
Quality ID #46 (NQF 0097): Medication Reconciliation Post-Discharge
– National Quality Strategy Domain: Communication and Care Coordination
– Meaningful Measure Area: Medication Management
2019 COLLECTION TYPE:
MEDICARE PART B CLAIMS
MEASURE TYPE:
Process – High Priority
DESCRIPTION:
The percentage of discharges from any inpatient facility (e.g. hospital, skilled nursing facility, or rehabilitation facility)
for patients 18 years of age and older seen within 30 days following discharge in the office by the physician,
prescribing practitioner, registered nurse, or clinical pharmacist providing on-going care for whom the discharge
medication list was reconciled with the current medication list in the outpatient medical record
This measure is submitted as three rates stratified by age group:
• Submission Criteria 1: 18-64 years of age
• Submission Criteria 2: 65 years and older
• Total Rate: All patients 18 years of age and older
INSTRUCTIONS:
This measure is to be submitted at an outpatient visit occurring within 30 days of each inpatient facility discharge
date during the performance period. This measure is appropriate for use in the ambulatory setting only. There is no
diagnosis associated with this measure. This measure may be submitted by Merit-based Incentive Payment System
(MIPS) eligible clinicians who perform the quality actions described in the measure based on the services provided
and the measure-specific denominator coding. This measure is not to be submitted unless a patient has been
discharged from an inpatient facility within 30 days prior to the outpatient visit.
This measure will be calculated with 3 performance rates:
1) Performance Rate 1: Percentage of discharges from any inpatient facility (e.g., hospital, skilled nursing
facility, or rehabilitation facility) for patients 18-64 years of age seen within 30 days following discharge in
the office by the physician, prescribing practitioner, registered nurse, or clinical pharmacist providing on-
going care for whom the discharge medication list was reconciled with the current medication list in the
outpatient medical record
2) Performance Rate 2: Percentage of discharges from any inpatient facility (e.g., hospital, skilled nursing
facility, or rehabilitation facility) for patients 65 years and older seen within 30 days following discharge in
the office by the physician, prescribing practitioner, registered nurse, or clinical pharmacist providing on-
going care for whom the discharge medication list was reconciled with the current medication list in the
outpatient medical record
3) Total Rate (Overall Performance Rate): Percentage of discharges from any inpatient facility (e.g., hospital,
skilled nursing facility, or rehabilitation facility) for patients 18 years of age and older seen within 30 days
following discharge in the office by the physician, prescribing practitioner, registered nurse, or clinical
pharmacist providing on-going care for whom the discharge medication list was reconciled with the current
medication list in the outpatient medical record
Measure Submission Type:
Measure data may be submitted by individual MIPS eligible clinicians using Medicare Part B claims. The listed
denominator criteria are used to identify the intended patient population. The numerator quality-data codes included

in this specification are used to submit the quality actions allowed by the measure on the claim form(s). All measure-
specific coding should be submitted on the claim(s) representing the denominator eligible encounter and selected
numerator option.
DENOMINATOR:
All discharges from any inpatient facility (e.g., hospital, skilled nursing facility, or rehabilitation facility) for patients 18
years of age and older seen within 30 days following discharge in the office by the physician, prescribing practitioner,
registered nurse, or clinical pharmacist providing on-going care.
DENOMINATOR NOTE: This denominator is based on discharges followed by an office visit, not patients.
Patients may appear in the denominator more than once if there was more than one discharge followed by
an office visit in the performance period.
