year
1
who visit the ER
or hospital for
mental health
or substance use
treatment get
follow-up
care within
30 days
3
Only 1 in 3
people
did NOT receive treatment
2
More than
2 in 3 people
4
Improving Mental Health Care: The Access Report
inseparable.us

Access to mental health
care in America today
The purpose of this report
State policymakers across the country have the power to improve access to
mental health care by championing and passing key policies that help expand
coverage of care, leverage the mental health workforce, and promote
prevention and early intervention.
4
These strategies, and their corresponding policy actions, help remove barriers
that prevent or delay people from accessing mental health care. Recognizing
that every state is unique, these policy solutions can be adapted to a state’s
economic, social, and political climate. The goal of this report is to foster an
open, nationwide exchange of effective policy solutions.
Following discussion of these strategies, we feature state-by-state data
snapshots of each state’s progress in adopting a range of policies that make
mental health care easier to find, easier to pay for, and more effective for
individuals and their families.
4
Throughout this report, references to mental health are intended to include substance use
disorders, autism spectrum disorders, and eating disorders. For simplicity, we use mental health
rather than behavioral health in all references.
We look forward to a future
when all mental health care
is accessible, affordable,
and effective for everyone.
5
Improving Mental Health Care: The Access Report
inseparable.us

Expand coverage of care
1
Require coverage of all medically necessary treatment.
Require coverage for out-of-network care.
Mandate accurate provider directories.
Insure more people through Medicaid.
Ensure continuous Medicaid coverage.
Extend Medicaid coverage to people in jails and prisons.
Leverage the mental health workforce
2
Expand the use of telemental health.
Adjust state licensure requirements.
Promote the use of peer and behavioral health.
support specialists.
Provide competitive reimbursement rates for providers.
Promote prevention and early intervention
3
Cover annual mental health screenings and wellness exams.
Waive formal diagnosis requirements for mental health care.
Address social determinants or drivers of health.
Integrate mental health care with primary care.
Policies at-a-glance
Access to mental health
care in America today
6
Improving Mental Health Care: The Access Report
inseparable.us

More than two-thirds of Americans who
need mental health treatment do not get it.
Policymakers have several levers to help close this gap, including approaches
to improve health insurance. Expanding coverage means both increasing the
number of people who have coverage and establishing patient protections to
ensure insurance companies are providing members with meaningful access
to mental health providers and coverage for all medically necessary treatment.
Policies to accomplish this include:
Require coverage of all
medically necessary treatment.
Require coverage for
out-of-network care.
Mandate accurate
provider directories.
Insure more people
through Medicaid.
Ensure continuous
Medicaid coverage.
Extend Medicaid coverage
to people in prison or jail.
State policies
that work
1
EXPAND COVERAGE OF CARE
7
Improving Mental Health Care: The Access Report
inseparable.us

Require coverage of all
medically necessary treatment
States typically allow insurers to use proprietary criteria to make
decisions about the necessity of a given treatment. This often
leads to denials of coverage for much-needed mental health
treatment deemed necessary by the patient’s doctor. Without
coverage, people may delay or skip treatment, elevating their
risks for severe mental health symptoms and relapses.
In 2019, a federal court found that United Behavioral Health used
flawed criteria to routinely deny mental health and substance
use claims for enrollees or to cut treatment short. In response,
several states have enacted laws to ensure that health plans use
transparent, nonprofit clinical guidelines to cover mental health
treatment that is consistent with generally accepted standards
of care. Following these standards helps ensure that health plans
will not inappropriately deny treatment claims.
State policies that work
EXPAND COVERAGE OF CARE
What states
can do
Require insurers to evaluate mental
health claims based on transparent,
nonprofit clinical guidelines.
Require insurers to cover all medically
necessary mental health treatment
consistent with generally accepted
standards of care.
8
Improving Mental Health Care: The Access Report
inseparable.us

Require coverage for out-of-network care
A lack of appropriate provider networks forces people to
obtain mental health care out-of-network at more than 5 times
the rate for other health needs. For many people, lack of in-
network providers means getting limited treatment – or no
treatment at all. As their health worsens, people often move
into public services such as Medicaid, shifting the cost burden
onto taxpayers.
Requiring health plans to cover out-of-network care when
timely, effective services can’t be found in-network benefits
everyone. People can find affordable care more easily, while
health plans gain key insights that can help them fill gaps that
will ultimately lead to better health outcomes at cost savings.
State policies that work
EXPAND COVERAGE OF CARE
What states
can do
Require health plans to cover
out-of-network care from licensed
providers when timely, appropriate,
medically necessary services aren’t
available in-network. Costs must not
be higher than what people pay for
in-network care.
Requiring health plans to pay for
out-of-network care when timely,
effective services can’t be found
in-network benefits everyone.
9
Improving Mental Health Care: The Access Report
inseparable.us

Mandate accurate provider directories
A major barrier to getting mental health care is finding in-network
providers. When people are forced to seek care outside their
insurance network, they often struggle with the high cost of
treatment. Being unable to find an in-network provider quickly
may also delay treatment or encourage people to go without –
which can threaten the well-being of entire families.
As the “front door” for finding in-network providers – and often
a selling point in choosing a health plan – provider directories
must be accurate and up to date. However, more than 53% of all
people looking for care have found themselves foiled by “ghost
networks” – provider directories that appear to have numerous
professionals in-network but are so full of inaccurate listings that
some people are unable to get any appointment at all.
State policies that work
EXPAND COVERAGE OF CARE
What states
can do
Create strong state enforcement mechanisms,
including automatic fines for plans that fail to
meet directory accuracy targets.
Require plans to regularly update directories,
conduct independent audits of directory data,
and mandate regular reporting of accuracy
compliance to state regulators.
Require public disclosure of directory
accuracy rates.
Provide a mechanism for beneficiaries and
providers to report directory inaccuracies to
health plans and state regulators.
Protect patients from out-of-network charges
if visit or stay was due to inaccurate provider
directory at time appointment was scheduled.
10
Improving Mental Health Care: The Access Report
inseparable.us

