
Louisiana Medicaid Page 1
© 2022 Caremark. All Rights Reserved.
Louisiana Department of
Health
“The data contained in pages 16, 17, 18, 19, 30, 31, 38, 96, 113, 141, 142, and 143 of the
proposal have been submitted in confidence and contain trade secrets and/or privileged or
confidential information and such data shall only be disclosed for evaluation purposes, provided
that if a contract is awarded to this Proposer as a result of or in connection with the submission
of this proposal, the State of Louisiana shall have the right to use or disclose the data therein to
the extent provided in the contract. This restriction does not limit the State of Louisiana’s right
to use or disclose data obtained from any source, including the Proposer, without restrictions.”
Presented for your consideration by:
One CVS Drive
Woonsocket, Rhode Island 02895
Caremark.com
Proposal for
Integrated Pharmacy
Benefit Management
Services

Louisiana Medicaid Page 2
© 2022 Caremark. All Rights Reserved.
LOUISIANA MEDICAID
MARCH 2022
Section I Cover Letter
Section II Executive Summary
Section III Technical Proposal
Section IV Cost Proposal
Section V CVS Health Exhibits
Tab 1 CVS Health 2019 10-K
Tab 2 CVS Health 2020 10-K
Tab 3 Sample Implementation Timeline
Tab 4 CVS Health’s Business Continuity Plan
Tab 5 CVS Health’s List of Diverse Suppliers
Tab 6 Certification Statement
Tab 7 Officer’s Certificate of Authority
Tab 8 Certificate of Good Standing
Tab 9 Louisiana Secretary of State Certificate of Authority
Tab 10 Pricing Commitment Document
Tab 11 Limited Distribution Drugs With Access
Tab 12 Limited Distribution Drugs Without Access

Louisiana Medicaid Page 3
© 2022 Caremark. All Rights Reserved.
Germaine Becks-Moody March 30, 2022
Louisiana Department of Health
Medical Vendor Administration
P.O. Box 91030 Bin # 24
Baton Rouge, LA 70821-9030
Dear Germaine,
On behalf of CVS Health, I am pleased to present this proposal for pharmacy benefit management (PBM)
services to Louisiana Medicaid. Following your requested format, our proposal details the unique and
comprehensive services CVS Health can offer to help you achieve your goals.
This includes:
• A pharmacy benefits management (PBM) experience aligned to your commitments
• Smarter ways to control your costs
• Reduced spend and improved care for members with high-cost conditions
• Value beyond a traditional pharmacy benefits manager.
We look forward to the opportunity to discussing how we can be the best choice for the single Pharmacy Benefit
Manager for Louisiana’s Managed Care Organizations and their enrollees. If you have any questions or need
further information, please contact me at Michael.Jaeger@CVSHealth.com or call me at 469-524-7211. Thank
you for your consideration. We would be extremely pleased to enter into an agreement to provide pharmacy
benefit services to the five Managed Care Organizations in Louisiana.
Best regards,
Michael Jaeger
Director, Strategic Sales, CVS Health

Louisiana Medicaid Page 4
© 2022 Caremark. All Rights Reserved.
∙ Summary information about the Proposer's organization.
CVS Health provides a best-in-class Medicaid pharmacy benefit manager. We currently support 27 managed
Medicaid health plans, of which three are currently in Louisiana, with 135 unique lines of business,
representing more than 27 million enrollees, of which nearly one million are in Louisiana, across 37 states.
These plans cover children, nondisabled adults, pregnant women, individuals with disabilities, and seniors
eligible for both Medicaid and Medicare benefits.
DIFFERENTIATORS
Improved clinical and cost outcomes are achieved through our sophisticated programs. Our Medicaid-specific
clinical programs are geared toward reducing fraud, waste, and abuse; improving quality; managing costs;
and improving outcomes. When state-mandated formularies or preferred drug lists are required, we work with
our clients to ensure compliance. We have robust specialty programs, and our member engagement outreach
efforts are designed to provide high-quality clinical care. Further, we ensure members have access to the
most cost-effective and clinically appropriate medication through retail, specialty, and mail channels.
Our knowledge and expertise in managed Medicaid allow us to improve the per member per month (PMPM)
performance and operational efficiency of our managed Medicaid clients. We know plans are most successful
managing costs and meeting requirements when they have access to Medicaid experts who are dedicated to
helping them reach their goals. The clinical, account, and analytics experts in our managed Medicaid segment
provide detailed, consultative support to help our clients manage the complexities of their business.
• Encounter processing: We currently support Medicaid encounter submissions in 30 states. We maintain a
proprietary encounter processing system (EMS) that interfaces with our claims adjudication engine to extract
all adjudicated claims nightly. EMS prepares NCPDP encounter file transactions for submission to states in
the required formats.
• Formulary management: From closed formularies to therapeutic interchange programs, we have the
management expertise to develop the most appropriate level of formulary management. We developed a
Medicaid-specific formulary template to provide appropriate clinical and cost-effective formulary management
for managed Medicaid coverage providers.
• Fraud, waste, and abuse: We use comprehensive tools proven to solve fraud and abuse to effectively
control costs in relevant areas of a Medicaid environment.
• HEDIS scores: Through our comprehensive clinical solutions, we proactively engage members and their
prescribers with evidence-based clinical health improvement opportunities that support your efforts to meet or
exceed various HEDIS measures.
• NCQA accreditation: We support NCQA member connection standard MEM-4 by providing members the
information they need to understand and use their pharmacy benefits. This information is provided through
our website, Caremark.com, and over the phone.
• Network management: We offer multiple retail network options—including national, limited, and custom—to
provide optimal geographic coverage while allowing clients to manage their retail pharmacy spending. We will
develop a network with you that meets geo access requirements. We have successfully implemented
preferred network strategies in multiple states for our managed Medicaid clients.

Louisiana Medicaid Page 5
© 2022 Caremark. All Rights Reserved.
• PMPM performance: Our dedicated account teams provide ongoing analysis and consultation for a variety of
issues, including management of PMPM performance to meet client goals during challenging budgetary
times. We designed our PMPM trend forecasting tool specifically for health plan support, given the need to
evaluate opportunities at the therapeutic class level.
• Specialty medication management: Our specialty management capabilities address drug spending under
the pharmacy and medical benefits. We are the only specialty pharmacy that integrates rare disease
management—which is critical to controlling overall costs related to this small but high-cost population.
• State requirements: We maintain a dedicated Medicaid regulatory compliance support team that meets with
client staff to discuss the regulations and Medicaid requirements in a state with regard to PBM operations.
They review new requirements to advise clients on the impact of our operations and proactively identify new
and proposed requirements and communicate them to clients.
• Utilization management: We create Medicaid-specific criteria for prior authorization, step therapy, and
quantity limit programs to control high utilization, abuse, and access to high-cost drugs. We also provide
exception processing and member-level overrides, upon request.
∙ Location of Central Administrative Office with Full Time Personnel, including the address for all
office locations with full time personnel.
The following is a list of offices, locations, and primary functions of CVS Health and our prescription benefit
management affiliates:
Office
Function
Addresses
CVS Health
CVS Health Headquarters
One CVS Drive
Woonsocket, Rhode Island 02895
CVS Health
PBM Operations Centers
9501 E. Shea Boulevard
Scottsdale, Arizona 85260
750 West John Carpenter Freeway
Suite 1200
Irving, Texas 75039
CVS Caremark Medicare Part D
Medicare Part D Operations
Centers
9501 E. Shea Boulevard
Scottsdale, Arizona 85260
CVS Health
Data Services
Scottsdale Data Center
9501 E. Shea Boulevard.
Scottsdale, Arizona 85260
Back-up Site
One CVS Drive
Woonsocket, Rhode Island 02895
CVS Health Customer Care
Customer Care Facilities
800 NW Chipman Road, Suite 5830
Lee’s Summit, Missouri 64063

Louisiana Medicaid Page 6
© 2022 Caremark. All Rights Reserved.
6950 Alamo Downs Parkway
San Antonio, Texas 78238
2401 Cherahala Boulevard
Knoxville, Tennessee 37932
600 Penn Center Boulevard
Pittsburgh, Pennsylvania 15235
2700 W. Frye Road
Chandler, Arizona 85224
29300 Aurora Road
Solon, OH 44139
1451 Center Crossing Road
Las Vegas, NV 89144
CVS Health Mail Service
Program
Mail Service Pharmacies
Regional Order Creation Centers
(ROCCs)
620 Epsilon Drive
Pittsburg, Pennsylvania 15238-2808
1400 Business Center Drive
Mt. Prospect, Illinois 60056 - 6071
6935 Alamo Downs Parkway
San Antonio, Texas 78238 - 4501
Prescription Processing (Frontend)
Centers
Number 1 Great Valley Boulevard
Wilkes-Barre, Pennsylvania 18702
620 Epsilon Drive
Pittsburgh, PA 15238
7034 Alamo Downs Parkway
San Antonio, TX 78238
4121 E. Cotton Center Boulevard
Phoenix, AZ 85040
800 Biermann Court
Mount Prospect, IL 60056
10302 West Emerald Street
Boise, ID 83704
Dispensing Pharmacies
1780 Wall Street
Mount Prospect, Illinois 60056

Louisiana Medicaid Page 7
© 2022 Caremark. All Rights Reserved.
Number 1 Great Valley Boulevard
Wilkes-Barre, Pennsylvania 18702
Consumer Health Interactive
Consumer Website Developer
539 Bryant Street, Suite 200
San Francisco, California 94107
CVS Health specialty
Specialty Pharmacies
2700 West Frye Road
Chandler, Arizona 85224
9310 Southpark Center Loop
Orlando, Florida 32819
CVS Health Specialty Pharmacy
CareTeam - Accordant
4900 Koger Boulevard, Suite 100
Greensboro, North Carolina 27407-2710
CVS Health
Government Affairs
1300 I Street NW, Suite 525 West
Washington, District of Columbia 20005
∙ Name and address of principal officer.
CAREMARKPCS, L.L.C.
Following is the list of principal officers of CaremarkPCS, L.L.C.:
• John M. Conroy (President and Treasurer)
• Thomas S. Mofatt (Vice President and Secretary)
• Cheryl Baliey (Vice President)
• Melanie K. St Angelo (Assistant Secretary).
Note: Because it is a limited liability company, CaremarkPCS, L.L.C. does not have directors. The L.L.C. is managed by its sole member,
Caremark Rx, L.L.C.
∙ Name and address for purpose of issuing checks and/or drafts.
CVS Caremark
PO Box 848001
Dallas, TX 75284-8001
∙ For corporations, a statement listing name(s) and address(es) of principal owners who hold five
percent (5%) interest or more in the corporation.
The shareholder(s) that own 5% or more of the common stock of CVS Health Corporation include:
• The Vanguard Group, Inc. (8.1%)
Louisiana Medicaid Page 8
© 2022 Caremark. All Rights Reserved.
∙ If out-of-State Proposer, give name and address of local representative; if none, so state.
CT Corporation System
3867 Plaza Tower Dr.
Baton Rouge, LA, 70816-4378
∙ If the Proposer was engaged by LDH within the past twenty-four (24) months, indicate the
contract number and/or any other information available to identify the engagement; (if none, so
state).
Not Applicable.
∙ Proposer's state and Federal tax identification numbers.
Business Entity
Federal Tax ID #
CaremarkPCS Health, L.L.C.
75-2882129

Louisiana Medicaid Page 9
© 2022 Caremark. All Rights Reserved.
The cover letter should include a positive statement of compliance with the contract terms
defined herein. If the Proposer cannot comply with any of the contract terms, an explanation of
each exception should be supplied. The Proposer should indicate the specific section and
language in the RFP and submit exceptions or exact contract modifications that it may seek.
CVS Health confirms we can comply with the contract terms defined within the RFP unless otherwise stated
below:
Section
Language
Exception
Addendum 5 –
Section 5
Addendum 5 –
Section 12
Section 1.38
Record
Ownership
5. Record Ownership: All records, reports, documents, and
other material delivered or transmitted to Contractor by the
Department shall remain the property of the Department,
and shall be returned by Contractor to the Department, at
Contractor's expense, at termination or expiration of this
contract. All records, reports, documents, or other material
related to this Contract and/or obtained or prepared by
Contractor in connection with the performance of the
services contracted for herein shall become the property of
the Department, and shall, upon request, be returned by
Contractor to the Department, at Contractor's expense, at
termination or expiration of this contract.
12. Ownership of Proprietary Data: All non-third party
software and source code, records, reports, documents,
and other material delivered or transmitted to Contractor by
the State shall remain the property of the State, and shall
be returned by Contractor to the State, at Contractor's
expense, at termination or expiration of this contract. All
non-third party software and source code, records, reports,
documents, or other material related to this Contract and/or
obtained or prepared by Contractor in connection with the
performance of the services contracted for herein shall
become the property of the State, and shall be returned by
Contractor to the State, at Contractor's expense, at
termination or expiration of this contract.
1.38 Record Ownership
All records, reports, documents, or other material related to
any contract resulting from this RFP and/or obtained or
prepared by the Contractor in connection with the
performance of the services contracted for herein shall
become the property of the Department and shall, upon
request, be returned by the Contractor to the Department,
at the Contractor’s expense, at termination or expiration of
the contract.
CVS Health confirms with the exception of
any Contractor confidential information that
may be contained within them.
Addendum 5 –
Section 13
Section 1.22
Use of
Subcontractors
13. Subcontracting: Contractor shall not enter into any
subcontract for work or services contemplated under this
Contract without obtaining prior written approval of the
Department. Any subcontracts approved by the
Department shall be subject to conditions and provisions as
the Department may deem necessary; provided, however,
that notwithstanding the foregoing, unless otherwise
CVS Health confirms with the exception
that if LDH requires written approval of
subcontractors, there could be a cost
associated with holding permission.

Louisiana Medicaid Page 10
© 2022 Caremark. All Rights Reserved.
provided in this contract, such prior written approval shall
not be required for the purchase by Contractor of items and
services that are incidental but necessary for the
performance of the work required under this contract.
1.22 Use of Subcontractors
Unless provided for in the Contract, the prime Contractor
shall not contract with any other party for any of the
services herein contracted without the express prior written
approval of the State.
Addendum 5 –
Section 21
Section 1.32
Liability and
Indemnification
21. Indemnity: Contractor agrees to protect, indemnify, and
hold harmless the State of Louisiana and the Department
from all claims for damages, costs, expenses, and attorney
fees arising in Contract or tort from this Contract or from
any acts or omissions of Contractor's agents,
subcontractors, employees, officers, or clients, including,
but not limited to, premises liability and any claim based on
any theory of strict liability. This provision does not apply to
actions or omissions for which La. R.S. 40:1237.1, et seq.
provides malpractice coverage to Contractor, nor claims
related to treatment and performance of evaluations of
persons when such persons cause harm to third parties
(La. R.S. 13:5108.1(E)). Further, it does not apply to
premises liability when the services are being performed on
premises owned and operated by the Department.
We agree to indemnify and defend LDH
from any and all claims or losses that you
incur to the extent the claims or losses are
due to CVS Health negligence or breach of
our obligations or warranties as described
in the Prescription Benefit Management
Agreement. Our obligation to indemnify
you will be limited to the extent any claim or
loss is due to your negligence or actions.
We expect LDH to indemnify CVS Health
based on similar terms and will provide
contract language to reflect this
commitment.
Addendum 5 –
Section 42
42. Contractor must comply with the Office of Technology
Services (OTS) Information Security Policy,
https://www.doa.la.gov/Pages/ots/InformationSecurity.aspx.
b. Contractor must follow OTS Information Security Policy
for Data Sanitization requirements for any equipment
replaced during the Contract and at the end of the contract,
for all equipment which house confidential/restricted data
provided by the State.
d. If Contractor will have access to data originating from the
Centers for Medicare and Medicaid Services (CMS), then
Contractor must ensure their computer system is in
compliance with CMS latest version of the Minimum
Acceptable Risk Standards for Exchanges (MARS-E)
Document Suite, currently MARS-E 2.0. The CMS MARS-E
2.0 requirements include but are not limited to the below
listed requirements:
- Multi-factor authentication is a CMS requirement
for all remote users, privileged accounts and non-
privileged accounts. In this context, a “remote
user” is referencing staff accessing the network
from offsite, normally with a client virtual private
network with the ability to access CMS data.
- Perform criminal history check for all staff prior to
granting access to CMS data. All employees and
contractors requiring access to Patient Protection
CVS complies with its own Information
Security Policies and Control Standards
which are aligned with NIST, HIPAA, PCI-
DSS and CIS Benchmarks and comply with
legal and regulatory requirements.
CVS Complies with our own data
sanitization requirements which are
compliant with NIST-800-88.
We comply with the MFA requirement for
all remote users and privileged accounts.
We do not require Multi-factor
authentication for non-privileged accounts
that are not remote users.
We do not conduct reference checks as
part of our background checks. However,
we do conduct a criminal check.

Louisiana Medicaid Page 11
© 2022 Caremark. All Rights Reserved.
and Affordable Care Act (PL 111-148) sensitive
information must meet personnel suitability
standards. These suitability standards are based
on a valid need-to-know, which cannot be
assumed from position or title, and favorable
results from a background check. The background
checks for prospective and existing employees (if
not previously completed) should include, at a
minimum, contacting references provided by the
employee as well as the local law enforcement
agency or agencies.
1.8.10
Proposed Staff
Qualifications
Include full resumes of all proposed key personnel
identified for key roles. Each person identified for a role
above should be included in the resume section. Each
resume should demonstrate the qualifications and
experience relevant to the position proposed. Each resume
should include work history, the specific functions
performed, and how the experience relates to the assigned
role. Résumés of all known personnel working or
overseeing the LDH Pharmacy Program should be
included. Résumés of proposed personnel should include,
but not be limited to:
• Experience with Proposer.
• Previous experience in projects of similar scope
and size.
• Educational background, certifications, licenses,
special skills, etc.
Provide three (3) references for each proposed Key
Personnel candidate demonstrating experience in a similar
role on one or more projects similar to Section 2. Scope of
Work requirements. Each reference should include:
• Name of the person to be contacted.
• Contact phone number.
• Client name and address.
• Brief description of work.
• Dates (month and year) of employment.
These references should be able to attest to the
candidate’s specific qualifications.
CVS Health agrees in concept with the
staffing requirements as noted in the RFP.
At present we are not including names and
resumes. Given the highly competitive
nature of this procurement and the
Louisiana state-based requirement, the
hiring pool may be greatly reduced. Once
the award is announced bidders will have
an opportunity to assemble a team with the
best talent. As we work closely with the
state during subsequent stages of the
project and begin to better understand in
full scope the needed resources to fully
align objectives we will add individuals with
mutually agreeable backgrounds and
experience to ensure the business
outcomes are delivered.
1.30.1
Contractor’s
Insurance
If so requested, the Contractor shall also submit copies of
insurance policies for inspection and approval of the
Department before work is commenced.
CVS Health confirm with the exception that
policies are deemed to be proprietary and
therefore complete copies are not shared
externally.
1.30.2.2
Commercial
General
Liability
The Contractor shall maintain during the life of the contract
such Commercial General Liability Insurance which shall
protect Contractor, the Department, and any Subcontractor
during the performance of work covered by the contract
from claims or damages for personal injury, including
accidental death, as well as for claims for property
damages, which may arise from operations under the
CVS Health confirms with the exception
that subcontractors are not coved by our
CGL policy. We maintain Commercial
General Liability insurance with policy limits
of $4,500,000 per occurrence, $28,000,000
general aggregate. This policy is in excess
of a $500,000 self-insured retention. The

Louisiana Medicaid Page 12
© 2022 Caremark. All Rights Reserved.
contract, whether such operations be by the Contractor or
by a Subcontractor, or by anyone directly or indirectly
employed by either of them, or in such a manner as to
impose liability to the Department.
insurance carrier is ACE American
Insurance Company with policy effective
dates of January 1, 2022 through January
1, 2023. We maintain an Umbrella Liability
policy which provides coverage in excess
of $50,000,000. Subcontractors are not
covered by our Commercial General
Liability policy.
1.30.4.3 All
Coverage
All policies must be endorsed to require thirty (30) Calendar
Days written notice of cancellation to the Agency.
CVS Health confirms with the
understanding that our policies provide
notice to the named insured only. Our
insurance carriers are unable to endorse
each customer.
1.30.6
Verification of
Coverage
In addition to the Certificates, Contractor shall submit the
declarations page and the cancellation provision for each
insurance policy. The Agency reserves the right to request
complete certified copies of all required insurance policies
at any time.
CVS Health confirms with the exception
that policies are deemed to be proprietary
and therefore complete copies are not
shared externally.
2.1.8.1General
Requirements
The Contractor shall:
• Capture recoveries from other state or Federal
entities or third-party payers.
CVS Health does not confirm. We do not
provide any recoveries from State, federal,
or third-party payers.
Please refer to Section 1.86 of the
Technical Proposal for details on our
TPL/Subrogation capabilities.
2.1.9.1
General Drug
Claim
Adjudication
System
Requirements.
The Contractor’s Drug Claim Adjudication system shall:
• Comply with the latest version of the W3C Mobile Web
Application Best Practices for browser-based
components.
• Comply with the current Authoring Tool Accessibility
Guidelines (ATAG) as published by the Worldwide
Web Consortium (W3C).
CVS Health strives to comply with the
latest version of WCAG (2.1 currently) and
A/AA conformance levels. To that end, we
have an enterprise-wide policy which
establishes our organizational
standards and expectations for digital
accessibility. In addition, CVS Health has a
digital accessibility team dedicated to
empowering product teams to build
accessible products and support assets
that may require a remediation roadmap.
2.1.9.2
General Drug
Claim
Processing
Requirements.
• Process and reimburse Drug Claims without
inappropriate denials, delays, or recoupments.
• If the Contractor has a pattern, as determined by
the MCO, of inappropriately denying, delaying or
recouping Provider payments for services, the
Contractor may be subject to Monetary Penalties
equal to one and one-half (1.5) times the value of
the Drug Claims inappropriately denied, delayed,
or recouped, contract cancellation, or refusal to
contract in a future time period.
CVS Health confirms with the exceptions
that the criteria inappropriately deny,
delaying or recouping provider payments
shall be mutually determined prior to the
contract effective date.

Louisiana Medicaid Page 13
© 2022 Caremark. All Rights Reserved.
• If the Contractor has a pattern, as determined by
the MCO, of inappropriately denying, delaying, or
recouping Provider payments for services after
the termination of the Contract, the Contractor
may be subject Monetary Penalties equal to one
and one-half (1.5) times the value of the Drug
Claims inappropriately denied, delayed, or
recouped.
2.1.9.3
Drug Claims
Systems
Requirements
• Correct each deficiency by an effective date to be
determined by LDH.
CVS Health confirms with the exception
that deficiencies will be corrected by an
agreed upon date.
2.1.9.4
Information
Systems
Availability
• Notify designated LDH staff via phone and
electronic mail within fifteen (15) minutes of
discovery of a problem that results in delays in
report distribution or problems in online access to
critical systems functions and information, in order
for the applicable work activities to be rescheduled
or handled based on system unavailability
protocol.
CVS Health does not confirm. We can
notify LDH staff with 24 hours of discovery
of a problem.
2.1.9.4
Information
Systems
Availability
• Resolve and implement system restoration within
sixty (60) minutes of official declaration of
unscheduled system unavailability of critical
functions caused by the failure of system and
telecommunications technologies within the
Contractor’s span of control. Unscheduled system
unavailability to all other system functions caused
by system and telecommunications technologies
within the Contractor’s span of control shall be
resolved, and the restoration of services
implemented, within eight (8) hours of the official
declaration of system unavailability.
CVS Health does not confirm. Our standard
target restoration time for Priority 1 Events
is 3 hours.
2.1.9.13
Utilization
Management
• Provide the capability to produce an extract file of
procedure code drug pricing to be shared and
utilized by other stakeholders processing Drug
Claims for Provider administered pharmaceuticals
upon implementation by LDH.
CVS Health does not adjudicate claims
based on procedure codes. However, we
will share the pricing details of all claims
processed.
2.1.9.17 Third
Party Liability
• Verify and update its system within four (4) Business
Hours of receipt of an update request, if an Enrollee is
unable to access PBM Covered Services until the
update is made. This includes updates on coverage,
including removal of coverage that existed prior to the
Enrollee’s linkage to the MCO that impacts
Adjudication or Enrollee access to PBM Covered
Services.
CVS Health does not confirm. We will verify
and update the systems in a mutually
agreed upon timeframe.
2.1.9.17.2
Post-Payment
Recoveries
If TPL is identified after a Drug Claim has been
Adjudicated, the Contractor shall:
CVS Health does not confirm. Please refer
to Section 1.86 for our TPL/Subrogation
capabilities.

Louisiana Medicaid Page 14
© 2022 Caremark. All Rights Reserved.
2.1.9.17.3 LDH
Right to
Conduct
Identification
and Pursuit of
TPL
• Initiate recovery of reimbursement within sixty (60)
Calendar Days after the end of the calendar month in
which the TPL is identified.
• Not perform post-payment recovery for TPL from
Providers for Drug Claims with dates of service (DOS)
older than ten (10) months, except when the liable
third party is traditional Medicare, Tricare, or
CHAMPUS.
• Recover from the Provider if the liable third party is
traditional Medicare, Tricare or CHAMPUS, and more
than ten (10) months have passed since the DOS.
• Allow Providers sixty (60) Calendar Days from the
date stamp of the recovery letter to refute the recovery
with a one-time thirty (30) Calendar Day extension at
the Provider’s request.
• Refer pay and chase Drug Claims directly to the liable
third parties.
• Refer Point of Sale (POS) Drug Claims directly to the
carrier.
• Initiate an automatic recoupment at the expiration of
the sixty (60) Calendar Day time period if an extension
request is not received from the Network Provider and
at the expiration of the ninety (90) Calendar Day time
period if an extension is requested by the Network
Provider if the Network Provider has not remitted the
payment to the Contractor.
• Identify and track potential TPL recoveries. The
system shall produce reports indicating open
receivables, closed receivables, amounts collected,
amounts written off, and amounts avoided. These
reports shall be made available to LDH upon request.
• Identify the existence of potential TPL to pay for PBM
Covered Services through the use of trauma code
edits in accordance with 42 CFR §433.138(e).
• Seek reimbursement in accident/trauma related cases
when Drug Claims in the aggregate equal or exceed
five hundred dollars ($500.00) as required by the State
Plan and Federal Medicaid guidelines and may seek
reimbursement when Drug Claims in the aggregate
are less than five hundred dollars ($500.00). Failure to
seek reimbursement may result in Monetary Penalties
as specified in Attachment G, Table of Monetary
Penalties.
• Notify LDH when subpoenas duces tecum are
received and report the resulting recoveries to LDH.
• The amount of any recoveries collected by the
Contractor outside of the Drug Claims processing
system shall be treated by the Contractor as offsets to
medical expenses for the purposes of reporting.
• Obtain written approval from LDH prior to accepting a
TPL settlement on accident/trauma-related Drug
Claims equal to or greater than twenty-five thousand
dollars ($25,000.00).
• Upon receipt of a subpoena duces tecum, the
Contractor shall produce documents responsive to
said subpoena by the date of return indicated therein
(or shall contact the party who caused issuance of the
subpoena, in order to request additional time to

Louisiana Medicaid Page 15
© 2022 Caremark. All Rights Reserved.
respond) if the production is authorized under La. R.S.
13:3715.1. Upon receipt of a request for records not
sent via subpoena, the Contractor shall release PHI or
a response explaining why PHI cannot be released to
the individual or entity making the request, within
fifteen (15) Calendar Days of receipt of the request
and a written authorization, as set forth in La. R.S.
40:1165.1(A)(2)(c). The Contractor is solely
responsible for any sanctions and costs imposed by a
court of competent jurisdiction for failure to comply
with the requirements of La. R.S. 40:1165.1(A)(2)(c) or
for failure to respond Timely to a subpoena duces
tecum. Additionally, LDH may impose sanctions
against the Contractor for failure to properly or Timely
respond to requests for PHI.
• All records requests received by the Contractor shall
be investigated by the Contractor (or its vendor) for
possible TPL recoveries, resulting in issuance of a lien
statement (or notice of lack thereof) to the requesting
party, as provided for in La. R.S. 46:446.
• When the Contractor has actual knowledge that an
insurer or other risk bearing entity of an Enrollee has
filed for bankruptcy and the Network Provider files a
Drug Claim for reimbursement with the Contractor with
dates of service prior to the date the insurer or other
risk bearing entity filed bankruptcy, the Contractor
shall reimburse the Network Provider with the
Louisiana Medicaid Program as the primary insurer
only if the Enrollee was enrolled with the Contractor at
the time the service was provided and the Network
Provider has not been paid. The Contractor shall seek
reimbursement as a creditor in the bankruptcy
proceeding or from a liable third party. If the Network
Provider files a Drug Claim for reimbursement with the
Contractor with dates of service after the date the
insurer or other risk bearing entity filed for Chapter 11
bankruptcy, the insurer or other risk bearing entity
shall continue to be the primary insurer. If the Network
Provider files a Drug Claim for reimbursement with the
Contractor with dates of service after the date the
insurer or other risk bearing entity filed for Chapter 7
bankruptcy, the Louisiana Medicaid Program shall be
the primary insurer.
• Transfer one hundred percent (100%) of its TPL
recoveries to the appropriate MCO.
• Void encounters for Drug Claims for which the full
Louisiana Medicaid Program paid amount is being
recouped. For recoupments for which the full
Louisiana Medicaid Program paid amount is not being
recouped, the Contractor shall submit adjusted
encounters for the Drug Claims.
• Provide TPL information to the MCO in a format and
medium described in the MCO Manual and shall
cooperate in any manner necessary, as requested by
the MCO, with the MCO and/or its designee.
LDH Right to Conduct Identification and Pursuit of TPL

Louisiana Medicaid Page 16
© 2022 Caremark. All Rights Reserved.
LDH may invoke the Contractor’s right to pursue TPL
recoveries if the Contractor fails to recover reimbursement
from the liable third party to the limit of legal liability within
three hundred sixty-five (365) Calendar Days from date(s)
of service of the Drug Claim(s).
If the MCO determines that the Contractor is not actively
engaged in cost avoidance activities, the Contractor may
be subject to Monetary Penalties as set forth in Attachment
V, Table of Monetary Penalties.
2.1.14.1
Customer
Service Center
(CSC)
• Locate its primary CSC site in the State.
CVS Health confirms with the exception
that our customer care representatives will
be located in Louisiana but will work
virtually to support LDH. There will be no
physical call center located in Louisiana.
2.1.14.1
Customer
Service Center
(CSC)
• Handle emergent Provider issues twenty‐four (24)
hours per day, seven (7) days per week.
CVS Health does not confirm. Our Provider
Help Desk is open Monday through Friday
from 8 AM to 5:30 PM.
Attachment V:
Monetary
Penalties
Employment of Key Personnel: One thousand dollars
($1,000) per Calendar Day per key personnel position for
failure to have an individual serving in a full‐time acting or
permanent capacity in any key personnel position for more
than two (2) consecutive Calendar Days, for each Calendar
Day the key personnel has not been appointed.
CONFIDENTIAL
Attachment V:
Monetary
Penalties
Additional Personnel Requirements: One thousand dollars
($1,000) per appropriate staff person per meeting or event
for failure to provide subject appropriate staff member(s) to
attend a meeting or event when required.
One thousand dollars ($1,000) per appropriate staff person
per meeting or event for failure to attend a meeting or event
in person when required by the Contract or requested by
LDH.
CONFIDENTIAL
Attachment V:
Monetary
Penalties
Covered Outpatient Drugs: The actual cost incurred by an
Enrollee for obtaining Covered Outpatient Drugs from a
non-Medicaid source, as authorized by LDH, due to failure
of the Contractor to provide the service.
CONFIDENTIAL
Attachment V:
Monetary
Penalties
Enrollee Help Desk:
Five thousand dollars ($5,000) per Calendar Day for failure
to provide appropriate staff to answer calls from Enrollees
from 7:00 a.m. to 7:00 p.m. Central Time, Monday through
Friday.
Five thousand dollars ($5,000) per Calendar Day for failure
to provide a voice message system to receive calls outside
CONFIDENTIAL

Louisiana Medicaid Page 17
© 2022 Caremark. All Rights Reserved.
of 7:00 a.m. to 7:00 p.m. Central Time, Monday through
Friday.
Five thousand dollars ($5,000) for each thirty (30) second
time increment, or portion thereof, by which the daily
average hold time exceeds the maximum acceptable hold
time.
Five thousand dollars ($5,000) for each percentage point
for each standard that fails to meet the requirements for a
monthly reporting period.
Attachment V:
Monetary
Penalties
Drug Claims Data: Ten thousand dollars ($10,000) per
Calendar Day for failure to submit accurate and complete
Drug Claims data to the MCO.
In addition to the above, a quarterly offset equal to the
value of the rebate assessed on the disputed encounters
may be deducted from the Contractor.
CONFIDENTIAL
Attachment V:
Monetary
Penalties
Information Systems Availability
Fifteen thousand dollars ($15,000) per Calendar Day per
core eligibility and Claim’s processing system that is not
restored within seventy‐two (72) hours of declared disaster.
One thousand dollars ($1,000) per hour for failure to
restore system functions within the Contractor’s span of
control beyond the time limits provided in the Contract.
CONFIDENTIAL

Louisiana Medicaid Page 18
© 2022 Caremark. All Rights Reserved.
Attachment V:
Monetary
Penalties
CONFIDENTIAL

Louisiana Medicaid Page 19
© 2022 Caremark. All Rights Reserved.
CONFIDENTIAL

Louisiana Medicaid Page 20
© 2022 Caremark. All Rights Reserved.
With deep experience dating starting in 1969, CVS Health began the industry that came to be known as
pharmacy benefit management by creating more efficient and economical ways for members to receive
prescriptions. To keep pace with a rapidly changing health care market, we have evolved beyond the original
business of claims processing and administrative services to include new areas of health management and health
care information technology, as well as becoming deeply experienced in the Medicaid market.
We are URAC-accredited and have supported managed Medicaid clients since 1988. We currently support 27
managed Medicaid health plans, of which three are currently in Louisiana, with 135 unique lines of
business, representing more than 27 million Enrollees, of which nearly one million are in Louisiana,
across 37 states. Our Medicaid health plans cover children, nondisabled adults, pregnant women, individuals
with disabilities, and seniors eligible for both Medicaid and Medicare benefits. We’re always evolving to meet
changes in Medicaid program designs and regulations.
Prepared for Louisiana Department of Health | March 30, 2022
CVS Health will bring the Louisiana Department of Health best in class programs and
services:
• Unparalleled current experience providing pharmacy benefit management services in Louisiana
• Point of service claim adjudication system. CVS Health owns the source code to the system, RxClaim,
which enables us to make changes to the software based on client needs.
• Best in class technology and analytics to ensure drug dispensing accuracy and safety
• Guaranteed transparency to reduce costs and increase accountability
• Commitment to reducing opioid misuse in Louisiana
• Providing clinical programs that improve health outcomes
• Seamless transition and implementation
• Key personnel located in Louisiana and other dedicated resources

Louisiana Medicaid Page 21
© 2022 Caremark. All Rights Reserved.
Given we cover over half of managed Medicaid enrollees across the country, we recognize and understand their
unique needs. Many Medicaid enrollees have multiple co-occurring chronic conditions requiring complex drug
regimens. The top drug classes used by Medicaid enrollees demonstrate the chronic physical and mental health
conditions our enrollees have: antivirals, antiasthmatics, antipsychotics, antidiabetics, antidepressants,
anticonvulsants, analgesics, and antihyperlipidemics. To address the complex, need of the Medicaid population,
we have tailored our programs and services to meet our enrollees’ needs
Unparalleled current experience providing pharmacy benefit management services in
Louisiana
LDH will not have a more qualified respondent to the Single PBM request for proposals. As of the date of our
submission, more than 50% of Louisiana’s managed Medicaid enrollees who are enrolled in managed
Medicaid are being serviced on CVS Health’s systems through the three Managed Care Organizations we
support; Aetna Better Health Louisiana, Healthy Blue Louisiana (Anthem, Inc.) and Louisiana Healthcare
Solutions (Centene Corp.). This means that there will be minimum Enrollee and MCO disruption when the state
transitions to the Single PBM. CVS Health has experience working with state Medicaid agencies to implement
uniform preferred drug lists (PDLs), uniform clinical criteria, administrative edits, formulary grandfathering/prior
use exceptions, and National Average Drug Acquisition Cost (NADAC) plus FFS dispensing fee pricing with
lesser of methodologies. Because of this experience, we are well-placed to assume the contract with LDH and
continue to serve Louisiana’s Medicaid managed care organization (MCOs).
• Enrollees prior authorizations and medications for 50% of enrollees will seamlessly transfer, resulting in
full continuity of care. The initial implementation accuracy for go-live is at 100%. The maintenance of
business plan changes accuracy is at 99%.
• Because the CVS Health’s pharmacy network includes all of LDH’s pharmacies, no enrollee will have to
change pharmacies.