Denominator Criteria (Eligible Cases):
SUBMISSION CRITERIA 1: Patients 18-64 years of age on date of encounter
SUBMISSION CRITERIA 2: Patients aged 65 years and older on date of encounter
SUBMISSION CRITERIA 3: All Patients 18 years of age and older
AND
Patient encounter during the performance period (CPT or HCPCS): 90791, 90792, 90832, 90834,
90837, 90839, 90845, 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215, 99324,
99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347,
99348, 99349, 99350, 99495, 99496, G0402, G0438, G0439
AND
Patient discharged from an inpatient facility (e.g., hospital, skilled nursing facility, or rehabilitation
facility) within the last 30 days
NUMERATOR (SUBMISSION CRITERIA 1 & 2 & 3):
Medication reconciliation conducted by a prescribing practitioner, clinical pharmacists or registered nurse on or within
30 days of discharge
Definition:
Medication Reconciliation – A type of review in which the discharge medications are reconciled with the
most recent medication list in the outpatient medical record. Documentation in the outpatient medical record
must include evidence of medication reconciliation and the date on which it was performed. Any of the
following evidence meets criteria: (1) Documentation of the current medications with a notation that
references the discharge medications (e.g., no changes in meds since discharge, same meds at discharge,
discontinue all discharge meds), (2) Documentation of the patient’s current medications with a notation that
the discharge medications were reviewed, (3) Documentation that the provider “reconciled the current and
discharge meds,” (4) Documentation of a current medication list, a discharge medication list and notation
that the appropriate practitioner type reviewed both lists on the same date of service, (5) Notation that no
medications were prescribed or ordered upon discharge; (6) Documentation that patient was seen for post-
discharge follow-up with evidence of medication reconciliation or review, (7) Documentation in the discharge
summary that the discharge medications were reconciled with the current medications; the discharge
summary must be in the outpatient chart.
NUMERATOR NOTE: Medication reconciliation should be completed and documented on or within 30 days
of discharge. If the patient has an eligible discharge but medication reconciliation is not performed and
documented within 30 days, submit 1111F with 8P.
Numerator Quality-Data Coding Options:
Patient receiving Hospice Services, Patient Not Eligible:

Denominator Exclusion: G9691: Patient had hospice services any time during the
measurement period
OR
Documentation of Reconciliation of Discharge Medication with Current Medication List in the
Medical Record
Performance Met: CPT II 1111F: Discharge medications reconciled with the current
medication list in outpatient medical record
OR
Discharge Medication not Reconciled with Current Medication List in the Medical Record, Reason
Not Otherwise Specified
Append a submission modifier (8P) to CPT Category II code 1111F to submit circumstances when the
action described in the numerator is not performed and the reason is not otherwise specified.
Performance Not Met: 1111F with 8P: Discharge medications not reconciled with the current
medication list in outpatient medical record, reason
not otherwise specified
RATIONALE:
Medications are often changed while a patient is hospitalized. Continuity between inpatient and on-going care is
essential.
CLINICAL RECOMMENDATION STATEMENTS:
Medication reconciliation post-discharge is an important step to catch potentially harmful omissions or changes in
prescribed medications, particularly in elderly patients that are prescribed a greater quantity and variety of
medications (Leape, 1991). Although the magnitude of the effect of medication reconciliation alone on patient
outcomes is not well studied, there is agreement among experts that potential benefits outweigh the harm (Coleman,
2003; Pronovost, 2003; IOM, 2002; IOM, 2006). Medication reconciliation post-discharge is recommended by the
Joint Commission patient safety goals (Kienle, 2008), the American Geriatric Society (Coleman, 2003), Society of
Hospital Medicine (Kripalani, 2007; Grennwald, 2010), ACOVE (Assessing Care of Vulnerable Elders; Knight, 2001),
and the Task Force on Medicines Partnership (2005). Additionally, measurement of medication reconciliation post-
discharge has been cited by the National Quality Forum and the National Priorities Partnership as a measurement
priority area (NQF, 2010)
No trials of the effects of physician acknowledgment of medications post-discharge were found. However, patients
are likely to have their medications changed during a hospitalization. Estimates suggest that 46% of medication
errors occur on admission or discharge from a hospital (Pronovost, 2003). Therefore, medication reconciliation is a
critical piece of care coordination post-discharge for all individuals who use prescription medications. Prescription
medication use is common among adults of all ages, particularly older adults and adults with chronic conditions. On
average, 82% of adults in the U.S. are taking at least one medication (prescription or nonprescription,
vitamin/mineral, herbal/natural supplement); 29% are taking five or more. Older adults are the biggest consumers of
medications with 17-19% of people 65 and older taking at least ten medications in a given week (Slone Survey,
2006).