What states
can do
Expand Medicaid eligibility to low-income
adults up to 133% of the federal poverty level.
Extend coverage to low-income adults through
a private option.
Insure more people through Medicaid
Changes to state-level Medicaid policies can help more people
obtain mental health services. Expanding eligibility makes it
possible for single, low-income adults with mental health conditions
to enroll in Medicaid. Without this option, individuals must first
qualify for federal disability, a lengthy and complex process that
can delay treatment.
Insuring more people can also be achieved by using Medicaid funds
to purchase private coverage for low-income adults (an approach
known as private option). However, people with coverage through
a private option may face higher out-of-pocket costs than those
covered by Medicaid.
Research shows that expanding coverage leads to a significant
increase in the number of people who get regular care for chronic
conditions, and decreases the chance that they will need costly
emergency room care. Coverage also increases the likelihood that
people will get the services and supports they need to prevent
mental health emergencies and promote good health.
State policies that work
EXPAND COVERAGE OF CARE
Expanding eligibility makes it possible
for single, low-income adults with mental
health conditions to enroll in Medicaid.
11
Improving Mental Health Care: The Access Report
inseparable.us

Ensure continuous Medicaid coverage
When people with mental health conditions have trouble navigating
Medicaid processes for renewal or redetermination, their coverage
often expires. Lapses in coverage – often called churn – lead to
delayed or discontinued care, including medications. This can
trigger severe symptoms in people with mental health conditions.
In fact, churn is associated with much higher monthly health care
costs and administrative costs.
In January 2024, all states will be required to provide 12 months of
continuous Medicaid eligibility for children; however, no comparable
requirement exists for adults, so state policymakers will have to
proactively adopt that standard.
State policies that work
EXPAND COVERAGE OF CARE
What states
can do
Require continuous Medicaid
eligibility for all adults.
Adopt a Medicaid state plan option to provide
12 months of continuous postpartum coverage –
a period when many birthing parents experience
mental health conditions.
Adopt a simplified, fast process for verifying
Medicaid and CHIP eligibility.
Require Medicaid to implement presumptive
eligibility, allowing multiple entities to make
temporary eligibility determinations.
12
Improving Mental Health Care: The Access Report
inseparable.us

Extend Medicaid coverage to people
in prison or jail
A large share of people in jails and prisons have mental health
conditions. Many of these individuals became involved with
the legal system because of their illness and, if they received
treatment, could avoid future justice system involvement. Federal
regulations have historically barred the use of Medicaid funds
for most health care services while someone is in custody. But
in April 2023, the Centers for Medicare and Medicaid Services
(CMS) issued new guidance on 1115 demonstration opportunities
(waivers) that allow Medicaid financing of medical services before
people are released from custody. Taking this step improves
access to care for inmates, which supports their successful reentry
and yields benefits to taxpayers by reducing the high cost of
repeated arrests and emergency department visits.
State policies that work
EXPAND COVERAGE OF CARE
What states
can do
Apply for a Medicaid 1115 waiver to improve
coverage and connections to care for people in
jails, prisons, or youth detention facilities.
Suspend coverage for people who are
incarcerated instead of terminating it.
Support in-reach programs that facilitate
coverage and care prior to release, strengthen
discharge planning, and ensure access to post-
release mental health services and medications.
Designate jails and prisons as qualified entities
for Medicaid presumptive eligibility.
Promote data and information sharing across
agencies to streamline enrollment and access
to services.
13
Improving Mental Health Care: The Access Report
inseparable.us

The widespread shortage of
behavioral health professionals plays
a key role in reducing access to care.
While there is no doubt we need to widen the pipeline of future
providers, the following policies offer opportunities to better leverage
the existing workforce.
To accomplish this, state policymakers can:
State policies
that work
2
LEVERAGE THE MENTAL HEALTH
WORKFORCE
Expand the use of
telemental health.
Adjust state licensure
requirements.
Promote the use of peer
and behavioral health
support specialists.
Provide competitive
reimbursement rates
for providers.
14
Improving Mental Health Care: The Access Report
inseparable.us

Expand the use of telemental health
Telemental health services, which grew exponentially during the
COVID-19 pandemic, account for 1 in 3 outpatient mental health
visits. These online services give us a clear path to expanding the
capacity of the mental health system by allowing providers to serve
more patients in more areas.
Telemental health also helps us bring mental health together with
primary care received in doctor’s offices, hospitals, clinics, and other
settings. In addition to increasing access to care, telemental health
meets people where they are, overcoming the limits of geography to
allow people of all backgrounds to connect with culturally competent
and age-specific providers. Audio-only telemental health is especially
helpful for people in rural areas who lack reliable broadband access,
as well as people who have difficulty using digital technology. In the
wake of the pandemic, state policymakers can and should adopt
policies to maintain and expand access to telemental health.
State policies that work
LEVERAGE THE MENTAL HEALTH WORKFORCE
What states
can do
Require commercial health insurers and state
Medicaid plans to cover telehealth services and
reimbursement at the same rate as in-person care.
Specifically include mental health conditions in
telehealth coverage and audio-only coverage.
Ensure that telemental health services are
offered through platforms accessible to people
with disabilities.
Prohibit insurers from requiring prior authorization
for telemental health services.
Create flexibility in licensing, credentialing,
and malpractice issues to allow greater use of
telemental health services.
15
Improving Mental Health Care: The Access Report
inseparable.us