Louisiana Medicaid Page 22
© 2022 Caremark. All Rights Reserved.
• Our existing Medicaid clients in Louisianaalready follow the LDH preferred drug list (PDL) and we will be
able to quickly code and test the PDL,for the two additional plans
• Communications and data exchanges between three of the five MCOs and LDH will remain in place,
which will mean a more efficient implementation and less effort for LDH and MCOs.
• CVS Health completed approximately 194,000 prior authorizations for delegated services for the Medicaid
population.
As the PBM for three of the current five MCOs, we are experts in LDH’s policies, programs, and regulations. We
have developed Louisiana specific policies and regulations to address transparent pricing, maximum allowable
cost (MAC) requirements, and pharmacy network audit requirements among others.
Guaranteed transparency to reduce costs and increase accountability
CVS Health currently complies with Louisiana statutory requirements for pharmacy pricing for both local and chain
pharmacies. We will provide LDH with real-time and unredacted access to our claims adjudication engine,
RxClaim. With this access, LDH will be able to view and audit our claims adjudication to ensure we do not pay
the pharmacies amounts that are different from the LDH-established pricing methodology, including the LDH MAC
list and related pricing.
When we implement changes to the PDL or benefit design, LDH will have unfettered access to our pre-production
testing environment to develop testing scenarios. This will allow LDH to provide test scenarios and have a higher
level of comfort with 100% accuracy prior to moving the coding to production.
Best in class technology and analytics to ensure benefit set up accuracy, drug
dispensing and accuracy and safety it
CVS Health continually invests in technology to improve our performance and to provide our clients increased
accuracy in benefit set up, near real-time review of claims to identify drug utilization anomalies not caught at the
point of sale, and aberrant claims that may require auditing.
We use sophisticated algorithms and real-time claims surveillance to automatically identify benefits administration
issues. These rule-based and machine-learning algorithms detect potential issues with benefit coding during near
real-time claims adjudication. Our claims surveillance process runs multiple times a day. Because of the near
real-time reporting, we are able to conduct rapid response reviews of aberrant claims adjudication.
Our Drug Savings Review program provides a thorough review of a enrollee’s medication profile within 72 hours
after claim adjudication. When combined with our ongoing review of the enrollee’s prescription history, it helps us
identify those who might be at risk for drug interactions or drug-induced disease conditions, regardless of the
point of service. This can result in identification of opportunities to help reduce unnecessary prescriptions and
streamline enrollee therapy.
Our Pharmacy Performance Department believes that the best way to protect patient safety and the financial
resources of LDH is through rapid response desktop reviews. We developed a highly effective leading-edge
algorithm to review every claim submitted for reimbursement.
The algorithm contains a closely held set of rules that identifies claims that are potentially erroneous or unusual.
The claims flagged as erroneous undergo a secondary review by certified pharmacy technicians to spot claims in
need of correction. The claims are also flagged for the specific reason why the claim appears to be incorrect. If
the auditor feels there is an issue, they will call the pharmacy and review the claim over the phone.

Louisiana Medicaid Page 23
© 2022 Caremark. All Rights Reserved.
The rapid response process is invisible to the enrollee- only CVS Health and the Kentucky pharmacy know that
an error occurred on the claim, thereby preserving the Pharmacist-Patient bond. This reinforces the trust between
the pharmacist and patient, which is important to maintaining the pharmacist as a trusted member of the
enrollee’s health care team.
Commitment to reducing opioid misuse in Louisiana
CVS Health recognizes the importance of state Medicaid program efforts around drug safety and opioid misuse.
CVS Health will support conitue to support as it does today with it’s existing MCO client relationships in Lousiana,
the MCO compliance to the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment
for Patients and Communities (SUPPORT) Act. As a PBM one way we will help clients prevent opioid misuse and
abuse by implementing through our Prescription Safety Management Program (PSMP), which is a holistic
program to address opioids use and related drug safety. The SPMP is a single dynamic solution that can help
improve safety and utilization of prescribed controlled substances such as opioids, pain medications, and muscle
relaxants. Our PSMP consists of four pillars. This program can be tailored for LDH and MCOs needs. We
understand we will not implement this program without LDH approval and consistent with all LDH current opioid
review requirements.
Pillar 1 is integral helping LDH prevent opioid misuse and abuse for Medicaid enrollees. We use a combination of
prospective and retrospective drug utilization review edits to identify inappropriate prescriptions before they are
dispensed and within 72 hours post-dispensing.
• Point of sale safety messages. These safety alerts ensure that pharmacists are appropriately aware of
safety risks during dispensing. Safety messages help to reduce high dosage, and unsafe combinations.
Example safety messages related to Opioids are:
− Cumulative Morphine Milligram Equivalent Edit
− Buprenorphine/Opioid Edit
− Duplicate Long Acting Opioid Edit
Prescription
Safety
Management
Program
Prevention
Identification
Intervention
Investigation

Louisiana Medicaid Page 24
© 2022 Caremark. All Rights Reserved.
− Opioid/Benzodiazepine Edit
− Contains many of our CMS required edits for Medicare Part D enrollees
• Prior Authorizations/ UM – We also have a comprehensive set of utilization management edits, creating
“hard stops” to support prudent prescribing. These PA edits include:
− MME based quantity limits
− Post PA quantity limit durations
− Step therapy (e.g. IR before ER)
− Increased access to drugs to treat opioid use disorder (e.g. lifting PAs on buprenorphine/naloxone)
−
• Naïve therapy Opioids Days-Supply limits - We have instituted 7-day supply limits for adult new-to-therapy
enrollees, and also offer a 3-day supply limit for enrollees aged 19 and under.
− CMS Compliant with 7 Day initial opioid prescription for acute pain CMS Mandate for 2019 for opioid
naïve patients
• Retrospective Safety Review - Identifies opioid safety concerns for enrollees within 72 hours of adjudication
for medications and sends prescriber communication to prescriber. Examples of retrospective safety review
include:
− Neonatal Abstinence
− Opioid/Antipsychotic
Clinical programs that improve health outcomes
CVS Health will bring our Transform Care program which combines clinical expertise and data analytics to
enhance MCOs’ disease management strategies with targeted, comprehensive, plan enrollee support that bridges
the gap between their everyday lives and their physician’s office.
For example, our Transform Diabetes Care uses advanced analytics to assess enrollee pharmacy data, along
with biometric insights from a connected glucometer, to better understand their diabetes management and unique
needs. This enables our MCOs to develop personalized ‘interventions, delivered by health care professionals, to
help improve their medication management, blood glucose control, and condition management.
Our outcomes-based model focuses on improvements in blood glucose control, adherence and healthy
behaviors, while targeting an aggregate, one-point average decrease in A1C among the uncontrolled portion of a
diabetic population. Integrated systems enable collaboration between our program and providers, plans and
existing disease management programs to effectively extend the reach of the physician, support client goals and
align all points of care throughout enrollee therapy. This coordinated approach to diabetes management helps
drive the greatest improvements in care for enrollees with diabetes, while helping our clients better protect their
pharmacy investment.

Louisiana Medicaid Page 25
© 2022 Caremark. All Rights Reserved.
A seamless transition and implementation
Your dedicated implementation team will ensure a successful and timely transition for you and your members,
with our comprehensive approach. Over the past 10 years, CVS Health has built a track record of successfully
implementing new partnerships with our health plan clients. Our standardized processes and tools align
ownership and accountability for consistent results through a proven, stable, repeatable process with robust
testing that removes risk from transition to a new PBM. Our collaborative partnership leverages best practices that
help ensure our goals are aligned to your success.
To help ensure accuracy, we thoroughly test eligibility files in both the test and production environments during
the process of implementing a new client and benefit plans. Testing includes identifying and confirming
formatting, field values, and record counts. All results are documented and shared with the client for each test file
received. Our benefit accuracy is 100% upon implementation.
As noted, LDH and the MCO’s implementation process will be much more efficient than any other PBM
because of our significant presence today. We already implemented the LDH PDL and clinical criteria,
provider roster download, and claims payment to the LDH pharmacy network. This will limit primary areas of
testing to accepting the 834 file directly from LDH, loading LDH pricing methodologies, and sending the claims
encounter file on a weekly basis. We will only have to implement data exchanges and payment files between CVS
Health and AmeriHealth Caritas of Louisiana and United Healthcare Community Plan. Our. Our current presence
is a true value-added benefit for the smooth transition to the MCO PBM model.
Providing a skilled and effective local account team
We will ensure the LDH-assigned staff is tailored to the need of LDH, the MCOs, and Medicaid enrollees

Louisiana Medicaid Page 26
© 2022 Caremark. All Rights Reserved.
The CVS Health account team will provide the insights we have based upon local and national Medicaid
experience. On a quarterly basis we will meet with LDH to provide data insights and opportunities to improve
outcomes and reduce costs. These meetings will demonstrate why CVS holds the majority of managed Medicaid
business in the nation. We understand that not every MCO pharmacy management tool is available in FFS
programs, however, we are confident that we can help LDH drive better outcomes and cost savings through the
quarterly review.
Our goal is to provide you and your enrollees the best service, support, and strategies – with continued
innovation and investments in cost management, clinical solutions, and cutting-edge technology – to help
lower costs, improve outcomes, and increase satisfaction.
Thank you for your consideration.
Medicaid: Multi-state plan client case study
This Medicaid was concerned with helping enrollees meet their health challenges. Our data analysis showed that only
9% of enrollees had complex conditions, but they accounted for 72% of pharmacy spend, including nearly all of
specialty medication spend. These enrollees averaged 29 pharmacy visits per year, and 40% had 7 or more
maintenance therapies. Antidiabetics were a top category for these enrollees and for their chronic members as well.
Both the complex and chronic enrollees represented 17% of the plan’s enrollment and averaged 12 pharmacy visits
per year.
Based upon this MCOs input and population health-level data, we recommended a number of actions. Based on the
proposed actions, tight management in terms of formulary choices, step therapy and quantity limits helped this plan
save $720 million and kept gross trend in the low single digits. Prior authorization reduced wasteful spend; and
compounds, opioids, and hyperinflated drugs were also targeted. In addition, the plan implemented vaccination
services for this diverse population to support preventative care.
Key results over a 12-month period include:
• $720 million in pharmacy spend savings
• 2.3% gross trend
• $275 million wasteful spend savings, a reduction of 15%
• $445 million inefficient spend savings, a reduction of 23%

Louisiana Medicaid Page 27
© 2022 Caremark. All Rights Reserved.
1.8 Proposal Response Format
Proposers should respond, item by item, to each section under 1.8 Proposal Response Format.
There is no intent to limit the content of the proposals, and Proposers may include any additional
information deemed pertinent. Emphasis should be straightforward and concise statements,
summarizing the Proposer's ability to satisfy the requirements of the RFP and outlining the
exceptional qualities they bring to the proposal.
Proposals should include information that will assist the Department in determining the level of
quality and timeliness that may be expected. The Department shall determine, at its sole
discretion, whether or not the RFP provisions have been reasonably met. The proposal should
describe the background and capabilities of the Proposer, give details on how the services will
be provided, and shall include a breakdown of proposed costs. Work samples may be included
as part of the proposal.
Proposals should address how the Proposer intends to assume complete responsibility for
timely performance of all contractual responsibilities in accordance with Federal and State laws,
rules, regulations, policies, procedures, and manuals and the State Plan.
Proposals submitted for consideration should follow the format and order of presentation
described below:
1.8.1 Cover Letter
A cover letter should be submitted on the Proposer's official business letterhead explaining the
intent of the Proposer. Cover letter should contain the following information:
• Summary information about the Proposer's organization.
• Location of Central Administrative Office with Full Time Personnel, including the address for
all office locations with full time personnel.
• Name and address of principal officer.
• Name and address for purpose of issuing checks and/or drafts.
• For corporations, a statement listing name(s) and address(es) of principal owners who hold
five percent (5%) interest or more in the corporation.
• If out-of-State Proposer, give name and address of local representative; if none, so state.
• If the Proposer was engaged by LDH within the past twenty-four (24) months, indicate the
contract number and/or any other information available to identify the engagement; (if none,
so state).
• Proposer's state and Federal tax identification numbers.
The cover letter should include a positive statement of compliance with the contract terms
defined herein. If the Proposer cannot comply with any of the contract terms, an explanation of
each exception should be supplied. The Proposer should indicate the specific section and
language in the RFP and submit exceptions or exact contract modifications that it may seek.
Please refer to CVS Health’s Cover Letter.
1.8.2 Table of Contents

Louisiana Medicaid Page 28
© 2022 Caremark. All Rights Reserved.
The proposal should contain a table of contents, and each section in hard copy submissions
should be separated by a tabbed page that includes headings and numbering to match the
corresponding section of the RFP.
1.8.3 Executive Summary
This section serves to introduce the scope of the proposal. It shall include administrative
information including Proposer contact name and phone number, and the stipulation that the
proposal is valid for a time period of at least ninety (90) Calendar Days from the date of
submission. This section should also include a summary of the Proposer's qualifications and
ability to meet the State agency's overall requirements in the timeframes set by the agency.
Please refer to Section II for CVS Health’s Executive Summary.
1.8.4 Company Background and Experience
The Proposer should give a brief description of their organization or corporate entity including
brief history, corporate or organization structure, number of years in business. The Proposer
shall include copies of its latest three (3) years of audited financial statements. The proposal
should indicate the Proposer’s firm has a record of prior successful experience in the
implementation of the services sought through this RFP. Proposers should include statements
specifying the extent of responsibility on prior projects and a description of the projects’ scope
and similarity to the scope of services outlined in this RFP. All experience under this section
should be in sufficient detail to allow an adequate evaluation by the Department. The Proposer
should have, within the last thirty-six (36) months, implemented a similar type of project.
Proposers should identify at least two customer references for projects implemented in the last
twenty-four (24) months. References shall include the name, email address and telephone
number of each contact person.
The Proposer shall provide a brief statement if any of the following has occurred: Within the last
ten (10) years, Proposer’s Pharmacy Benefits Manager contract was (1) terminated or not
renewed for non‐performance or poor performance; and/or (2) terminated on a voluntary basis
prior to the contract end date. The Proposer must provide the name and contact information of
the lead program manager of the contracting entity.
The Proposer shall disclose all financial, legal, contractual, and other business interests of the
Proposer and any Subcontractor, affiliate, partner, parent, subsidiary, or other similar entity
related to the activities detailed in the Scope of Work. In this section, a statement of the
Proposer’s involvement in litigation that could affect this work should be included. If no such
litigation exists, the Proposer should so state.
Proposers should clearly describe their ability to meet or exceed the qualifications described in
the Mandatory Qualifications for Proposer section.
Proposers should clearly describe their ability to meet or exceed the desired qualifications
described in the Desirable Qualifications for Proposer section.
Ranked #4 on the Fortune 500 list, CVS Health Corporation is the largest health care provider in the United
States with integrated offerings across the entire spectrum of health care. Through our unique suite of assets,

Louisiana Medicaid Page 29
© 2022 Caremark. All Rights Reserved.
we are reinventing health to offer innovative solutions that help people on their path to better health. We are
focused on enhancing access to care, lowering overall health care costs for members and payors, and
improving health outcomes. We effectively manage health care costs and improve health care outcomes
through the following divisions and associated start dates:
• CVS Pharmacy: The retail segment of CVS Health Corporation is America’s leading retail pharmacy. The
first CVS Pharmacy store, selling health and beauty products, was founded in 1963 in Lowell, Mass. by
brothers Stanley and Sidney Goldstein and partner Ralph Hoagland. In 2015, CVS Health Corporation
acquired Target’s Pharmacy and Clinic business.
• CVS Caremark: The pharmacy benefit management (PBM) and mail service pharmacy segment of CVS
Health Corporation provides a full range of PBM services. Pharmaceutical Card System (PCS), a
predecessor of Caremark, was founded in 1969 in Scottsdale, Arizona, effectively launching the
pharmacy benefit management industry.
• CVS Specialty: The specialty pharmacy business of CVS Health Corporation (part of the PBM segment)
includes our specialty pharmacy services for patients who require treatment for rare or complex
conditions. We pioneered hemophilia home care and began supplying specialty medications in 1978, via
predecessor Baxter Health Care Corporation.
• Aetna: The medical business of CVS Health Corporation is one of the nation’s leading diversified health
care benefits companies with a broad range of traditional, voluntary and consumer-directed health
insurance products and related services. Founded in 1853 in Hartford, Connecticut, we entered the group
health insurance business in 1936.
• CVS MinuteClinic: The retail medical clinic business of CVS Health Corporation (part of the Retail
segment) is the leading retail medical clinic provider in the United States. The first QuickMedx centers
(the predecessor to MinuteClinic) opened in the Minneapolis-St. Paul area in May 2000 as a more
affordable alternative to ERs and urgent care centers.
• Omnicare: The long term care business of CVS Health Corporation (part of the Retail segment) is a
national provider of pharmacy services to the long-term care market, which includes skilled nursing
facilities and independent and assisted living communities. Acquired in 2015, it enhances our service
offerings to address the needs of an aging population across the continuum of senior care.
CVS Health Corporation, together with its subsidiaries, is the nation’s premier health innovation company
helping people on their path to better health. We have three reportable segments: Pharmacy Services,
Retail/LTC, and Corporate. These segments include our brands, which are outlined in the following high-level
organizational structure.

Louisiana Medicaid Page 30
© 2022 Caremark. All Rights Reserved.
CaremarkPCS Health, L.L.C. ("CVS Health") is a wholly-owned direct subsidiary of CaremarkPCS, L.L.C., a
subsidiary of Caremark Rx, L.L.C., whose ultimate parent company is CVS Health Corporation.
With roots dating back to 1969, CVS Health began the industry that came to be known as pharmacy benefit
management by creating more efficient and economical ways for Enrollees to receive prescriptions. To keep
pace with a rapidly changing health care market, we have evolved beyond the original business of claims
processing and administrative services to include new areas of health management and health care
information technology. CVS Health has provided PBM services in Louisiana to MCOs, and we currently
support over one million enrollees, covering more than 50% of all managed Medicaid lives within the State of
Louisiana.
We are URAC-accredited and have supported managed Medicaid clients since 1988. We currently support 27
managed Medicaid health plans, of which three are currently in Louisiana, with 135 unique lines of business,
representing more than 27 million Enrollees, of which nearly one million are in Louisiana, across 37 states.
Our Medicaid health plans cover children, nondisabled adults, pregnant women, individuals with disabilities,
and seniors eligible for both Medicaid and Medicare benefits. We’re always evolving to meet changes in
Medicaid program designs and regulations.
CONFIDENTIAL
CVS Health Corporation
Corporate
Executive
Mangaement
Corporate Relations
Legal
Compliance
Human Resources
Information
Technology
Finance
Pharmacy
Services
CVS Caremark
(PBM)
CVS Specialty
Retail/LTC
CVS Pharmacy
CVS MinuteClinic
Omnicare (LTC)
Health Care
Aetna

Louisiana Medicaid Page 31
© 2022 Caremark. All Rights Reserved.
CONFIDENTIAL
CVS HEALTH INVESTMENTS IN LOUISIANA
CVS Health has more than 2,400 Louisiana-based employees as of January 1, 2022. We have more than
80 CVS Pharmacy locations, including seven HealthHUB and seven MinuteClinic locations, within the State of
Louisiana, as well as a Coram specialty infusion suite.
MANDATORY AND DESIRABLE QUALIFICATIONS
As stated above, CVS Health has extensive experience as a PBM for MCOs in the Louisiana Medicaid
program. In addition, CVS Health continues to grow its business in other PBM Medicaid markets, as
exemplified by the addition of Anthem Incorporated and Centene Corporation.
Further, CVS Health confirms that its headquarters and offices are located inside the continental United
States, and it has provided the requested three years of audited financial statements as attachments to this
proposal response, to demonstrate the company’s strong financial standing.
As the current PBM for three MCOs serving the Louisiana Medicaid population, CVS Health confirms its
ability to accept, price, and process physician-administered Drug Claims, apply UM criteria as specified by

Louisiana Medicaid Page 32
© 2022 Caremark. All Rights Reserved.
LDH, maintain e-prescribing tools, and support the PDL, prior authorization program, and all coverage details
of the Louisiana Medicaid Program.
From time to time, CVS Health and its subsidiaries and affiliates have been subject to various legal
proceedings in the normal course of business. However, CVS Health is not aware of its involvement in any
litigation that could affect its work in meeting the activities details in the Scope of Work. Please refer to
Section V Tab 1 and 2 for CVS Health’s 10-K reports for 2019 and 2020. To view CVS Health’s 2021 10-K
report, please refer to the following link: https://d18rn0p25nwr6d.cloudfront.net/CIK-0000064803/d06cfa07-
b8f8-49c0-9f5c-552a41b68e5d.pdf
Over the last 5 years, we have not been provided notice of deficiency, non-compliance or terminations due to
defaults or with cause. We do not have any clients that have terminated with us due to the performance of
services. Clients who have terminated with us over the last 5 years have done so during a competitive RFP
process or due to changes within their own companies such as moving to an exchange, limiting their benefit
offering, or acquisitions and changes to business structure.
1.8.5 Approach and Methodology
Proposals should define the Proposer’s approach and methodology in providing services and
identify the tasks necessary to meet the RFP requirements of the provision of services, as
outlined in the RFP, and as specifically found in Section 1.8.6, Administrative Data, Section 1.8.7,
Word Plan/Project Execution; and Section 1.8.8, Detailed Scope Response. Proposals should
include enough information to satisfy evaluators that the Proposer has the appropriate
experience, knowledge and qualifications to perform the scope of services as described herein.
Proposers should respond to all requested areas.
CVS Health’s mature approach to project management and governance will be a key driver to our collective
success throughout this implementation.
PROJECT GOVERNANCE
The Figure below outlines a best practice starting point for how we will work with LDH to align resources and
responsibilities to ensure a strong one-to-one collaborative relationship throughout the implementation life
cycle. All functional areas will have a single, accountable owner from CVS Health. In addition to those
owners, we will incorporate key roles such as Implementation Program Managers and Enterprise Quality
Managers to provide cross-functional accountability around key items such as activity completion timeliness,
current and accurate project artifacts, all testing outcomes for all areas, and data integrity. Our goal is to
establish formal roles and responsibilities both at a workstream level and cross-functionally to ensure
appropriate oversight and accountability across the entire implementation process.

Louisiana Medicaid Page 33
© 2022 Caremark. All Rights Reserved.
Project Management Methodology
One of CVS Health’s key guiding principles is that we must execute against a single, integrated project plan.
Again, we will start with a best practice standard plan for this implementation and review it line by line jointly
to ensure that all activities are included. Each activity will ensure that we have tied in the appropriate
dependencies, that there is an appropriate amount of time for handoffs of work (examples: deliver test results,
review test results, provide feedback, clarify feedback, review final results, approve results) to set the
appropriate expectations. All tasks will be tied to one single, accountable owner rather than groups of people
or functional areas. The entire methodology around the plan is to ensure that it clearly states who will be
doing what through the entire implementation to ensure its success. Any need to adjust these activities after
they are agreed upon and baselined will be governed by a joint change control process.
We use a comprehensive project plan that outlines each implementation task and includes defined timelines
and deliverables around documenting and approving client requirements in time to fully configure and test
prior to the plan effective date. Because of diverse client needs, our implementation process is flexible
enough to allow focus on the unique requirements of each client’s implementation. The Implementation
Project Manager and Account Team will ensure that our management and implementation team work to
deliver a successful implementation and will manage escalations as needed.
Our project management methodology begins with an interrelated series of activities illustrated in the Figure
below; these activities enable and ultimately lead to:
• Development activities: Coordination of test and production eligibility files, review Enrollee
communications, build the benefit plan designs, and receipt of vendor transition files.
• Testing activities: unit, system integration, performance and user acceptance testing.
• Deployment activities: Coordination of Enrollee communications, receipt of final eligibility file, Customer
Care begins taking calls, and the website is available for Enrollees to access.

Louisiana Medicaid Page 34
© 2022 Caremark. All Rights Reserved.
• Maintenance activities: Monitoring all post effective activities including Customer Care, Enrollee
communications, and ensuring accuracy of claim adjudication.
Establishing and agreeing upon a formal escalation process early in the life of a project is key to its success.
As such we will work with the MCOs to establish a successful project escalation structure. In our experience,
the structure illustrated in the below Figure has proven effective.

Louisiana Medicaid Page 35
© 2022 Caremark. All Rights Reserved.
Each MCO’s dedicated Account Team will be involved with all aspects of Implementation to help ensure
seamless service and accountability. Each MCO’s Implementation Project Manager will be the single point of
contact and will lead and drive the implementation process from start to finish. Our proven experience in
health plan implementations has shown that the strategic advisory role of our dedicated Implementation
Project Manager is central to securing an efficient transition with minimal disruption.
CVS Health subject matter experts will be assigned to various project workstreams. We have a proven
process that tracks all the important milestones and timeframes, including standard templates for project
status reports. We propose holding weekly project status and issue management meetings with the LDH team
and each of the MCOs.
Change, Risk, Action, Issue and Decision (CRAID) Management
We have successfully implemented hundreds of clients, including many Medicaid MCOs, by utilizing proven
project management tools such as our integrated Change, Risk, Action, Issue and Decision (CRAID) log,
illustrated in the below Figure. This artifact combined with the expertise and knowledge of our implementation
team, we will demonstrate highly consultative capabilities when it comes to risk mitigation, issue resolution,
and contingency planning. Our CRAID log is designed to gather key information tied to a risk or issue – a
single accountable owner, an actionable mitigation plan for risks, a clear outline of activities for the resolution
of issues, and a clear understanding of contingency plans should an agreed upon mitigation approach fail. We
will work together through our management of activities within the project plan to identify these items and
have the CVS Health team lead the joint discussion around the establishment of a clear, joint problem
statement, owner, due date, and mitigation planning.

Louisiana Medicaid Page 36
© 2022 Caremark. All Rights Reserved.
Examples of actual risks we have encountered on our PBM implementation, as well as solutions we have
found successful, include:
Risk 1: Dependence on the incumbent vendor to provide accurate refill, prior authorization, claims, and/or
account balance files. Resolution: We will work with LDH and the incumbent PBMs to establish a
comprehensive PBM transition plan, including an extensive routine of testing protocols. We will also host
weekly meetings to monitor timeframes and key deliverables.
Risk 2: Transferring prior authorizations. Resolution: Because prior authorization coding differs among
PBMs, we thoroughly review the prior authorization information from the incumbent PBM in order to determine
the most appropriate translation method for loading the other PBM’s prior authorization data into our system.
This is typically done by either identifying a one-to-one match of the prior authorization codes or by analyzing
the drug categories supplied on the file to determine which benefit structures need to be overridden under the
new plan design. This will help ensure the prior authorizations load correctly into our system.
Risk 3: Notifying Enrollees of their new PBM vendor. Resolution: We believe in proactive communication to
Enrollees to help ensure successful implementations. We will develop a phased communication strategy
using various communication vehicles to communicate to Enrollees the change in vendors. Sample strategies
can include a welcome message using IVR, access to all of the necessary information through
Caremark.com, benefit fair participation, incumbent vendor messaging, and pre-enrollment Customer Care
support.
1.8.6 Administrative Data
This section should:
• State Proposer’s knowledge and understanding of the needs and objectives of LDH
Pharmacy and the MCOs as related to the scope of this RFP.

Louisiana Medicaid Page 37
© 2022 Caremark. All Rights Reserved.
LDH will not have a more qualified respondent to the Single PBM request for proposals. As of the date of
our submission, more than 50% of Louisiana managed Medicaid Enrollees who are enrolled in
managed Medicaid are being serviced on CVS Health’s systems through the three Managed Care
Organizations we support: Aetna Better Health Louisiana, Health Blue Louisiana (Anthem, Inc.)
and Louisiana Healthcare Solutions (Centene Corp.). This means that there will be minimum Enrollee
and MCO disruption when the state transitions to the Single PBM.
• Enrollee prior authorizations and medications for more than 50% of Enrollees will seamlessly transfer,
resulting in full continuity of care. The initial implementation accuracy for go-live is at 100%. The
maintenance of business plan changes accuracy is at 99%.
• Because CVS Health’s pharmacy network includes all of LDH’s pharmacies, no Enrollee will have to
change pharmacies.
• Communications and data exchanges between three of the five MCOs and LDH will remain in place,
which will mean a more efficient implementation and less effort for LDH and MCOs.
• In 2021, CVS Health completed approximately 200,000 prior authorizations for the book of business
delegated services for the Medicaid population.
As the PBM for three of the current five MCOs, we are experts in LDH’s policies, programs, and
regulations. We have developed Louisiana specific policies and processes to address plan requirements,
as needed, and are prepared to continue to do so as part of the single PBM program.
Our approach to becoming the MCO PBM will be to continue the same work we do today and when the
new MCO contracts are implemented:
• Point of service claims adjudication including coordination of benefits
• Transparent pricing
• Point of service drug utilization review
• Pharmacy payments
• Fraud waste, and abuse monitoring
• Prior authorization
• Retrospective drug utilization review programs
• Our gold standard network audit program
• Our opioid program that has reduced use and misuse
• Enrollee and provider support
Accountability
We know that price transparency is a State priority. CVS Health will be a fully accountable partner to LDH.
We will provide LDH with unredacted access to our claims adjudication engine results through
our Client Online Services portal. With this access, LDH will be able to view and audit our claims
adjudication to ensure claims are paid appropriately and in accordance with LDH-established pricing
methodology, including the LDH MAC list and related pricing.
When we implement changes to the PDL or benefit design, LDH will have unfettered access to our pre-
production testing environment to develop testing scenarios. This will allow LDH to provide test scenarios
and have a higher level of comfort with 100% accuracy prior to moving the coding to production.
Best in class technology and analytics to ensure benefit set up accuracy, drug
dispensing and accuracy and safety
CVS Health continually invests in technology to improve our performance and to provide our clients
increased accuracy in benefit set up, near real-time review of claims to identify drug utilization anomalies
not caught at the point of sale, and aberrant claims that may require auditing.

Louisiana Medicaid Page 38
© 2022 Caremark. All Rights Reserved.
LDH will have the same technology and analytics that their Louisiana MCOs have today. We use
sophisticated algorithms and real-time claims surveillance to automatically identify benefits administration
issues. These rule-based and machine-learning algorithms detect potential issues with benefit coding
during near real-time claims adjudication. Our claims surveillance process runs multiple times a day.
Because of the near real-time reporting, we are able to conduct rapid response reviews of aberrant claims
adjudication.
Our Drug Savings Review program is an enhanced, buy-up option available should Louisiana or any of
the MCOs be interested, and provides a thorough review of a Enrollee’s medication profile within 72
hours after claim adjudication. When combined with our ongoing review of the Enrollee’s prescription
history, it helps us identify those who might be at risk for drug interactions or drug-induced disease
conditions, regardless of the point of service. This can result in identification of opportunities to help
reduce unnecessary prescriptions and streamline Enrollee therapy.
Best in Class Pharmacy Network Audit
As a company staffed with hundreds of pharmacist-employees, we understand the need to minimize
pharmacist provider abrasion during the auditing process. We use CVS Health employees to audit our
pharmacy network to help ensure that covered drugs are filled in accordance with the provider
agreement.
Additionally, our Pharmacy Performance Department believes that the best way to protect patient safety
and the financial resources of LDH is through rapid response desktop reviews. We developed a highly
effective leading-edge algorithm to review every claim submitted for reimbursement.
The algorithm contains a closely held set of rules that identifies claims that are potentially erroneous or
unusual. The claims flagged as erroneous undergo a secondary review by certified pharmacy technicians
who may call the pharmacy and review the claim over the phone.
The rapid response process is invisible to the Enrollee – if the technician reviews the claims with the
pharmacy, only CVS Health and the pharmacy know that a review occurred on the claim, thereby
preserving the Pharmacist-Patient bond. This reinforces the trust between the pharmacist and patient,
which is important to maintaining the pharmacist as a trusted member of the Enrollee’s health care team.
CONFIDENTIAL
Clinical programs that improve health outcomes
CVS Health can offer our enhanced Transform Care program if LDH or the MCOs are interested, which
combines clinical expertise and data analytics to enhance MCOs’ disease management strategies with
targeted, comprehensive, Enrollee support that bridges the gap between their everyday lives and their
physician’s office.
For example, our Transform Diabetes Care uses advanced analytics to assess Enrollee pharmacy data,
along with biometric insights from a connected glucometer, used by some Enrollees, to better understand
their diabetes management and unique needs. This enables our MCOs to develop personalized
‘interventions, delivered by health care professionals, to help improve their medication management,
blood glucose control, and condition management.
Our outcomes-based model focuses on improvements in blood glucose control, adherence and healthy
behaviors, while targeting an aggregate, one-point average decrease in A1C among the uncontrolled
portion of a diabetic population. Integrated systems enable collaboration between our program and
providers, plans and existing disease management programs to effectively extend the reach of the
physician, support client goals and align all points of care throughout Enrollee therapy. This coordinated
approach to diabetes management helps drive the greatest improvements in care for Enrollees with
diabetes, while helping our clients better protect their pharmacy investment.

Louisiana Medicaid Page 39
© 2022 Caremark. All Rights Reserved.
A seamless transition and implementation
As noted, LDH’s and the MCO’s implementation process with CVS Health will be much more
efficient than any other PBM because of our significant presence today. We will already have
implemented the LDH PDL and clinical criteria, provider roster download, and claims payment to the LDH
pharmacy network. This will limit primary areas of testing to accepting the 834 file directly from LDH,
loading LDH pricing methodologies, and sending the claims encounter file on a weekly basis. We will only
have to implement data exchanges and payment files between CVS Health and AmeriHealth Caritas of
Louisiana and United Healthcare Community Plan. Our current presence is a true value-added benefit for
the smooth transition to the Single PBM model.
Post-Payment Recoveries
CVS Health provides a number of services to assist Medicaid in their post-service recoveries and cost-
avoidance strategies for drug reimbursement claims.
CVS Health maintains a dedicated Third-Party Liability (TPL) and Subrogation team for the processing of
Medicaid TPL/Subrogation claims (e.g. Pay & Chase) per applicable state and federal law. This same
team maintains direct working relationships with all US states, and national service providers for Third-
Party Liability and Subrogation services.
CVS Health maintains several services to identify and process Medicaid TPL & Subrogation claims
including direct connections to service providers and many US States. These direct connections allow
for the adjudication of digitally presented claims within 72 hours of receipt. CVS Health remits payments
to the appropriate state and/or Managed Medicaid Organization within 21 calendars days.
• In 2021 – CVS Health processed 36M TPL/Subrogation Medicaid Claims with 99.99% presented
digitally. 96% adjudicated within 7 days, and 99.999% within 60 days.
CVS Health also maintains a series of services to assist Medicaid with their cost avoidance
strategies. CVS Health will reject a drug claim submitted with Medicaid as primary when CVS Health is
aware of alternative coverage legally responsible to provide payment ahead of Medicaid.
CVS Health also offers a new premier service to maximize the effectiveness of Medicaid’s post-service
recovery and avoidance strategies. In instances where Medicaid pays primary for a member with
primary coverage on a CVS Health administered and delegated plan, CVS Health can initiate a
TPL/Subrogation claim when directed on behalf of the Medicaid plan. This enhanced service allows the
Medicaid plan to recovery post-service payments in under 30 days.
** This service is exclusively provided by CVS Health. The service provides both an cost effective
solution in recovering service fees from the appropriate primary payor, while also avoiding the
commissions and/or fees charged by all national service providers for TPL/Subrogation services.
All TPL/Subrogation activities, including reimbursements, are recorded in our system of record, and is
made available to Medicaid and/or Managed Medicaid Organizations. CVS Health will make available
the required reports and files, in a format acceptable to Medicaid or national format, to assist Medicaid in
their administration of the plan and financial reconciliations.
Where required by Medicaid, or federal and/or state law, CVS Health will assist the Medicaid with post-
service recovery, the identification of alternative coverage/eligibility, respond timely to all valid legal
inquiries, audits, or similar.