One observational study showed that 1.5 new medications were initiated per patient during hospitalization, and 28%
of chronic medications were canceled by the time of hospital discharge. Another observational study showed that at
one week post-discharge, 72% of elderly patients were taking incorrectly at least one medication started in the
inpatient setting, and 32% of medications were not being taken at all. One survey study faulted the quality of
discharge communication as contributing to early hospital readmission, although this study did not implicate
medication discontinuity as the cause. (ACOVE)
Implementing routine medication reconciliation after discharge from an inpatient facility is an important step to ensure
medication errors are addressed and patients understand their new medications. The process of resolving

discrepancies in a patient’s medication list reduces the risk of these adverse drug interactions being overlooked and
helps physicians minimize the duplication and complexity of the patient’s medication regimen (Wenger, 2004). This in
turn may increase patient adherence to the medication regimen and reduce hospital readmission rates.
First, a medication list must be collected. It is important to know what medications the patient has been taking or
receiving prior to the outpatient visit in order to provide quality care. This applies regardless of the setting from which
the patient came — home, long-term care, assisted living, etc. The medication list should include all medications
(prescriptions, over-the-counter, herbals, supplements, etc.) with dose, frequency, route, and reason for taking it. It is
also important to verify whether the patient is actually taking the medication as prescribed or instructed, as
sometimes this is not the case.
At the end of the outpatient visit, a clinician needs to verify three questions:
1) Based on what occurred in the visit, should any medication that the patient was taking or receiving prior to
the visit be discontinued or altered?
2) Based on what occurred in the visit, should any prior medication be suspended pending consultation with
the prescriber?
3) Have any new prescriptions been added today?
These questions should be reviewed by the physician who completed the procedure, or the physician who evaluated
and treated the patient.
• If the answer to all three questions is “no,” the process is complete.
• If the answer to any question is “yes,” the patient needs to receive clear instructions about what to do — all
changes, holds, and discontinuations of medications should be specifically noted. Include any follow-up
required, such as calling or making appointments with other practitioners and a timeframe for doing so
Institute for Healthcare Improvement (IHI)
COPYRIGHT:
This Physician Performance Measure (Measure) and related data specifications were developed by the National
Committee for Quality Assurance (NCQA). The Measure is copyrighted but can be reproduced and distributed,
without modification, for noncommercial purposes (eg, use by healthcare providers in connection with their practices)
without obtaining approval from NCQA. Commercial use is defined as the sale, licensing, or distribution of the
Measure for commercial gain, or incorporation of the Measure into a product or service that is sold, licensed or
distributed for commercial gain. All commercial uses must be approved by NCQA and are subject to a license at the
discretion of NCQA. NCQA is not responsible for any use of the Measure. NCQA makes no representations,
warranties, or endorsement about the quality of any organization or physician that uses or reports performance
measures and NCQA has no liability to anyone who relies on such measures or specifications. (C) 2012-2018
National Committee for Quality Assurance. All Rights Reserved.
Limited proprietary coding is contained in the Measure specifications for user convenience. Users of proprietary code
sets should obtain all necessary licenses from the owners of the code sets. NCQA disclaims all liability for use or
accuracy of any CPT or other codes contained in the specifications.
CPT(R) contained in the Measure specifications is copyright 2004-2018 American Medical Association. LOINC(R)
copyright 2004-2018 Regenstrief Institute, Inc. This material contains SNOMED Clinical Terms(R) (SNOMED CT[R])
copyright 2004-2018 International Health Terminology Standards Development Organisation. ICD-10 copyright 2018
World Health Organization. All Rights Reserved.
The performance Measure is not a clinical guideline and does not establish a standard of medical care and has not
been tested for all potential applications.
THE MEASURE AND SPECIFICATIONS ARE PROVIDED "AS IS" WITHOUT WARRANTY OF ANY KIND.




2019 Medicare Part B Claims Flow Narrative for Quality ID#46 NQF #0097:
Medication Reconciliation Post-Discharge
Please refer to the specific section of the specification to identify the denominator and numerator information for use
in submitting this Individual Specification. This measure will be calculated with 2 Performance Rates.