Adjust state licensure requirements
State licensure and credentialing rules can block qualified
professionals from practicing across state lines, reducing the
number of providers available in a given state or region. Many
states are changing licensing requirements to allow more
flexibility for mental health professionals. Several states are also
joining interstate licensure compacts such as the Psychology
Interjurisdictional Compact (PSYPACT), the Counseling Compact,
and the Social Work Licensure Compact. This makes it easier
for providers to practice in more than one state and expands the
capacity of the whole system.
State policies that work
LEVERAGE THE MENTAL HEALTH WORKFORCE
What states
can do
Join interstate compacts to permit licensed,
eligible mental health professionals to practice in
member states.
Adopt flexible terms or revisions of state licensure
Streamline processes and provide resources
to ensure timely approval of applications for
licensure or credentialing.
Provide stipends or other financial supports for
meeting licensure and credentialing requirements.
Many states are changing licensing
requirements to allow more flexibility
for mental health professionals.
16
Improving Mental Health Care: The Access Report
inseparable.us

Promote the use of peer and behavioral
health support specialists
Studies show the value of incorporating trained, licensed peer
support specialists and behavioral health support specialists,
including community health workers and paraprofessionals,
into the mental health workforce. These specialists can expand
workforce capacity and fill crucial gaps in care. For example, peer
support specialists can help people understand their diagnosis,
engage in treatment, and support their recovery. They may also
provide additional services, such as assistance with securing
benefits, housing, or employment. These non-clinical services
help people navigate the health care system, lower emergency
department and hospitalization use, and expand the system’s
capacity to meet individuals’ needs.
State policies that work
LEVERAGE THE MENTAL HEALTH WORKFORCE
What states
can do
Require state Medicaid plans to cover peer
and behavioral health support services,
including for youth.
Open pathways for training of peer and
behavioral health support specialists.
Encourage the integration of these specialists
into health care teams, including crisis
response teams.
Peer support specialists can help
people understand their diagnosis,
engage in treatment, and support
their recovery.
17
Improving Mental Health Care: The Access Report
inseparable.us

Provide competitive reimbursement rates
for providers
Policies that support competitive compensation for mental
health providers are essential to broadening the mental health
workforce. In a major study of private health plans, analysts found
that U.S. psychiatrists were paid an average of 20% less than
primary care physicians using the same or equivalent billing codes,
despite having more training. Other mental health professionals –
especially trained peer support specialists – are often reimbursed
at rates that don’t reflect the rising need and demand for services.
When mental health providers are not paid enough, they may
leave insurance networks or even leave their profession, further
reducing access to care.
State policies that work
LEVERAGE THE MENTAL HEALTH WORKFORCE
What states
can do
Require reimbursement rates that reflect
living wages, payment parity with other
medical professions, and market demand.
Require public posting of Medicaid
reimbursement rates.
In a major study of private health plans,
analysts found that U.S. psychiatrists
were paid an average of 20% less than
primary care physicians using the same
or equivalent billing codes, despite
having more training.
18
Improving Mental Health Care: The Access Report
inseparable.us

Studies show the value of both
prevention and early intervention in
reducing and addressing mental health
and substance use issues.
The sooner people find effective care, the sooner they can recover – enabling
them to thrive at home, school, work, and in the community. Prevention and
early intervention also trim health care costs, which benefits individuals, health
care systems, and the economy.
Early intervention depends on easy access to services and supports when
signs of a mental health condition first show up.
To support young people and adults in getting treatment
early, states can adopt policies that:
State policies
that work
3
PROMOTE PREVENTION
AND EARLY INTERVENTION
Cover annual mental health
screenings and wellness exams.
Waive requirements of
a formal diagnosis for
reimbursement of mental
health care.
Address the impact of
social determinants or drivers
of health.
Integrate mental health care
with primary care.
19
Improving Mental Health Care: The Access Report
inseparable.us

Cover annual mental health screenings
and wellness exams
Research shows that the earlier a person gets effective mental
health treatment, the better the outcomes. In contrast, treatment
delays lead to worsening mental health conditions that are
more complex and harder to treat. Making annual mental health
screenings widely available in a wide range of settings can identify
risks early and even prevent conditions from developing.
State policies that work
PROMOTE PREVENTION AND EARLY INTERVENTION
What states
can do
Require insurance companies to cover
yearly mental wellness exams without
cost-sharing.
Offer incentives for wider use of
trauma-informed mental health
screenings.
Research shows that the
earlier a person gets effective
mental health treatment, the
better the outcomes.
20
Improving Mental Health Care: The Access Report
inseparable.us

Waive formal diagnosis requirements
for mental health care
In many states, providers are not allowed to bill for mental health
services unless their young patient has a formal diagnosis. This
flawed rule puts the cart before the horse by making families
accept a formal diagnosis before gaining access to the care
that keeps mental health issues from escalating. Further, formal
diagnoses are not always appropriate: for example, a child may
experience anxiety or depression in the wake of a death or other
traumatic event, yet not develop a lasting mental health condition.
States can clear the way for youth to get the care they need by
removing the formal diagnosis requirement for billing.
State policies that work
PROMOTE PREVENTION AND EARLY INTERVENTION
What states
can do
Require Medicaid and private insurance
coverage of certain youth mental
health services without requiring
a formal diagnosis.
States can clear the way for youth
to get the care they need by
removing the formal diagnosis
requirement for billing.
21
Improving Mental Health Care: The Access Report
inseparable.us