Louisiana Medicaid Page 40
© 2022 Caremark. All Rights Reserved.
While CVS Health does not expect to be presented settlements or otherwise be presented with requests
that would result in Medicaid recovering all the funds for which Medicaid is entitled, CVS Health will
provide proper notification to Medicaid if such instances arise in our performance of our responsibilities.
• Provide a written explanation of the Proposer’s organizational structures of both operations
and program administration, and a description of how the components communicate and
work together in both an administrative and functional capacity from the top down.
Ensuring LDH’s, MCOs’, and Medicaid Enrollees’ satisfaction is the core of our Client Service Team
philosophy. Our model will allow the LDH and MCOs Service Teams the flexibility, innovation, and
collaboration needed to achieve outstanding results on behalf of LDH.
The Client Services’ vision is to achieve exceptional client loyalty by delivering unparalleled service
through effective communication and coordination. We aim to achieve client loyalty through:
• Greater face-to-face collaboration processes among internal team members
• An emphasis on quality, turnaround times, and LDH convenience
• More rigorous processes to track and deliver on LDH and MCO day-to-day needs
• A streamlined team approach, ensuring delivery and accuracy of LDH benefit plan changes on or
before deadlines
• A collaborative focus on the effective execution of the LDH’s strategies.
• We are focused on continuously adapting our support philosophy to stay in line with the evolving
needs of LDH.

Louisiana Medicaid Page 41
© 2022 Caremark. All Rights Reserved.
MCO SERVICE TEAMS
In addition to supporting LDH, all Louisiana MCOs will have access to the expertise of the LDH Service
Team. Each team member has extensive experience supporting Medicaid Enrollees. Every state is
unique in their requirements and we will ensure continuity of the current account teams assisting the
Louisiana MCOs we service today. For the MCOs we don’t serve today, we will take pride in selecting
team members with backgrounds and experiences with significant Medicaid experience.
CHANGES IN ACCOUNT TEAM ASSIGNMENT
We will agree not to change the assigned Executive Director, Account Director, or Audit Pharmacist
without LDH’s consent, except in the case of a promotional opportunity, request for reassignment,
employee termination, or other reasonable justification to manage the business.
We recognize the importance of continuity and consider client relationships a top priority. We strive to
minimize changes to account teams whenever possible. LDH and the MCOs will be notified immediately
in the event of a key personnel change. We will create a comprehensive and thorough succession plan to
support the transfer of knowledge and responsibility from your key contact to their replacement.
In addition, account team members have access to our customer relationship management tool. This
central repository stores specific contact and account information to ensure continuous support of the
client relationship.
Your satisfaction is paramount, and we carefully choose account team members based on your unique
requirements. We are driven to achieve 100% client satisfaction and retention. Our account team
members’ individual employee evaluations and overall CVS Health evaluations are based on client
feedback regarding service performance and overall satisfaction.

Louisiana Medicaid Page 42
© 2022 Caremark. All Rights Reserved.
If you are not completely satisfied with your account team and request a replacement, we will address
your concerns and make changes as necessary.
LDH ACCESS TO SUBJECT MATTER EXPERTS
One of the responsibilities of your account team is to engage subject matter experts across our company
including doctors, pharmacists, nurses, IT, reporting and more. This engagement may be initiated by the
account team or in response to an LDH request. Each member of your account team makes it a priority to
remain informed with the most up-to-date information to assist you in all areas.
TRAINING
Our implementation and account teams will work to ensure that Customer Care Representatives are
trained on any Louisiana-specific information via computer-based training, bulletin postings to the internal
proprietary online tool, and through desk-based reference information.
LDH-specific training will be administered to focus on the overall business culture and unique needs of
Louisiana Medicaid Enrollees. This training is designed to help Customer Care Representatives fully
understand the unique plan design parameters and culture of Louisiana Medicaid. Our goal is to serve as
an extension of your benefits offices, and LDH-specific training provides our representatives with the
information they need to achieve that goal.
• Contain a brief summary setting out the Proposer’s management philosophy including, but
not limited to, the role of Quality Control, Professional Practices, Supervision, Distribution of
Work and Communication System.
To serve our health plan client base we staff our account service team with knowledgeable, experienced
professionals whose focus is providing the highest level of customer service for our clients. Customer
service excellence starts at the top of our organization and every colleague is responsible and
accountable to work collaboratively with others across our organization from Customer Care, Mail,
Specialty, Marketing, Plan Design, Analytics and more to support your goals and align your strategic
direction with our capabilities. We take pride in selecting team members with background and experience
that best meet your unique needs. Customer satisfaction is a key performance metric across our
enterprise and while your account team is the front line, they have the backing of our entire organization
in ensuring the success of your programs.
Our consultative services play a major role in supporting our clients’ strategic goals for managing
pharmacy and total health care trend, while working together to improve health outcomes.
Your account services team will include dedicated account management resources with managed
Medicaid expertise. These resources include clinical, account, and client services teams. We will also
include management of per member per month (PMPM) performance to meet client goals during
challenging budgetary times. And, of course, we can help ensure our compliance with policy and
legislative tracking activities associated with Medicaid regulations at the state level.
Our “management philosophy” is one of service excellence for all constituents. Our Caremark Service
Excellence team, is a cross functional group that oversees the issues management process, instituting
core operational discipline and leading the culture transformation. They create visibility to trends and high
priority issues; drive accountability; and ensure issue prevention through better collaboration. This is
comprised of leaders across account management, benefits, client services, data operations, analytics,
finance, IT, product, human resources, and Medicare operations that meets weekly to address client and
member issues. Our focus is to ensure that we address issues as they arise, so we can align the right
resources to resolve issues, do a thorough root cause analysis, and then take action. This philosophical
approach applies not just in high priority events but also in smaller teams across the organization as we
have transformed how we think about continuous improvement.

Louisiana Medicaid Page 43
© 2022 Caremark. All Rights Reserved.
We will work collaboratively with LDH to ensure our team is fully trained on all aspects this program. To
start, the identified team members all have deep Medicaid experience including in Louisiana. As we
respond to this RFP and in the subsequent months, will work diligently to ensure all of our team members
are fully oriented to the LDH and this program.
CVS Health provides employees working within the Medicaid space the foundational skills and expertise
to be successful in meeting our clients specific needs. Our Medicaid educational approach is
multipronged. We provide our Medicaid internal stakeholders with detailed Medicaid trainings that cover
both internal and external market information. For example, these trainings cover the following topics:
• Foundation in how the federal government works with states to fund and administer Medicaid
• Overview of enrollment, eligibility and coverage (mandatory & optional benefits)
• Overview of quality and incentive programs
• Understanding of care delivery models including managed care and managed care organizations
(MCOs)
• Highlight of key policy developments impacting the program, including trends in drug benefit
management and future payment reform options
We also realize that each state is unique, and to that end, we generate regularly updated market profiles
on each Managed Medicaid state that we operate in – including the State of Louisiana. We also regularly
review and share local, state and federal Medicaid news and information with key Medicaid market
stakeholders on a daily, weekly and monthly schedule. Taken together, this foundational and ongoing
educational support in Medicaid ensures not only the success of our employees but also the success of
our clients who operate in this complex and rapidly changing market.
In addition, department programs are supported by full-time, dedicated professional Learning and
Development teams that deliver educational programs specific to their individual department, job function,
and professional development needs.
We design onboarding and learning programs tailored to the roles of our colleagues serving our clients.
Tracks are designed specifically for Sales, Strategic Account Executives, Clinical Advisors, and Account
Managers. We benchmark against and leverage other learning professionals and tools, including
Corporate Executive Board, XBInsight, Huthwaite, and Salesforce.
Our account management new-hire training program, a three-week onboarding program, employs a
blended solution with instructor-led, online and on-the-job training for technical system proficiency and
soft-skill building. On-the-job activities alongside an assigned mentor supplement structured training for
autonomy and immediate application of knowledge to support adult learning principles. Learning guidance
and feedback throughout training elicits performance to identify additional development opportunities. A
final assessment is required to transition into the role and interface with clients. Account Managers enter
the position with a range of experience, from recent college graduates to experienced customer service
professionals. Pre- and post-assessments show an average 65% increase in learning objective
knowledge. Customer retention and loyalty surveys, a measure of level four evaluation, show only a 3%
differential in overall performance ratings between new and tenured Account Managers, an indication that
new-hire training effectively prepares students to serve clients at a comparable level to tenured Account
Managers.
Ongoing education opportunities for sales professionals are delivered throughout the year through office
hours, Investing in You, and Learning Exchange virtual trainings. All learning curricula and content are
indefinitely accessible on Max+, a sales collateral library and knowledge portal that can be accessed by
account team members (online or by mobile) in the client relationship management tool that is central to
their job functions.

Louisiana Medicaid Page 44
© 2022 Caremark. All Rights Reserved.
All new hires and contingent workers must complete the courses below within 30 days of employment.
Additionally, all employees and contingent workers must complete these same courses on an annual
basis. All courses listed have been delivered over the past 12 months.
• Integrity Training (Code of Conduct) – New hire and annual
• HIPAA Privacy and Security – New hire and annual
• Medicare Fraud Waste and Abuse – New hire (all employees) and annual (those who are directly or
indirectly involved with the benefit).
CVS Health also provides the following training to CVS Health Clinical Advisors and Service Team
members.
Objective: Enable team members with key strategic & background information on the health plan
Medicaid market
Proposed Scope of Training:
• Foundation in how the federal government works with states to fund and administer Medicaid
• Overview of enrollment, eligibility and coverage (mandatory and optional benefits)
• Overview of quality and incentive programs
• Understanding of care delivery models including managed care and MCOs
• Highlight of key policy developments impacting the program, including trends in drug benefit
management and future payment reform options
• Understanding of Medicaid clients’ needs and expectations
• Louisiana Medicaid policies, key regulations, and compliance
Once account team members complete orientation, they are exposed to a variety of additional in-depth
classes, workshops, and webinars related to their positions and job responsibilities.
ACCOUNT MANAGERS
New Account Managers are required to complete a new-hire course focusing on operational processes,
system functionality, our programs and services, and internal departments. Throughout class, new hires
work on client activities and complete additional courses focusing on value-added services and soft-skills
development (e.g., communication, relationship building, critical thinking). These courses are designed to
set their knowledge foundation and build successful client relationships.
ACCOUNT TEAM CONTINUING DEVELOPMENT
Developmental training is ongoing for all Account Team members. Regularly scheduled offerings provide
additional training for all colleagues, along with comprehensive consultative and professional skill
building, including:
• Interaction and communication skills;
• Louisiana Medicaid regulations
• Presentation skills
• Time management.
• Medicaid Clinical advisors weekly meetings
• Regulatory Affairs Committee monthly meetings
• Regulatory Affairs, compliance and legal weekly meetings
• Medicaid Operations and Strategy meetings - monthly
• Department Specific Medicaid training i.e. Encounters team, Finance team, Government Services
team, Clinical Teams, Account Management

Louisiana Medicaid Page 45
© 2022 Caremark. All Rights Reserved.
Medicaid Ongoing Best Practice Training:
• Recurring MCO/PBM – joint operations meetings
• Recurring MCO/PBM- Pharmacy trends/performance meetings
Mentoring programs are provided for all levels of Account Services team members to promote an
environment of open communication, continuous growth, and best practice/knowledge sharing. Product
training and upskilling are communicated and delivered by various methods, including weekly electronic
sales briefings, quarterly sales calls, e-learning modules, recorded conference calls, regional meetings,
and an annual national sales meeting.
Our Implementation and Account teams will work to ensure that Customer Care Representatives are
trained on any client-specific information via computer-based training, bulletin postings to the internal
proprietary online tool, updates to Client Information Forms, and through desk-based reference
information.
CVS Health will ensure that all trained employees with the appropriate qualifications, or other personnel
as approved by LDH, are available for all claims administration services as outlined in the proposal.
1.8.7 Work Plan/Project Execution
The Proposer should articulate an understanding of, and ability to, effectively implement
services as identified in Section 2. Scope of Work. In this section, the Proposer should state the
approach it intends to use in achieving each objective of the scope as outlined, including a
project work plan and schedule for implementation.
The Proposer should:
• Provide a written explanation of how the operations and program administration components
of the Proposer’s organizational structures will support service implementation. Individual
components should include plans for supervision, training, technical assistance, as well as
collaboration as appropriate.
Your executive-led account services team will be responsible for executing a smooth and seamless
implementation. The team works together to provide a highly consultative and well-coordinated transition,
bringing all necessary subject matter experts together to support your program start-up, and help ensure
all program requirements are fully defined and met.
IMPLEMENTATION – A COLLABORATIVE PROCESS
An implementation project manager will be responsible for assembling and leading a team of experts in
the areas of eligibility, benefit design, provider networks, clinical programs, member communications,
vendor transition, and technology and customer service, as needed. Our team meets with your team
members in their respective areas to guide them through gathering and documenting your specific
requirements and confirm understanding through a rigorous review and approval process that will include
outlining how each set of requirements will be tested.
During the implementation process, we will continue to meet with you to help ensure full understanding of
requirements, address any questions, and resolve issues that may arise throughout the process. Your
account services team will also conduct ongoing post-implementation meetings to help ensure that all
aspects of the program are in place and are operating to your requirements.

Louisiana Medicaid Page 46
© 2022 Caremark. All Rights Reserved.
MAINTAINING CLIENT COMMUNICATION
Following implementation, account service personnel will be available, as required, to effectively manage
all aspects of your account. Client support, as well as clinical experts, will be available by telephone or
for on-site meetings, as needed, over the course of a plan year.
ONGOING COLLABORATION
Our experienced account management team is focused on executing on your initiatives through
proactive, professional collaboration. We employ a tenured team with analytic and clinical experience.
Our insights and recommendations help you control costs, maintain high employee satisfaction, achieve
your health and wellness goals and accomplish your business objectives. We do this through strategic
meetings, formulary and specialty management strategy discussions, operational tools for tracking and
training and regulatory support for topics such as retiree benefit options and ACA compliance.
• Demonstrate an ability to hire staff with the necessary experience and skill set that will
enable them to effectively meet the needs of Enrollees.
CVS Health has a deep bench of internal talent and our plan is to leverage those resources to staff our
team. We are confident that by the award deadline we can have our team in place at that time. We will
provide written notification to LDH and the MCOs of anticipated vacancies of Key Management Staff
within two (2) business days of receiving the individual’s resignation notice, our notice to terminate an
individual, or the position becomes vacant. CVS Health will work with LDH to fill Key Management
Personnel positions should any vacancies remain open at the time of contract award.
Your satisfaction is paramount, and we carefully choose account team members based on your unique
requirements. We are driven to achieve 100% client satisfaction and retention. Our account team
members’ individual employee evaluations and overall CVS Health evaluations are based on client
feedback regarding service performance and overall satisfaction.
If you are not completely satisfied with your account team and request a replacement, we will address
your concerns and make changes as necessary. CVS Health will not substitute or exchange Key
Management Personnel without the LDH’s written approval.
We recognize the importance of continuity and consider client relationships a top priority. We strive to
minimize changes to account teams whenever possible. LDH will be notified immediately in the event of a
key personnel change. Within ten (10) business days of receiving the resignation, we will create a
comprehensive and thorough succession plan to support the transfer of knowledge and responsibility
from your key contact to their replacement. LDH reserves the right to approve or reject the plan.
In addition, account team members have access to our customer relationship management tool. This
central repository stores specific contact and account information to ensure continuous support of the
client relationship.
CVS Health will provide resumes of proposed replacement candidates to LDH within thirty (30) calendar
days after vacancy occurs. If a suitable replacement candidate has not been identified within that time
period, CVS Health will provide weekly updates to LDH.

Louisiana Medicaid Page 47
© 2022 Caremark. All Rights Reserved.
• Demonstrate an understanding of, and ability to implement, the various types of
organizational strategies to be integrated within the day-to-day operations.
We have extensive experience in implementing clients with complex pharmacy benefits. These
implementations typically consist of the receipt of multiple eligibility feeds, the building of hundreds of
different benefit plan designs, and the delivery of complex communications to members. As a testament
to our configurable setups, in a recent welcome season we implemented 330 clients of which 259 were
new clients – serving 3.2 million members.
We handled more than 14,209 mailing projects, 1832 inbound member data transition files, and deployed
approximately 54,000 plan benefit changes. We had 387 million test claims processed. On January 7
th
,
the busiest day of the year, we processed over 11.3 million claims and a record 249.5 million claims in the
month of January. We are pleased to report our client satisfaction rating is 97%.
We use our claims processing system as the backbone of our primary operations for pharmacy benefit
administration and claims processing. This will enable a smooth transition for current downstream clients,
as we have great depth of experience with all of the functionality and architecture. In addition, we have
created an environment where we run rigorous test scenarios to help ensure all possible combinations of
edits and criteria are correctly executed.
IMPLEMENTATION TEAM
You will be supported by an experienced, dedicated Implementation team, led by your Implementation
Project Manager. Your Implementation Project Manager will be the single point of contact and will
oversee the implementation process from start to finish. The strategic advisory role of our dedicated
Implementation Project Manager is central to securing an efficient transition with minimal disruption. We
are committing dedicated individuals to manage your account both during your implementation and
throughout your relationship with us.
Your executive-led account services team, in conjunction with your dedicated Implementation Project
Manager, will be responsible for executing a smooth and seamless implementation.
• Collaboration through the discovery process at the kick off meeting
− Open communication to determine and document shared terminology
− Obtain client requirements around plan design, hierarchy, reporting, etc. and help ensure these
are thoughtfully documented in the Client Requirements Document
− Define the timeline using the Project Plan and identify specific tasks needing client sign-off
− Proactively anticipate and document any obstacles that may occur by using the Issues/Risk log
• Experienced implementation professionals
− Matrix of subject matter experts (SMEs) matching your structure and SMEs
− Oversight of end-to-end certification testing and client test environment
− Establish responsibility on both sides for critical decisions
• Governance of the Process
− Follow our proven methodology for managing a successful implementation
− Establish escalation process for quick issue resolution for risk and issue resolution
− Agreed upon timeframes for thorough review and testing.
To align with your complex pharmacy benefit needs, the implementation process is very detailed. Subject
matter experts are assigned and all implementations are managed with a detailed project plan. We have
a proven process that tracks all of the important milestones and timeframes.

Louisiana Medicaid Page 48
© 2022 Caremark. All Rights Reserved.
• Discover: Understanding your lines of business and priorities. Bring key decision makers to
meetings, provide all necessary information and data files and execute timely review and approval of
requirement documents to support the gathering process. Discuss the implementation guide which
provides a roadmap for the process. Document your requirements and provide our recommendations
on plan design, hierarchy, and reporting needs. Determine frequency of communications and
meetings
• Build: Continue attending weekly meetings and completing key client milestones as we execute
activities to implement your requirements
• Test: Support testing and quality assurance activities by continuing to attend weekly meetings,
providing timely approval of test results and supporting vendor collaboration.
• Deploy: Participate in final implementation activities involving preparation, coordination, and quality
checks driven by the CVS Health Implementation Manager leading up to and including the effective
date.
• Maintenance: Monitoring all post effective activities including Customer Care, member
communications, and ensuring accuracy of claim adjudication. Resolution of any identified gaps or
plan design elements from the plan effective date.
BENEFIT TESTING
Our unique and proprietary testing capabilities are key to minimizing operational impacts to plans during
an implementation. Key features include:

Louisiana Medicaid Page 49
© 2022 Caremark. All Rights Reserved.
All of our testing is conducted in a pre-production environment, allowing for plan design changes as
needed until the expected outcome is reached. When test results are confirmed as satisfactory, the plan
design will be moved to our production environment. Client Benefits conducts comprehensive testing that
includes three steps: processing claims (test scenarios), reviewing the data, and verifying/validating the
results.
• Processing Claims – During the claims processing step, claims are created and run against the
benefit design. The test scenarios are built around the client’s benefit design. Typically, a drug is
tested from every category based on the client’s benefit design. While testing for coverage or
exclusion, we will also include testing for pricing, quantity versus time , age limits, contingent
therapy/prior use exceptions, and accumulation testing which includes deductible, out of pocket, and
maximum allowable benefit. Accumulation testing is handled manually to help ensure claims
calculate correctly before the accumulation level, the crossover claim, and after the accumulation
level is reached.
• Reviewing the Data – The second step requires Client Benefits to review their testing outcomes. In
this step we review our test results to confirm that claims accepted or rejected as expected, based on
the client’s benefit design. For rejected claims, we confirm the reject is valid. If the reject is not
related to drug exclusion, it is reviewed to determine if plan and/or macro modifications are
needed. If plan and/or macro modifications are made, retesting will occur to confirm changes provide
the valid drug coverage or exclusion outcomes before moving to the third step in the testing process.
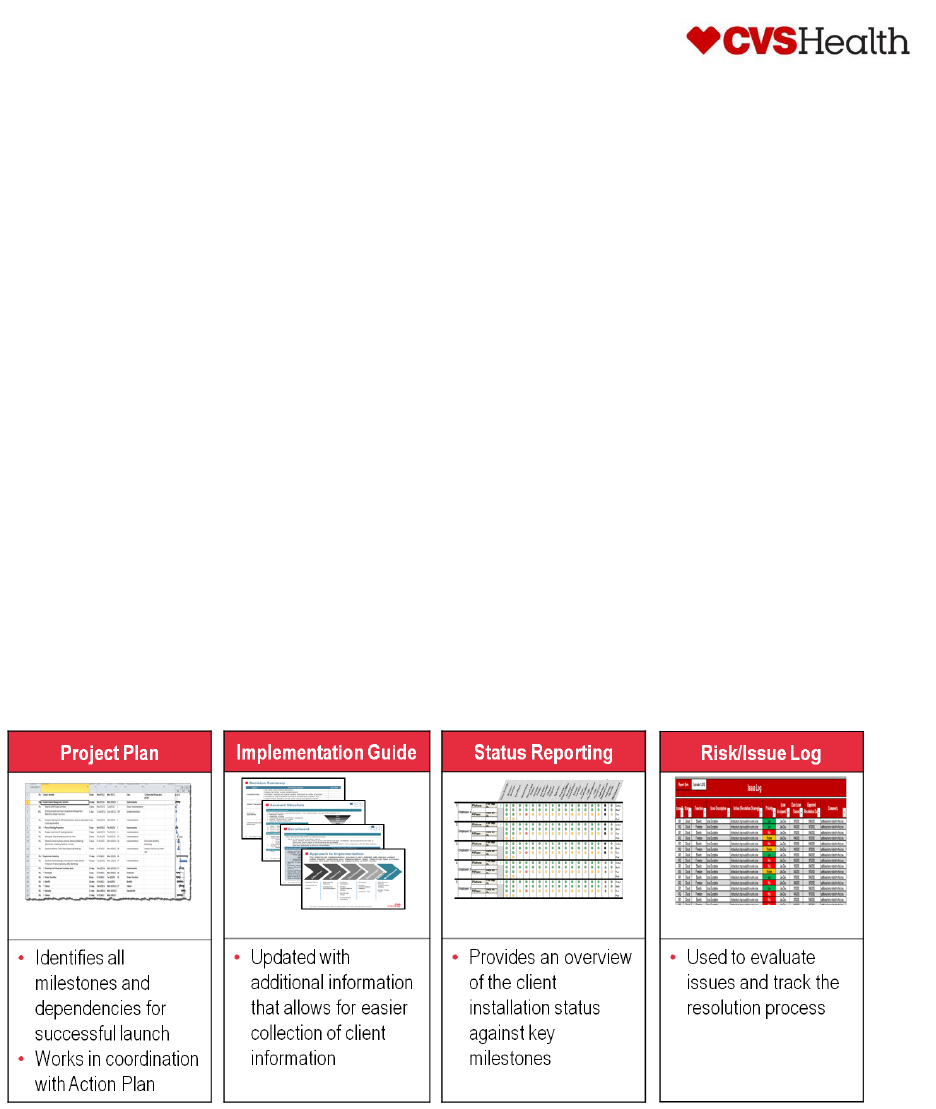
Louisiana Medicaid Page 50
© 2022 Caremark. All Rights Reserved.
• Verifying/Validating Results – The last step of the testing process is to confirm the outcomes are as
expected. We validate drug coverages and exclusions against client documentation. When
reviewing the outcomes, we also confirm the member's copay is correct and the claim calculated as
expected based on the contracted prices. If we find any discrepancies during this step, we will
identify what caused the issue, make any required plan modifications, and process a new set of
claims for review. All test cases and results are reviewed.
CLIENT IMPLEMENTATION TESTING FOR CLIENTS
After benefit testing is completed in the pre-production environment, the client’s data is promoted to the
Client Test Environment (CTE), which is a production-like environment; to perform further testing that
includes production, eligibility, plan, utilization management rules, prior authorizations, and pricing. Test
claims or production claims can be used for testing. After the claims are processed, claim files are
produced which can be reconciled to financials and available to be loaded into client’s Data
Warehouse. Also, an invoice from our billing system will be generated for your review. You will have the
ability to not only reconcile the financials but also the formats should you elect to load these files into your
system(s). Testing can take four to eight weeks to complete before going live, assuming no re-tests are
needed.
TOOLS FOR SUCCESS
We document the implementation status with proprietary tools, including a Project Plan, Implementation
Guide, Status Reports, and Risk/Issues Log. Together, these four tools will help ensure business units
are provided with the correct information, allowing sufficient time to execute on key tasks.
Our Implementation Project Plan monitors the progress of the implementation by outlining tasks,
responsible parties, and targeted completion dates, with a focus on the following key components:
• Plan Design
• Eligibility
• Management Reports
• Benefit Communications
• Finance
• Vendor Transition.

Louisiana Medicaid Page 51
© 2022 Caremark. All Rights Reserved.
We can incorporate executive summaries and dashboard reports, if desired, to provide the progress of
the implementation to your upper management. Project Plan updates occur in real-time throughout the
process and are shared with you on a weekly basis or more frequently if needed. In addition, the
Implementation Project Manager will provide an action log throughout the process detailing conversations
and any needed issue resolution.
We recommend a minimum of weekly meetings to review the current Implementation Project Plan and
Open Action Items. In addition, weekly meetings can occur at the executive level to provide a briefing on
implementation status and identified risks or issues.
• Demonstrate knowledge of services to be provided and effective strategies to achieve
objectives and effective service delivery.
CVS Health provides a best-in-class Medicaid pharmacy benefit manager. We currently support 27
managed Medicaid health plans, of which three are currently in Louisiana, with 135 unique lines of
business, representing more than 27 million Enrollees, of which nearly one million are in Louisiana,
across 37 states. Our Medicaid health plans cover children, nondisabled adults, pregnant women,
individuals with disabilities, and seniors eligible for both Medicaid and Medicare benefits. We’re always
evolving to meet changes in Medicaid program designs and regulations.
DIFFERENTIATORS
We recognize and understand the uniqueness of the Medicaid population. With more than half of
Medicaid members managing multiple conditions, the complexity of drug regimens is a major factor in
nonadherence. As the level of complexity goes up, the rate of adherence goes down. Mental illness,
which has a high incidence among this population, can affect a member’s ability to understand and/or
remember treatment regimens. Communication challenges also exist, as there is generally a low level of
health literacy, which can affect a member’s lifestyle choices. Language barriers, including lower literacy
levels and non-English-speaking members, may create challenges for effective communication between
members and providers. And limited mobility and/or access to transportation make it difficult for members
to get to the pharmacy to refill prescriptions or to providers for appropriate care. Among the Medicaid
population, disease states and utilization patterns may vary by state, but typically the top drug classes in
our book of business are antivirals, antiasthmatics, antipsychotics, antidiabetics, antidepressants,
anticonvulsants, analgesics, and antihyperlipidemics.
Improved clinical and cost outcomes are achieved through our sophisticated programs. Our Medicaid-
specific formulary and clinical programs are geared toward reducing fraud, waste, and abuse; improving
quality; managing costs; and improving outcomes. When state-mandated formularies or preferred drug
lists are required, we work with our clients to ensure compliance. We have robust specialty programs, and
our member engagement outreach efforts are designed to provide high-quality clinical care. Further, we
ensure members have access to the most cost-effective and clinically appropriate medication through
retail, specialty, and mail channels.
Our knowledge and expertise in managed Medicaid allow us to improve the per member per month
(PMPM) performance and operational efficiency of our managed Medicaid clients. We know plans are
most successful managing costs and meeting requirements when they have access to Medicaid experts
who are dedicated to helping them reach their goals. The clinical, account, and analytics experts in our
managed Medicaid segment provide detailed, consultative support to help our clients manage the
complexities of their business.

Louisiana Medicaid Page 52
© 2022 Caremark. All Rights Reserved.
• Encounter processing: We currently support Medicaid encounter submissions in 30 states. We
maintain a proprietary encounter processing system (EMS) that interfaces with our claims
adjudication engine to extract all adjudicated claims nightly. EMS prepares NCPDP encounter file
transactions for submission to states in the required formats.
• Formulary management: From closed formularies to therapeutic interchange programs, we have the
management expertise to develop the most appropriate level of formulary management. We
developed a Medicaid-specific formulary template to provide appropriate clinical and cost-effective
formulary management for managed Medicaid coverage providers.
• Fraud, waste, and abuse: We use comprehensive tools proven to solve fraud and abuse to
effectively control costs in relevant areas of a Medicaid environment.
• HEDIS scores: Through our comprehensive clinical solutions, we proactively engage members and
their prescribers with evidence-based clinical health improvement opportunities that support your
efforts to meet or exceed various HEDIS measures.
• NCQA accreditation: We support NCQA member connection standard MEM-4 by providing
members the information they need to understand and use their pharmacy benefits. This information
is provided through our website, Caremark.com, and over the phone.
• Network management: We offer multiple retail network options—including national, limited, and
custom—to provide optimal geographic coverage while allowing clients to manage their retail
pharmacy spending. We will develop a network with you that meets geo access requirements. We
have successfully implemented preferred network strategies in multiple states for our managed
Medicaid clients.
• PMPM performance: Our dedicated account teams provide ongoing analysis and consultation for a
variety of issues, including management of PMPM performance to meet client goals during
challenging budgetary times. We designed our PMPM trend forecasting tool specifically for health
plan support, given the need to evaluate opportunities at the therapeutic class level.
• Specialty medication management: Our specialty management capabilities address drug spending
under the pharmacy and medical benefits. We are the only specialty pharmacy that integrates rare
disease management—which is critical to controlling overall costs related to this small but high-cost
population.
• State requirements: We maintain a dedicated Medicaid regulatory compliance support team that
meets with client staff to discuss the regulations and Medicaid requirements in a state with regard to
PBM operations. They review new requirements to advise clients on the impact of our operations and
proactively identify new and proposed requirements and communicate them to clients.
• Utilization management: We create Medicaid-specific criteria for prior authorization, step therapy,
and quantity limit programs to control high utilization, abuse, and access to high-cost drugs. We also
provide exception processing and member-level overrides, upon request.
Customer feedback and our knowledge of industry trends have resulted in the following best practices
in our managed Medicaid segment.
CLINICAL SUPPORT
A clinical pharmacist with managed Medicaid experience is assigned to each account. Your clinical
pharmacist will provide comprehensive clinical solutions and online reporting to help you meet HEDIS
standards. They can also provide insight into how you can implement evidence-based interventions to
improve member health. Our clinical support can target health management programs for the Medicaid
population, including an emphasis on disease states/conditions such as HIV and behavioral health. You
can also take advantage of the managed Medicaid drug list that can save you time and money.
• Describe approach and strategy for project oversight and management.

Louisiana Medicaid Page 53
© 2022 Caremark. All Rights Reserved.
One of CVS Health’s key guiding principles is that we must execute against a single, integrated project
plan. Again, we will start with a best practice standard plan for this implementation and review it line by
line jointly to ensure that all activities are included. Each activity will ensure that we have tied in the
appropriate dependencies, that there is an appropriate amount of time for handoffs of work (examples:
deliver test results, review test results, provide feedback, clarify feedback, review final results, approve
results) to set the appropriate expectations. All tasks will be tied to one single, accountable owner rather
than groups of people or functional areas. The entire methodology around the plan is to ensure that it
clearly states who will be doing what through the entire implementation to ensure its success. Any need
to adjust these activities after they are agreed upon and baselined will be governed by a joint change
control process.
We use a comprehensive project plan that outlines each implementation task and includes defined
timelines and deliverables around documenting and approving client requirements in time to fully
configure and test prior to the plan effective date. Because of diverse client needs, our implementation
process is flexible enough to allow focus on the unique requirements of each client’s implementation. The
Implementation Project Manager and Account Team will ensure that our management and
implementation team work to deliver a successful implementation and will manage escalations as
needed.
Our project management methodology begins with an interrelated series of activities illustrated in the
Figure below; these activities enable and ultimately lead to:
• Development activities: Coordination of test and production eligibility files, review Enrollee
communications, build the benefit plan designs, and receipt of vendor transition files.
• Testing activities: unit, system integration, performance and user acceptance testing.
• Deployment activities: Coordination of Enrollee communications, receipt of final eligibility file,
Customer Care begins taking calls, and the website is available for Enrollees to access.
• Maintenance activities: Monitoring all post effective activities including Customer Care, Enrollee
communications, and ensuring accuracy of claim adjudication.

Louisiana Medicaid Page 54
© 2022 Caremark. All Rights Reserved.
Establishing and agreeing upon a formal escalation process early in the life of a project is key to its
success. As such we will work with the MCOs to establish a successful project escalation structure. In our
experience, the structure illustrated in the below Figure has proven effective.