Submission Criteria 1
1. Start with Denominator
2. Check Patient Age:
a. If Patient Age is 18 through 64 Years on Date of Service equals No during the performance period, do
not include in Eligible Population. Stop Processing.
b. If Patient Age is 18 through 64 Years on Date of Service equals Yes during the performance period,
proceed to check Encounter Performed.
3. Check Encounter Performed:
a. If Encounter as Listed in the Denominator equals No, do not include in Eligible Population. Stop
Processing.
b. If Encounter as Listed in the Denominator equals Yes, proceed to check Patient Discharged from
Inpatient Facility (eg Hospital Skilled Nursing Facility) Within the Last 30 Days.
4. Check Patient Discharged from Inpatient Facility (eg Hospital Skilled Nursing Facility) Within the Last 30 Days:
a. If Patient Discharged from Inpatient Facility (eg Hospital Skilled Nursing Facility) Within the Last 30
Days as Listed in the Denominator equals No, do not include in Eligible Population. Stop Processing.
b. If Patient Discharged from Inpatient Facility (eg Hospital Skilled Nursing Facility) Within the Last 30
Days as Listed in the Denominator equals Yes, include in Eligible Population.
5. Denominator Population
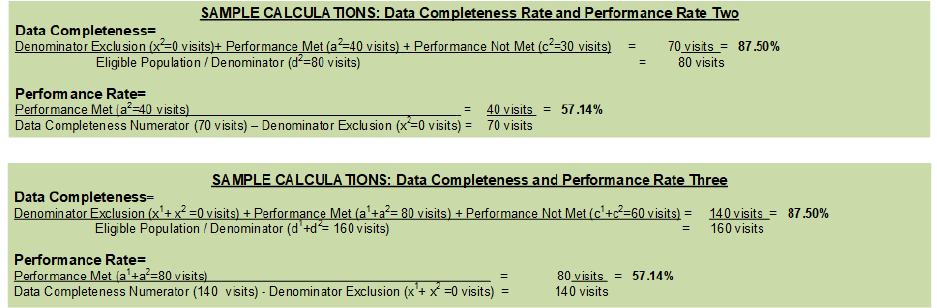
a. Denominator Population is all Eligible Visits in the Denominator. Denominator is represented as
Denominator in the Sample Calculation listed at the end of this document. Letter d
1
equals 80 visits in
the Sample Calculation.
6. Start Numerator
7. Check Patient Had Hospice Services Any Time During the Measurement Period:
a. If Patient Had Hospice Services Any Time During the Measurement Period equals Yes, include in Data
Completeness Met and Denominator Exclusion.
b. Data Completeness Met and Denominator Exclusion letter is represented as Data Completeness and
Performance Rate in the Sample Calculation listed at the end of this document. Letter x
1
equals 0 visits
in the Sample Calculation.
c. If Patient Had Hospice Services Any Time During the Measurement Period equals No, proceed to
check Discharge Medications Reconciled With Current Medication List in Outpatient Medical Record.
8. Check Discharge Medications Reconciled With the Current Medication List in Outpatient Medical Record:

a. If Discharge Medications Reconciled With the Current Medication List in Outpatient Medical Record
equals Yes, include in Data Completeness Met and Performance Met.
b. Data Completeness Met and Performance Met letter is represented as Data Completeness and
Performance Rate in the Sample Calculation listed at the end of this document. Letter a
1
equals 40
visits in the Sample Calculation.
c. If Discharge Medications Reconciled With the Current Medication List in Outpatient Medical Record
equals No, proceed to check Discharge Medications Not Reconciled with Current Medication List in the
Medical Record, Reason Not Specified.
9. Check Discharge Medications Not Reconciled with Current Medication List in the Medical Record, Reason Not
Specified:
a. If Discharge Medications Not Reconciled with Current Medication List in the Medical Record, Reason
Not Specified equals Yes, include in Data Completeness Met and Performance Not Met.
b. Data Completeness Met and Performance Not Met letter is represented as Data Completeness in the
Sample Calculation listed at the end of this document. Letter c
1
equals 30 visits in the Sample
Calculation.
c. If Discharge Medications Not Reconciled with Current Medication List in the Medical Record, Reason
Not Specified equals No, proceed to check Data Completeness Not Met.