Address social determinants or
drivers of health
Social determinants or drivers of health (SDOH) are factors that
have a strong influence on individual and family health. They
include housing, nutrition, health benefits, social support networks,
transportation, education, and employment – all vital in promoting
timely access to care and better health outcomes. Waivers based
on SDOH and health-related social needs (HRSN) have been
shown to reduce health disparities.
Unhoused people, for example, often struggle to manage mental
health issues, partly because it can be so hard to find care and
stick with a treatment plan. States are now using 1115 waivers to
address health-related social needs such as housing and nutrition
services to help high-need populations get care and experience
better outcomes.
State policies that work
PROMOTE PREVENTION AND EARLY INTERVENTION
What states
can do
Pursue Medicaid 1115 waivers to
address SDOH/HRSN for people
with mental health or multiple
(co-occurring) conditions.
Waivers based on social determinants
or drivers of health and health-related
social needs have been shown to
reduce health disparities.
22
Improving Mental Health Care: The Access Report
inseparable.us
Integrate mental health care
with primary care
Integrated health care brings primary health and mental
health services together in a single setting where people
and families can receive coordinated, effective treatment.
Studies show that integrated care not only increases access
to mental health services, it also improves health outcomes
and reduces costs. In addition, integrated care reduces the
perception of stigma and helps overcome this barrier to
seeking and receiving essential services.
State policies that work
PROMOTE PREVENTION AND EARLY INTERVENTION
What states
can do
The Collaborative
Care Model (CoCM)
and Primary Care
Behavioral Health
(PCBH) model are
proven approaches
to providing
integrative care.
With CoCM, the team is led
by a primary care provider
and includes a psychiatrist
and other mental health care
professionals. Care is patient-
centered, outcome-driven,
and evidence-based.
With PCBH, a mental health
professional joins the primary
care team to foster a more
coordinated approach to all
health conditions, from stress
to pain management and
prevention of future illness.
Services are provided to all
patients, whether or not they
have a prior mental health
diagnosis.
Provide financial support for health systems
to adopt effective models of integrated care.
Allow Medicaid billing for mental and primary
care services delivered on the same day.
Require reimbursement for mental health benefits
provided through CoCM or PCBH models.
Expand delivery of primary care services in
community-based programs such as Certified
Community Behavioral Health Clinics.
Review licensing regulations and develop
credentialing programs to reduce burdens
for peer support specialists, community health
providers, and other professionals who are
part of integrated care models.
Offer financial incentives for providers who
reduce health disparities for people with
mental health conditions.
23
Improving Mental Health Care: The Access Report
inseparable.us

State progress:
improving access to care
Meaningful
progress
Partial
progress
Little or no
progress
State policymakers across the
country have the power to improve
access to mental health care.
Inseparable’s state snapshots provide an overview of
each state’s progress in adopting a range of policies
in the categories below that make mental health care
easier to find, easier to pay for, and more effective for
individuals and their families.
1 EXPAND COVERAGE OF CARE
Policy goal Scoring
Require plans to use transparent,
nonprofit clinical guidelines and cover
all medically necessary treatment
Enacted legislation
No enacted legislation
Cover out-of-network care at no extra
cost if timely in-network care
is not available
Enacted legislation
No enacted legislation
Extend Medicaid eligibility
to low-income adults
Adopted
Adopted, but not implemented
Not adopted
Provide Medicaid coverage
to persons prior to release
from custody
Approved reentry waiver
Pending reentry waiver
No reentry waiver
24
Improving Mental Health Care: The Access Report
inseparable.us