Louisiana Medicaid Page 55
© 2022 Caremark. All Rights Reserved.
Each MCO’s dedicated Account Team will be involved with all aspects of Implementation to help ensure
seamless service and accountability. Each MCO’s Implementation Project Manager will be the single
point of contact and will lead and drive the implementation process from start to finish. Our proven
experience in health plan implementations has shown that the strategic advisory role of our dedicated
Implementation Project Manager is central to securing an efficient transition with minimal disruption.
CVS Health subject matter experts will be assigned to various project workstreams. We have a proven
process that tracks all the important milestones and timeframes, including standard templates for project
status reports. We propose holding weekly project status and issue management meetings with the LDH
team and each of the MCOs.
• Articulate the need for, and the ability to implement, a plan for continuous quality
improvement. This includes (but is not limited to) reviewing the quality of services provided
and staff productivity.
CVS Health and its integrated services including CVS Health is committed to continuous efforts to deliver
the best products and services to meet the needs of customers, including patients/plan members, clients,
and prescribers. CVS Health’s culture of continuous quality improvement is based on identifying
innovative solutions to pharmacy and health care delivery challenges. Our leaders must be the driving
force behind a high-performance culture created to help ensure the service and care provided to our
customers exceeds expectations. CVS Health colleagues embrace continuous quality improvement as
part of their everyday work responsibilities. Our front-line colleagues are encouraged to identify
opportunities to improve processes within their work environment and to bring forward larger ideas for
CVS Health to remain a market leader in pharmacy care innovation. It is this collaboration between
leaders and front-line staff that identifies opportunities to help improve quality and deliver the highest-level
quality of care and service to our customers.
Within each core business unit (BU), quality measures and goals are established and pursued to meet
the vision and mission of the individual BU, as well as the overall Program. These measures and goals
include:
• Alignment of governance, leadership, structures, and processes that drive results and drive
accountability throughout the organization
• Utilization of an organized, systematic approach to help improve and optimize quality, and to ensure
consistency of performance across service channels
• Provision of clear, concise messages to members and clients about our commitment to quality and
how we operationalize it to meet their needs and goals
• Development and sharing of organization-wide, best tools, practices, and methodologies to optimize
process-driven results
• Alignment of actions and measurements with CVS Health strategic imperatives and business
initiatives
• Alignment of/coordination between specific BU performance improvement initiatives based upon
recommendations from the Executive Leadership Team (ELT)
CVS Health PBM Services specifically strives for continuous quality improvement in the following areas:
• Medication (Drug Therapy) Management – safe, effective, and appropriate use of medications to
help increase adherence and deliver improved health outcomes.
• Operations Excellence – continuous high-quality execution in PBM and pharmacy processes and
human performance.
• Value and Affordability – process improvements that directly impact the cost to deliver quality
services to our customers.

Louisiana Medicaid Page 56
© 2022 Caremark. All Rights Reserved.
• Client and Member Satisfaction – identification of opportunities to measure and improve key
stakeholder experiences
QUALITY AT CVS HEALTH
The Program scope covers areas within CVS Health, including, but not limited to, CVS Health
®
Mail
Service Pharmacy, Customer Care, CVS Specialty
®
Pharmacy, Client/Account Management Services,
Drug Therapy Management, Health Call Center, Medicare Part D, Clinical and Professional Services, and
Accordant
®
.
Specifically, CVS Health provides quality service and care to our customers by utilizing consistent quality
improvement methodologies, cross departmental communication, and cross functional representation on
projects. CVS Health employs various evidence-based quality tools and methodologies (e.g., Lean Six
Sigma) to support continuous quality improvement. To evaluate the effectiveness of processes and
services:
• Key quality indicators are identified
• Data are collected
• Quantifiable performance metrics and goals are defined
• Baseline measurements and reporting timelines are established
For these performance goal(s), re-measurements are taken at established time frames (e.g., quarterly),
and if a measurement indicates a meaningful variation from the performance goal(s), the data are
analyzed; a root-cause matrix is completed; and a process improvement is identified, developed and
implemented, as needed. The new and revised processes are then monitored for effectiveness and
updated to maintain new performance levels. Ineffective process improvements are evaluated and
revised accordingly. Periodic re-measurement of performance metrics continues as long as necessary to
ensure defined goals are maintained.
PBM QUALITY SERVICES COMMITTEE (MAIL PHARMACY OPERATIONS,
SPECIALTY PHARMACY OPERATIONS, AND CUSTOMER CARE)
• Provides an annual report to the Quality Management Committee (QMC) on the effectiveness of the
Operations Quality management program
• Accurately tracks and reports on non-conformances for Mail and Specialty Operations and Clinical
Operations
• Provides ongoing analysis of non-conformance root causes
• Directly links into the various processes within the business for ongoing process improvement
initiatives
• Reviews credible safety literature, at least annually, for recommendations and application of best
practices regarding medication safety, risk-reduction tools, and error-prevention strategies
• Performs call monitoring to ensure effective, courteous, and accurate communication to members
regarding medications and pharmacy services
• Provides call mentoring to ensure appropriate communication to prescribers
CLINICAL QUALITY COMMITTEE (CQC)
• Oversee the clinical quality measurement/improvement activities of PBM clinical programs and
provide regular reports to the CMO concerning those activities
• Track ongoing accreditation activities and review indicators associated with various programs to
include, but not limited to, NCQA, URAC, and Medicare Part D
• Review the DTM Program quality indicators associated with the program

Louisiana Medicaid Page 57
© 2022 Caremark. All Rights Reserved.
• Oversee the annual review and update of clinical policies and other documents such as the UM
Program Description, Annual UM Program Evaluation and the CQC Charter
• Review quality dashboard results on a quarterly basis and provide an annual review to the QMC of
the effectiveness of the PBM’s clinical quality programs
• Provide oversight and monitor performance of UM programs, appeals, and Medicare Part D Quality,
and general clinical consistency by way of the following subgroups:
− UM Subgroup: Provide reporting of UM program activities, including operational metrics, audit
metrics, UM Annual Program Description and UM Annual Program Evaluation, and applicable
policies and procedures
− Vendor Subgroup: Manage all activities related to required quality oversight for Independent
Review Organization (IRO) vendors and internal clinicians and medical directors including the
quality of clinical appeal decisions, operational metrics, and relevant policies and procedures.
Subgroup also collaborates with internal Vendor Audits and Procurement regarding effective use
of external IRO vendors
− Medicare Part D Quality Subgroup: Monitor clinical outcomes, both effectiveness and quality, of
key enterprise clinical programs (e.g., MTM, concurrent and retroactive DUR) for CVS Health
Medicare Part D Enrollees. Subgroup also performs oversight of these clinical programs for
compliance with Centers for Medicare & Medicaid (CMS) regulations and guidance
− Clinical Consistency Committee: Evaluate and recommend the primary clinical guidelines to be
used as references across the enterprise in clinical communications and programs using an
analytical framework to ensure reproducibility as well as consistent clinical messages
ACCREDITATION
As a component of the Program, CVS Health monitors its compliance with various accreditation standards
that either directly or indirectly impact business operations. These include, but are not limited to, National
Committee for Quality Assurance (NCQA), URAC, Joint Commission, Drug Distributor Accreditation
(formerly VAWD), and Digital Pharmacy Accreditation (formerly VIPPS). If gaps are identified in processes
relative to standards, recommendations are made and plans are created and implemented to achieve full
compliance.
QUALITY MANAGEMENT PROCESS
LEAN SIX SIGMA
Colleagues are trained on continuous quality improvement methodologies, where applicable. One such
training program focuses on Lean Six Sigma. This training and mentoring program emphasizes the
following topics:
• Reduction/elimination of defects and/or waste from a process
• Timely flow of a process
• Reduction of variation using statistical tools
• Ongoing process control and continuous process improvement
• Yielding of dramatic results for the organization
• Define, Measure, Analyze, Improve, Control (DMAIC) model
Colleagues utilize the skills learned when leading and/or participating in improvement initiatives. There
are Six Sigma-certified Master Black Belts, Black Belts, and Green Belts available within CVS Health to
provide support for newly trained colleagues. Additionally, these Six Sigma-certified individuals are
utilized to broaden the skill depth of various business units when an opportunity for improvement has
been identified and an initiative is launched, including appropriate identification of metrics, data, and
more.

Louisiana Medicaid Page 58
© 2022 Caremark. All Rights Reserved.
TOTAL QUALITY MANAGEMENT (TQM) - QUALITY IMPROVEMENT
METHODOLOGIES
There are various process improvement methodologies that we utilize to support the quality framework
essential to building and re-enforcing a culture of continuous quality improvement. TQM emphasizes the
DMAIC process as a framework for identifying and investigating areas of the PBM for process/outcome
improvements. Teams using TQM frequently collaborate with and borrow techniques from the staff
trained in Lean Six Sigma.
REPORTING
The final component of the Program framework is the ongoing measurement and tracking of key
performance metrics/indicators. To ensure continuous quality, the enterprise has identified measurable
and data-driven key indicators. CVS Health uses this quantifiable data to identify significant quality
improvement opportunities and to design necessary corrective action plans.
A data-driven approach is also used to measure the effectiveness of these initiatives on business
practices and outcomes. Effectiveness is benchmarked against internal data (e.g., set quality goals and
year-over-year comparisons) and external performance data (e.g., URAC annual measures reporting)
where available. A data management program is in place to ensure the integrity of the key quality metrics
prior to the collection and analysis of work processes and subsequent evaluation of identified
performance initiatives.
In addition, CVS Health measures performance through other modalities, including satisfaction surveys,
consultant feedback, service warranties and performance related to client performance guarantees.
Information is tracked, analyzed, and utilized to identify gaps and opportunities for improvement for the
development of performance/quality improvement initiatives. Results of these activities are communicated
to relevant staff through the QMC.
• Demonstrate an understanding of and ability to implement data collection, as needed.
Data is derived from multiple sources depending on the program. In addition to pharmacy claims, data
may be self-reported by the patient, captured and reported by the CareTeam, or provided to us by the
medical vendor.
PATIENT REPORTED
Patient reported data can be captured through our specialty digital communication tools. This can also be
captured through our patient engagement points that happen as part of our standard specialty fill process,
through CVS Specialty Pharmacy, as well as when patients are engaged by the Accordant nurse team.
CLINICAL PROGRAM CAPTURE
We collect outcomes as part of our clinical program engagement with the prescriber. One example of this
is when we obtain lab value/results as part of the Specialty Guideline Management program and the
clinical review of a drug within the prior authorization process.
MEDICAL DATA

Louisiana Medicaid Page 59
© 2022 Caremark. All Rights Reserved.
We can often determine certain outcomes based on the prescription claims and history of the patient. For
example, if we see the start of a secondary treatment option it can indicate that the primary therapy did
not provide the overall intended outcome.
INTEGRATION AND REPORTING
Medical (ICD-10) data elements are captured and stored in the CVS Health Data Warehouse and our
fully-integrated technology system. This data streamlines processes because evaluations and outcomes
analysis can be made electronically, not requiring manual intervention. This data is also available to
clients for on demand reporting using our web-enabled reporting tool, RxNavigator.
Our RxClaim suite of systems offers a comprehensive set of automated reports that provide key financial
and utilization statistics essential to analyzing your pharmacy benefit program. Example reports include:
• Drug usage;
• Management activity;
• Enrollee utilization; and
• Pharmacy providers.
Unlike many pharmacy benefit managers, we use a hierarchy to set up eligibility. .
Custom Reporting
In addition to automated reports, our claims processing suite of systems has direct interface with our
proprietary RxNavigator reporting tool, which lets you manipulate your mail, retail, and specialty
prescription claims data and design custom reports with hundreds of variables. RxNavigator provides
secure access to pharmacy claims data using a Web browser, software upgrades are transparent to the
user, and no special software is needed to access the program. RxNavigator is user-friendly, allowing
flexible formatting and interactive dashboard capabilities.
DATA WAREHOUSING AND DECISION SUPPORT
Our Analytic Consultants and your designated representatives will have access to our Enterprise Data
Warehouse (EDW) repository. The EDW facilitates storage, linkage, and rapid retrieval of prescription
information and other health data and advanced tools, such as statistical analysis system software, which
allows large amounts of data to be accessed faster than ever before. While traditional reporting gives the
user a historical perspective, we provide intelligent reporting—reports with built-in interactive features that
enable users to manipulate data with future projections and understand how to influence and shape those
developments.
Our data warehousing technology employs a combination of proprietary and third-party-developed
software systems in a client/server environment. This system provides access to ad hoc queries and
reports (e.g., clinical, administrative, financial). Highlights of our data warehousing systems include:
• More than 220,000 pharmacy entities with name, address, and classification information;
• Multiple therapeutic classification systems;
• Online data resources that currently include nearly 16 million drug pricing records with historical
information spanning more than seven years;
• Oracle, Teradata and Hadoop
• Proprietary enhancement data sets.
Coordinating Data with MCOs
CVS Health works together with MCOs to coordinate care for their Enrollees through detailed activity
reporting, data integration and coordination of clinical services, where appropriate. We have accrued vast
experience working directly with medical health plans and payors to coordinate patient care as part of our

Louisiana Medicaid Page 60
© 2022 Caremark. All Rights Reserved.
focused campaign to connect and integrate care for Enrollees. We will provide full pharmacy claims data
and pharmacy insight reports to LDH and MCOs, and we offer clients a number of medication adherence
and care improvement products such as Pharmacy Advisor®, Transform Diabetes Care and Enrollee
targeting. These programs are designed to complement programs offered by a Enrollee’s medical
provider.
Our programs support providers by helping high-risk Enrollees address a multitude of drug-related
problems in an effort to improve overall health outcomes. We think long-term by continuing to work with
Enrollees post-hospital discharge to help prevent hospital readmission. All of these targeted efforts with
Enrollees are communicated to the provider and care managers to facilitate coordinated care.
ENROLLEE-LEVEL ACTIVITY REPORTING
We are committed to supporting LDH and MCOs through fact-based decision making, which is why we’ve
developed key clinical reporting tools that provide LDH and MCOs access to the information and insight
LDH and MCOs need to better understand and slow the growth of drug spending. Our clinical
management reports provide timely summary information, derived from the system’s detail-level data, to
answer management and operational questions more completely and facilitate decision-making
processes.
We have developed Enrollee-level activity data files in order to better coordinate with LDH’s and MCOs’
care management teams. These files arm the MCOs’ care manager with Enrollee-specific interventions,
based on the Enrollee’s most current treatment scenario.
The Adherence Activity Report provides detailed tangible measures of adherence such as persistency
curves, first-fill drop-off rates, medication possession ratio, and optimal adherence rates. The report was
designed to provide additional detailed adherence metrics within several commonly utilized therapeutic
classes.
DATA INTEGRATION
We coordinate with our clients’ disease management programs to help improve Enrollee identification and
predictive modeling to help boost engagement through targeted outreach. For example, we can send the
MCO biweekly first-fill maintenance reports. Also, our online reporting tool, RxNavigator, can be used by
the MCO to access patient-specific pharmacy data in near real-time to help optimize treatment plans,
including identifying and addressing gaps in care.
We currently have an integrated, enterprise data warehouse that integrates both medical and pharmacy
claims, and this integrated data set can be used across a number of programs that provide a longitudinal
view of Enrollee’s medical and pharmacy history.
Examples of how we have integrated this data include:
• Assessment of opportunities to better manage drugs that are delivered through both the medical and
pharmacy benefit, including support for rebates on medical specialty pharmacy, medical claims
repricing, site-of-care alignment, integrated prior authorization programs between medical and
pharmacy benefits, and drug benefit alignment. Uses include opportunity assessment and sizing,
program operations, and ongoing reporting and tracking.
• Collaboration with clients on scientific investigations into topics of interest such as total medical cost
for non-adherent populations as well as the appropriate use of medications with black-box warnings
in their population 65+ years of age
• Evaluation of the impact of an intervention such as a pharmacy benefit design change on the future
total cost of care (pharmacy and medical care costs)
• Integration of medical claims history as part of ‘smart coding/smart edits’ capability for prior
authorization programs. With smart PA, a prescription is submitted directly to the pharmacy. The
system reviews medical, lab and pharmacy data (provided by the client on a regular basis) to answer

Louisiana Medicaid Page 61
© 2022 Caremark. All Rights Reserved.
the clinical criteria. If met, the request is approved and drug dispensed with no Enrollee or physician
disruption.
CLINICAL SERVICE COORDINATION
Several clinical solutions utilize a collaborative case management approach that has proven successful in
effectively coordinating care and prevention with our MCO clients.
Our clinical pharmacists will work collaboratively with LDH and MCOs, their care coordination/case
management departments, and physicians to coordinate care for high-risk Enrollees. Through programs
such as closing gaps in medication therapy, Safety and Monitoring, and Retrospective DUR, we
communicate with both primary care physicians and case managers regarding pertinent Enrollee-specific
health care opportunities. These activities prompt physicians to act upon relevant information, while
looping in the case manager to update the Enrollee’s care plan and avoid duplicative efforts.
• Demonstrate an understanding of fiduciary duty, and knowledge of all applicable Louisiana
legislative requirements.
CVS Health will accept limited fiduciary responsibility for the purpose of adjudicating claims and
processing appeals related to prescription drug benefits provided by client.
Serving the Medicare and Medicaid markets is one of our corporate priorities. We have invested heavily
in both the infrastructure and personnel required to effectively serve the needs of health plans in the
complex and evolving government programs arena, and we will continue such investments to support
clients’ success.
The Government Services organization includes Regulatory Affairs, Client Advisors, and Operations
teams. Responsibilities include working closely with our Government Affairs team to influence CMS and
state policy decisions; reviewing, interpreting, communicating, and implementing new regulations; as
aligning our programs with quality measures; monitoring client performance; and driving improvement
initiatives.
Government Services Regulatory Affairs serves as the single source for all regulatory research and is
supported by both internal and external legal counsel when necessary. When regulatory issues become
known, the team works with the affected operational areas for implementation, including project
management and policy and procedures support. Government Services staff participate in PCMA and
NCPDP workgroups and coordinate with the Medicaid Health Plans of America and the Association for
Community Affiliated Plans.
During initial conversations related to implementation, the Government Services Medicaid Client Advisor
and Implementation Manager will meet with you to discuss the regulations and Medicaid requirements in
a particular state as they relate to PBM operations. Ongoing, Government Services and our legal team
will review new requirements to advise you on the impact to our operations. We will also proactively
identify new and proposed requirements and communicate them to you.
Government Services Regulatory Affairs will take the lead on developing regulatory crosswalks for the
Medicaid requirements in the dual demonstrations. We understand that state Medicaid agencies will have
significant oversight in the dual demonstrations, and we will build from the relationships we have with our
current clients, many of which participate.
• Define its functional approach in providing the services.

Louisiana Medicaid Page 62
© 2022 Caremark. All Rights Reserved.
CVS Health has extensive experience with applying state Medicaid uniform preferred drug lists (PDLs)
accurately and timely. Over half of the states where we have Medicaid MCO clients have state required
PDLs. We have experience applying state required benefit designs in the following states: Arizona,
Arkansas, Delaware, Florida, Illinois, Iowa, Kansas, Louisiana, Massachusetts, Michigan, Minnesota,
Mississippi, Nebraska, New Hampshire, Ohio, Pennsylvania, Rhode Island, Texas, Virginia and
Washington.
We routinely meet and exceed 95% PDL adherence in these states and will do so in Louisiana.
OUR APPROACH TO IMPLEMENTING BENEFIT CHANGES
CVS Health will provide LDH and the five MCOs with consistent, ongoing support regarding benefit
design changes by assigning a Benefit Relationship Manager (BRM) to your dedicated CVS Health
Service Team. The BRM will work to help make sure all benefit design changes are made on a timely
basis. The BRM also helps ensure quality delivered through - among other things - extensive plan change
testing.
When LDH provides notice with a benefit change, we will facilitate a requirements analysis documentation
meeting and draft a Requirements Analysis Document (RAD) subject to approval. We will provide LDH
and/or the MCOs with the tools to request benefit changes. We provide two routes for requesting benefit
changes. First, LDH and/or the MCOscan send a written request to your assigned BRM who completes a
benefit change request and forwards it to the Client Benefit department to input the change. We can also
provide LDH and/or the MCOs access to Salesforce.com for you to submit the request directly. This will
be a Single Sign On link available via Client Care Access (CCA), and the link will display as “CLIENT
CENTER”.
We use Salesforce.com to track and report benefit changes to track and report benefit changes to our
clients. This state-of-the-art Customer Relationship Management (CRM) tool enables us to track end-to-
end benefit changes and offers real-time monitoring. This technology enables you to keep track of the
status of its benefit changes. After all appropriate quality checks have been executed, we will send
confirmation to LDH and/or the MCOs confirming the change has been completed.
Once the Client Benefit department receives the change request, the benefits coding team will
immediately implement the change to ensure that the change is completed with one business day. If the
Benefits team identifies that more time is needed, they will provide the information related to an extension
to the CVS Health Account Director detailed to each
MCO. The Account Director will notify and request
permission to extend the implementation timeframe.
Extended timeframes may be needed when there are
complex clinical criteria for coding and testing; this may
be discussed and agreed upon as needed. The initial
implementation accuracy for go-live is at 100%. The maintenance of business plan changes
accuracy is at 99%.
The following is the process for benefit set-up and changes:
• LDH or the MCOs submits a benefit change request to CVS Health
• The Benefits team codes the change in a pre-production environment
• The Benefits team conducts testing using mock claims
• The BRM reviews the results with LDH and/or the MCOs.
• The approved benefit change coding is promoted to production
BENEFITS TESTING
In the past 12 months, CVS Health has
processed over 100,000 benefit change
requests with an average of 99%
accuracy.

Louisiana Medicaid Page 63
© 2022 Caremark. All Rights Reserved.
CVS Health tests benefits set up in a production-like environment that will include LDH and/or the MCO
Enrollee information for the greatest accuracy in identifying issues. After we code the benefit, we
conduct a detailed testing protocol to ensure 100% accuracy prior to production. LDH will have
complete access to review and conduct your own testing through the Client Test Environment (CTE)
portal. We find that this testing transparency has led to collaboratively identifying issues with initial
requirements gathering in addition to coding. The below table 1 details CVS Health’s testing protocol.
CVS Health Benefits Set Up Testing Protocol
Software
Quality
Assurance
Create test strategies and plans to help ensure software changes will
undergo comprehensive testing
Create test scenarios that map to each requirement within functional
specifications document
Benefit Plan
Testing
Review and create test scenarios that will map to requirement within the
Client Requirements Document (CRD)
Quality review of the testing encompasses the review of each unique
component CRD before promoting into production
Requirements: PDL, clinical criteria, administrative edits, pricing/network
and non-adjudication items
Benefit plans are tested by functional area based on plan set up and
components
Query
Validation
Predefined queries will be run in both a production-like and a production
environment to compare benefits coded vs. expected results, as
documented in CRD
The test results are reviewed with the benefits coding team to help ensure
that all discrepancies are addressed or validated with the client
Client
Implementation
Testing
Assesses real-time test scenarios focused on Enrollee experiences in a
production-like environment and validates their benefits coded and
compares the results with client requirements
Test results are reviewed and shared with business partners and the client
Client Testing
Clients are provided access to the CTE, which is a production-like
environment to perform their own testing with their Enrollees and benefit
plans
Clients can work with their Account Managers to obtain access to this
environment. Clients also may coordinate with their Account Managers to
receive additional training on CTE and the claim adjudication application.
If issues or errors arise, we take the following steps to quickly address and resolve:
• Proactive and Early Reviews - Live claim reviews are conducted beginning midnight of the effective
date of implementation. These live claim reviews continue at an established frequency throughout the
first few days and then taper-off over the next couple weeks until we both concur that no further
review at this level is needed.
• Prompt Prioritization - Errors are prioritized so that the corrections are updated in the system as
quickly as possible. Assessments are then made to determine if the error resulted in rejected claims.
If so, pharmacies are contacted to reprocess the claim and the Enrollee is contacted advising their
prescription is ready for pick up. If the error resulted in paid claims, but incorrectly paid, then a

Louisiana Medicaid Page 64
© 2022 Caremark. All Rights Reserved.
request is submitted to our Finance department to conduct the impact analysis and determine the
financial reconciliation needed.
• Financial Reconciliation Process - Once an error is identified and corrected in the system, the
issue is then sent to our Finance team for resolution and financial reconciliation of the incorrectly
processed claim(s). The Finance team researches the reported issue and confirms that the
appropriate corrections have been made in the system. The team then queries and analyzes claims
for the identified timeframe to determine the financial impact to the affected parties (e.g., Enrollee,
client, etc.) and then calculates any adjustments needed to make all parties whole for the impacted
transaction and initiates financial restitutions.
• Root Cause Analysis (RCA) - Benefits coding defects are assigned to an Advisor level resource to
perform and document the root cause of the defect and identify the defect prevention method (DPM).
Based on the RCA and DPM, the issues are fixed so they are not repeated again. Standard Test
Beds are updated accordingly to test for these defects going forward.
CVS Health’s Continuous Testing Processes
CVS Health uses sophisticated algorithms and real-time claims surveillance to automatically identify
benefits administration issues. These rule-based and machine-learning algorithms detect potential issues
with benefit coding during near real-time claims adjudication. Our claims surveillance process runs
multiple times a day. Because of the near real-time reporting, we are able to conduct rapid response
reviews of aberrant claims adjudication. If an actual issue is identified, the Claims Manager will notify LDH
and/or the MCO, and the benefits set up will be corrected within one business day.
We will document any benefit coding errors that resulted in the accuracy of implementing and maintaining
the PDL. We will report PDL adherence percentage to LDH on a monthly basis. The LDH-assigned Chief
Operational Officer will attest to the accuracy of the measurement. If the accuracy rate falls below 95%,
we will initiate a root cause analysis (described above) immediately to determine if the inaccuracy was
due to unusual circumstances or whether there is a systemic issue that must be corrected.
During its continuous testing and surveillance, CVS Health may identify opportunities for policy changes
that could benefit LDH and reduce provider administrative burden. When potential opportunities are
identified, we will conduct an analysis of the potential impact on providers, Enrollees, MCOs, and LDH to
ensure the change does not adversely impact any group, provides a measurable benefit such as
administrative simplification, and will not inadvertently compromise the administration of the LDH
pharmacy program. Opportunities for change will be presented to LDH at least quarterly.
Encounter Data
Following adjudication, claims are stored in the RxClaim platform. On a weekly basis, or more frequently if
needed, CVS Health will provide LDH (or designee) a full adjudicated claim encounter file. Whenever
claims are adjusted, the encounter files will be updated to reflect the adjustments. This encounter data file
will be designed to meet LDH specifications and can be altered to meet LDH’ changing needs. Any
changes to the encounter file will be implemented within 30 days of after LDH notifies CVS Health of a
change.
• Define its functional approach in identifying the tasks necessary to meet requirements.
We have implemented thousands of clients and structured the implementation process around proven
project management tools and methodology. We use a comprehensive project plan that outlines each

Louisiana Medicaid Page 65
© 2022 Caremark. All Rights Reserved.
implementation task and includes defined timelines and deliverables around documenting and approving
client requirements in time to fully configure and test prior to the plan effective date. Because of diverse
client needs, our implementation process is flexible enough to allow focus on the unique requirements of
each client’s implementation. The Implementation Project Manager and Account Team will ensure that
our management and implementation team work to deliver a successful implementation and will intervene
if necessary.
We currently support Medicaid encounter submissions in 37 states, including DC. Our proprietary system
prepares NCPDP encounter file transactions for submission to the states in the required formats. We also
receive response files from the state that identify rejected encounters and the corresponding rejection
codes. We can correct rejected encounters and resubmit them based on a LDH or the five MCOs agreed-
upon process. We also provide a reporting package that allows for health plan monitoring of the
delegated encounter function.
WORKING WITH STATES
Because our clients are the contract holders with state agencies, we typically have limited direct
involvement with the states. In a few instances, we had the opportunity to work directly with a state,
include California, New York, and South Carolina.
HISTORY AND EXPERIENCE
We have been processing encounter data for our clients that delegate this function to us since the
inception of our Medicaid business. We have successfully submitted encounters on all iterations of
NCPDP file format, and we validate each file in accordance with the individual state and/or CMS
requirements. Additional charges may apply for any custom formatting. We will work with LDH or the five
MCOs to define the frequency of file submissions and align all reporting, operational processes, and
tracking with state and/or CMS submission requirements.
IMPLEMENTATION TESTING
Encounter file testing is included in new client implementations if LDH or the five MCOs delegates the
encounter function to CVS Health and if the state has a testing environment available. We may need 120
days to implement testing if we have not worked with the state on encounter files previously.
We will establish file timeline dates and frequency with LDH or the five MCOs prior to implementation. In
all cases, we use state requirements as a guide for timeliness of submissions and resubmissions.
ENCOUNTER STATISTICS
Encounter Accuracy
Our encounter accuracy rate for Medicaid clients has been above 99.0%.
Encounter Data Acceptance and Rejection
Our encounter data acceptance/rejection rate across all of our Medicaid clients has been 98.1%.
Quality Reports
Across our clients and states, we average over 97% initial acceptance. We work with our clients and
internal partners to drive final rejection rates to under 1% within our control (excludes retro-eligibility
issues and value-added services).

Louisiana Medicaid Page 66
© 2022 Caremark. All Rights Reserved.
• Describe the approach to Project Management and Quality Assurance.
Please refer to the response above regarding CVS Health’s approach to Project Management during
implementation and through the life of the contract, as well as our Continuous Quality Assurance Program
that is utilized in all facets of our PBM service model.
• Provide a proposed Project Work Plan that reflects the approach and Agile project
management methodology, tasks and services to be performed, deliverables, timetables, and
staffing.
Our implementation process is aligned with LDH’s complex pharmacy benefit management needs.
Subject matter experts are assigned, and implementations managed based on a detailed project plan and
proven systems used to track timeframes and critical milestones.
For context, an illustrative high-level implementation timeline is provided below in Figure 4. This timeline
represents workstreams associated with a wide variety of CVS Health PBM implementations; this timeline
– and the underlying detailed implementation work plan – will be tailored to include the work streams
specific to LDH’s implementation.
Figure 4. High-Level Model Implementation Timeline
The detailed implementation work plan requested is included in Section IV Tab 4. Our work plan reflects
key work streams within our solution implementation, including:
• Plan Design
• Eligibility
• Management Reports
• Enrollee Communications
Business Area Month 1 Month 2 Month 3 Month 4 Month 5 Pre-Imp.
Discovery
(post-award tasks)
Define Account Structure (CAG)
Underwriting & Network Pricing
Vendor Transition
Clinical
Benefits
Specialty
Mail Ops
Eligibility
Consumer Driven Health***
Customer Care
Member Communication
Finance
Claims File
eBusiness
Encounter File
Integration Testing***
Effective
Date
Collect
Build
Collect Build
T
Collect Build
Collect Build Test
Collect Build Test
Collect Build Test
C Build
Build
Test
Collect Build Test
Collect
Build
Collect Build
Test
Collect Test
BCollect T
Deploy
Collect Build Test
Collect Build Test
Deploy
Deploy
Deploy
Deploy
Deploy
Deploy
Kick-Off Meeting
T Deploy
Deploy
C TestBuild
Collect Build Test Deploy

Louisiana Medicaid Page 67
© 2022 Caremark. All Rights Reserved.
• Clinical
• Finance
• Enrollee Data Transition
We wanted to note the following assumptions that went into the construction of this plan:
1. Given that this plan must be jointly owned by CVS Health and LDH, any scope changes post baseline
will require joint change control.
2. Requirements will be finalized and jointly signed off in an appropriate, mutually agreed upon
timeframe after project kickoff.
3. The plan accounts for appropriate client review and sign off of key documents (requirements, test
results, etc.).
4. The plan establishes a “pencils-down” period prior to go live to ensure that no late activities introduce
changes in the solution that could adversely impact solution deployment.
Please refer to Section V Tab 3 for the Sample Implementation Timeline
• Provide approach and detail the methodology/formula in defining the applicable transaction
fee.
Transaction fee was calculated by incorporating all costs associated with requested and required services
in this request for proposal. Transaction fee will apply to all paid claims
• Explain processes to implement in order to complete all tasks and phases of the project in a
timely manner, as outlined within Section 2. Scope of Work.
We are committed to providing you with a smooth and detail-focused implementation process. We are
aware that every health plan is unique in its service delivery infrastructure, lines of business, and
membership. Our long history of supporting health plans has given us the knowledge to understand
health plan complexities, forecast obstacles, and mitigate risks of member disruption during
implementation. You will benefit from our extensive experience implementing and supporting complex
and varied plan designs, including options such as CDH, accumulators, multiple deductibles, and more.
We have extensive experience in implementing clients with complex pharmacy benefits. These
implementations typically consist of the receipt of multiple eligibility feeds, the building of hundreds of
different benefit plan designs, and the delivery of complex communications to members. As a testament
to our configurable setups, in the 2020 welcome season we implemented 371 clients of which 280 were
new clients – serving 4.3 million members.
We handled more than 14,209 mailing projects, 1832 inbound member data transition files, and deployed
approximately 54,000 plan benefit changes. We had 387 million test claims processed. On January 7
th
,
the busiest day of the year, we processed over 11.3 million claims and a record 249.5 million claims in the
month of January. We are pleased to report our client satisfaction rating is 97%.
We use our claims processing system as the backbone of our primary operations for pharmacy benefit
administration and claims processing. This will enable a smooth transition for current Blue clients, as we
have great depth of experience with all of the functionality and architecture. In addition, we leverage
Artificial Intelligence and Machine Learning technologies to perform several levels of testing, to help
ensure all possible combinations of edits and criteria are correctly executed.
CRUCIAL STEPS FOR A SUCCESSFUL IMPLEMENTATION

Louisiana Medicaid Page 68
© 2022 Caremark. All Rights Reserved.
At the initial planning meeting, the Strategic Account Executive, Account Manager, Implementation
Program Manager, and your designated benefit personnel will meet to identify a comprehensive list of all
tasks and timeframes that need to be completed by each party. We believe that a successful
implementation hinges on the completion of each identified task. Based on our experience in
implementing clients, the following factors prove critical for a smooth implementation:
• Collaboration through the discovery process at the kick off meeting
− Open communication to determine and document shared terminology
− Obtain client requirements around plan design, hierarchy, reporting, etc. and help ensure these
are thoughtfully documented in the Client Requirements Document
− Define the timeline using the Project Plan and identify specific tasks needing client sign-off
− Proactively anticipate and document any obstacles that may occur by using the Issues/Risk log
• Experienced implementation professionals
− Matrix of subject matter experts (SMEs) matching your structure and SMEs
− Oversight of end-to-end certification testing and client test environment
− Establish responsibility on both sides for critical decisions
• Governance of the Process
− Follow our proven methodology for managing a successful implementation
− Establish escalation process for quick issue resolution for risk and issue resolution
− Agreed upon timeframes for thorough review and testing.
To align with your complex pharmacy benefit needs, the implementation process is very detailed. Subject
matter experts are assigned and all implementations are managed with a detailed project plan. We have
a proven process that tracks all of the important milestones and timeframes.
• Discover: Understanding your lines of business and priorities. Bring key decision makers to
meetings, provide all necessary information and data files and execute timely review and approval of
requirement documents to support the gathering process. Discuss the implementation guide which
provides a roadmap for the process. Document your requirements and provide our recommendations
on plan design, hierarchy, and reporting needs. Determine frequency of communications and
meetings
• Build: Continue attending weekly meetings and completing key client milestones as we execute
activities to implement your requirements
• Test: Support testing and quality assurance activities by continuing to attend weekly meetings,
providing timely approval of test results and supporting vendor collaboration.
• Deploy: Participate in final implementation activities involving preparation, coordination, and quality
checks driven by the CVS Health Implementation Manager leading up to and including the effective
date.
• Maintenance: Monitoring all post effective activities including Customer Care, member
communications, and ensuring accuracy of claim adjudication. Resolution of any identified gaps or
plan design elements from the plan effective date.
BENEFIT TESTING
Our unique and proprietary testing capabilities are key to minimizing operational impacts to plans during
an implementation. Key features include:

Louisiana Medicaid Page 69
© 2022 Caremark. All Rights Reserved.
All of our testing is conducted in a pre-production test environment, allowing for plan design changes as
needed until the expected outcome is reached. When test results are confirmed as meeting client
requirements, the plan design will be moved to our production environment. Client Benefits conducts
comprehensive testing using our proprietary automated testing tools that includes three steps: ingesting
requirements and generating test scenarios (test claims), execute test scenarios by adjudicating the
claims using the client benefit plan designs, and verifying/validating the results.
Generating Test Scenarios – During this step, client requirements are ingested into our test automation
tool, test claims are generated, along with requirements traceability matrix document, ensuring 100% of
the client benefit designs have corresponding test scenarios, and execute against the benefit plan design.
Any client specific or unique scenario can also be added to the test bed prior to execution. Typically, a
drug is tested from every category, including negative test scenarios like plan exclusions and non-
preferred drugs based on the client’s benefit and clinical design. While testing for coverage or regulatory
compliance, we will also include testing for pricing, quantity versus time, age limits, contingent
therapy/prior use exception, accumulations which includes deductible, out of pocket, and maximum
allowable benefit as well as specific section of test scenarios for regulatory requirements with expected
test results. Accumulation testing involves multi-step testing for each accumulation level, to help ensure
claims calculate correctly before the accumulation level, the crossover claim, and after the accumulation
level is reached.
Execute Testing – The second step requires Client Benefits to submit the test claims and adjudicate
against the benefit plans and compare the expected versus actual test results. In this step we compare,
using our automated test tool, test results with the client requirements to confirm that claims paid or

Louisiana Medicaid Page 70
© 2022 Caremark. All Rights Reserved.
rejected as expected. For rejected claims, we confirm the reject is valid, including the reject message. If
the reject is not related to drug exclusion, it is reviewed to determine if plan and/or macro modifications
are needed. If plan and/or macro modifications are made, retesting will occur to confirm changes provide
the valid drug coverage or exclusion outcomes before moving to the third step in the testing process.
Reviewing Results – The last step of the testing process is to review the test results with our Client and
confirm the intended outcomes are achieved. We demonstrate the test coverage, test conditions set up
and the test results which we compare against client requirements. When reviewing the outcomes, we
also confirm the member's copay is correct and the claim calculated as expected based on the contracted
prices. If we find any discrepancies during this step, we will identify what caused the issue, make any
required plan modifications, and process a new set of claims for review. All test cases and results are
reviewed and signed off before promoting the benefit plan into production.
CLIENT IMPLEMENTATION TESTING FOR CLIENTS
After benefit testing is completed in the pre-production environment, the client’s data is promoted to the
Client Test Environment (CTE), which is a production-like environment; to perform further testing that
includes production, eligibility, plan, utilization management rules, prior authorizations, and pricing. Test
claims or production claims can be used for testing. After the claims are processed, claim files are
produced which can be reconciled to financials and available to be loaded into client’s Data Warehouse.
Also, an invoice from our billing system will be generated for your review. You will have the ability to not
only reconcile the financials but also the formats should you elect to load these files into your system(s).
In addition, PDE files, Encounter files can also be generated and verified. Finally, member information
can be tested using our digital portal. Testing can take four to eight weeks to complete before going live.
This level of testing simulates for a member experience at point of sale and ensures 99% of the member
issues are addressed.
• Articulate the ability to develop and implement a Continuity of Operations Plan (COOP) in the
event of an emergency.
We conduct annual exercises to ensure our preparedness in the event of certain emergencies and/or
disruptions. We have experienced business interruptions as a result of power loss, network disruptions,
and severe weather, all of which have been handled successfully by our contingency plans. These
business workarounds include the use of facility generator power, transferring calls to other locations,
staff working from home, and other pre-planned strategies.
Please refer to Section V Tab 4 for CVS Health’s Business Continuity Plan.
• Refer to specific documents and reports that can be produced as a result of completing
tasks, to achieve the requested deliverables.
We execute the implementation process and document status with a suite of proprietary tools, including a
single integrated Project Plan, Implementation Guide, and Change - Risk, Actions, Issues and Decisions
(C-RAID) log. Collectively, this integrated suite of tools ensures LDH, your respective vendors, and CVS
Health business units are provided with complete, timely, and accurate information, allowing sufficient
time to execute key tasks.
Our Implementation Project Plan tracks the progress of the implementation by outlining tasks, responsible
parties (including LDH and your vendors), dependencies, and expected completion dates, with a focus on
all components required for implementation. With some examples, but not all inclusive, noted below:

Louisiana Medicaid Page 71
© 2022 Caremark. All Rights Reserved.
• Plan Design
• Eligibility
• Management Reports
• Member Communications
• Clinical
• Finance
• Member Data Transition.
We will incorporate executive summaries and dashboard reports, as desired, to provide you with progress
of the implementation to your senior management. Project Plan updates occur in real-time throughout the
process and are shared with you on a weekly basis or more frequently if needed. In addition, the
Implementation Project Manager will provide access to the project plan, client milestone report, and C-
RAID log throughout the process detailing plans, expectations, and follow up items to successfully
complete the implementation.
• Identify all assumptions and constraints for work plan tasks.
We wanted to note the following assumptions that went into the construction of this plan:
1) Given that this plan must be jointly owned by CVS Health and LDH, any scope changes post baseline
will require joint change control.
2) Requirements will be finalized and jointly signed off in an appropriate, mutually agreed upon
timeframe after project kickoff.
3) The plan accounts for appropriate client review and sign off of key documents (requirements, test
results, etc.).
4) The plan establishes a “pencils-down” period prior to go live to ensure that no late activities introduce
changes in the solution that could adversely impact solution deployment.
Please refer to Section V Tab 3 for the Sample Implementation Timeline
• Discuss what flexibility exists within the work plan to address unanticipated problems which
might develop during the contract period.