10. Check Data Completeness Not Met:
a. If Data Completeness Not Met, the Quality Data Code was not submitted. 10 visits have been
subtracted from the Data Completeness Numerator in the Sample Calculation.

2019 Medicare Part B Claims Flow Narrative for Quality ID #46 NQF #0097:
Medication Reconciliation Post-Discharge
Please refer to the specific section of the specification to identify the denominator and numerator information for use
in submitting this Individual Specification. This measure will be calculated with 2 Performance Rates.
Submission Criteria 2
1. Start with Denominator
2. Check Patient Age:
a. If Patient Age at Date of Service is equal to or greater than 65 Years equals No during the performance
period, do not include in Eligible Population. Stop Processing.
b. If Patient Age at Date of Service is equal to or greater than 65 Years equals Yes during the
performance period, proceed to check Encounter Performed.
3. Check Encounter Performed:
a. If Encounter as Listed in the Denominator equals No, do not include in Eligible Population. Stop
Processing.
b. If Encounter as Listed in the Denominator equals Yes, proceed to check Patient Discharged from
Inpatient Facility (e.g Hospital Skilled Nursing Facility) Within the Last 30 Days.
4. Check Patient Discharged from Inpatient Facility (e.g Hospital Skilled Nursing Facility) Within the Last 30 Days:
a. If Patient Discharged from Inpatient Facility (e.g Hospital Skilled Nursing Facility) Within the Last 30
Days as Listed in the Denominator equals No, do not include in Eligible Population. Stop Processing.
b. If Patient Discharged from Inpatient Facility (e.g Hospital Skilled Nursing Facility) Within the Last 30
Days as Listed in the Denominator equals Yes, include in Eligible Population.
5. Denominator Population:
a. Denominator Population is all Eligible Visits in the Denominator. Denominator is represented as
Denominator in the Sample Calculation listed at the end of this document. Letter d
2
equals 80 visits in
the Sample Calculation.
6. Start Numerator
7. Check Patient Had Hospice Services Any Time During the Measurement Period:
a. If Patient Had Hospice Services Any Time During the Measurement Period equals Yes, include in Data
Completeness Met and Denominator Exclusion.
b. Data Completeness Met and Denominator Exclusion letter is represented in the Data Completeness
and Performance Rate in the Sample Calculation listed at the end of this document. Letter x
2
equals 0
visits in the Sample Calculation.
c. If Patient Had Hospice Services Any Time During the Measurement Period equals No, proceed to
check Discharge Medications Reconciled With the Current Medication List in Outpatient Medical
Record.
8. Check Discharge Medications Reconciled With the Current Medication List in Outpatient Medical Record:
a. If Discharge Medications Reconciled With the Current Medication List in Outpatient Medical Record
equals Yes, include in Data Completeness Met and Performance Met.
b. Data Completeness Met and Performance Met letter is represented as Data Completeness and
Performance Rate in the Sample Calculation listed at the end of this document. Letter a
2
equals 40
visits in the Sample Calculation.
c. If Discharge Medication Reconciled With the Current Medication List in Outpatient Medical Record
equals No, proceed to check Discharge Medications Not Reconciled with Current Medication List in
the Medical Record, Reason Not Specified.
9. Check Discharge Medications Not Reconciled with the Current Medication List in the Medical Record, Reason
Not Specified:
a. If Discharge Medications Not Reconciled with the Current Medication List in the Medical Record,
Reason Not Specified equals Yes, include in Data Completeness Met and Performance Not Met.
b. Data Completeness Met and Performance Not Met letter is represented as Data Completeness in the
Sample Calculation listed at the end of this document. Letter c
2
equals 30 visits in the Sample
Calculation.
c. If Discharge Medications Not Reconciled with the Current Medication List in the Medical Record,
Reason Not Specified equals No, proceed to check Data Completeness Not Met.
10. Check Data Completeness Not Met:
a. If Data Completeness Not Met, the Quality Data Code was not submitted. 10 visits have been
subtracted from the Data Completeness Numerator in the Sample Calculation.