2 LEVERAGE THE MENTAL HEALTH WORKFORCE
Policy goal Scoring
Cover telemental health services in
commercial insurance and reimburse
at in-person rates
Required coverage at in-person rates
Coverage OR in-person rate requirement
No coverage or reimbursement requirement
Join the Psychology
Interjurisdictional Compact
Enacted legislation
Enacted, but not implemented
No enacted legislation
Join the Counseling Compact
Enacted legislation
Enacted, but not implemented
No enacted legislation
Join the Social Work Licensure
Compact
Enacted legislation
Enacted, but not implemented
No enacted legislation
Cover trained peer support
specialists in state Medicaid plan
Covered in Medicaid plan
Limited coverage in Medicaid plan
Not covered in Medicaid plan
3 PROMOTE PREVENTION AND EARLY INTERVENTION
Policy goal Scoring
Cover annual mental health wellness
exams without co-pays
Enacted legislation
No enacted legislation
Adopt state Medicaid waiver to
cover social determinants of health
Approved health-related social needs waiver
Pending or limited approved waiver
No health-related social needs waiver
Cover the Collaborative Care
Model of integrated mental health
and primary care services in
commercial insurance plans
Enacted legislation
No enacted legislation
Cover the Collaborative Care
Model of integrated mental health
and primary care services in the
state Medicaid plan
Enacted legislation
No enacted legislation
25
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
ALABAMA
867
people living in
Alabama have a
diagnosed mental
health condition
THOUSAND
52.5%
19.2%
10.0%
Only 20.7% received specialty care*
Only 37.3% received specialty care*
only
26.3%
17.5
16.2
26
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
ALABAMA
27
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
ALASKA
138
people living in
Alaska have a
diagnosed mental
health condition
THOUSAND
47.4%
25.7%
10.8%
Only 39.6% received specialty care*
Only 38.3% received specialty care*
only
30.8%
18.3
26.7
28
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
ALASKA
29
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
ARIZONA
people living in
Arizona have a
diagnosed mental
health condition
MILLION
50.4%
21.3%
10.6%
Only 27.5% received specialty care*
Only 52.7% received specialty care*
only
33.3%
28.0
18.3
1.21
30
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
ARIZONA
31
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
ARKANSAS
524
people living in
Arkansas have a
diagnosed mental
health condition
THOUSAND
46.6%
27.0%
9.2%
Only 24.9% received specialty care*
Only 39.4% received specialty care*
only
36.5%
15.2
18.8
32
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
ARKANSAS
33
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
CALIFORNIA
people living in
California have a
diagnosed mental
health condition
MILLION
54.0%
26.5%
7.0%
Only 30.0% received specialty care*
Only 46.0% received specialty care*
only
33.7%
17.3
10.5
6.84
34
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
CALIFORNIA
35
Improving Mental Health Care: The Access Report
inseparable.us
STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
COLORADO
people living in
Colorado have a
diagnosed mental
health condition
MILLION
58.3%
18.5%
8.0%
Only 25.4% received specialty care*
Only 43.9% received specialty care*
only
30.2%
20.7
21.3
1.11
36
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
COLORADO
37
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
CONNECTICUT
573
people living in
Connecticut have a
diagnosed mental
health condition
THOUSAND
57.4%
22.6%
5.1%
Only 30.0% received specialty care*
Only 57.9% received specialty care*
only
37.4%
34.2
10.4
38
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
CONNECTICUT
39
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
DELAWARE
156
people living in
Delaware have a
diagnosed mental
health condition
THOUSAND
54.9%
20.6%
5.7%
Only 40.6% received specialty care*
Only 47.9% received specialty care*
only
34.8%
43.7
11.6
40
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
DELAWARE
41
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH MEDICAID
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
ARE UNINSURED
WITH MEDICAID
Includes dual-eligibles
covered by both
Medicare and Medicaid.
DISTRICT OF COLUMBIA
153
people living
in D.C. have a
diagnosed mental
health condition
THOUSAND
61.8%
Only 65.1% received specialty care*
46.6
6.2
24.9%
3.7%
Data
unavailable
for % of
people visiting
the ER or
hospital for
mental health
or substance
use treatment
who get follow-
up care within
30 days.
Data unavailable
FOR COMMERCIAL INSURANCE
42
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
DISTRICT OF COLUMBIA
43
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
FLORIDA
3.61
people living in
Florida have a
diagnosed mental
health condition
MILLION
50.4%
17.8%
12.1%
Only 18.2% received specialty care*
Only 46.5% received specialty care*
only
28.0%
26.7
14.1
44
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
FLORIDA
45
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
GEORGIA
1.87
people living in
Georgia have a
diagnosed mental
health condition
MILLION
54.4%
18.0%
12.7%
Only 27.3% received specialty care*
Only 36.9% received specialty care*
only
33.2%
14.8
14.0
46
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
GEORGIA
47
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
HAWAII
227
people living in
Hawaii have a
diagnosed mental
health condition
THOUSAND
55.5%
20.4%
3.6%
Only 43.0% received specialty care*
Only 47.1% received specialty care*
only
29.8%
17.2
13.5
48
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
HAWAII
49
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
IDAHO
377
people living
in Idaho have a
diagnosed mental
health condition
THOUSAND
54.5%
20.1%
8.5%
Only 31.4% received specialty care*
Only 44.5% received specialty care*
only
34.4%
14.9
22.4
50
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
IDAHO
51
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
ILLINOIS
2.09
people living in
Illinois have a
diagnosed mental
health condition
MILLION
58.4%
19.8%
6.9%
Only 23.4% received specialty care*
Only 37.4% received specialty care*
only
30.7%
23.8
10.9
52
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
ILLINOIS
53
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
INDIANA
1.21
people living in
Indiana have a
diagnosed mental
health condition
MILLION
57.0%
19.8%
7.5%
Only 26.2% received specialty care*
Only 57.8% received specialty care*
only
38.2%
28.0
15.4
54