Louisiana Medicaid Page 72
© 2022 Caremark. All Rights Reserved.
Our account management approach is designed for flexibility and agility to detect and avoid escalated
issues through a single, centralized tracking system. Our single platform connects Account Managers with
IT, Operations, Sales, Government Affairs, and Retail and allows for early identification, effective
resolution, and reporting. We see evidence of this in our successful 2021 welcome season, where we
saw a 22% reduction in volume of total issues reported and 52% reduction in mean time to resolve
issues.
CAREMARK CSX CENTER OF EXCELLENCE
Our Caremark Service Excellence team, a cross functional group that oversees the issues management
process, instituting core operational discipline and leads the culture transformation. They create visibility
to trends and high priority issues; drive accountability; and ensure issue prevention through better
collaboration. This is comprised of leaders across account management, benefits, client services, data
operations, analytics, finance, IT, product, human resources, and Medicare operations that meets weekly
to address client and member issues. Our focus is to ensure that we address issues as they arise, so we
can align the right resources to resolve issues, do a thorough root cause analysis, and then take action.
RESOLVING YOUR INQUIRIES
The account team strives for same-day response time. If any issue cannot be resolved within two
business days, within one business day of receipt by the Account Manager, we will provide an estimated
time of resolution by electronic or verbal communication to the requestor. Depending on the complexity of
the inquiry, request, or concern, the Account Manager will escalate unresolved issues to a leader or the
appropriate area within our organization for consultation. The Account Manager will provide updates and
an estimated timing of issue resolution.
Each Account Manager has an assigned backup who can review your plan design and any custom or
unique needs. Our expectation is that the backup Account Manager is appropriately informed so they can
support your needs while your assigned contact is unavailable.
To stay closely connected with you and ahead of the constantly changing health care landscape, we
recommend several types of structured meetings throughout the year.
MONTHLY MEETINGS
Monthly meetings with your account team focus on executing on your initiatives. For these meetings, we
will engage internal subject matter experts who can present new products and services, as well as share
insights and recommendations to help you control costs, maintain high employee satisfaction, achieve
your health and wellness goals, and accomplish your business objectives. Common topics for discussion
at these monthly meetings include formulary, specialty management strategy, operational tools for
tracking and training, and regulatory support for topics such as retiree benefit options and ACA
compliance. We can also present dashboards that illustrate plan progress toward your goals. Dashboards
are updated on an ongoing basis, and your account team will work with you to determine meeting
frequency (e.g., monthly, quarterly) so you can have an executive summary overview of key operational
indicators. A sample is shown below.

Louisiana Medicaid Page 73
© 2022 Caremark. All Rights Reserved.
Our trend management tools, including RxInsights and RxNavigator, benchmark and forecast outcomes.
Our newest tool, Dynamic Trend Manager, analyzes real-time trend drivers, focusing on diabetes and
hyperinflation management. Your account team can share these and a variety of other ongoing strategies
during your meetings.
QUARTERLY MEETINGS
In addition to ongoing plan design management, we recommend quarterly meetings with your Strategic
Account Executive and other necessary parties based on topics for discussion. The team will present a
summary of financial and utilization trends as well as operational effectiveness. Along with colleagues
with analytical and clinical expertise, the account team can present analyses and models to help your
staff better assess cost savings, member satisfaction, and health improvement options.
ANNUAL MEETINGS
We will hold an annual review meeting to address the past year’s experience based on a plan
performance analysis. Your Strategic Account Executive and Clinical Advisor will work with your staff to
map out strategic objectives and goals for the following plan year. Discussion may include plan design
enhancements, cost-share adjustments, and clinical program recommendations to further manage costs,
improve health outcomes, and achieve any other LDH-specific goals.
We include a wide range of metrics during ongoing plan management meetings and annual reviews with
clients. Metrics vary by client but may include:
• Analyses and models related to cost savings, member satisfaction, and health improvement options;

Louisiana Medicaid Page 74
© 2022 Caremark. All Rights Reserved.
• Clinical program performance;
• Cost-share metrics;
• Operational effectiveness;
• Past year’s experience based on plan performance analysis;
• Plan design performance; and
• Summary of financial and utilization trends.
• Document procedures to protect the confidentiality of records in LDH databases, including
records in databases that may be transmitted electronically via e-mail or the Internet.
Our information security program provides the framework for the protection of information assets from
unauthorized disclosure, modification, or destruction through the development and dissemination of
policies, standards, procedures, guidelines, and information security awareness. Our program and
processes are in support of stringent industry standards, including HIPAA, NIST 800-53, ISO 27001, and
PCI-DSS. The controls and programs address the following aspects of our information security program.
• Our risk assessment process includes vulnerability scans of the internal and external network, PCI,
and Web applications, as well as penetration testing, wireless rogue testing, and vulnerability/patch
management.
• We maintain technical, administrative, and physical controls designed to enforce policies and detect
and prevent security risks. These include:
− Antivirus, anti-spam, and anti-spyware programs;
− Centrally managed and enforced workstation policies to reduce administrative access and
privileges, enforce password controls, mandate password-protected screen savers, and remove
access to USB and removable media ports;
− Enforcement of minimum security baselines;
− File system monitoring and integrity protection;
− Full disk encryption on all laptops and desktops;
− Mobile device management and security standards; and
− Patch management.
• Security awareness training is ongoing and offered in many ways through required job-specific
training. Our Compliance department tracks all training, including annual security awareness and
HIPAA privacy training. Additionally, security professionals receive ongoing training and obtain and
maintain their professional certifications as required.
• Web application security and developer training programs provide standards for new and existing
application development to include authentication, authorization, session management, data security,
secure coding practices, and secure Web server configuration following an established system
development life cycle process. All developers are required to complete annual software security
training.
• Our Security Operations Center performs network monitoring and alerting using network-based
controls to identify, quarantine, and prevent unauthorized access to network-based resources.
Additional controls used to restrict access to networks, systems, and applications include firewalls,
Internet content filtering, intrusion detection and prevention systems, data loss prevention, network
segmentation, and two-factor authentication for remote access.
• Our Third-Party Risk Management Program performs vendor risk assessments prior to contracting
with any outsourced service provider.

Louisiana Medicaid Page 75
© 2022 Caremark. All Rights Reserved.
ENCRYPTION POLICIES FOR DATA AT REST AND IN TRANSIT
Appropriate procedures and measures are in place to encrypt sensitive data transmitted over public
networks in conformance to the specifications of FIPS 140-2 and to encrypt PHI and PII at rest in
compliance with all applicable regulatory requirements and standards so that it cannot be accessed by
unauthorized persons.
CVS Health employs encryption technologies with minimum key lengths of 128-bits for symmetric
encryption and 1024-bits for asymmetric encryption. A documented policy for the management of the
encryption keys and associated processes adequate to protect the confidentiality and privacy of the keys
and passwords used as inputs to the encryption algorithm is in place.
Per the Payment Card Industry Data Security Standard (PCI-DSS), CVS Health encrypts all payment card
information in accordance with the requirements and current version of the regulation.
All organization laptops and desktops are encrypted using full disk encryption and are prohibited from
using removable media through the enforcement of technical controls. Removable media drives can be
enabled if there is a business justification for doing so. However, if an exception is granted, all removable
media must be encrypted through technical controls in accordance with the CVS Health encryption and
key management standard.
• Clearly outline the solution’s technical approach as it relates to a service-oriented
architecture. Proposer should describe how their solutions will utilize the State’s Enterprise
Service Bus and API Gateway components for all API or real time interfaces, or any
interactions with other EA or State technology components. Proposer should also describe
how their solution will integrate with the State’s Identity Access Management/Single Sign On
system for both internal and external users. The Proposer shall clearly identify any systems
or portions of systems outlined in the proposal, which are considered proprietary in nature.
CVS Health is able to integrate with the State’s service bus and API gateway component as needed. CVS
Health also has rich offerings of proprietary APIs covering most common PBM functions which they can
utilize. CVS will integrate with other source systems as needed.
We offer single sign-on (SSO) capability using SAML 2.0 technology. This time-saving process eliminates
the need for members to login twice and seamlessly integrates the member’s experience from the Client’s
benefits platform to the CVS Health PBM platform.
SSO uses the eligibility criteria sent from the Client to authenticate the member, allowing for a seamless
login experience. Members can also create a separate username and password, allowing them access to
Caremark.com and our mobile capabilities directly.
An SSO implementation requires development and testing by the client, as well as coordination between
the client and the Account Management team. Required parameters to be passed in the SSO payload are
member ID, first name, last name, date of birth, gender, carrier ID if a client has multiple carriers, and
CVS Health-assigned SSO requestor ID.
We also support SSO deep links, which allow members to land in a specific area of Caremark.com after
clicking on links such as Check Drug Cost & Coverage, Find Savings and Opportunities, Rx Savings
Report, Print Member ID Card, Secure Message Center, and Account Balance. We encourage clients to
provide deep links for members on their websites for ease of use.
As a recent enhancement to our mobile website, clients that have SSO capabilities on Caremark.com
now have this capability with the mobile site.

Louisiana Medicaid Page 76
© 2022 Caremark. All Rights Reserved.
LENGTH OF TIME FOR SETUP
A typical SSO project takes approximately 10-12 weeks. SSO projects require IT work from the Client and
CVS Health IT teams. The timeline is largely dependent on how quickly the client can build, test, and
deploy. Nonstandard SSO implementations will require additional time.
MINIMUM AND MAXIMUM USER ID LENGTH
We require user IDs to be seven to 24 characters long.
As the PBM for more than 50% of the State’s Medicaid Enrollees, we have systems, infrastructure
and staffing already in place to meet the program requirements. As a result, we provide the
smoothest, lowest-risk path to implementing LDH’s pharmacy benefit management model.
SYSTEMS
CVS Health has a robust suite of information systems that are already in use across hundreds of clients,
including all of our Louisiana Medicaid MCO clients. Our information systems and associated
infrastructure are architected to enable multiple concurrent implementations at minimal risk to all clients.
The core component of our information systems suite is RxClaim, our claims processing solution. We own
RxClaim’s source code, which enables us to make changes to the software based on client needs.
Moreover, RxClaim has been purposely built to be highly scalable and flexible; as such it can be
continuously enhanced to keep pace with client requirements and changes in state and federal laws and
rules. Finally, RxClaim already interfaces with e-prescribing networks such as Surescripts and with source
systems for prescriber, drug and other critical input data.
Other components of our information systems suite include a robust data warehouse and our
RxNavigator report management solution.
A high-level architectural diagram of our information systems suite, components of which vary depending
on the client implementation, is shown below:

Louisiana Medicaid Page 77
© 2022 Caremark. All Rights Reserved.
INFRASTRUCTURE
CVS Health has built a highly available and resilient infrastructure upon which it operates its information
systems and key business functions. Following are descriptions of key components of this infrastructure:
• We continuously invest in state-of-the-art operating platforms for our information systems. RxClaim is
hosted on IBM’s most advanced technology: Power8System model 880 hardware, 64-bit RISC.
Redundancy is built into every aspect of RxClaim. This includes primary and secondary processors
for production, a processor for development, and fully redundant disk storage systems.
• Our integrated claims adjudication data communications network ensures high availability, fault
tolerance and consistent quality of service by leveraging multiple compatible WAN/LAN architectures.
The WAN is comprised of an optimal mix of dedicated point-to-point private lines, multiprotocol layer
switching (MPLS) using traditional T-1 lines, and flexible WAN ethernet to provide greater access to
additional capacity. The LAN services are 1 Gb and 10 Gb ethernet on dedicated internal hardware to
isolate adjudication service from other traffic types. Our claims processing systems have average
uptimes over 99.9% annually.
• Our systems are hosted in redundant data centers supported by uninterruptible power supply (UPS)
and diesel-driven power generators to ensure continuous operation and exceptional business
continuity.
• Our information systems were architected “from the ground up” with scalability as a primary goal; as
such it can accommodate significant increases in processing requirements.
A high-level infrastructure diagram is provided below:

Louisiana Medicaid Page 78
© 2022 Caremark. All Rights Reserved.

Louisiana Medicaid Page 79
© 2022 Caremark. All Rights Reserved.
1.8.8 Detailed Scope Response
Describe its proposed approach to meeting each of the requirements below. The narrative
response should demonstrate clear understanding of all the requirements in each category. Any
requirement not clearly addressed in the response may negatively affect the Proposer’s scoring.
The Proposer should respond, at a minimum, to the following sections:
• Coordination with the MCOs: Describe the proposed approach to meet the requirements for
coordination with the MCOs included in Section 2.1.3, including detailed transition activities.
CVS Health works together with MCOs to coordinate care for their Enrollees through detailed activity
reporting, data integration and coordination of clinical services, where appropriate. We have accrued vast
experience working directly with medical health plans and payors to coordinate patient care as part of our
focused campaign to connect and integrate care for Enrollees. We will provide full pharmacy claims data
and pharmacy insight reports to LDH and MCOs, and we offer clients a number of medication adherence
and care improvement products such as Pharmacy Advisor®, Transform Diabetes Care and Enrollee
targeting. These programs are designed to complement programs offered by a Enrollee’s medical
provider.
Our programs support providers by helping high-risk Enrollees address a multitude of drug-related
problems in an effort to improve overall health outcomes. We think long-term by continuing to work with
Enrollees post-hospital discharge to help prevent hospital readmission. All of these targeted efforts with
Enrollees are communicated to the provider and care managers to facilitate coordinated care.
ENROLLEE-LEVEL ACTIVITY REPORTING
We are committed to supporting LDH and MCOs through fact-based decision making, which is why we’ve
developed key clinical reporting tools that provide LDH and MCOs access to the information and insight
LDH and MCOs need to better understand and slow the growth of drug spending. Our clinical
management reports provide timely summary information, derived from the system’s detail-level data, to
answer management and operational questions more completely and facilitate decision-making
processes.
We have developed Enrollee-level activity data files in order to better coordinate with LDH’s and MCOs’
care management teams. These files arm the MCOs’ care manager with Enrollee-specific interventions,
based on the Enrollee’s most current treatment scenario.
The Adherence Activity Report provides detailed tangible measures of adherence such as persistency
curves, first-fill drop-off rates, medication possession ratio, and optimal adherence rates. The report was
designed to provide additional detailed adherence metrics within several commonly utilized therapeutic
classes.
DATA INTEGRATION
We coordinate with our clients’ disease management programs to help improve Enrollee identification and
predictive modeling to help boost engagement through targeted outreach. For example, we can send the
MCO biweekly first-fill maintenance reports. Also, our online reporting tool, RxNavigator, can be used by
the MCO to access patient-specific pharmacy data in near real-time to help optimize treatment plans,
including identifying and addressing gaps in care.
We currently have an integrated, enterprise data warehouse that integrates both medical and pharmacy
claims, and this integrated data set can be used across a number of programs that provide a longitudinal
view of Enrollee’s medical and pharmacy history.
Examples of how we have integrated this data include:

Louisiana Medicaid Page 80
© 2022 Caremark. All Rights Reserved.
• Assessment of opportunities to better manage drugs that are delivered through both the medical and
pharmacy benefit, including support for rebates on medical specialty pharmacy, medical claims
repricing, site-of-care alignment, integrated prior authorization programs between medical and
pharmacy benefits, and drug benefit alignment. Uses include opportunity assessment and sizing,
program operations, and ongoing reporting and tracking.
• Collaboration with clients on scientific investigations into topics of interest such as total medical cost
for non-adherent populations as well as the appropriate use of medications with black-box warnings
in their population 65+ years of age
• Evaluation of the impact of an intervention such as a pharmacy benefit design change on the future
total cost of care (pharmacy and medical care costs)
• Integration of medical claims history as part of ‘smart coding/smart edits’ capability for prior
authorization programs. With smart PA, a prescription is submitted directly to the pharmacy. The
system reviews medical, lab and pharmacy data (provided by the client on a regular basis) to answer
the clinical criteria. If met, the request is approved and drug dispensed with no Enrollee or physician
disruption.
CLINICAL SERVICE COORDINATION
Several clinical solutions utilize a collaborative case management approach that has proven successful in
effectively coordinating care and prevention with our MCO clients.
Our clinical pharmacists will work collaboratively with LDH and MCOs, their care coordination/case
management departments, and physicians to coordinate care for high-risk Enrollees. Through programs
such as closing gaps in medication therapy, Safety and Monitoring, and Retrospective DUR, we
communicate with both primary care physicians and case managers regarding pertinent Enrollee-specific
health care opportunities. These activities prompt physicians to act upon relevant information, while
looping in the case manager to update the Enrollee’s care plan and avoid duplicative efforts.
DATA EXCHANGE INTERFACES
CVS Health can exchange data with LDH and other vendors utilizing LDH approved interface layouts,
including those for Enrollee eligibility and pharmacy enrollment. Our drug file will maintain compatibility
with the state-identified systems. CVS Health offers a detailed paid claims data file that is forwarded to
clients through electronic transmission in a 4,000-byte layout. The claim file provides clients with detailed
information on claims that are paid on behalf of Enrollees. Claim data files can be generated daily,
weekly, four times a month, or twice monthly, coinciding with the billing cycle, but can go out on a more
infrequent basis (i.e., quarterly, semiannually, or annually) if so desired.
The claim data file can integrate pharmacy utilization data with your medical benefit program data and/or
to extrapolate summary reports that highlight data at any level (e.g., specific drugs, Enrollees, groups).
The file layout and frequency for sending data files can be customized to suit LDH’s requirements. The
current data file format supports pharmacy claims exceptionally well and provides all of the necessary
information from a pharmacy claims perspective. For example, the claim data file contains the Basis of
Reimbursement Determination which would allow LDH to see which pricing value (e.g. MAC, FUL, U&C)
was used to determine the payment rate to the pharmacy and reject codes (e.g. NDC not covered or
duplicate claim). Although our system can accommodate your specific preference for the claim file layout,
we recommend that you use the current data file layout, which includes many of the NCPDP data fields.
Client Testing Environment
CVS Health can provide a designated Client Test Environment (CTE), which is a “production-like”
RxClaim environment for our clients to test with our adjudication (RxClaim) application. The CTE is
production-like for the applications needed during testing, and the IT code is deployed to the CTE
immediately after Production. CTE is a stand-alone environment, which includes the client hierarchy

Louisiana Medicaid Page 81
© 2022 Caremark. All Rights Reserved.
structure, and Enrollee information. The CTE environment for client testing is maintained to model and
test benefit design changes, including:
• Mass claim adjudication
• New benefit edits
• New pricing/reimbursement
The client-specific security setup is applied to this environment so that each client's data is secure and
can be viewed only by the client's users. Clients have the ability to perform testing with client-specific
eligibility, benefit changes, and its impacts through claims processing within four to eight weeks prior to
the deployment date. Access to CTE is available to a mutually agreed upon timeline with client and CVS
Health. We work with our clients to provide adequate time for testing to ensure quality and client
satisfaction. CVS Health maintains separate development, test, and production environments.
Operational data containing Confidential or Proprietary information is not used in test or development
environments.
CVS Health will engage the State directly to review test results for Louisiana specific changes and we will
review the changes and test results with the State prior to all major releases.
Testing Process
CVS Health uses a standard development lifecycle and testing philosophy to ensure quality processes.
We do not move to the next phase of client specific IT development requests without approvals from the
CVS Health Account Team. We employ the philosophy of “Test Early and Test Often,” with the belief that
when testing is actively maintained throughout a project, better quality results in the form of: clearer
requirements and schedules, reduced costs of defects, and minimized production defects. These testing
activities are accomplished through a combination of manual and automated processes throughout the
project and executed at all levels of testing.
User Acceptance Testing is performed as a final phase of testing by the end-users to ensure that the
product being delivered matches the requirements and expectations of those users. Any training
requirements are handled during this phase to ensure that the business is educated on all changes and
functionality being delivered.
TRANSITION PLAN
In the event that our contract is not renewed, CVS Health will develop a Transition/Turnover Plan
(referred to as “Turnover Plan”) and provide it to LDH at least one hundred and eighty days (180) prior to
the transition to a new vendor/vendor(s). The Turnover plan will include details on how and when we
propose to transition data files, documentation and other materials back to the State or their new vendor. .
Our plan will include a list of the files we believe are necessary for full transition to another vendor and
our proposed timeline for transition activities.
The proposed outline for the turnover plan is as follows:
1. Overview and Objectives
2. Overall contract termination timeline and post contract commitments
3. Turnover/Transition Team, Roles and Responsibilities
4. Transition Tasks, Activities and Schedule
5. Initial Risks and Mitigation Strategies
6. Communication Plan – including who we will communicate with and the frequency of communication
as agreed upon with LDH
7. Data File Transfer – Proposed types and schedule - including Testing as agreed with LDH and or new
vendor

Louisiana Medicaid Page 82
© 2022 Caremark. All Rights Reserved.
8. Ongoing Maintenance of System Files and Correction of any Errors as required by our contract with
LDH
9. Contingency Plan – should there be a delay in transition as agreed upon with LDH
Once the document is approved by LDH, we would begin to execute against it and engage LDH and their
new vendor as well as the MCOs on a regular basis to discuss progress and conduct bi-weekly check ins.
Non-proprietary documentation will be transitioned per the schedule agreed upon in the plan. Data files
will be scrubbed of any proprietary pricing or other proprietary information and transmitted to the new
vendor according to the agreed upon plan. Once data and file requirements are agreed to we cooperate
with LDH and the new vendor(s) to “fine tune” the proposed dates to ensure reasonable deadlines are
created for each deliverable. Most data files can be sent by secured electronic connection directly to the
new PBM, which expedites the delivery of data. The general timeline involves sending the majority of data
prior to the transition date with a lag file shortly thereafter to complete the data transfers. Depending on
the type of files requested during the termination and the amount of notice given prior to the transition
date, we will transition as much data as possible beforehand with all data being fully transitioned shortly
after the contract termination date.
We confirm that we will perform Medicaid run-out services including the processing of claims post
termination for the time period and pursuant to the terms that shall be agreed to by CVS Health and LDH.
Below is a sample screenshot of our tracking tool checklist:
CVS Health has not had many full client terminations but our most recent health plan customer who
terminated within the last 5 years, sent us an email indicating that the transition process went well and
thanked CVS Health for the work we did to seamlessly transition to their new PBM.
Upon notification of our contract end date, CVS Health would immediately begin inventorying Louisiana-
specific documentation, data, records, files and methodologies in place for the contract. This is
accomplished by both our business team and our IT team. We identify those items we believe are

Louisiana Medicaid Page 83
© 2022 Caremark. All Rights Reserved.
necessary to transition to LDH and/or their new vendor to continue operations of the pharmacy program.
Prior to including them in the Turnover plan, we provide the list of items broken down by business files
and data files to LDH for agreement and approval. Once LDH approval is received we then begin working
on our Turnover/Transition plan that will be delivered no later than one hundred eighty days (180) prior to
the contract end date.
In general, standard data transfer requests are limited to any or all of the following, as requested by the
client: Claims History (up to 12 months), Open Mail Order Refills (excluding compounds, controlled
medications, and specialty medications– unless specifically requested), Open Prior-Authorizations,
Current Account Balances, and Accumulator files, including lag files. Such files will not contain our pricing
information or other proprietary information.
TURNAROUND TIME TO PROVIDE FILES
A minimum 6-week lead time is required for the timely processing of data files anticipated to be a part of
the Turnover Plan, including the exchange of both test and production files. Longer lead times are
required for more substantial populations or longer time periods. Once data and file requirements are
established, we will cooperate with you and your new vendor to establish reasonable deadlines for each
deliverable. Information and communications will be sent to the new vendor in accordance with the
agreed-upon deadlines, transmission process and security standards.
PHI
Upon termination of the agreement for any reason, we shall return or destroy all PHI created or received
by CVS Health as a business associate of LDH in connection with our agreement. CVS Health will scrub
pricing information prior to transitioning claims files and/or history that contains costs and pricing
information to LDH’s new pharmacy benefits manager.
CVS Health will identify in its Turnover Plan all training that we believe is required to take over operations
of the pharmacy program. This includes day to day operations as well as weekly, monthly and annual
business functions. CVS Health assumes the incoming vendor will have their own proposed processes
using their own system, therefore CVS Health will provide Louisiana-specific processes and information
to the new vendor who will then conduct training directly with their teams and respective organization.
CVS Health will manage against the Turnover plan schedule, as agreed to by LDH. As documentation of
operations is turned over to LDH or their vendor, we will request a signoff by the State. Similarly, for data
files transitioned to LDH or their new vendor, we will expect a sign off from the vendor and the State. For
each step of the transition process as we complete items that are not files, but important part of turnover,
we will share the updated status of each task, activity and milestone in the proposed biweekly meetings
with LDH and the new vendor.
CVS Health will designate a Turnover lead to manage the CVS Health items contained in the plan and
maintain a Turnover related action item, risk and issue log. If we are awaiting another stakeholder to take
an action prior to our execution of a particular task, we will denote that in Turnover meetings with the
State and escalate the item for LDH action if the lack of action by a stakeholder begins to infringe upon
our ability to meet the Turnover plan milestone dates. The CVS Health Turnover lead will meet internally
with CVS Health business and IT staff on a weekly basis to check on the progress of their assigned
Turnover tasks. The Turnover lead will also be the primary contact for the State as the plan is executed.
At each scheduled turnover meeting, we will provide the status and progress on our activities and alert
LDH to any lagging tasks owned by LDH or new vendor. A communication method for this status
reporting will be agreed upon as a part of the Turnover plan.
At the conclusion of turnover activities, CVS Health will request confirmation from LDH that no further
knowledge transfer or files are necessary.

Louisiana Medicaid Page 84
© 2022 Caremark. All Rights Reserved.
CVS Health has implemented security measures in compliance with all federal standards related to the
Confidentiality, Integrity and Availability (CIA) of data files. As a part of transition/turnover, we document
each item or file we transition with an assigned turnover identification number. As we execute against our
Turnover Plan, each file is generated and quality checked to ensure its contents are what are expected.
This ensures the integrity of the file. We would then securely transition the file to LDH or their designated
vendor and this would be tracked using the assigned Turnover identification number. Files are encrypted
and transmitted via secure file transfer protocol (SFTP). This ensures that the files sent maintain their
Confidentiality, Integrity and Availability during the turnover process.
• Pharmacy and Prescriber network management: Describe each network separately, including
but not limited to, compliance with Federal and State regulations, as well as addressing each
subsection.
CVS Health understands the LDH pharmacy network requirements and we build our networks with a
focus on providing broad access, choice, and convenience – to maintain and enhance member
satisfaction, along with competitive pricing – to help reduce total costs for LDH, the MCOs, and Enrollees.
We recognize that there will be times when an Enrollee has an emergency which may require access to
an out-of-state pharmacy. We have two solutions that can potentially address continuity and access to
prescription benefits in this situation:
1. CVS Health can implement our currently contracted National network of pharmacies as a “wrap
around” or complimentary network to the LDH Medicaid network. With this option, pharmacies are able to
submit the emergency claim online in real-time and the Enrollee will receive his/her medication without
delays.
2. CVS Health can implement a specific “out of network” message to the pharmacy attempting to fill a
medication for an Enrollee; the pharmacy will contact CVS Health to obtain an emergency override,
based on the plan parameters established by LDH.
CVS Health has the flexibility to accommodate the LDH custom process for maintaining accurate
pharmacy network information in our systems, as well as implementing the LDH’s preferred approach to
handling emergency fill situations with out-of-network pharmacies.
PHARMACY CREDENTIALING STANDARDS
CVS Health will develop a Provider Agreement template that has been approved by LDH and specifies
the requirements for participation in the Louisiana Medicaid Network. Each pharmacy applicant
requesting membership in our network must have specific credentials and meet specific contractual
standards, including, but not limited to:
• Active membership in the National Council for Prescription Drug Programs (NCPDP) and compliance
with HIPAA regulations (e.g., NPI Number, etc.)
• Appropriate state licensure
• A valid DEA number at time of enrollment
• ACA Compliant
• Evidence that all prescriptions are dispensed as dictated by applicable state laws
• The ability to meet all of the contractual and professional obligations for participation in a network,
including:
− Mandatory requirements for electronic transmission of claims
− Submission of U&C charges
− Submission of accurate claims data
− Evaluation of concurrent drug utilization review alerts, along with other online claims processing
messaging
− Compliance with contract and MAC pricing

Louisiana Medicaid Page 85
© 2022 Caremark. All Rights Reserved.
− Valid tax ID number
• Proof of insurance and compliance with malpractice liability requirements
• Submission of the pharmacy’s customary service levels (e.g., delivery services, language
accommodations, emergency hours).
To contract with CVS Health, an independent retail pharmacy must complete all pages of the Membership
Enrollment Form and comply with all data and licensing requirements. The Membership Enrollment Form
includes the pharmacy’s demographic and ownership information. In addition, the following
documentation must be returned by the pharmacy:
• A signed provider contract
• A completed Provider Service Levels form
• A copy of the State Provider License and DEA certificate
• A copy of the Liability Insurance Policy.
To enroll a new chain store, we must receive a request from the chain headquarters. We do not require
hard copies of insurance policy, and state license certificates for members of a chain pharmacy upon
enrollment. The chain headquarters is responsible for ensuring that each store has this information.
Recredentialing Criteria
Our recredentialing process is completed through a survey questionnaire sent to network pharmacies
requesting that each targeted pharmacy verify the data we have on file for that pharmacy. A sample of
data fields include (not all inclusive): pharmacy name, address, phone, fax, e-prescribing participation,
additional services offered, and licensure.
Data on the returned survey are entered into a database and compared to the current data on file. Once
the comparison has been completed, changes are loaded to the master pharmacy database.
Excluded Provider Review
We require that all participating retail pharmacies agree, in writing, to meet all state and federal licensing
requirements. Prior to enrollment, the pharmacy must provide evidence of an active state license.
During the pre-enrollment process, and on a monthly basis, we perform all required § 455.436 Federal
database and some state reviews for excluded providers. If we learn from this review about a CVS
Health network pharmacy that is not in good standing with the OIG, we terminate that pharmacy’s
membership in all our networks. In addition, we frequently contact state board of pharmacy websites and
personnel to verify pharmacy status when it appears that a given pharmacy may be under review by a
regulatory body.
Roster Enrollment Process
CVS Health has extensive experience in implementing and maintaining Medicaid state roster enrollment
processes across multiple states. We will coordinate with LDH to administrator to the Louisiana State
Medicaid requirements tied to the 21st Century Cures Act. The act requires that all providers who provide
services to Medicaid recipients must be enrolled with the state Medicaid in order for the state to make
payments.
• Drug Claims/System Requirements: Describe the approach to, including but not limited to,
processing Drug Claims consistently across all MCOs, compliance with Federal and State

Louisiana Medicaid Page 86
© 2022 Caremark. All Rights Reserved.
regulations, LDH policy, programming flexibility, compound drug policy and process for
benefit changes.
The flexibility of our plan design system is virtually unlimited, which is one of the advantages of selecting
CVS Health as your pharmacy benefit manager. We administer thousands of different plan design
variations, and unlike others in the industry, we own the RxClaim system and are able to implement
benefit configuration modifications on a client-specific basis to accommodate any unique plan design
provisions our clients may present.
CVS Health could assign our standard BIN/PCN for Medicaid which is 004336/MCAIDADV or can create
a unique BIN/PCN if needed. Each MCO will then have its own RxGRP assigned. The RxBIN, RxPCN,
RxGRP, and Cardholder ID will all appear on the Enrollee’s ID card along with the pharmacy help desk
number and the Enrollee care number.
RxClaim can accommodate LDH-defined program policies and designs, including the ability to establish
adjudication rules customized for each LDH program by category codes, eligibility status, Enrollee
attributes (e.g., age, medical condition), drug or drug class (e.g., brand/generic status, drug coverage
status, PDL status), Medicare- Medicaid dual eligible status and other criteria specified by LDH
We are often presented with complex plan designs by our many Health Plan clients. A recent example of
a complex plan design is as follows:
• A large health plan client requested utilization management that included Medicaid real-time smart
prior authorizations.
• The smart prior authorization requires the system, during claim adjudication, to evaluate Enrollee
diagnosis, age/gender considerations, period to date edits, quantity restrictions, and step and
concurrent therapies.
• Using a component-based approach, we can connect edits together with “and” as well as “or”
conditions to create the real-time evaluation.
• Upon successfully meeting the criteria, the claim pays without any intervention and significantly
reduces the number of calls for prior authorization. The claim rejects only when all the criteria are not
met.
Our adjudication platforms are programmed to ensure accuracy, security, and processing efficiency. We
employ several design features to identify fraudulent activities including claim surveillance, and plan
designs which identify unusual prescribing activities, and suspicious claim submission practices.
Our adjudication platform also performs a series of edits against a client’s specific plan design to ensure
utilization, formulary, and claim submission practices meet the intent of each client, and protect against
waste, fraud, and abuse in claim submissions. Our average response time is 0.17 seconds for online
pharmacy transactions.
SYSTEM EDITS
RxClaim performs eligibility verification, claim adjudication, provider validation, duplicate claims edits, and
concurrent drug utilization review (DUR) edits online, in real time. Other edits include Enrollee cost share
calculation, incorrect price, expiration date, prescription validity and claim cost. RxClaim can also process
claims for non-drug items, such as diabetic supplies, pursuant to the coverage policies established by
LDH. This single platform, POS technology maintains complete Enrollee history and instantly updates
plan and eligibility specifications. Enrollee history will be augmented through the integration of twelve
months of historical pharmacy claims (or all claims if the Enrollee has been enrolled for less than twelve
months) and prior authorization approvals for each Enrollee.
RxClaim maintains historical medical, lab and pharmacy data (as provided by the client) for use in prior
authorization adjudication. Historical data will provide the clinical information needed to perform ongoing

Louisiana Medicaid Page 87
© 2022 Caremark. All Rights Reserved.
clinical edits, audits and prior authorizations. Historical information will allow CVS Health to utilize existing
approved prior authorizations as well as implement prior authorization overrides for specific patients. The
ability to grandfather prior approvals will minimize the any disruption to Enrollee access to previously
approved treatment regimens. CVS Health will require providers to seek a new prior authorization after
the historical prior authorization end date.
When a pharmacy claim enters RxClaim, it is assigned a unique internal control number (ICN) so the
claim can be tracked throughout the claim processing cycles.
During the adjudication process, benefit/program-specific edits are applied to the incoming claim. These
edits include:
• Verifying that the pharmacy is/was eligible to perform the services requested and/or was eligible to
receive reimbursement for the billed service on the date of service.
− Application of restrictions specific to a pharmacy such as special claim reviews, payment
withholds, withholds for delinquent taxes, or other limitations as instructed by LDH.
− Denial of payment for services rendered by an ineligible pharmacy provider as defined by LDH
policies.
• Verifying that the Enrollee is eligible for pharmacy benefit being requested, for the date of service on
the claim, including restrictions that might preclude claim payment such as other coverage or cost
sharing requirements.
• Verifying that if the prescribing provider is valid and reject claims containing invalid prescriber
information. This may include:
• Verifying that the National Drug Code (NDC) on the claim is valid and represents a coverable drug,
rejecting claims for drugs not coverable in the program. This would include, under Medicaid, the
drugs eligibility. under the Medicaid Drug Rebate Program (MDRP)
• Verifying that the claim follows program limitations such as age, gender, quantity limits, days supply
limits or per Enrollee monthly prescription count limits, rejecting claims that violate program limitation
rules.
• Verifying if a claim is for a drug that should be covered by another payer, for example, rejecting
claims for Medicare Part D covered drugs when the Enrollee is identified as a dual-eligible (covered
by both Medicare and Medicaid) or if the Enrollee is covered under a commercial or other health plan
• Identification of 340B claims by requiring the dispensing provider submit specific information based
on LDH requirements. RxClaim can utilize the following NCPDP information to identify 340B claims:
− Basis of Cost Determination Code value 08 – submitted in NCPDP field 423-DN
− Submission Clarification Code value 20 – submitted in NCPDP field 420-DK
Variables used in monitoring for duplicate claims include:
• Enrollee identification number
• Date of fill
• NDC number/GCN
• NCPDP
• Refill code
• Prescription number.
These system edits, applied at the point of service, act as an automated management tool to monitor and
help ensure compliance with program parameters before a prescription is dispensed. Our extensive
verification and authorization edits combine with extensive pharmacy desk audit and field audit
capabilities to provide industry leading claim management capabilities.
Online claims requiring additional intervention vary by client. This variation depends on how restrictive the
client’s benefit plan design is and how well the client has communicated that information to its Enrollees.

Louisiana Medicaid Page 88
© 2022 Caremark. All Rights Reserved.
COMPOUND DRUG CLAIMS
The industry-wide NCPDP D.0 standard for multi-ingredient compounds is required for compound claims,
and CVS Health supports this functionality. This functionality captures each ingredient used in the
compounded prescription. In D.0 format, the pharmacist would submit the following elements:
• Compound Indicator
• The NDC, Quantity, Submitted Ingredient Cost for each individual component in the recipe
• Total Quantity and total Usual & Customary price
• Level of Effort value.
The claims adjudication system will determine an allowable ingredient cost for each NDC using lesser of
logic— for example comparing the AWP discount, MAC (if applicable), and the submitted ingredient cost
for each individual component in the recipe. These individual allowable ingredient costs by NDC are then
combined to create an Allowable Final Ingredient Cost. At this point, there is a final check to compare the
Allowable Final Ingredient Cost plus dispensing fee and Level of Effort (LOE) Fee to the pharmacy
submitted total Usual & Customary price for determination of the overall final charge.
The NCPDP D.0 standard for multi-ingredient compounds provides an allowance for professional services
called Level of Effort, or LOE. The following table lists the current LOE values and descriptions.
Level of Effort
Description
11
• Single-ingredient capsule
• Any combination of commercially available products
12
• Two-ingredient capsule/suppository
• Transdermal gel
13
• Three or fewer ingredient cream/ointment/gel*
• Three-ingredient capsule/suppository*
• Two or fewer ingredient troche*
• Non-complex suspension
• Table triturate*
14
• Topical containing controlled substance
• Three or more ingredient troche*
• Four or more ingredient cream/ointment/gel*
• Four or more ingredient capsule/suppository*
• Complex suspensions (e.g., pediatric/altering
PH/base to salt conversion)
• Chemotherapy cream/ointment/gel*
• Hormone therapy (capsules/troches/suppositories)
15
• Sterile products (limited to aqueous bronchial and
nasal inhalations (does not include nasal sprays or
irrigations), injections, irrigations for wounds, and ophthalmic
drops and ointments per USP 797)
* Using bulk (powder) APIs.
Additional adjudication edits may apply based on plan design parameters (e.g., prior authorization,
managed drug limits) and CMS requirements.
PAPER CLAIMS
CVS Health receives all paper claims into a company owned secured facility. Claims are recorded and
scanned into a workflow management system which facilitates the review and adjudication process in
accordance with each client’s plan design, as well as managed all resulting letters and reimbursement
processes. Paper claims are processed within the agreed upon number of business or calendar days, or
within 30 days if no other requirement is provided.

Louisiana Medicaid Page 89
© 2022 Caremark. All Rights Reserved.
Our Quality Control Audits team employs a practice to randomly select and audit processed claims to
measure both data and financial accuracy. Claims are selected based on a client’s design confidence
rating, or similar sampling methodology. We have historically maintained a 99% or higher accuracy rate
for all submitted paper claims. Claims must be submitted using the NCPDP Universal Claim Form and will
be processed within 10 calendar days of receipt.
MASS CLAIM ADJUSTMENTS
CVS Health does not adjust original claims. To provide a clean audit trail, a claim must be reversed and
resubmitted with the correct data on the new submission. Both original claims and void/reversed claims
are included on a client’s claims tape. The reversed/voided claim contains exactly the same data
elements as the original claim, with the exception of the dollar fields being negative. The dollar fields
contain negative dollar amounts, thus reversing/crediting the original claim.
The RxClaim number is used to track a claim, and a sequence number, tied to the RxClaim number,
increments down with each change to a claim. An original claim is sequence number 999. Any future
transactions carry a sequence number one down from the previous number. The only exception is that a
reversal keeps the same sequence number as the original claim.
Generally, in claims adjustment situations, individual claim details are reported back to the client. In these
instances, we complete individual claim adjustments once the benefit change has been entered into the
claims processing system. Claim adjustment dollars then appear within the client’s drug spend invoice. If
as a result of the adjustment the Enrollee overpaid for the medication, then that Enrollee is sent payment
for their overpayment. In situations in which the adjustment is negative – in other words, when Enrollees
have received benefits to which they were not entitled and/or have paid insufficient copays – we can
produce a report identifying the individual claim discrepancies. At this point, the client will need to
determine whether collection activity should take place. The recovered overpayment dollars are included
in a proprietary “refund” tape to the client.
REIMBURSEMENT PROCEDURE FOR A DISCREPANCY
Upon final and conclusive determination of a discrepancy revealed by an audit procedure, as detailed in
the MCO contract, the party that benefited from the overpayment will pay such sums to the other party
within 15 business days of delivery of the conclusive audit findings.
FOCUSED ON FLEXIBILITY, AGILITY, AND DEPENDABILITY
Our integrated claims adjudication processing suite of systems is designed to allow flexibility in the
administration of multiple plan designs in your prescription drug program. Anticipating client needs, the
suite of systems is designed without upper-limit boundaries, and system hardware is upgraded before
current bandwidth or CPU cycle allocations/capacity levels are exhausted.
Timely System Changes
Our knowledgeable and experienced staff make all system enhancements and conduct ongoing
maintenance. Our account teams work collaboratively with clients prior to, during, and after
implementation to ensure plan design terms and expectations are clearly defined, tested, and approved
prior to becoming effective. LDH will be included in every step of transitioning Enrollees to CVS Health,
including pre- and post-implementation testing for quality assurance. CVS Health is committed to
ensuring post implementation changes to accommodate federal or state regulatory or policy requirements
will occur within thirty (30) calendar days of notification by LDH.
System Reliability
We maintain the highest claims processing capacity in the industry, with more than two billion claims
processed annually. We maintain a highly available, resilient environment twenty-four hours per day,
seven days per week, three hundred sixty-five days per year with average uptimes over 99.9% annually.
We ensure all data and reference files used in RxClaim are accurate and updated in a timely manner.

Louisiana Medicaid Page 90
© 2022 Caremark. All Rights Reserved.
Capacity on demand allows readily expandable infrastructure for claims volume increases, keeping client
and Enrollee disruption at a minimum. We invest over $2.0 billion annually on enterprise-wide initiatives
including technology and health care innovations such as Specialty Connect, the digital user experience,
and the Digital Innovation Lab. CVS Health will provide LDH and MCOs an annual risk assessment report
regarding the operation of RxClaim, including assessment findings and mitigation activities.
CVS Health IT Service Center technicians are available 24/7 to respond to system or technical problems.
This team is equipped to handle all support services related to online access via the Internet, and the IT
Service Center is available through a toll-free phone number.
During normal business hours, your account team will notify LDH and the affected MCOs in the event of a
Priority 1 or 2 RxClaim Adjudication system issue within fifteen minutes of discovery of the issue. When a
client-impacting incident is identified, a significant event notification is sent to the Sales and Account
Manager distribution list. Your service team will tailor a custom communication for you and provide
updates until service has been restored. When a rare unscheduled service interruption does occur, all
application processing is moved to the backup system. When the primary systems are fully operational,
processing would be returned to the main data center. Within 5 days of the system issue, we will provide
LDH and affected MCOs with a Root Cause Analysis and summary of actions taken to remedy the issue.
Scheduled downtime is kept to a minimum. During application maintenance downtime, when access to
the system is not available, the system displays the online message Host Unavailable. Scheduled
downtime is planned well in advance and is communicated promptly to all clients. For system
maintenance, the adjudication application is moved to the backup system, and then the maintenance is
executed on the primary system. At the end of the maintenance, the application is moved back to the
primary system.
Because of our extremely high percentage of availability, pharmacies rarely need an alternative access
arrangement, ensuring Enrollees get the help they need when they need it. We are also highly focused on
client and Enrollee data protection and have more than 24 programs in place to guard against
unauthorized access, disclosure, modification, or destruction of sensitive and pertinent data files.
CVS Health can track and report on the specific edits and adjudication rules in effect by date of service
and date of payment, the date a rule was changed, added or deleted, and the benefit plan under which
the rule is used for claim adjudication. An updated list of all active and inactive edits is maintained,
including those that require a prescriber seek prior authorization. This list will be made available to LDH
or other parties at LDH’ request.
• Covered Drug List (CDL) / Preferred Drug List (Single PDL): Describe in detail how the
Proposer will operationalize and maintain compliance with the Single PDL and prior
authorization requirements.
LDH will not have a more qualified respondent to the MCO PBM request for proposals. As of the date of
our submission, more than 50% of LDH’s Enrollees enrolled in MCOs are being serviced on CVS
Health’s systems. CVS Health has experience working with state Medicaid Agency providers to
implement uniform preferred drug lists (PDLs), uniform clinical criteria, administrative edits, formulary
grandfathering/prior use exceptions, and National Average Drug Acquisition Cost (NADAC) plus state
Medicaid agencies dispensing fee pricing with lesser of methodologies. Because of this experience, we
are well-placed to assume the contract with LDH and continue to serve Louisiana’s Medicaid managed
care organization (MCOs).
PHYSICIAN CONNECTIVITY
We have long been a leader in physician connectivity and believes that e-prescribing will continue to grow
as a communication medium. Today more than 60% of all physicians transmit prescriptions electronically.

Louisiana Medicaid Page 91
© 2022 Caremark. All Rights Reserved.
As such, we have made significant investments into the improvements of and delivery of e-prescribing
tools to benefit payors, prescribers, and members.
Through our connection with Surescripts, we are able to provide prescribers with Enrollee eligibility,
patient prescription claim history, formulary, coverage information, and more. We provide this service on
behalf of our clients as part of our comprehensive pharmacy management services.
We have approved hundreds of vendors to access this information, representing more than 1,000,000
prescribers who prescribe electronically using a variety of physician connectivity tool. We provide the
following information:
• Confirm Eligibility
• Display formulary information
• Display coverage (e.g., prior authorization, step therapy, quantity limits, etc.)
• Display alternatives, including generics, automatically for drugs that are non-formulary or not covered.
There is a standardized process in place to pull this information out of the adjudication platform to make it
available through e-prescribing. The system identifies, without manual intervention, all active client
formularies (e.g., when a new client comes on board), and creates the formulary and benefit file using the
National Council of Prescription Drug Programs (NCPDP) Formulary and Benefit version 3.0. The
information is sent to Surescripts approximately day three of the month. This monthly process captures all
changes active on the first day of the month and helps ensure availability to physicians within their e-
prescribing tool.
In addition to the formulary process, we support a nightly eligibility process that feeds additions, edits and
deletions to the Surescripts Master Patient Index (MPI). Electronic Health Records vendors either pre-
process eligibility nightly for the next day’s schedule, or during the prescribing process. Surescripts will
receive a 270 eligibility request from the e-prescribing vendor and forwards it to us based on the MPI. We
confirm active eligibility and respond with 271 responses, including a formulary ID which will map to the
files made available through the monthly process.
Through this process, we help clients achieve their prescribing goals by supporting benefit design at the
point of prescribing, and helping physicians select benefit-aligned medications, lowering costs and
reducing patient disruption at the pharmacy.
DIGITAL TOOLS TO HELP ENROLLEES MANAGE THEIR PRESCRIPTION DRUGS
AND ACCESS THE HEALTH INFORMATION CENTER
Once an enrollee’s benefit becomes active, Caremark.com provides them with tools, information, and
services to help them better manage their prescriptions. Additionally, we have a vast library of health
information materials that enrollees my access to help increase health literacy. and medication costs. We
designed our enrollee-facing digital tools to support our goals of enhancing enrollee engagement and
empowering enrollees to take an active role in their health care.
PDL and Limitations
Enrollees can learn more about their plan to:
• Access a downloadable drug list
• View or print ID cards (also viewable on mobile phones for use at the pharmacy)
• Access drug lists, quantity limit information, and other important guidelines about their medications
Mobile Tools
Every Enrollee will have access to our digital app to help them manage their prescription drug benefit. We
are focused on finding innovative ways to engage and communicate with enrollees, and we look for

Louisiana Medicaid Page 92
© 2022 Caremark. All Rights Reserved.
opportunities to use new technologies to help them manage their prescriptions and keep them connected.
To increase convenience and improve the Enrollee experience, we provide prescription management
tools through our mobile site, Caremark.com, as well as free apps for iPhone and Android users. As the
first PBM to develop mobile capabilities for prescription benefit management, we continue to invest in
these experiences to provide on-the-go access to key prescription and benefit tools, information, and
transactions.
We continue to invest in these mobile experiences, focusing on finding new, innovative methods to
engage and communicate with enrollees in ways that are easiest for them. We seek out opportunities to
use technologies to help them manage their prescriptions and stay connected—especially for those
enrollees who are always on the go or those who don’t have easy access to a desktop or laptop.
Mobile capabilities provide another integrated point of access, offering tools and services when and
where enrollees want them. For iPhone and Android users, the free apps allow enrollees to register,
check drug costs, check their orders and history, refill and request new mail service prescriptions, view
their benefit ID card, and locate a nearby network pharmacy using their smart phone GPS locator
function.
Additionally, prior to registering or logging in, our iPhone or Android app allows enrollees to:
• Refill a mail service prescription: Our Easy Refill function allows an enrollee to scan their mail service
prescription bar code and submit a refill before registering or logging in by scanning the label bar
code
• Check for drug interaction: The Drug Interaction feature allows enrollees to learn how current
medications they are taking may interact with each other, food or beverage, or any OTC medications
they may be taking, all with the simple scan of a bar code on medication or OTC bottles
• Identify a pill: Our Pill Identifier feature helps enrollees identify unknown pills by their markings,
coloring, and shape.
ENSURING COMPLIANCE WITH LOUISIANA PDL
CVS Health will be in compliance with the Louisiana PDL. LDH will also have access to our ad hoc
reporting system for virtually unlimited clinical ad hoc reporting capabilities. Using our user-based ad hoc
reporting tools, we can produce reports that include formulary compliance, drug category/specific drugs,
information on chains vs. independent pharmacies, and brand/generic usage. With this ad hoc reporting
system we can break out reports for groups or sections within the plan.
• Behavioral Health Policies and Procedures: Describe the proposed approach to meet the
requirements in Section 2.1.11.
CVS Health currently works with several of the MCOs operating in the Louisiana Medicaid market, to
operationalize the 90-day Prior Authorization overrides of behavioral health discharge medications for
those Enrollees that the MCOs identify as being eligible. CVS Health will ensure that LDH plan policies
are maintained, in consultation with the MCO’s psychiatrist and the behavioral health facility’s prescribing
physician in determining the safety and medical necessity of the prescribed medications.
In addition, our DUR and Fraud, Waste, and Abuse programs are designed to ensure safe prescribing
through a series of safety messages, RetroDUR, and UM edits at the pharmacy point of sales. These
edits will apply to all of the LDH network pharmacies.
• Point of sale safety messages. These safety alerts ensure that pharmacists are appropriately aware
of safety risks during dispensing. Safety messages help to reduce high dosage, and unsafe
combinations. Example safety messages related to Opioids are:
− Cumulative Morphine Milligram Equivalent Edit
− Buprenorphine/Opioid Edit

Louisiana Medicaid Page 93
© 2022 Caremark. All Rights Reserved.
− Duplicate Long Acting Opioid Edit
− Opioid/Benzodiazepine Edit
− Opioid/Antipsychotic Edit
• Prior Authorizations/ UM – We also have a comprehensive set of utilization management edits,
creating “hard stops” to support prudent prescribing. These PA edits include:
− MME based quantity limits
− Post PA quantity limit durations
− Step therapy (e.g. IR before ER)
− Increased access to drugs to treat opioid use disorder (e.g. lifting PAs on buprenorphine/naloxone)
• Naïve therapy Opioids Days-Supply limits - We have instituted 7-day supply limits for adult new-to-
therapy enrollees, and also offer a 3-day supply limit for enrollees aged 19 and under.
− CMS Compliant with 7 Day initial opioid prescription for acute pain and CMS Mandate for 2019 for
opioid naïve patients
• Retrospective Safety Review - Identifies opioid safety concerns for enrollees within 72 hours of
adjudication for medications and sends communication to prescriber. Examples of retrospective
safety review include:
− Neonatal Abstinence
− Opioid/Antipsychotic
• Specialty drugs and pharmacies: Describe the proposed approach to meet the requirements
in Section 2.1.12.
As the current PBM for three of the MCOs operating in the Louisiana Medicaid market, CVS Health has
experience managing specialty drug claims for Enrollees in an open specialty pharmacy network that
provides adequate access to Specialty medications. CVS Health will continue to administer an LDH-
approved Specialty Drug List, and will provide the list on at least a quarterly basis to LDH, the MCOs and
participating Providers.
• Drug Utilization Review (DUR): Describe the operations for the prospective component of
DUR including compliance with Federal regulations and coordination with the LDH DUR
Board, LDH pharmacy staff and the MCOs.
CVS Health maintains a ProDUR system that is fully compliant with Section 1927 of the Social Security
Act. Our ProDUR system is designed to promote patient safety and reduce clinical abuse and misuse of
outpatient drugs, providing important clinical messaging to the dispensing pharmacy regarding potential
adverse outcomes and inappropriate therapies.
Our system can perform up to 500 concurrent DUR edits on every prescription – in real time to help
ensure the prescription meets both administrative and Enrollee safety criteria. These automated claims
messages are sent to retail pharmacies in real-time, allowing for pharmacists to contact the prescriber
and adjust before the prescription is dispensed.
Administrative edits, on the other hand, often are modified for an individual client’s plan designs and can
be customized for clients that require additional plan-wide control of utilization to achieve their goals. The
POS Safety Review Solution enables delivery of real-time safety alerts to all pharmacies through their
computer systems at the point of dispensing any time a prescription is filled that triggers a safety issue.

Louisiana Medicaid Page 94
© 2022 Caremark. All Rights Reserved.
As part of the benefit set up and ongoing maintenance, LDH will have real-time unredacted access to the
set of parameters and variables applicable to ProDUR functionality. All messaging will be available in
addition to the following minimum requirements:
• Full or partial NDC code matching (including multiple NDC codes subject to potential drug/drug
interaction)
• Date of service range
• Product strength and quantity
• Days’ supply
The claims system sends a warning (passive alert) or reject message (soft block alert). Passive alerts are
informational warning messages sent to the pharmacist for evaluation and do not require the pharmacist
to send a response to CVS Health. Soft block alerts are clinical warning messages that alert the
pharmacist of a potential issue. Soft alerts prevent claim adjudication until appropriate action is taken by
the pharmacist and the pharmacist sends override code that allows the pharmacist to adjudicate the claim
if the medication is appropriate for the patient. The response codes used by our ProDUR system comply
with NCPDP Professional Pharmacy Services intervention code standards. ProDUR adjudication rules will
be based on the configurations approved by LDH. New alerts and messaging required by LDH will be
implemented into our ProDUR system and provided to the pharmacy upon implementation. ProDUR
alerts can be applied to single drug claims or multiple line compound drug claims. Additionally, multiple
alerts can be returned to the pharmacy in a single response transaction.
ProDUR alerts and responses are appended to the adjudicated claims and stored in the data warehouse.
The below table provides a representative list of the ProDUR edits and plan design messaging we offer.
These automated, consistent claims messages are delivered in real-time to mail and retail pharmacies,
providing pharmacists with the information they need to contact the prescriber and adjust before the
prescription is dispensed.
ProDUR Edits and Descriptions
ProDur Edits
Description
Ingredient duplication
Same generic ingredients in more than one drug
prescribed (includes combination products)
This is a hard edit.
Drug-age
Checks for medication potentially inappropriate at
Enrollee’s age; includes both pediatric and geriatric
dosing concerns.
This is a message.
Drug-to-drug interactions
Checks Enrollee drug history for severe interactions
between two or more drugs (as defined by Medi-
Span)
This is a message.
Drug-disease interaction
Checks for drug-disease interaction if Enrollee or
prescriber has provided a diagnosis, or infers
potential interaction using Medi-Span parameters.
This is a message.
Drug-gender
Checks Enrollee drug history for drugs that should
not be used by their gender. For example, the use
of testosterone products by women.
This is a message.
Drug-pregnancy
Check for drugs that should not be used by
pregnant women or women trying to become
pregnant based on Enrollee information or current
Louisiana Medicaid Page 95
© 2022 Caremark. All Rights Reserved.
use of prenatal vitamins or fertility treatments and
age.
This is a message.
Drug-Allergy
Drug-allergy check will occur if m Enrollee has
provided their medication allergies.
This is a soft edit.
Excessive Duration
Detects regimens that are longer than the maximal
limit of therapy for a drug product based on the
product’s common uses.
This a message.
High drug dose
Identifies doses that exceed the maximum
recommended dose by 25%.
This is a message.
Therapeutic duplication
Checks for two or more drugs from the same
therapeutic category.
This is a message.
Low drug dose
Identifies doses that are lower than the
recommended starting dose.
This is a message.
Refill too soon
Will only allow the prescription to be filled on or after
the date on which it should be filled, based on plan
design. Recognizes dosage changes, which would
prevent a refill too soon reject with a previous fill of
a drug at a different dosage and has standard refill
too soon logic that would require a percentage of
the current supply to be used up to a threshold
when there are no dosage changes.
Hard Reject. Will only allow the prescription to be
filled on or after the date on which it should be filled,
based on plan design.
Underuse Precaution (Drug Regimen
Compliance)
Messages the pharmacist when late prescription
refills may indicate the Enrollee is non-compliant
with prescribed medications.
This is a message.
Excessive Controlled Substance Screening
Messages the pharmacist when four or more claims
for the same controlled substance are prescribed
within 90 days.
Ineligible Enrollee
At retail, the pharmacist will contact the Benefit
office.
This is a reject.
Ineligible drug
Drug not covered by LDH. Return the prescription to
the Enrollee and inform him/her that the drug is not
covered.
This is a reject.
Incorrect AWP or formula price
Resubmit the claim with the correct pricing.
This is an alert but will pay.
PDL/ non-PDL
PDL non-compliance alert.
This is a reject.
Quantity Limits
Will reject for quantities greater than permitted by
LDH. The pharmacist will be informed that the
quantity limit has been exceeded.
This is a reject.
Step Therapy
Claim will reject if prerequisite therapy is not in the
claim history. Pharmacist message will note that a
step therapy is required. Generics first step therapies
will note that a generic must be used before the
brand is covered. Instructions for any available prior

Louisiana Medicaid Page 96
© 2022 Caremark. All Rights Reserved.
authorizations will be included in the step therapy
reject message.
This is a reject.
Prior Authorization
Claims that do not meet prior authorization screen
out criteria will reject with a message to the
pharmacist that a prior authorization is required,
including instructions for the prescriber to call an
appropriate 800 number.
This is a reject.
*Alert = claim pays; Reject = claim denied
CONFIDENTIAL
The below table describes these administrative edits:
ProDUR Edits and Descriptions
ProDur Edits
Description
Message
Multiple antipsychotics in
children
Monitors antipsychotic drugs in
children under the age of 18. This
edit can be customized to state-
requirements.
Soft Reject
Cumulative APAP check for
excessive acetaminophen
utilization across multiple
prescriptions
While the current MediSpan
maximum daily dose edit (dose
check) and quantity limits imposed
by the formulary, captures
Enrollees taking more than the
maximum daily dose of
acetaminophen within a single
prescription, the cAPAP edit will
identify Enrollees exceeding 4
grams (4,000 mg) of
acetaminophen across different
drugs by calculating the
cumulative “acetaminophen
ingredient” contribution across
multiple active APAP containing
prescriptions (tablets and liquids).
The historical look back period will
ensure that the days’ supply will
overlap with APAP-containing
product presented at the point of
sale.
Soft Reject 88 – PPS CODE
REQD: APAP EXCEEDS 4
GM/DAY
Dose check/maximum dose
multiplier to identify claims with
excessively high doses (applies
to all drugs)
The purpose of this edit is to
identify doses of medications that
greatly exceed the FDA-approved
maximum dose. While the base
edit triggers at 1.25 times the
maximum daily dose assigned by
MediSpan (which is not
necessarily set at the FDA-labeled
max dose) and returns a message
response, this enhanced
functionality adds a multiplier that
is configurable to the MediSpan
Soft Reject 88 - PPS CODE
REQD: MAX DOSE EXCEEDED –
5x max.

Louisiana Medicaid Page 97
© 2022 Caremark. All Rights Reserved.
maximum daily dose edit. The
purpose of this multiplier is to
identify egregiously high doses at
the point of sale. The default value
for the multiplier has been
selected at “5” times the maximum
daily dose for the claim presented
at the point of sale. Applies to ALL
drugs, not just controlled
substances.
Excessive controlled-substance
claims (for the same drug or
different controlled substances)
within the past 30 days
CVS Health has had an excessive
controlled substances edits for
many years. The “base” edit
“messages” the pharmacist when
four or more claims for the same
controlled substance is prescribed
within 90 days. The enhanced
Excessive Controlled Substance
edit targets more egregious
potential controlled substance
overutilization than the base edit.
The enhanced edit will return a
soft reject requiring the pharmacist
to enter an override. There are two
triggers for this edit:
• Multiple drugs: This edit
targets Enrollees taking five or
more unique controlled
substances within a class of drugs
(same GPI 2) within the previous
30 days. This edit is not
recommended for long term care
(LTC) plans.
• Multiple claims: This edit
targets Enrollees filling
prescriptions for 8 or more claims
for the same controlled substance
(GPI 10) within the previous 30
days. This edit is not
recommended for LTC plans.
Soft Reject 88 – PPS CODE
REQD: MULTI CII-V IN LAST 30
DAYS.
Multiple Pharmacies Edit
Enrollees filling multiple
prescriptions within the same
drug class at four or more
pharmacies (applies to all drugs
Identifies Enrollees filling multiple
prescriptions within the same drug
class (GPI 2) at four or more
pharmacies. The goal of this edit
is to support a consolidated
approach to care by reducing
therapeutic duplication, potential
drug interactions and pharmacy
shopping. Applies to ALL drugs,
not just controlled substances.
Soft Reject 88 – PPS CODE
REQD: >=4 PHARMACIES/SAME
DRUG CLASS.