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
INDIANA
55
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
IOWA
612
people living in Iowa
have a diagnosed
mental health
condition
THOUSAND
58.6%
20.0%
4.9%
Only 36.4% received specialty care*
Only 49.2% received specialty care*
only
37.0%
11.3
16.0
56
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
IOWA
57
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
KANSAS
502
people living in
Kansas have a
diagnosed mental
health condition
THOUSAND
59.0%
15.2%
9.2%
Only 27.2% received specialty care*
Only 46.5% received specialty care*
only
36.6%
14.2
18.6
58
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
KANSAS
59
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
KENTUCKY
788
people living in
Kentucky have a
diagnosed mental
health condition
THOUSAND
48.9%
28.9%
5.6%
Only 21.2% received specialty care*
Only 47.5% received specialty care*
only
31.0%
35.6
17.1
60
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
KENTUCKY
61
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
LOUISIANA
812
people living in
Louisiana have a
diagnosed mental
health condition
THOUSAND
45.4%
32.0%
7.5%
Only 26.1% received specialty care*
Only 42.0% received specialty care*
only
31.6%
30.8
14.6
62
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
LOUISIANA
63
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MAINE
258
people living
in Maine have a
diagnosed mental
health condition
THOUSAND
55.3%
19.5%
5.4%
Only 22.6% received specialty care*
Only 48.9% received specialty care*
only
44.2%
30.1
17.8
64
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MAINE
65
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MARYLAND
1.08
people living in
Maryland have a
diagnosed mental
health condition
MILLION
58.6%
20.3%
6.1%
Only 34.0% received specialty care*
Only 48.5% received specialty care*
only
39.2%
41.1
9.8
66
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MARYLAND
67
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MASSACHUSETTS
1.26
people living in
Massachusetts have
a diagnosed mental
health condition
MILLION
60.6%
23.2%
2.5%
Only 41.2% received specialty care*
Only 55.1% received specialty care*
only
48.6%
32.6
9.0
68
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MASSACHUSETTS
69
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MICHIGAN
1.69
people living in
Michigan have a
diagnosed mental
health condition
MILLION
54.9%
23.5%
5.1%
Only 29.7% received specialty care*
Only 51.6% received specialty care*
only
35.1%
25.8
14.1
70
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MICHIGAN
71
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MINNESOTA
1.08
people living in
Minnesota have a
diagnosed mental
health condition
MILLION
61.3%
18.5%
4.3%
Only 36.1% received specialty care*
Only 55.5% received specialty care*
only
41.4%
14.7
13.5
72
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MINNESOTA
73
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MISSISSIPPI
482
people living in
Mississippi have a
diagnosed mental
health condition
THOUSAND
47.6%
24.0%
11.9%
Only 18.5% received specialty care*
Only 42.7% received specialty care*
only
22.7%
14.4
13.9
74
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MISSISSIPPI
75
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MISSOURI
1.14
people living in
Missouri have a
diagnosed mental
health condition
MILLION
58.3%
14.7%
9.3%
Only 23.2% received specialty care*
Only 44.7% received specialty care*
only
31.4%
27.5
18.6
76
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MISSOURI
77
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
MONTANA
299
people living in
Montana have a
diagnosed mental
health condition
THOUSAND
52.1%
19.8%
8.0%
Only 32.9% received specialty care*
Only 53.8% received specialty care*
only
32.3%
13.4
26.4
78
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
MONTANA
79
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NEBRASKA
349
people living in
Nebraska have a
diagnosed mental
health condition
THOUSAND
62.0%
14.9%
7.0%
Only 36.7% received specialty care*
Only 60.0% received specialty care*
only
40.6%
8.8
14.4
80
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NEBRASKA
81
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NEVADA
613
people living in
Nevada have a
diagnosed mental
health condition
THOUSAND
52.3%
20.8%
11.4%
Only 26.0% received specialty care*
Only 42.3% received specialty care*
only
25.9%
23.4
20.0
82
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NEVADA
83
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NEW HAMPSHIRE
246
people living in
New Hampshire have
a diagnosed mental
health condition
THOUSAND
62.7%
13.5%
5.0%
Only 28.3% received specialty care*
Only 49.0% received specialty care*
only
42.2%
30.7
17.9
84
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NEW HAMPSHIRE
85
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NEW JERSEY
1.36
people living in
New Jersey have a
diagnosed mental
health condition
MILLION
60.3%
18.4%
7.2%
Only 28.9% received specialty care*
Only 45.9% received specialty care*
only
37.3%
32.0
7.8
86
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NEW JERSEY
87
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NEW MEXICO
people living in
New Mexico have a
diagnosed mental
health condition
THOUSAND
38.4%
34.4%
10%
Only 34.8% received specialty care*
Only 50.4% received specialty care*
only
30.3%
30.5
23.8
393
88
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NEW MEXICO
89
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NEW YORK
people living in
New York have a
diagnosed mental
health condition
MILLION
53.5%
27.6%
5.2%
Only 33.7% received specialty care*
Only 21.0% received specialty care*
only
23.8%
21.0
8.2
3.12
90
Improving Mental Health Care: The Access Report
inseparable.us
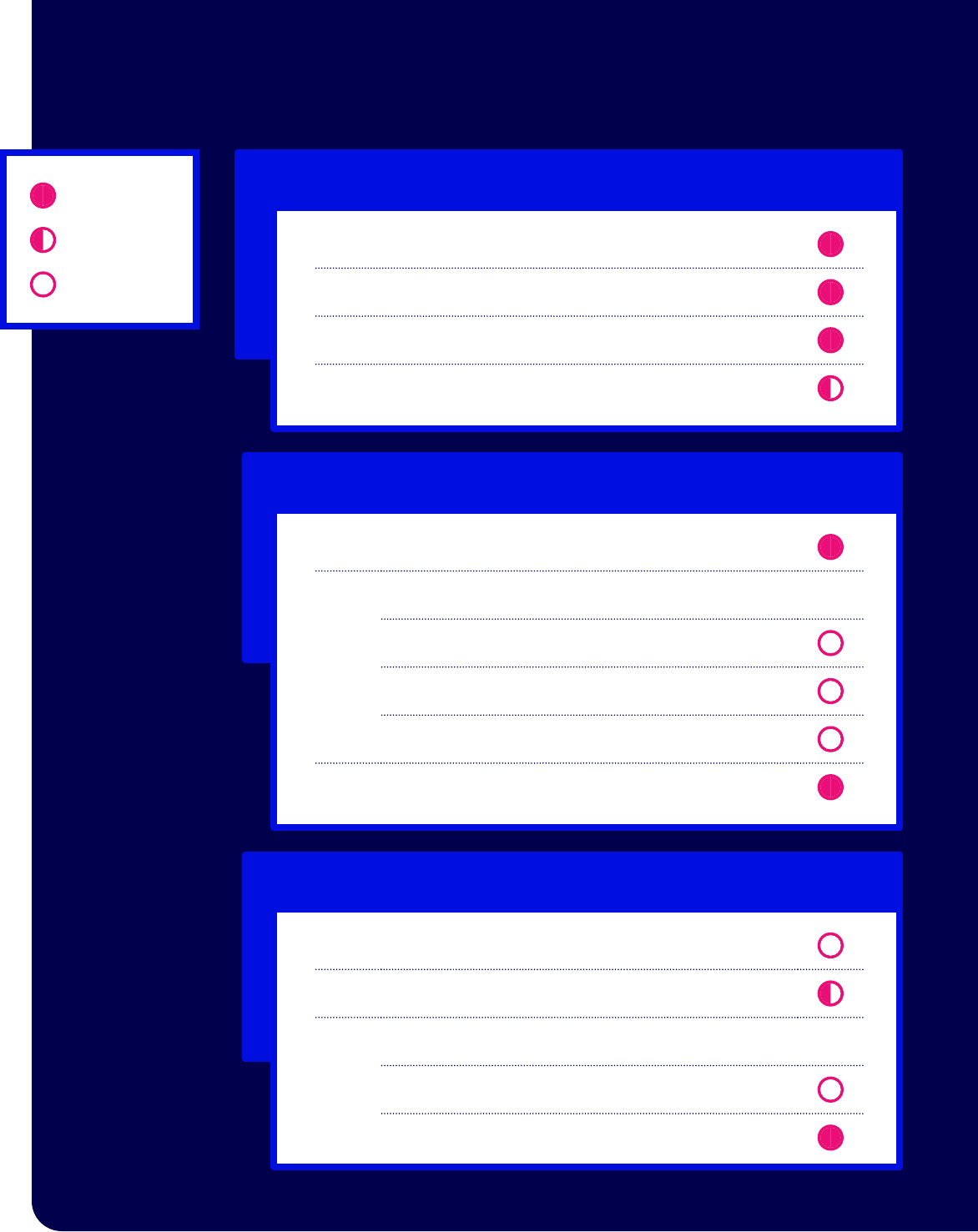
STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NEW YORK
*
* Effective January 1, 2025.
91
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NORTH CAROLINA
people living in
North Carolina have
a diagnosed mental
health condition
MILLION
52.9%
18.8%
10.4%
Only 26.2% received specialty care*
Only 35.3% received specialty care*
only
28.5%
24.4
13.4
1.81
92
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NORTH CAROLINA
93
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NORTH DAKOTA
people living in
North Dakota have
a diagnosed mental
health condition
THOUSAND
65.4%
9.8%
7.7%
Only 27.3% received specialty care*
Only 39.7% received specialty care*
only