Louisiana Medicaid Page 98
© 2022 Caremark. All Rights Reserved.
Multiple Prescribers Edit
Enrollees filling multiple
prescriptions within the same
drug class prescribed by four or
more prescribers (applies to all
drugs
Identifies Enrollees filling multiple
prescriptions within the same drug
class (GPI 2) by four or more
prescribers within past 30 days.
The goal of this edit is to support a
consolidated approach to care by
reducing therapeutic duplication,
potential drug interactions and
doctor shopping. Applies to ALL
drugs, not just controlled
substances.
Soft Reject 88 – PPS CODE
REQD: >=4
PRESCRIBERS/SAME
DRUG CLASS.
Buprenorphine/
Opioid
Identifies opioid use after the
patient has begun opioid use
disorder treatment with a
buprenorphine product. The
patient should not receive any new
opioid Rx after they start
buprenorphine. After reviewing the
patient’s medication history, the
pharmacist will have the option of:
(1) filling the Rx as written based
on his/her professional judgment
or
(2) contacting the prescriber to
determine a further course of
action.
Soft Reject 88 – PPS CODE
REQD: HX BUPRENORP, EXCL
OPIOID
Duplicate Therapy (multiple
long acting opioids)
This edit will be set up to soft
reject when prescribed drugs have
the same therapeutic effects as
medication(s) the patient is
currently taking.
Duplicate Therapy (DUPTHER):
The Duplicate Therapy Edit
checks for two or more
medications from the same
therapeutic category. If a previous
prescription in the same class was
dispensed within a given time
period of the current prescription,
the alert would be transmitted to
the dispensing pharmacy.
Soft Reject 88 - PPS CODE
REQD: 2 OR MORE LA OPIOIDS
Drug-Drug
Interactions
(Opioids and
benzodiazepines)
This edit will be set up to soft
reject the pharmacist when
interacting drug combinations are
identified.
Checks the Enrollee’s prescription
history for interactions between
two or more drugs.
Soft Reject 88 - PPS CODE REQD:
DRUG INT OPIOIDS AND
BENZO
Additionally, our Drug-Inferred Health State edit system can screen for drug therapy concerns for the
following conditions:
• Cardiovascular disease
• Cerebrovascular disease
• Central nervous system disease
• Renal disease
• Endocrine disease

Louisiana Medicaid Page 99
© 2022 Caremark. All Rights Reserved.
• Chronic pain syndromes
• Substance use disorder
• Gastrointestinal disease
• Psychiatric disease
• Respiratory disease
CVS Health is familiar with and its operations are in compliance with the Substance Use-Disorder
Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT
Act) which includes required coverage of Medication Assisted Treatment service and drugs and the use
of implement safety edits and automated claim review processes. The edits and process include review
for duplicate fills, early fills, and exceeding LDH established drug quantity limitations, as well as
establishing Maximum Daily Morphine Milligram Equivalents (MME) and concurrent drug use edits (e.g.
opiates and benzodiazepines). CVS Health will continue to work with the MCOs to follow the State’s
specifications for permitted exclusions, prospective safety edits, maximum daily MME safety edits, early
refill edits, clinical authorization criteria for monitoring and management antipsychotic medications for
children, and retrospective automated claim reviews.
Morphine Milligram Equivalent (MME) DUR Edit
This POS edit checks for excessive opioid utilization (GPI-65) via cumulative morphine equivalent dose
(cMED) across multiple drugs and prescriptions. This edit will identify all active opioid prescriptions in a
Enrollee’s drug profile and convert the opioid dose to the equivalent dose of morphine. The cMED is
calculated as follows:
• cMED per day is calculated for each opioid prescription.
• The cMED is calculated based on all opioid prescriptions in the last 90 days of the Enrollee’s claim
history that are still active on the day of the new opioid claim.
• Enrollees in hospice or with a claim for a cancer drug in the last 180 days are automatically excluded
from this edit.
The goal of this edit is to identify potentially dangerous levels of opioid use, including potential misuse
and prescriber shopping. The edit will return a soft reject if the cMED dose is greater than 90 mg AND the
Enrollee has received opioid prescriptions from four or more prescribers in the previous 30 days.
Reporting
ProDUR Activity Report
CVS Health provides our MCOs with the following ProDUR reporting. The ProDUR Activity Report
summarizes claim activity that produces a safety alert and the number of impacted Enrollees. Activity
reports can be requested on a monthly basis 15 days after month close. Key types of POS Safety Review
edits available today are as follows:
• Apparent drug misuse
• Cumulative APAP (acetaminophen)
• Cumulative morphine
• Dose check multiplier
• Drug-age precaution
• Drug-disease precaution
• Drug-drug interactions
• Drug-gender alert
• Excessive controlled substances—multiple drugs
• Excessive controlled substances—number of therapies
• Drug-pregnancy alert
• Excessive duration alert
• High-dose alert
• Ingredient duplication

Louisiana Medicaid Page 100
© 2022 Caremark. All Rights Reserved.
• Low-dose alert
• Multiple pharmacies
• Multiple prescribers
• Refill too soon
• Therapeutic duplication
• Underuse precaution
• Provider and Enrollee support: Describe approach to provide appropriate staff for Provider
and Enrollee inquiries and compliance with LDH and MCO requirements.
As we are currently supporting Enrollees by working with three out of the five MCOs providing pharmacy
benefit management in Louisiana, we understand the importance of providing excellent service and
accurate information. Valuing the Enrollees trust and time, we empower our Customer Care
representatives to provide the best service and up-to-date information as possible. Our comprehensive
training programs along with our call center technology ensure the support for providers and Enrollee
needs. Our staff is already highly trained to handle any LDH-specific questions and have continual
support and training opportunities when needed. We use state-of-the-art call center technology and
implement upgrades to the system to ensure we are providing the best quality service to Enrollees as well
as monitoring communications to ensure our call center staff are meeting certain standards.
OVERALL APPROACH TO PROVIDING PROVIDER AND ENROLLEE SUPPORT
We have been committed to providing high-quality customer service with each customer contact and view
our Customer Care teams as powerful advocates to help ensure that we are fulfilling our commitments to
LDH. We arm our Customer Care Representatives with LDH-specific knowledge, comprehensive training,
and helpful tools to help ensure that all Enrollees receive the personalized attention and tailored
messaging that is essential to Enrollees education and empowerment and to influencing positive behavior
change.
PHYSICIAN HELP DESK
The CVS Health Provider Help Desk is a central point of facilitation, problem resolution, and triage for the
internal departments that interact with physicians and their office staff. To help add value to the
physician’s experience with us, the Provider Help Desk operates with two main objectives:
• Address and resolve physician-related issues that arise throughout the organization
• Serve as a continuous quality-improvement function by tracking and trending, and performing root
cause analysis, to better reveal opportunities for process improvement.
Our experience has shown that the Provider Help Desk enhances the physician experience and
effectively contributes to internal process improvements.
HOURS OF AVAILABILITY
The Provider Help Desk currently operates Monday through Friday, from 8 a.m. to 4:30 p.m. Central Time
Zone. Outside of those normal business hours, we offer a convenient voicemail service for providers to
leave messages. Inquiries are responded to promptly on the next business day.
PHARMACY HELP DESK
Our Customer Care Center includes a Retail Customer Care team that will work with the LDH pharmacy
network and out of network pharmacies for troubleshooting point of service online claim transmissions.
Retail Customer Care Representatives have access to retail pharmacy electronic transactions, allowing
them to assist with eligibility concerns, rejected claim resolution, and clarification of adjudicated claims.
The Retail Customer Care Representatives also provide triage support on inquiries regarding pharmacy

Louisiana Medicaid Page 101
© 2022 Caremark. All Rights Reserved.
payment, LDH enrollment, and other general support, providing the retail pharmacist with a single point of
contact.
Pharmacists can dial our toll-free number to select options from the Retail Services Interactive Voice
Response menu for assistance. The options available from that menu include eligibility, rejected claim re-
processing, and network questions. Pharmacy inquiries are authenticated prior to the release of any
Protected Health Information (PHI). These services are available 24 hours a day, seven days a week.
Please note, pharmacies always have the option to speak to a Pharmacy Help Desk Representative if
they have additional questions or if the Interactive Voice Response (IVR) is unable to provide the answer
or direction needed to adjudicate the claim.
Our Pharmacy Help Desk is led by a management team that is in constant communication with our
Account Services unit, our Customer Care unit, and other supporting areas, which results in greater
consistency and the availability of the most up-to-date information needed to resolve any questions and
concerns related to the Louisiana Medicaid program. As the PBM for three of the current five MCOs, we
have already been supporting pharmacists in your network.
Available When Your Enrollees Need Us
Our Customer Care Representatives are available to all Enrollees through toll-free phone service 24
hours a day, seven days a week. With access to these customer care representatives as well as
registered pharmacists, Enrollees are provided with timely responses to inquiries about their prescription
benefits, prescription orders, paper claims, and other important drug-specific information. With CVS
Health already serving more than 50% of LDH’s Enrollees enrolled in MCOs at the time of this
submission, there will be minimum disruption to the Enrollee when they call us for help and an easy
transition for the remaining Enrollees. Whether the Enrollee wishes to speak to a bilingual representative
or requires emergency access to a registered pharmacist, our Customer Care Centers are prepared to
support their needs.
Accurate Responses to Your Enrollees’ Inquiries
Customer Care Representatives have been using the customer service online database, coupled with
their specialized training, to respond promptly to Enrollees’ calls. The online system provides access to all
LDH-specific and plan design information, Enrollee profiles, utilization history, order status, eligibility
status, claim status, and Louisiana pharmacy locations. The system also provides representatives with
screen access for handling prescription refill requests. Form requests and other special requests are
forwarded to support areas for handling. Representatives log activity to track specific call types and to
enter comments into the online system that document specific customer contact. Questions regarding
medication and therapy are forwarded to a registered pharmacist. Our Customer Care unit also offers the
following:
• Customer Care Representatives have access to retail network pharmacy online transactions to
answer pharmacist inquiries and resolve Enrollee prescription issues that occur at retail. Mail
Customer Care Representatives are supported by the Participant Services Teams located in each of
our mail service pharmacies. The Participant Services Teams’ focus is on providing prompt
responses to special handling and research requests.
• The Customer Care Off-line Support Unit supports the Customer Care Representatives with forms
fulfillment requests. Enrollee’s online records are updated with status/resolution information, and
callbacks or written responses are provided as appropriate. Special handling/expedited requests are
logged and tracked to confirm compliance with standards.
• Written correspondence and email inquiries are directed to the Customer Care Communications Unit
who will provide consistent and timely responses. Inquiries are researched as needed and are
responded to within two (2) business days for emails and within 10 days for written correspondence.
Executive communications are subject to management review and approval. The Communications
Unit tracks written inquiries by type of inquiry and what category the individual will fall under.
Specifically for LDH, a specific indicator would identify the individual as an LDH Enrollee. These
communications would be grouped together, and periodic feedback is then provided on overall and

Louisiana Medicaid Page 102
© 2022 Caremark. All Rights Reserved.
specific trends to Customer Care Management, training, LDH points of contact, and Account
Managers.
• For added convenience 24 hours a day, 7 days a week, we provide toll-free Touch-Tone and voice
integration telephone access to prescription services, along with online access at Caremark.com.
Enrollees can order prescription refills, check order status, find conveniently located network
pharmacies, or obtain order forms and claim forms.
Location of Call Center Staff and Monitoring Policies for Full Staffing
CVS Health already provides a dedicated Customer Care Team to service LDH's Enrollees. With our
extensive experience providing dedicated Customer Care Teams; LDH can be confident that our
Customer Care Representatives are empowered to function as Enrollee’s advocates by engaging
Enrollees and educating them on how to maximize their prescription benefit. With CVS Health already
supporting three of the five MCOs providing services in the Louisiana Medicaid program, all Customer
Care Representatives are trained and have the correct materials.
LDH will have a dedicated call center staff working remotely within the State of Louisiana - and after-
hours Customer Care service will be provided from our Customer Care facility in San Antonio, Texas. All
Staff will be properly trained and have the correct materials specific to the Louisiana Medicaid program.
We provide customer service 24 hours a day, seven days a week, 365 days a year. During the overnight
hours, your Enrollees’ calls will be handled through our San Antonio office.
In order to monitor and ensure full staffing during operational hours for the call center, we use Aspect
Workforce Management. Aspect Workforce is a forecasting and staffing software that features real-time
adherence and productivity reporting. With this software, we are able to staff our Customer Care Units at
half-hour intervals based on a forecasted call volume. The model uses a queuing methodology that
incorporates arrival rates, handle times, and representative availability.
Technology and Automation Used by the Contractor for its Call Center Functions.
Our call center technology enables enhanced service performance. The telecom technology currently
provides the following capabilities:
• We have a total of 7,000 trunks distributed across our Commercial Care organization (which includes
Medicaid). A trunk is a connection between the phone company switch and the subscriber’s (CVS
Health’s) telephone. During a standard business day, we currently operate at about 30% capacity (or
utilizes approximately 2,100 trunks). During Welcome Season, capacity can increase to up to 50% on
peak days. Advanced call routing, ensuring calls are routed to the appropriate representative in an
effective and efficient manner
• Advanced technology to handle call routing without human intervention
• Enhanced administrative reporting capabilities to produce standard reports, with the flexibility to
design ad hoc reports for improved internal analysis
• A dedicated call center switch that provides disaster recovery/redundancy among sites
• An IVR system provides 24-hour, 7-day capabilities for the request of prescription refills, order status,
and claim and mail order forms, while offering the capability to locate a retail pharmacy
• Architecture that is scalable across multiple sites and contact center configurations
• Accommodates single-skill and multiple-skill configurations in both single-site and multiple-site
environments
• Ability to forecast, staff, and schedule non-traditional contacts so that we can manage agents
effectively with special web, email, or phone skills
• Offers a variety of service metrics to guide the service quality for each line of business. The available
metrics that we have systems in place to measure include call volume, abandonment rate, talk time,
handle time, and average speed of answer

Louisiana Medicaid Page 103
© 2022 Caremark. All Rights Reserved.
In order to deliver the best quality support to the Enrollees, we maintain state-of-the-art call center
technology and implement upgrades to the system on an ongoing basis. We continue to refresh our
customer care ICM (Intelligent Contact Management) servers. Our Cisco ICM component drives calls into
a central data location; analyzes the nature and source of the call; and then routes the call to the most
suitable customer service branch, depending on capacity and capability. This component works efficiently
by identifying the nature of the call, while maintaining our competitive Average Speed of Answer (ASA)
rate. Continuous improvements to the IVR have been made to several self-service modules as well as the
development to enhance the flow of information from the IVR to Customer Care representatives to help
ensure a smooth service flow from automated to Customer Care representative provided services. Our
goal is to create and maintain a best in class IVR experience.
Our Customer Care Center uses an automatic call distribution (ACD) telephone system designed to
handle incoming call volume efficiently. The ACD system tracks and monitors incoming and outgoing call
volumes, which enables us to deploy the appropriate number of representatives during the required hours
of operation. The system also helps to ensure proper distribution of calls and provides a high level of
capacity to accommodate additional lines.
All of our Customer Care Centers are seamlessly integrated, using the same online claims processing
system and supporting technology ensuring the same experience each time an Enrollee calls. Our call
distribution and tracking system as well as system inquiry and research applications are integrated
among all of the service centers. This integration enables all representatives to access and respond
consistently and appropriately to inquiries, regardless of the service center in which the representatives
are located. In the event that we experience unpredicted or high-volume call periods, our distribution
system has the ability to route Enrollee calls to an available representative at one of our other facilities.
Such routing occurs on an as needed and temporary basis.
Training Approach and Training Resources Provided to Call Center Staff Specific to
the Louisiana Medicaid Program, Pharmacy Services, and Enrollee Needs
We provide our teams, including supervisors, with LDH specific training, which enables our Customer
Care Representatives to:
• Provide Enrollees with detailed prescription benefit information
• Teach Enrollees how to submit a claim
• Verify order information
• Research claim inquiries about how a claim is paid
• Maintain account information
• Create, view, and resolve requests online, which allows for improved tracking of Enrollee requests
• View communications that have been sent to Enrollees
• Order ID cards and forms
• Coordination of Benefits
• Eligibility Status
Customer Care is committed to the highest level of training and continual support for our representatives.
We work hard to ensure our Customer Care Representatives have access to the tools and education they
need to effectively support Enrollees and resolve issues. We hire representatives who have a minimum of
six months experience in a customer care environment with a high impact customer care role. Customer
Care Representatives must have demonstrable qualifications such as empathy, problem solving, critical
thinking, and self-direction. Our education requirement for Customer Care Representatives is a verifiable
High School diploma or GED. Given we cover three of the five MCOs in the state, we recognize and
understand Louisiana’s Medicaid Enrollees’ unique needs and how to provide them with the best
customer care, and that process starts with our training and support to our Customer Care
Representatives.

Louisiana Medicaid Page 104
© 2022 Caremark. All Rights Reserved.
Comprehensive New Hire Training Program
New hire training for new Customer Care Representatives lasts six weeks and includes a blend of
classroom training and live call integration. In addition to learning customer care skills, learners are
provided with scenario-based learning, such as an Enrollee needing information on a new drug listed on
the PDL, through system demonstrations and system simulations that incorporate hands-on role play.
Representatives split their training time in a classroom setting, observing tenured colleagues, and
participating in on-the-job experiential learning.
Milestone Assessments
New representatives are required to pass three Milestone assessments on content and information
learned during training.
Additionally, we provide new representatives with PALs. PALs are peers that serve as guides and
mentors while they are taking live calls with Enrollees. New hires are graded on calls by our Quality team
to assist in determining whether or not they have mastered the skills required to successfully handle live
Enrollee calls independently.
Customer Care Representatives are monitored regularly – during New Hire training and throughout their
tenure – to ensure that accurate and appropriate information is provided on a consistent basis.
Behavioral Analytics™
Customer Care Representatives receive training on our Behavioral Analytics application. This unique
offering helps turn unstructured call content into structured, usable call data – helping us discover
coaching and training opportunities more quickly for our team members. We record calls using this
application and give representatives the opportunity to listen to their own call experience with a Enrollee.
They can consult with their Supervisors and receive constructive feedback and positive reinforcement.
The application helps us analyze our Enrollee interactions based on objective data. We are able to use
this information to reduce service escalations and enhance Enrollee experiences. We are also able to
measure and track our performance against key metrics, such as average hold time, total talk time,
transfer rate, etc.
Famous for Service
We believe our Famous for Service culture and mindset sets the stage for creating an outstanding
experience for each of our LDH Enrollees, including the current Louisiana Medicaid Enrollees we serve
and future LDH Enrollees. The experience we create is one where our Enrollees feel heard, understood,
and as if they are working with us as a team striving together for better health. We understand the
difficulties many Medicaid Enrollees have with multiple co-occurring chronic conditions requiring complex
drug regimens, combating various social determinants of health, or both. Starting on day one of training,
colleagues are introduced to the concepts and purpose of the Famous for Service culture. Throughout
new hire training and beyond, we infuse customized behavioral development and recognition programs
that build upon the core behaviors that were identified by business operation leaders in collaboration with
training and development. These behaviors drive the foundation of the organic journey and evolutionary
approach that we are creating together to ensure that we are differentiating ourselves to stay competitive
in the healthcare marketplace.
The affirmation statements and objectives for the five core Famous for Service behaviors identified for
Customer Care are as follows:
Famous for Service

Louisiana Medicaid Page 105
© 2022 Caremark. All Rights Reserved.
Accountability and Ownership
I take personal accountability for my actions and
results.
• Demonstrate ownership behaviors by using critical
thinking skills
• Create an outstanding Enrollee experience through
committing to act, self-awareness, remaining
objective, first call resolution, and positive
consultation
• Plan three ways to take personal accountability for
actions and results.
Listen and Anticipate
I hear the spoken and unspoken needs of the
Enrollee.
• Recognize and apply active listening techniques
• Recognize the importance of staying focused
• Create a personal strategy for focused listening
• Identify needs, spoken and unspoken, by asking
questions.
Be Caring
I demonstrate caring and acknowledge all Enrollee
comments appropriately.
• Evaluate the feelings of a Enrollee
• Overcome potential caring challenges
• Apply empathetic listening techniques
• Respond to Enrollee comments effectively with
empathy and caring.
Be Resourceful
I maximize all the tools available to me.
• Demonstrate collaborative problem solving
Assess situations and resources available to you
• Act quickly to resolve Enrollee issues by
maximizing your resources
• Apply resourcefulness techniques
Educate the Enrollee
I proactively guide Enrollees on how to use their
benefits.
• Identify the key components of reacting versus
responding to a Enrollees needs
• Recognize the significance of building a positive,
long-term health care relationship with Enrollees
• Explain how you can actively and supportively
shape the future of healthcare by educating the
Enrollee
Our implementation and account teams will continue to ensure that Customer Care Representatives are
trained on any LDH Enrollee-specific information via computer-based training, bulletin postings to the
internal proprietary online tool, updates to Enrollee Information Forms, and through desk-based reference
information.
Use of Back-up Staff to Support Increased Call Volumes, How CVS Health Ensures
Such Staff are Trained and Have the Correct Materials Specific to the Louisiana
Medicaid Program, and Location of These Staff.
Our Customer Care Center uses an automatic call distribution (ACD) telephone system designed to
handle incoming call volume efficiently. The ACD system tracks and monitors incoming and outgoing call

Louisiana Medicaid Page 106
© 2022 Caremark. All Rights Reserved.
volumes, which enables us to deploy the appropriate number of representatives during the required hours
of operation. The system also helps to ensures proper distribution of calls and provides a high level of
capacity to accommodate additional lines.
All of our Customer Care Centers are seamlessly integrated, using the same online claims processing
system and supporting technology, meaning all staff has and will continue to have the correct materials
specific to the Louisiana Medicaid program. Our call distribution and tracking system as well as system
inquiry and research applications are integrated among all of the service centers. This integration enables
all representatives to access and respond consistently and appropriately to inquiries, regardless of the
service center in which the representatives are located. In the event that we experience unpredicted or
high-volume call periods, our distribution system has the ability to route Enrollee calls to an available
representative at one of our other facilities. Such routing occurs on an as needed and temporary basis.
How CVS Health will Meet and Monitor Call Center Standards, and How CVS Health
will use Monitoring Results to Adjust Operations, as Needed
Quality assurance performance tracking is an important element in coaching and development for the
individual representative. Daily, weekly, monthly, and quarterly data is disseminated to enable ongoing
assessment and intervention.
Accuracy measurement is present throughout call monitoring that is conducted by both our Quality
Assurance Team and Supervisors. A combined minimum of eight calls are monitored for each Customer
Care Representative. Supervisors utilize reporting from Behavior Analytics that may present challenges to
the Customer Care Representative such as First Call Resolution results, call back rate, and silent time
along with behavior specific components. Their review is based on the coaching needs of the Customer
Care Representative while our Quality Team’s reviews are random.
Targeting calls that have been identified as resulting in a call back or struggles interacting with a specific
behavior has allowed us to coach and develop our Customer Care Representatives to provide
personalized customer service.
Our Customer Care Department strives to provide quality, courteous, and professional customer service
at all times. Our representatives are frequently reminded of the challenges many Medicaid Enrollees’ can
have daily. Any reoccurring quality issues are addressed through standard corrective action plans or
retraining, as deemed appropriate.
We have zero tolerance for unprofessional or rude behavior as well as failure to follow through on
commitments made to Enrollees. Any employee who is observed exhibiting rudeness or other
unprofessional behavior will be subject to disciplinary action, not limited to corrective action or
termination.
Our Customer Care Representatives log all Enrollee inquiries electronically into our system. During each
call, a record is created regarding types of questions asked, special requests made, and actions taken by
the Customer Care Representative. Customer Care can access this data via monthly reports or through
an online service.
Additionally, our Customer Care teams use a web-based reference tool, which maintains online
procedures, processes, benefit design, and “job aids” to assist them in responding to Enrollees inquiries.
We employ Information specialists who work closely with resources across the organization, including our
Account Managers and Customer Care Training staff, to ensure information is maintained accurately.
The Quality Assurance Team
The Quality Team reviews a monthly targeted sample of calls from LDH Enrollees.

Louisiana Medicaid Page 107
© 2022 Caremark. All Rights Reserved.
The Quality Team and Customer Care Supervision conduct ongoing call audits across the enterprise
targeting behaviors and performance relative to goals which are based on our vision, mission, and values.
Representatives are provided coaching and development based on trends that may be discerned from
either the supervisor or quality observations.
CVS Health maintains call center services and call center lines to respond to LDH Enrollee claims
inquiries, questions, problems, and complaints regarding operations, and for other pharmacy Provider
and Enrollee support. We supply all required information systems, telecommunications, and dedicated
personnel to perform these operations.
Our Customer Care Representatives track 100% of Enrollee calls within our customer relationship
management application, regardless of inbound contact method. This system captures inquiry type,
pending action(s), representative name, and resolution for each call received. Additionally, the system
automatically documents all Customer Care Representative activities in the account.
Behavioral Analytics Support
All CVS Health call centers are equipped with Behavioral Analytics recording software. Behavioral
Analytics is an application that captures and analyzes the Enrollee’s call and displays call data in a
structured format to better target opportunities and reinforcements. Enrollees are notified of the recording
prior to speaking with a representative. Retained for up to 90 days, the recordings and associated data
are used to enhance the coaching and instruction provided to Customer Care Representatives (in the
areas of customer interaction, techniques of online research, etc.).
We ask that any difficulties encountered by any LDH Enrollee when working with a CVS Health Customer
Care Representative be reported immediately to the CVS Health Account Director. The CVS Health
Account Director will facilitate communication with the appropriate Call Center Manager for a coaching
and feedback session with the representative. The manager will determine whether emerging trends in
performance and/or behavior are evident, and whether additional developmental or disciplinary action is
needed.
Call Audits
Using the Behavioral Analytics data to identify trends, our Quality Assurance team conducts targeted call
monitoring to understand the key drivers and solutions to address them. It is important to CVS Health to
confirm many of these calls are identified as Louisiana LDH Enrollees to ensure we are providing the
upmost service. Each month, approximately 15% of calls per Customer Care Representative are
analyzed by our Behavioral Analytics tool. In addition, an average of two to four calls per Customer Care
Representative are reviewed by a combination of supervisors and quality team members. Quality
assurance performance tracking is also an important element in coaching and development for the
individual representative. Daily, weekly, monthly, and quarterly data are disseminated to enable ongoing
assessment and intervention.
CRM Tool for Enrollee Information
All Enrollee information is housed within our CRM, PeopleSafe which is populated with data originating
from RxClaim. Customer Care Representatives (CCRs) are able to utilize this system for order
placement, order status, billing, plan design information, fulfillment requests, etc. Additional benefit plan
specific details are housed in information forms supported within an extension of PeopleSafe. CCRs have
dual monitors to easily navigate the information required to service each call.

Louisiana Medicaid Page 108
© 2022 Caremark. All Rights Reserved.
CVS Health Customer Care utilizes PeopleSafe to document, categorize, process, and track all LDH
claim inquiries, pharmacy provider/Enrollee communications, and grievances and appeals. We assess all
deliveries of quality service to LDH Enrollees. We believe achieving quality in servicing Enrollee needs is
a combination of overall communication delivery, accuracy, and efficiency.
In an effort to further establish CVS Health as a pre-eminent service provider in the health care industry,
our Customer Care uses the Behavioral Analytics tool from Mattersight™. Behavioral Analytics allows us
to record, analyze, and interpret unstructured call content into structured, usable call data, which is then
used for coaching and training opportunities. The application also provides an objective view of our
service levels. We are able to analyze our Enrollees interactions based on substantial data, resulting in
reduced service escalations through proactive servicing. We can also utilize data from calls to enhance
the Enrollees experience and improve the Customer Care Representative’s performance.
CVS Health will acknowledge pharmacy Provider and Enrollee inquiries within one business day of
receipt.
Tracking Categories
The call reasons and tracking categories available to our representatives include the following:
• Billing/Payment
• Order Placement
• Order Status
• Fulfillment of forms, cards, etc.
• Paper Claims

Louisiana Medicaid Page 109
© 2022 Caremark. All Rights Reserved.
• Claim Inquiries
• Enrollee Questions
− Enrollee Problems
− Complaints Regarding Operations
− Eligibility
• CVS Health Programs
• Retail Pharmacy
• Plan Design/Plan Benefits
• Prescription Verification
• CVS Health Information
• Medicare
• Pharmacist Consultation
• Training
• Voice Response System or Website
• Appeals.
Reporting
LDH will have access to our total book-of-business statistics if you utilize a shared toll-free number. We
can create LDH Enrollee specific reports detailing this information on a monthly basis, or otherwise.
With our custom toll-free number, call metrics reports can be generated as well. These include number of
calls answered, average speed of answer, abandonment rate, and much more. These metrics can be
analyzed to improve ways of serving Louisiana’s Medicaid Enrollees. The reports can be furnished on a
monthly basis, or otherwise. Standard reporting is provided through the Account Team.
Any issues requiring assistance, research, and resolution by another area is tracked through Resolution
Manager, a task-based system that timestamps activity through the path of an issue, from the time the
task is created to the time it is closed. At the time of the initial telephone call, the Customer Care
Representative will generate the task, and it is forwarded to the appropriate area for resolution. Internal
reporting is generated to ensure that all tasks are resolved within the timeframe expected, and any
outliers are easily identified and addressed by management.
MONITORING REPRESENTATIVE PERFORMANCE
Through the performance review process, a Customer Care Representative’s performance is linked to
various goals and expectations that support our quality, Enrollee satisfaction, and Customer Care metrics.
TRAINING PROVIDED TO CUSTOMER CARE REPRESENTATIVES
We provide our Customer Care Representatives with an in-depth 3-day portal training. During this
training, Customer Care Representatives are given instruction on basic navigation as well as identifying
any potential issues. Training topics include, but are not limited to:
• Registration – requirements and steps, family access, etc.
• Navigation – ordering prescription refills, checking drug cost, updating personal information, setting
up alerts, accessing prescription history, etc.
• Identifying Potential Concerns – using the web error log to identify errors or problems Enrollees may
be encountering when using the website.
CVS Health is committed to the highest quality experience for Enrollees when they interact with our
Customer Care call centers and takes action to ensure our Customer Care Representatives (CCRs)
deliver professional service and expert benefit information. Rather than relying solely on traditional one-
on-one coaching sessions, we have developed an IMPACT Coaching model that enables both CCRs and
their supervisors to play a more active role in coaching and employee development. By partnering with

Louisiana Medicaid Page 110
© 2022 Caremark. All Rights Reserved.
peers to jointly practice improving their performance and building their interpersonal skills, IMPACT
Coaching helps strengthen our CCRs’ ability to support Enrollees with the information they need to make
smart health care choices and increase satisfaction with their prescription benefits.
SHARING CONSTRUCTIVE FEEDBACK TO IMPROVE PERFORMANCE
In our Customer Care Quality Monitoring Program, CCRs are provided coaching and development based
on trends that may be discerned from either their supervisor or quality observations. Under this program,
approximately 30% of calls per Customer Care Representative are analyzed by our Behavioral Analytics
tool each month. On average, up to four calls per Customer Care Representative are reviewed by our
quality team members. In addition, Supervisor review up to four calls per Customer Care Representative.
We find that targeting coaching strategies directed around calls that have been identified as resulting in a
callback or specific behaviors allows us to coach and develop our CCRs to improve overall Enrollee
experience. By adding a peer-to-peer program component to our coaching model, we now can more fully
engage our CCRs in performance improvement to help optimize their ability to deliver excellent Enrollee
service.
CCRs continue to receive side-by-side coaching from their Supervisor and also participate in one monthly
peer-to-peer performance improvement session. The session provides our CCRs with call feedback from
their Supervisor as well as three of their Customer Care peers, helping identify strengths and explore
opportunities for improvement. We find that by sharing constructive feedback and lessons learned in real-
life situations – such as handling upset Enrollees, deciding when to escalate calls, and helping each other
remain professional and composed in stressful situations – our CCRs are able to simultaneously
strengthen their own and their peers’ performance.
Feedback is provided on a standardized form to offer constructive input on all aspects of the call, from the
greeting and authentication process through closing the call, including categories such as courtesy and
empathy, first call resolution, providing accurate information, and proactive education. We continuously
work on providing information to our Customer Care Representatives to help educate them on the specific
and complex needs of some of the Enrollees we serve.
ADVANTAGES OF IMPACT COACHING
In addition to fully immersing our CCRs in the coaching process, our model:
• Promotes team building and engagement
• Enables sharing of best practices from peer to peer across all levels of experience
• Promotes the CVS Health culture and talent retention
• Leverages multiple coaching styles
• Enhances performance improvement for work-from-home colleagues with instant group feedback
• Guarantees that 100 percent of our CCRs are coached monthly.
• Leverages cooperative learning to increase employee engagement.
We value the input of our Enrollees and we have a process to capture that feedback. Upon speaking with
a Enrollee who provides feedback or suggestions on our processes, an electronic record of this
suggestion is created. This record is retained in the Enrollee’s history and will also be routed to a team of
individuals who review the information to determine the appropriate department where this feedback will
make the most impact, at which point the suggestion is submitted. Since we are currently working with
Enrollees in Louisiana, we have foundational knowledge of some of the experiences they’re facing and
the input they have already provided.
EXAMPLES OF ENROLLEE FEEDBACK
We received feedback from Enrollees that our IVR system was difficult to navigate, which resulted in a
Enrollee staying in the system for longer periods of time than they felt acceptable. As a result of this
feedback, we conducted a thorough analysis of our IVR system and implemented the following changes:

Louisiana Medicaid Page 111
© 2022 Caremark. All Rights Reserved.
• Voice recognition
• Test claim/Coverage/Pricing
Another example of feedback that resulted in process improvements had to do with the size of the vials in
which medications were dispensed. Enrollees had requested smaller sizes on multiple occasions. We
took action and re-engineered our systems and we now offer three (3) different vial sizes from which
Enrollees are able to choose.
CVS Health tracks Enrollee feedback and reasons for calls, in order to identify trends. With this
information, MCO account teams will work closely with LDH and the assigned customer care advisor to
monitor and discuss these issues with you. In addition, we will perform Enrollee surveys and share these
results with LDH.
• Oversight and monitoring: Describe the proposed approach to meet the requirements in
Section 2.1.15.
CVS Health understands the payment arrangement between the Contractor and the MCOs, with LDH not
paying CVS Health directly for any services, nor being party to the contracts between CVS Health and the
MCOs. Further, CVS Health already utilizes a Corrective Action Plan process that aligns with the
applicable oversight and monitoring requirements in Section 2.1.15 of the Scope of Work, as follows:
CVS Health shall submit to the MCO within 5 Business Days of receiving from the MCO a notice of non-
compliance with Applicable Law (or within such other time period to which the MCO might agree), a
Corrective Action Plan acceptable to the MCO that seeks to remediate the non-compliant issue(s).
Where an instance of noncompliance with Applicable Law has been identified by the MCO, PBM shall
provide to the MCO within 5 Business Days of receiving notice from the MCO (or within such other time
period to which the MCO might agree), a Corrective Action Plan acceptable to the MCO that seeks to
remediate the non-compliant issue(s).
CVS Health shall execute the Performance Improvement Plan within the timeframe stated in such plan.
Failure to satisfactorily remediate a non-compliant issue may constitute a Material Breach.
Compliance – Correction Accuracy and Timeliness is calculated as the number of days it takes the PBM
to provide to the MCO an acceptable corrective action plan to remediate non-compliant issue(s), after
CVS Health has received notice of non-compliance during a given period of measurement. Consistent
with CMS guidelines, non-compliance issues could be received via compliance letters, notices, warning
letters and corrective action plan requests, ad-hoc reports, compliance analysis, and annual Past
Performance Reviews during a given period of measurement
Where an instance of noncompliance with Applicable Law has been identified by the MCO or Government
Authority, CVS Health shall provide to the MCO within 5 Business Days of receiving notice from the MCO
(or within such other time period to which the MCO might agree), a corrective action plan acceptable to
the MCO that seeks to remediate the non-compliant issue(s).
• State and Federal Mandate Compliance: Describe the proposed approach to meet the
requirements in Section 2.1.17.
CVS Health confirms that it is in compliance with all applicable State and Federal laws, rules, regulations,
and will fully comply with any and all Federal, State and LDH audit requests. Our Provider networks are
in compliance with all applicable Federal and State laws, and will be contracted in full adherence to the

Louisiana Medicaid Page 112
© 2022 Caremark. All Rights Reserved.
State Plan. Our Provider Agreements require all participating retail pharmacies to agree in writing to
comply with all applicable federal and state laws and regulations.
We require all third parties utilized to comply with all federal and state privacy and security laws as well by
requiring Business Associate Agreements and conducting vendor assessment audits of the third parties
handling PHI regularly. We have a robust library of privacy and security policies which are reviewed
annually to help ensure compliance with all regulation changes and provide training to all employees
upon hire and annually thereafter. Additionally, our annual corporate training program includes a module
that provides all employees with an overview of HIPAA and employee responsibilities.
Our Government Affairs (GA) team, based in Washington D.C., comprises experts on State and Federal
legislative and regulatory issues affecting our business units, clients, and customers.
We are committed to helping ensure compliance with state and federal Medicaid regulations. Our
Medicaid Regulatory Affairs Department gathers Medicaid regulatory information for each State through a
variety of sources including but not limited to Government Affairs, PBM clients, and State Medicaid
Agencies. Our Medicaid regulatory team is supported by internal legal counsel (and outside law firms as
needed), who assist in reviewing new regulations to determine relevancy to the Medicaid business -- for
example, whether the regulations are applicable to state Medicaid Agencies, managed care, or both.
After the Medicaid Regulatory Department receives a new regulatory requirement, they review it internally
with CVS Health operations staff to determine what gaps, if any, exist in our ability to comply with the new
regulations. The Medicaid Regulatory Department works directly with the operations teams to ensure
understanding of the requirement and a compliant implementation. Collaterally, procedures may be
created and updated for the new requirements and if appropriate, internal and external communications
are drafted. The Account Teams distribute the client communications that are developed and reviewed
with the help of Regulatory, Legal or Client Experience teams.
The Medicaid Regulatory Department will review the state’s model managed care contract and during a
new implementation, account management, and operations teams prior to the implementation kick off and
is referenced often during implementation. This way, we are prepared to begin the implementation of new
business from a position of knowledge, which is helpful to the overall success of the project.
Data Retention Standards
We store member claims history detail—including all retail, mail, and paper claims—online for 48 months
plus the current plan year. After being stored online, all historical claims data is stored on tape in a
secure, climate-controlled facility as required by law. Claims data is stored for up to 15 years from the
date the claim is closed, depending on the specific client contractual requirement. CVS Health will
maintain plan and Enrollee data based on LDH policy.
• Audit: Describe approach to provide an audit program (Section 2.1.18).
A comprehensive pharmacy audit program is a key element in an effective prescription benefit
management solution. CVS Health’s Pharmacy Performance (Audit) program incorporates proactive
investigations, concurrent daily reviews, and retrospective audits/recoveries, with particular focus on
government programs.
The Pharmacy Performance Department reviews 100% of electronic claims data that pharmacies submit
to CVS Health. The below table describes our claims audits. Table
CVS Health’s Pharmacy Claims Audits
Point of Service Audits
Automatically using point-of-service system
edits—automated tool to monitor and ensure

Louisiana Medicaid Page 113
© 2022 Caremark. All Rights Reserved.
compliance to program parameters when the
prescription claim is adjudicated without utilizing
additional overhead
Next Day Consult
Next-day consult using additional automated
claims’ reviews where outlier claims are determined
and a daily professional review and outreach
occurs to validate and/or correct inappropriate
payments
Quarterly and Ongoing Retrospective Review
Quarterly and ongoing retrospective reviews that
tap into claim patterns at the pharmacy level,
resulting in follow-up audits for initial observation
and original documentation review on-site, and/or
investigational audits that commit to a deeper
dive—including drug purchasing and pedigree
validations
EXPERIENCED STAFF THAT DELIVER RESULTS
Our Pharmacy Performance Department has an audit staff of nearly 75 full-time professionals, many with
decades of audit and health care experience. Our staff are drawn from a variety of health care
backgrounds, including retail pharmacy professionals, certified pharmacy technicians, registered
pharmacists, registered nurses, a podiatrist, and a physician.
CONFIDENTIAL
These team members have significant combined retail, specialty, home infusion, and long-term care
pharmacy experience. Pharmacists lead the Pharmacy Performance Department, including one who
holds an active Louisiana pharmacy license. We have a Certified Fraud Examiner (CFE) to provide a full
understanding of problematic trends. Our industry standing is augmented by the close working
relationships we have with organizations such as the National Healthcare Anti-Fraud Association, and
National Association of Drug Diversion Investigators.
INTERNAL AUDIT STAFF REDUCES PHARMACY PROVIDER FRICTION
We use CVS Health employees to audit our pharmacy network to help ensure that Enrollee claims are
paid correctly. Our use of internal auditors also eliminates the incentive that external pharmacy audit firms
have to mark claims as being processed incorrectly for technical reasons. While these mis-marked claims
do not affect patient care, they can be used to enhance the revenue garnered by external firms at the
retail pharmacies’ expense. Thus, by using internal auditors, we will avoid charging back proper claims
inappropriately and preserve the positive relationship between the pharmacy network and Louisiana’s
Medicaid Enrollees.
CONFLICT OF INTEREST AVOIDANCE PROCEDURES
CVS Health has a culture of compliance and transparency. We understand that CVS Health’s PBM
auditing CVS pharmacies would give the appearance of a conflict of interest. Even though our Pharmacy
Performance Department conducts every audit in an unbiased manner, we contract with a national audit
vendor to perform independent audits of CVS retail pharmacies. We require the audit vendor uses the
exact same methodology for CVS pharmacies that the Pharmacy Performance Department auditors use
on non-CVS chain and independent pharmacies. We can provide LDH the contract CVS Health holds
with the independent audit firm for review upon LDH’ request.
FAIR BUT FIRM PHILOSPHY – EASING PROVIDER BURDEN
CVS Health’s PBM is staffed with hundreds of pharmacists and we understand that being a pharmacist is
a very challenging profession. Every day a pharmacist makes hundreds of decisions that both prevent

Louisiana Medicaid Page 114
© 2022 Caremark. All Rights Reserved.
harm to Medicaid Enrollees and improve their health and wellbeing. To recognize this contribution, we
designed procedures to minimize administrative burdens on Louisiana pharmacies. Our belief is that the
pharmacy should only have items brought to their attention that could result in either physical harm to a
Enrollee or financial harm to the State of Louisiana and its taxpayers.
We also know that pharmacies don’t have inactive time. Therefore, we designed our onsite to be
completed, end-to-end, within 90 minutes, including the exit interview. Our typical onsite audit reviews
100 to125 unique claims, which we select as the most likely to have discrepancies. This approach is
efficient for the pharmacy and maximizes the time the pharmacist spends on patient care and not
unnecessary claims review.
CVS Health created an educational approach to auditing as opposed to a “gotcha” approach, which
doesn’t account for the fact that mistakes happen. It is the best interest of Enrollees, pharmacies, and
LDH that our audit efforts help prevent the same error from re-occurring. Therefore, we staff the
Pharmacy
Performance Department with real-world pharmacy experience to bring meaningful understanding and
advice to pharmacies. This clinical approach to auditing focuses on findings that truly impact Enrollees,
rather than technical “gotchas” that only lead to provider friction.
THREE-PRONGED AUDIT APPROACH – IDENTIFY, DETECT, PREVENT, DETER
CVS Health’s has a three-pronged audit process designed to identify discrepancies, prevent and detect
FWA, and provide a deterrence message to pharmacies.
Identifying Discrepancies
We conduct statistical reviews on every pharmacy that has claims volume in excess of $1,000 and/or 100
or more claims submitted each quarter. The statistical analysis filters data to help identify claims outliers
that require further examination. After the analysis is completed, we provide a report that summarizes
pharmacy trends that indicate pharmacy deviations such as:
• Higher percentage of claims for a narrow set of higher costing NDC numbers
• Percentage of refilled claims
• Total number of claims
• Percentage of high dollar claims
• Average prescriptions per member per month
Pharmacies specializing in compounding, specialty drugs, long-term care, and mail service are compared
to like peers and analyzed separately to determine if potential discrepancies warrant closer scrutiny.
Annual market checks are conducted by evaluating current utilization, cost and market changes for
continuous honing and improvements of review criteria.
Detecting and Preventing Fraud, Waste and Abuse
When CVS Health identifies FWA involving a network pharmacy, we work closely with impacted clients—
with heavy prioritization of government-related organizations (e.g., Medicare Part D plans, Managed
Medicaid plans and Federal government clients, etc.)—to communicate the issues and to provide the
necessary support to correct future problems.
Providing a Deterrence Message for Future Activity
We developed our audit protocols to include an educational component as well as underlying messaging
for required self-improvement as a deterrence measure to diminish the occurrence of repeat offenses.
For example, high-dollar claims or abnormally high quantities or dosages on claims are reviewed as a
supplement to any system edits, and appropriate outreach to the identified pharmacies to validate and
educate is completed, as applicable.