33.5%
11.6
19
148
94
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
NORTH DAKOTA
95
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
OHIO
people living
in Ohio have a
diagnosed mental
health condition
MILLION
55.1%
21.6%
6.5%
Only 31.3% received specialty care*
Only 51.2% received specialty care*
only
35.9%
38.3
14.6
2.19
96
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
OHIO
97
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
OKLAHOMA
people living in
Oklahoma have a
diagnosed mental
health condition
THOUSAND
48.4%
20.1%
13.8%
Only 25.0% received specialty care*
Only 45.9% received specialty care*
only
29.8%
17.9
20.5
824
98
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
OKLAHOMA
99
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
OREGON
people living in
Oregon have a
diagnosed mental
health condition
THOUSAND
52.8%
23.8%
6.1%
Only 39.8% received specialty care*
Only 50.2% received specialty care*
only
33.8%
15.5
18.9
915
100
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
OREGON
101
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
PENNSYLVANIA
people living in
Pennsylvania have
a diagnosed mental
health condition
MILLION
56.9%
20.8%
5.4%
Only 33.6% received specialty care*
Only 46.9% received specialty care*
only
36.3%
36.4
14.2
2.24
102
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
PENNSYLVANIA
103
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
RHODE ISLAND
people living in
Rhode Island have
a diagnosed mental
health condition
THOUSAND
56.2%
23.9%
4.3%
Only 36.8% received specialty care*
Only 58.2% received specialty care*
only
46.5%
32.2
10.4
226
104
Improving Mental Health Care: The Access Report
inseparable.us
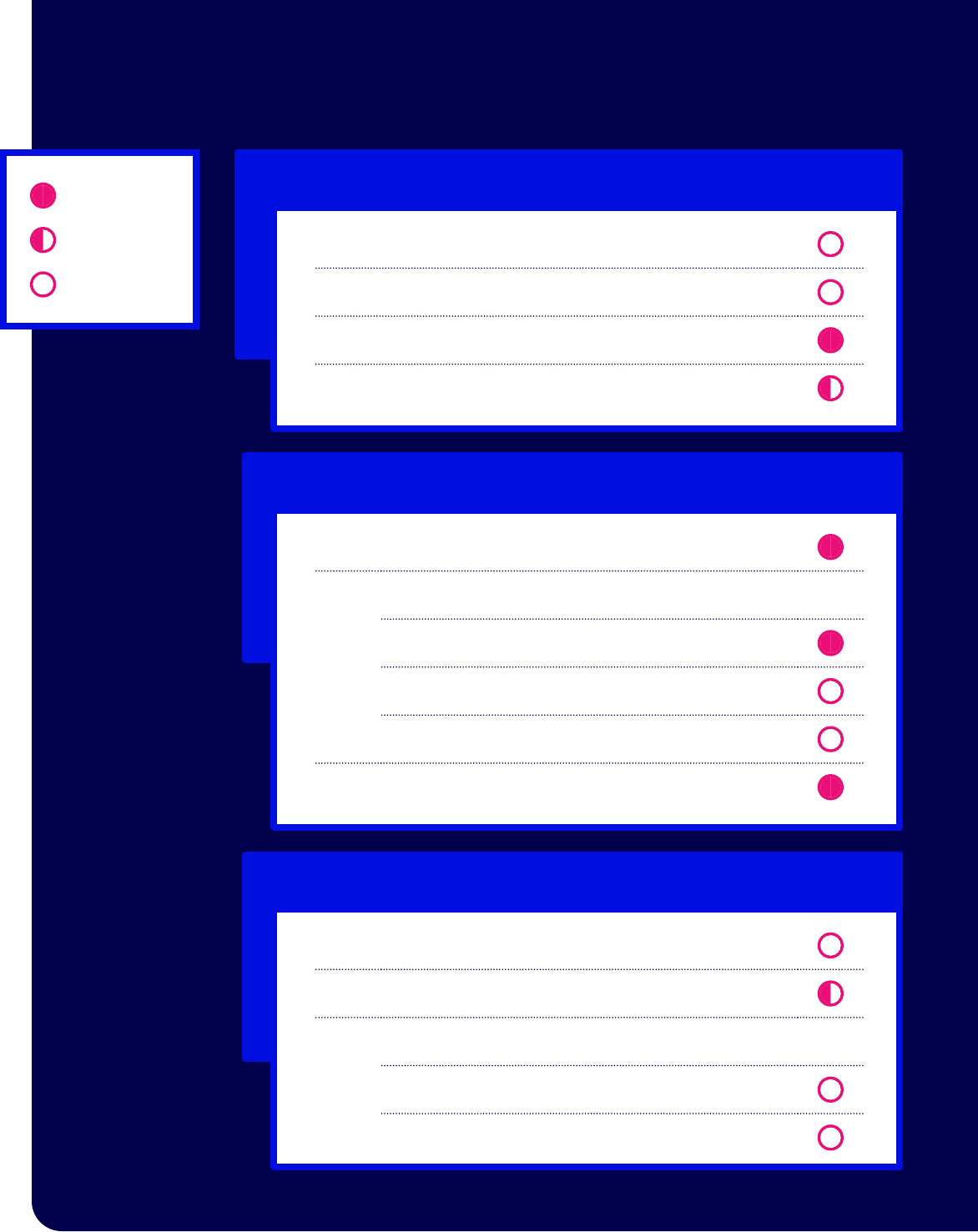
STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
RHODE ISLAND
105
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
SOUTH CAROLINA
people living in
South Carolina have
a diagnosed mental
health condition
THOUSAND
50.7%
20.1%
10.0%
Only 19.6% received specialty care*
Only 34.6% received specialty care*
only
24.8%
25.8
16.0
892
106
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
SOUTH CAROLINA
107
Improving Mental Health Care: The Access Report
inseparable.us
STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
SOUTH DAKOTA
people living in
South Dakota have
a diagnosed mental
health condition
THOUSAND
58.6%
13.8%
9.4%
Only 33.0% received specialty care*
Only 48.5% received specialty care*
only
31.6%
8.5
20.8
154
108
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
SOUTH DAKOTA
109
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
TENNESSEE
people living in
Tennessee have a
diagnosed mental
health condition
MILLION
53.5%
19.6%
10.1%
Only 16.2% received specialty care*
Only 41.4% received specialty care*
only
28.9%
33.9
16.8
1.32
110
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
TENNESSEE
111
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
TEXAS
people living
in Texas have a
diagnosed mental
health condition
MILLION
52.2%
16.9%
18.0%
Only 17.7% received specialty care*
Only 37.1% received specialty care*
only
24.7%
11.8
13.3
4.69
112
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
TEXAS
113
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
UTAH
people living
in Utah have a
diagnosed mental
health condition
THOUSAND
68.4%
11.0%
9.1%
Only 33.1% received specialty care*
Only 33.2% received specialty care*
only
38.4%
18.9
21.7
601
114
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
UTAH
115
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
VERMONT
people living in
Vermont have a
diagnosed mental
health condition
THOUSAND
54.0%
24.8%
3.4%
Only 24.8% received specialty care*
Only 50.6% received specialty care*
only
30.5%
25.4
17.7
132
116
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
VERMONT
117
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
VIRGINIA
people living in
Virginia have a
diagnosed mental
health condition
MILLION
58.7%
15.5%
6.8%
Only 28.7% received specialty care*
Only 48.8% received specialty care*
only
31.2%
20.4
13.4
1.46
118
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
VIRGINIA
119
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
WASHINGTON
people living in
Washington have a
diagnosed mental
health condition
MILLION
56.8%
21.0%
6.5%
Only 40.2% received specialty care*
Only 51.1% received specialty care*
only
32.5%
18.2
15.7
1.60
120
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
WASHINGTON
121
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
WEST VIRGINIA
people living in
West Virginia have
a diagnosed mental
health condition
THOUSAND
45.8%
28.1%
6.2%
Only 22.9% received specialty care*
Only 40.8% received specialty care*
only
30.1%
56.8
19.9
335
122
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
WEST VIRGINIA
123
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
WISCONSIN
people living in
Wisconsin have a
diagnosed mental
health condition
MILLION
59.8%
18.1%
5.4%
Only 36.9% received specialty care*
Only 47.0% received specialty care*
only
36.3%
21.8
14.7
1.08
124
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
WISCONSIN
125
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
WYOMING
people living in
Wyoming have a
diagnosed mental
health condition
THOUSAND
58.0%
11.5%
11.5%
Only 30.2% received specialty care*
Only 47.2% received specialty care*
only
35.9%
14.0
27.4
113
126
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving Access to Care
Expand coverage of care
1
Leverage the mental health workforce
Cover telemental health services in commercial insurance
and reimburse at in-person rates
Join interstate licensure compacts, such as:
Psychology Interjurisdictional Compact
(PSYPACT)
Counseling Compact
Social Work Licensure Compact
Cover trained peer support specialists in
state Medicaid plan
2
Promote prevention and early intervention
Cover annual mental health wellness exams
without co-pays
determinants of health
Cover the Collaborative Care Model of integrated
mental health and primary care services in:
Commercial insurance plans
State Medicaid plan
3
Meaningful
progress
Partial
progress
Little or no
progress
Require plans to use transparent, nonprofit clinical
guidelines and cover all medically necessary treatment
Cover out-of-network care at no extra cost
if timely in-network care is not available
Extend Medicaid eligibility to low-income adults
Provide Medicaid coverage to persons prior
to release from custody
WYOMING
127
Improving Mental Health Care: The Access Report
inseparable.us

STATE PROGRESS:
Improving
Access to Care
Coverage
Snapshot
Percentages of the
population with either
commercial insurance,
Medicaid, or no insurance.
Regardless of type of health
coverage, people with mental
health diagnoses are being
under treated.
WITH COMMERCIAL INSURANCE
WITH MEDICAID
Among people
visiting the ER
or hospital for
mental health or
substance use
treatment,
get follow-up
care within
30 days.
Drug overdose
deaths per
100,000
Suicides per
100,000
WITH COMMERCIAL
INSURANCE
WITH MEDICAID
ARE UNINSURED
Includes dual-eligibles
covered by both
Medicare and Medicaid.
Note: Percentages do not equal
100% as some people have
Medicare or military coverage.
* Specialty care is defined as care from a behavioral health specialist in an inpatient,
outpatient, or professional setting.
Sources: SAMHSA, 2021 National Survey on Drug Use and Health: Model-Based
Estimated Totals (prevalence of mental health conditions) and Milliman, “Access
Across America” (2023) Inseparable.us/accessacrossamerica (all other data).
NATIONWIDE
54.6%
21.1%
8.6%
Only 30.7% received specialty care
Only 44.3% received specialty care
only
33.8%
23.3
13.8
57.8
people living in
the U.S. have a
diagnosed mental
health condition
MILLION
128
Improving Mental Health Care: The Access Report
inseparable.us