Louisiana Medicaid Page 115
© 2022 Caremark. All Rights Reserved.
Another example: CVS Health identified through our daily review process a prescription for Enoxaparin
(for blood clots). This drug can be dosed different ways, depending on prevention versus active
treatment. A prescription was misread by a pharmacy and entered for a dose that would have potentially
caused bleeds. The daily review called the pharmacy and found the dosing error. The pharmacy had
actually put on their list to order that night. Due to CVS Health’s action, the dose was corrected and no
patient harm arose from the mistake.
DESKTOP REVIEWS
The Pharmacy Performance Department believes that the best way to protect patient safety and the
financial resources of LDH is through rapid response desktop reviews. We developed a highly effective
leading-edge algorithm to review every claim submitted for reimbursement.
The algorithm contains a closely held set of rules that identifies claims that are potentially erroneous or
unusual. The claims flagged as erroneous undergo a secondary review by certified pharmacy technicians
to spot claims in need of correction. The claims are also flagged for the specific reason why the claim
appears to be incorrect. If the auditor feels there is an issue, they will call the pharmacy and review the
claim over the phone. If the claim is incorrect, they will have the pharmacy correct the claim. Not only
does this save LDH money by avoiding payment for an inflated claim, it saves the pharmacy money
because that claim will not be recouped in a future audit. The other benefit to this approach is claims are
most frequently corrected in the same payment cycle, rather than having to wait to recoup funds through
an onsite audit down the road.
The rapid response process is invisible to the Enrollee - only CVS Health and the Louisiana pharmacy
know that an error occurred on the claim, thereby preserving the Pharmacist-Patient bond. This reinforces
the trust between the pharmacist and patient, which is important to maintaining the pharmacist as a
trusted member of the Enrollee’s health care team.
Statistical Auditing with PEAR
The Pharmacy Performance team analyzes all claims submitted to us by every pharmacy for the entire
book of business, including LDH’ Medicaid claims. A quarterly statistical review is performed to analyze
the utilization of every pharmacy that has submitted claims totaling $1,000 or more and/or processed
more than 100 claims in the previous quarter. The purpose of this analysis is to identify pharmacies with
claim activities indicating unusual trending and noncompliance to your program parameters. The quarterly
report used for this statistical analysis is the Pharmacy Exceptional Activity Report (PEAR).
100% of LDH’s pharmacy claims will be subject to a daily review and a quarterly statistical review.
The PEAR statistically measures certain criteria and evaluates pharmacies on the basis of their actual
claim activity within the parameters of an expected norm for a provider’s peer group. The pharmacy’s
peer group is based on their MSA (Metropolitan Statistical Area), which allows dispensing patterns to be
analyzed within regional variations, yet still be able to identify outliers requiring further examination.
Audits for mail service pharmacies, long term care and specialty pharmacies are distinct peer groups that
are analyzed as separate groupings. The report summarizes pharmacy trends that indicate any pharmacy
deviation in areas such as:
• Percentage of claims for less than 15 NDC numbers
• Percentage of claims that are refilled
• Total number of claims
• Percentage of high dollar claims
• Average prescriptions per member per month.
The content of the PEAR is reviewed annually to evaluate utilization, cost changes, market changes, and
the results of our monitoring efforts.

Louisiana Medicaid Page 116
© 2022 Caremark. All Rights Reserved.
ON-SITE / RETROSPECTIVE AUDITS
CVS Health designed our on-site procedures to verify the accuracy of claims submitted through
observation of original records including, among other things, prescription hard copies and patient
signature logs. On-site auditors will provide education to the pharmacy staff on LDH’s policies,
procedures, DUR programs, and proper billing methods, drug stock reviews, partial and return-to-stock
procedures, and more. We will conduct audits on a minimum of 5% of LDH’s pharmacies.
We are committed to identifying and eliminating drug diversion and insurance fraud. Our retrospective
audit analysis, including on-site audit and investigational audits, helps identify and eliminate fraud, waste,
and abuse.
Our on-site auditing process uses a proprietary program that performs a systematic review of the claims
history and automatically flags claims meeting specific criteria. The entire claim record, as transmitted by
the pharmacy and subsequently adjudicated by us, is made available at the audit site allowing the auditor
to deviate from the original audit plan as the situation dictates.
The audit function is also educational. Auditors will answer questions about CVS Health and LDH, inform
pharmacists about LDH’s programs and policies, and relay pharmacists’ concerns back to us. Educational
material is provided to all pharmacies to assist in improved program performance and to prevent future
point-of-service and submission issues.
Our on-site auditing process includes a systematic review of the pharmacy’s claims history. Specific
claims to be reviewed are selected by algorithms, which identify claims that meet specific criteria. Claims
may also be selected subjectively by the auditor for any number of reasons including the presence of
unusual trends. Claims may be chosen for audit based on, but not limited to, the following criteria:
Audit Criteria
• High dollar claims
• Quantity change within a prescription number
• High volume of claims per Enrollee
• High volume of controlled substances
• Unusual or unlikely drug combinations
• Apparent high dose
• “Doctor DAW” code claim submissions
• Compliance with FDA Risk Management Program requirements
• Quantity dispensed is within plan limits
• High number of refills
• Compliance with State and Federal laws and rules
• Amount paid for compounds is appropriate
• Random Claims
• Return-to-stock procedures (procedures for reversing claim billings for prescriptions not picked up)
Discrepancies
• Insufficient directions (e.g. UAD)
• Missing prescription
• Overbilled quantity
• Generic dispensed, brand billed
• Different drug billed
• Drug inventory shortage
• No signature log
• Cut quantity

Louisiana Medicaid Page 117
© 2022 Caremark. All Rights Reserved.
• Inaccurately billed compound
• Invalid prescription
• Wrong directions on dispensed prescription
• Invalid use of DAW codes.
PROACTIVE EDUCATION AND REPORTING EFFORTS
The Pharmacy Performance Department uses an educational and informative approach to foster positive
interactions between our audit staff and the retail pharmacy staff. Whether the audit-related event is
conducted face-to-face (on-site), through the mail (investigative), or by telephone (Daily Review or
Compound Review), we require our audit staff to complete every interaction with an educational
component.
This consistent interactive closure to an audit review, regardless of audit type, provides a professional,
proactive ending, allowing retail pharmacy staff and our audit staff to discuss preventive measures for
future issues and situations. This non-confrontational approach is well-received by pharmacies and
improves longer-term audit goals, such as improving the sentinel effect of avoiding similar discrepancies
from occurring in the future with the same pharmacies.
The sentinel effect, or the overall outcomes due to initial pharmacy audits/recoveries/education that
trigger corrective behavior in pharmacies for future claims’ submission and behavior, are difficult to
measure. Many organizations tout a 1% decrease in potential FWA spend. We achieve this by providing
the playbook we use to the pharmacies below, in addition to letting them know that CVS Health is actively
monitoring to catch errors when they occur so LDH and patients are not harmed.
Other educational efforts incorporated by Pharmacy Performance audit staff include:
• Written Education – Quarterly distribution of proactive audit tips based on retrospective patterns to
retail chains/PSAOs/independent pharmacies
• Face-to-Face Education – Participation in:
− Wholesaler/independent trade shows – face to face delivery of reports and audit presentations to
pharmacy owners
− Retail chain shows – face to face delivery of reports to all tiers of pharmacists (store, district, and
regional)
− Annual industry conferences – face to face meetings providing data and educational information
to corporate contacts of pharmacies geared toward the shared goal of eliminating fraud, waste,
and abuse
• Mis-fill Identification and Reporting – Reports to corporate contacts to collaborate toward
eliminating clinical dispensing issues to improve overall patient care.
Our dedicated audit staff will work closely with the LDH and its affiliated Bureaus, Offices, and
Committees, as well as our internal departments to ensure we provide the required information in a timely
manner and we are responsive to your needs. While we work with LDH through our contracted Louisiana
Medicaid MCOs, we welcome a direct relationship.
We believe that in a direct relationship with LDH it is important to know current challenges that could
impact the way that LDH considers potential formularies and edits. Therefore, we will provide reporting
that not only show the audit activities performed on behalf of LDH, but also provides insights into the
specific issues that are being uncovered at Louisiana pharmacies. CVS Health believes that reporting
information to identify new POS edits for commonly found errors will help guide pharmacies to high
quality care by preventing errors from occurring.
CVS Health also proposes that we form a relationship with a Subject Matter Expert at LDH that oversees
potential pharmacy cases that contain potential elements of FWA. We believe that when potential FWA is

Louisiana Medicaid Page 118
© 2022 Caremark. All Rights Reserved.
identified through tips, data analysis, or other means, we will want to create a deconfliction process,
where the underlying information is sent to LDH. We will follow LDH direction on whether the Pharmacy
Performance Department should investigate the issue or whether the Medicaid Fraud Control Group will
perform an investigation. CVS Health would be willing to provide data on the pharmacy activities through
an RFI (Request for Investigative Assistance), to assist the state in performing their review. We are
offering to give a more global view of the pharmacy should the State criminally pursue a pharmacy.
• Security and privacy: Describe the proposed approach to meet the requirements in Section
2.1.23.
CVS Health confirms that it is in compliance with all applicable State and Federal laws, rules, regulations,
and will fully comply with any and all Federal, State and LDH audit requests. Our Provider networks are
in compliance with all applicable Federal and State laws, and will be contracted in full adherence to the
State Plan. Our Provider Agreements require all participating retail pharmacies to agree in writing to
comply with all applicable federal and state laws and regulations.
We require all third parties utilized to comply with all federal and state privacy and security laws as well by
requiring Business Associate Agreements and conducting vendor assessment audits of the third parties
handling PHI regularly. We have a robust library of privacy and security policies which are reviewed
annually to help ensure compliance with all regulation changes and provide training to all employees
upon hire and annually thereafter. Additionally, our annual corporate training program includes a module
that provides all employees with an overview of HIPAA and employee responsibilities.
We have numerous established internal policies and procedures which relate to the appropriate use,
disclosure, confidentiality, and security of protected health information (PHI) required specifically under
HIPAA. The policies and procedures that specifically address disclosure of PHI include:
• Permitted uses and disclosures of PHI
• Verification/authentication of the entity and/or individual that is requesting PHI
• Minimum necessary evaluation procedure prior to use or disclosure of PHI
• Safeguarding PHI
• Use and disclosure of PHI as a Covered Entity or Business Associate
• Notice of Privacy Practices
• Disclosure for public health, health oversight, abuse and neglect, legal, or law enforcement purposes
• Confidential Communications
• Individual’s rights regarding PHI
• Privacy and Security training
• Confidentiality
• Rights to Privacy
• Privacy and Security Employee Sanctioning.
Data Security Standards
We have implemented a four-tiered security system to protect member confidentiality. Security is at the
desktop, server, database, and table levels. When a member is identified for inclusion in a health
improvement program, that member’s demographics and member-identifying information are stored in a
separate, secured table, and an encrypted member key is used to identify the member’s record with the
various data sets. Access management privileges are formally authorized and controlled, allocated to
users on a need-to-use and event by event basis for their functional role and documented for each
system. Authorization decision records shall be retained for 7 years from date of action. We also utilize
several system value parameters that control the validation of user passwords. Passwords carry an

Louisiana Medicaid Page 119
© 2022 Caremark. All Rights Reserved.
expiration date of 90 days. Moreover, paper shred bins are provided throughout locations for staff to
dispose of sensitive printed materials (such as mailing lists).
Appropriate procedures and measures are in place to encrypt sensitive data transmitted over public
networks in conformance to the specifications of FIPS 140-2 and to encrypt PHI and PII at rest in
compliance with all applicable regulatory requirements and standards so that it cannot be accessed by
unauthorized persons.
CVS Health employs encryption technologies with minimum key lengths of 128-bits for symmetric
encryption and 1024-bits for asymmetric encryption. A documented policy for the management of the
encryption keys and associated processes adequate to protect the confidentiality and privacy of the keys
and passwords used as inputs to the encryption algorithm is in place.
Security Incident Reporting
We have security policies and procedures in place for the reporting of security incidents as required by
federal or state law. Depending on the nature of the incident and, in particular, whether it resulted in an
unauthorized use or disclosure of PHI, we will report the security incident within ten (10) business days
from our Privacy Office becoming aware of the incident, or otherwise on a periodic basis, such as monthly
or quarterly, as agreed to with LDH. We will assume liability for our actions or inactions in this regard to
the same extent and subject to the same terms and conditions, as with respect to the performance of its
other contractual obligations as specified in our services agreement with the client.
We have established accounting of disclosures policies and procedures and tracking systems with a full
team of investigations support in the Privacy Office that address the requirements under HIPAA for
responding and resolving any complaint, question or determined issue. This includes notifying the
appropriate covered entity in the event that a breach occurs. These policies also consider the required
turnaround time for reporting disclosures, required involvement of the Privacy Officer, and invoke
appropriate components of the sanction policy.
Auditing Compliance
LDH shall have the right to audit compliance with (i) CVS Health’s data protection and information
security obligations set forth in this Agreement and Service Provider’s own internal policies, and (ii) the
terms of this Agreement, and shall grant LDH or its representative such reasonable access to its offices,
LDH specific records, LDH specific files and facilities as LDH or such representative may request so long
as it does not jeopardize the confidentiality of any other CVS Health’s clients, on reasonable advance
written notice and upon mutually agreed upon dates, to occur no more than once per calendar year, as
requested by LDH.
• Reporting and quality assurance: Describe the ability to provide standardized and ad hoc
reporting.
We have a thorough understanding of reporting requirements as defined in the RFP; our understanding is
built on our extensive experience working with Medicaid programs including providing PBM services to
more than 50% of Louisiana Medicaid managed care Enrollees.
Information in our automated reports is fully accurate based on data from our source systems at the time
the reports are produced. We use a dedicated IS Quality Assurance (QA) team that conducts testing in
compliance with QA best practices. As part of our continuous improvement program, the QA team tracks
and reports defects as they are identified. Testing includes functional, integrated end-to-end, and
regression testing for new and existing application development. Regression testing is performed for the
major, online applications before every integrated release and includes both manual and automated

Louisiana Medicaid Page 120
© 2022 Caremark. All Rights Reserved.
processes. The adjudication regression test involves a large volume of claims that mimic production
claims and various functional tests. The combined testing process ensures functionality and operational
integrity, and is used to develop processes and production certification.
Data provided in the standard RxNavigator report templates involve pulling data from the data
warehouse. Since RxNavigator is a self-service tool, we support requests from users when submitted to
confirm if the data and/or report is correct by working with our RxNavigator developers, data warehouse,
and/or other internal teams.
IDENTIFYING AND REPORTING TRENDS
CVS Health continuously monitors data, trends, and results for all its operational areas. Each data set
rolls into a monthly dashboard that is reviewed and analyzed by the executive leadership team during a
monthly meeting. We analyze both medical management metrics, including several prior authorizations
requested compared to the number that met medical necessity. We also review and analyze operational
metrics, including monitoring claims inventory, denial trends, and front-end rejection trends to ensure that
our systems are functioning correctly, claims are processing correctly and timely, and provider payments
are being issued. We find our internal processes effective for identification and remediation of any areas
that require improvement.
DASHBOARD REPORTING
CVS Health executive leadership uses a dashboard to review and analyze high-level data and metrics at
a glance. We will use of a similar dashboard across all Louisiana MCOs, as it will provide a comparable
overview of the key aspects of the health plan’s success and opportunities to make sure Enrollees and
providers are receiving optimal service from CVS Health.
LEVERAGING REPORTING RESULTS FOR PROCESS IMPROVEMENT AND
CORRECTIVE ACTION
CVS Health identifies trends through our reports. Therefore, we take a closer look at what could be
causing those trends and how we can address them. Prescription trend generally is considered to have
three components: price, drug mix, and utilization. We evaluate trend to identify the relative contribution of
each component. Utilization has been the primary component of trend for several years and reflects a
number of demographic trends. The aging of the population and the increasing incidence of chronic
illness are major factors in increased pharmaceutical utilization in the United States. Utilization increases
also are related to changes in clinical guidelines, such as the revision of recommended cholesterol levels;
new indications; and new products and their promotion.
In the next one to three years, drug mix will begin to mitigate trend as the patents will expire for numerous
drugs that currently have high utilization. As generic alternatives become available for these drugs, it is
expected that their cost will decrease. We can help reduce these components of prescription trend
through conducting a comprehensive analysis of Louisiana Managed Medicaid current performance.
Through these periodic analyses, we can recommend a variety of program offerings that will help LDH
proactively manage their prescription drug benefit. On a monthly basis, we communicate with clients
regarding current clinical issues that have a potentially significant impact on drug spend. Through regular
communication with our account management staff, information on significant new products, top
therapeutic drug categories, changes in the marketplace (such as top drugs and drug trends), drug list
updates, and standard plan design recommendations are discussed. We also are able to forecast the
potential impact of new product lines. Our proactive use of information will enable you to better manage
your drug spend and be better informed when new, potential blockbuster products enter the market.
Investing in Technology – Enhanced reporting provides our clients with integrated pharmacy and
medical data, the ability to report on interventions, further tying interventions to outcomes.
Data mining, or using your actual data for analyses, is common practice at CVS Health. We want to
ensure you can make the most of cost and plan management opportunities available through your

Louisiana Medicaid Page 121
© 2022 Caremark. All Rights Reserved.
pharmacy benefit. To assist in your decision making and further our commitment to improve health and
reduce total costs for your organization, we have developed a proprietary model, the Personalized
Opportunity Analysis, to estimate savings opportunities and the potential Enrollee impact. The analysis
provides a unique executive summary of your data to provide customized pharmacy and health savings
estimates associated with the latest innovative plan designs and clinical solutions to reduce your overall
health care costs and improve Enrollee health outcomes.
ONGOING ANALYSIS & SERVICES
Our consultative services can play a major role in support of your strategic objectives for managing
pharmacy and total health care trend. Your Chief Operational Officer and Financial Manager/Analytic
Consultant will perform a range of investigation, research, and analysis to help you understand your
pharmacy and health care trends, provide best-in-class benchmarking with peers, and share analytic
insights regarding the marketplace and regulatory climate.
RxInsights Review
In addition to supporting your analytic needs through customized, LDH-specific planning and reporting
tools, your service team will meet with you regularly to review your custom RxInsights report. The
RxInsights report is the basis for identifying opportunities for improved plan performance and
collaborating on solutions to manage your pharmacy benefit. Specifically, RxInsights:
• Identifies additional strategies you can implement to improve benefit performance;
• Identifies year-to-date or quarterly trends associated with price, product, and utilization;
• Makes specific recommendations supported by data;
• Monitors the impact of any plan design or clinical strategies you implemented; and
• Provides benchmarks for and monitors the performance of your pharmacy benefit.
Trend Analysis
Understanding the drivers of trend is paramount to planning and enacting solutions to control those
drivers. We are positioned to identify the strategic components and address the action to combat trend.
We have a variety of analyses to help you understand the key drivers of your trend (e.g., compounds) and
shape the focus of where you want to implement solutions to counteract these drivers. Our analysis also
shows where there are positive trend drivers (e.g., improved adherence to diabetes drugs) that could be
increasing pharmacy costs but will lower overall health care costs due to medical cost savings.
Additional Ad Hoc Analysis and Reporting
LDH will have the support of an Analytic Consultant who can develop a variety of reporting, analysis, and
modeling. This could include insights into the demographics of your population and how they influence
pharmacy utilization. For example, an adherence demographics analysis quantifies how population
demographic factors can influence adherence for key therapies, including diabetes, hyperlipidemia, and
hypertension.
PROSPECTIVE ANALYSIS CAPABILITIES
We proactively monitor drug products in the pharmaceutical development pipeline, and our Clinical Affairs
team identifies key drugs for drug-level utilization and cost-forecasting analysis. Using this information, we
can create a pipeline budget impact report for LDH.
We develop assumptions based on guidance from external physician consultants and available clinical
data to estimate potential utilization of the pipeline drug product after launch. Utilization assumptions

Louisiana Medicaid Page 122
© 2022 Caremark. All Rights Reserved.
include estimated shift rates between any existing therapies and the new pipeline drug product. We then
identify potential utilizers among your Enrollee population using your actual prescription utilization data
where drug products currently exist to treat the targeted disease state. Disease state prevalence rates are
used to identify potential utilizing Enrollee populations where existing drug treatments are not available or
cannot be captured through prescription utilization data. Adjustments are also created for potential cost
and average duration of therapy based on manufacturer-supplied and other research-based information.
Along with our cost and utilization assumptions, your data is applied to a forecasting model to create cost
forecasts over a 12-month period for the pipeline drug product. Your Clinical Advisor can provide the
pipeline forecast reports quarterly, with consultation on formulary and clinical management strategies.
Additionally, your actual utilization and expenditure for pipeline products are tracked and reported for 12
months after launch. Our assumptions used in the forecasting model are transparent, so you can make
adjustments based on your unique plan and in consultation with your account team.
CLINICAL QUALITY REPORTS
CVS Health is committed to supporting you through fact-based decision making, which is why we have
developed key clinical reporting tools that provide you access to the information and insight you need to
better understand and slow the growth of drug spending in your organization. Our clinical management
reports provide timely summary information, derived from the system’s detail-level data, to answer
management and operational questions more completely and facilitate decision-making processes.
Listed below are available clinical management reports. Several of the reports offer summary- and detail-
level data, which may allow LDH to do its own customization if needed.
OPPORTUNITY ANALYSIS REPORTS
Using your claims data, proactive medication management opportunity reports provide, at a detailed level,
opportunities for safety, health, and savings. These reports can be requested at any time, as long as we
have three to 12 months of your claims data.
Safety Opportunity Analysis
The Safety Opportunity Analysis identifies opportunities of the various CVS Health programs designed to
promote safety. Our safety solutions avoid medication errors, overutilization, and misuse. Our point-of-
sale (POS) safety reviews serve as a front-line safety precaution against potentially harmful drug
interactions. Retrospective safety reviews provide an additional safety net to identify and correct
medication issues within 72 hours. Finally, our Prescription Safety Management Identification,
Intervention, and Investigation Solutions address potential fraud, waste, and abuse and support safe and
appropriate utilization. The Safety Opportunity Analysis is a comprehensive report that can be provided
upon request.
Health Opportunity Analysis
Through the Health Opportunity Analysis, we can impact members’ health and control your health care
cost. This analysis provides the comprehensive support, education, and tools to make positive health
care decisions. The Health Opportunity Analysis is a comprehensive report that can be provided upon
request and includes the following analyses:
• Health key metric benchmarks:
− Medication adherence
• Core program opportunities:

Louisiana Medicaid Page 123
© 2022 Caremark. All Rights Reserved.
− Adherence to drug therapy
− Evidence-based plan design
− Gaps-in-care pharmacy
• Enhanced program opportunities:
− Condition management
− Medication therapy counseling
Savings Opportunity Analysis
The Savings Opportunity Analysis demonstrates the effect of our programs which ensure members get
the right medication at the right cost. The program opportunities demonstrated in this analysis were
created to empower members to make informed decisions about their care and positively influence
prescribing habits, reducing unnecessary drug costs and waste.
• Savings key metric benchmarks:
− Generic dispensing rate (GDR) and substitution rate
− Mail dispensing rate
− Cost per utilizer
− Pharmacy trend
• Core program opportunities:
− Comprehensive generic solutions
− FastStart
− Preferred product messaging
− Dose optimization
− Quantity limits
• Enhanced program opportunities:
− Prior authorization (PA)
− Step therapy with post-PA
− Quantity limits with post-PA
− Drug Savings Review
Generic Opportunity Report (Supplemental Savings Report)
The Generic Opportunity Report provides:
• Opportunities that exist within your population to increase generic dispensing;
• Key performance metrics that identify opportunities to increase GDR and track progress throughout
the year; and
• A greater level of detail regarding generic utilization and opportunity areas for improved generic
utilization.
The Generic Opportunity Report lets you clearly see areas for improved generic substitution and generic
in-class alternatives, along with the drivers available to impact those areas.
ACTIVITY REPORTS
Activity reports can be requested on a monthly basis 15 days after month close.
Pharmacy Advisor Adherence Activity Report (Supplemental Health Report)

Louisiana Medicaid Page 124
© 2022 Caremark. All Rights Reserved.
Research shows that interventions tailored to specific patient characteristics typically outperform more
traditional approaches. By evaluating available LDH-specific data, we engage Enrollees to improve their
medication-taking behavior and help them on the path to better health. The Adherence Activity Report
provides detailed tangible measures of adherence such as persistency curves, first-fill drop-off rates,
medication possession ratio, and optimal adherence rates. The report was designed to provide additional
detailed adherence metrics within therapeutic classes related to the following chronic conditions:
• Asthma/chronic obstructive pulmonary disease (COPD)
• Behavioral health
• Benign prostatic hyperplasia (BPH)
• Breast cancer
• Coronary artery disease
• Depression
• Diabetes
• Heart failure
• Hyperlipidemia
• Hypertension
• Osteoporosis
• Parkinson’s disease
Pharmacy Advisor 30- to 90-Day Activity Report
To improve Enrollee adherence, we identify Enrollees who are filling 30-day supplies of medication to
treat diabetes and cardiovascular conditions. The 30- to 90-day program engages prescribers, with
Enrollee follow-up as needed, to convert Enrollees’ prescriptions from a 30-day supply to a 90-day
supply. The Pharmacy Advisor 30- to 90-Day Activity Report provides a summary of the intervention
activity.
Pharmacy Advisor Counseling Activity Report
Pharmacy Advisor Counseling represents our continuing commitment to improve health outcomes and
reduce overall health care costs for our clients. The success of Pharmacy Advisor relies on proactive
interventions by pharmacists, either at a retail pharmacy or through outbound phone calls from our
dedicated call center. The goal of Pharmacy Advisor Counseling is to improve adherence and close gaps
in care by engaging with Enrollees to create positive behavior change. We improve adherence by
interacting with Enrollees who are beginning new therapies or at risk of discontinuing their therapy. When
an Enrollee appears to not be taking all recommended medications to manage a chronic condition, a
pharmacist counsels the Enrollee about these medications and informs their physician about the gap in
care. The Pharmacy Advisor Counseling Activity Report provides a summary of counseling activity for the
following conditions:
• Behavioral health
• Breast cancer
• Cardiovascular conditions
• Depression
• Diabetes
• Osteoporosis
• Respiratory conditions
Drug Savings Review Activity Report

Louisiana Medicaid Page 125
© 2022 Caremark. All Rights Reserved.
The Enhanced Drug Savings Review evaluates the long-term retail and mail drug histories of Enrollees to
identify situations in which our pharmacists can assist prescribers in selecting the most appropriate
medications. A CVS Health pharmacist communicates with the prescriber while using Enrollee-specific,
evidence-based recommendations within 72 hours of the claim processing. The Drug Savings Review
Activity report provides a detailed look at the number of interventions and types of communications
occurring within their population during a defined period of time. The report shows intervention activity by
program while also making Enrollee-level detail available. Reporting is provided on the following
programs (when available):
• Appropriate therapy management
• Condition management
• Dose optimization
• GI therapy management
POS DUR Activity Report
The Point of Sale (POS) DUR Activity Report summarizes claim activity that produces a safety alert and
the number of impacted Enrollees. Key types of POS Safety Review edits available today are as follows:
• Apparent drug misuse
• Cumulative APAP (acetaminophen)
• Cumulative morphine
• Dose check multiplier
• Drug-age precaution
• Drug-disease precaution
• Drug-drug interactions
• Drug-gender alert
• Excessive controlled substances—multiple drugs
• Excessive controlled substances—number of therapies
• Drug-pregnancy alert
• Excessive duration alert
• High-dose alert
• Ingredient duplication
• Low-dose alert
• Multiple pharmacies
• Multiple prescribers
• Refill too soon
• Therapeutic duplication
• Underuse precaution
Retrospective Safety Review Activity Report
As part of the Retrospective Safety Review, retail and mail prescriptions are reviewed daily for
appropriateness, and the prescriber is notified with an actionable Enrollee-specific communication within
72 hours of the claim processing. The program increases prescriber engagement and Enrollee safety.
The Retrospective Safety Review Activity Report provide a detailed look at the number of interventions
and types of communications occurring within your population during a defined period of time. The report
shows your intervention activity by program as well as Enrollee-level detail. The report can include the
following programs (when available):

Louisiana Medicaid Page 126
© 2022 Caremark. All Rights Reserved.
• Drug interaction management
• High utilization
• Therapeutic duplication management
• Age-appropriate management
• Duration of therapy management
Prescription Safety Management Solution Activity Report
The Prescription Safety Management solution targets high-risk drug classes, focusing on controlled
substances and inappropriate use and misuse-related indicators such as polypharmacy, provider
shopping, and high total controlled-substance claims volume. On a quarterly basis, clinical pharmacists
evaluate controlled-substance claims and available supporting medical data to identify potential
medication misuse and inappropriate claims for appropriate intervention. During subsequent quarters,
pharmacists conduct follow-up activities using physician responses and current claims activity. Situations
identified as potentially inappropriate may be referred to LDH for further action. Your account team can
provide a Prescription Safety Management Solution Activity Report to demonstrate the number of
Enrollees affected by the program, number of physician and Enrollee letters sent, physician responses,
and case referrals.
OUTCOMES REPORTS
Pharmacy Advisor 30-90 Day Outcomes
This report provides outcomes for the Pharmacy Advisor 30-90 Day program, which is focused on
improving member adherence through prescriber and member engagement, to convert prescriptions from
30-day supply to 90-day supply.
This report provides outcomes for Core Medication Management and Pharmacy Advisor, our
comprehensive strategy to reduce member medical costs through unique solutions that improve
adherence and close gaps in pharmacy care. These solutions, delivered across all channels (retail and
mail), address the growing prevalence and cost of chronic conditions and promote member behavior
change and cost-effective medications to improve clinical outcomes and reduce overall health care
expenses.
Pharmacy Advisor Adherence Outcomes Report
The Adherence to Drug Therapy program helps adherent Enrollees stay on therapy and non-adherent
Enrollees return to therapy. After implementing this program, an outcomes report provides Enrollee
demographics, a summary of movement from suboptimal to optimal, a summary of health care savings
achieved through our adherence initiatives, and the number of interventions. The report is available
annually and updated monthly. A baseline period of 12 months is required to demonstrate financial
savings.
Dose Optimization Outcomes Report
After LDH has implemented the Dose Optimization program, this report demonstrates the total Enrollees
impacted by the program, claims summary, total savings, and additional detail including drug regimen and
program savings per regimen. This report can be requested at least one month after implementation.
Drug Savings Review Outcomes Report

Louisiana Medicaid Page 127
© 2022 Caremark. All Rights Reserved.
The Drug Savings Review is used by clients to offer their Enrollees near-real-time claims review to
increase safety and capture savings earlier. It is important for actively enrolled clients to understand the
effectiveness of programs through tracking of program outcomes and the subsequent savings impact.
Reporting can be provided on the following programs (when available):
• Retrospective claim edits are processed for retail and mail service claims in appropriate therapy
management, condition management, dose optimization, and GI therapy management.
• CVS Health pharmacists typically communicate with the prescriber within 72 hours of the claim using
Enrollee-specific, evidence-based recommendations.
Quantity Limits Outcomes Reports
The Quantity Limits programs ensure Enrollees are not using more drug quantity than medically
necessary. After implementing the Quantity Limits program, these reports allow you to quantify the
program’s impact within your population by providing the actual program savings. This allows us to review
program performance with you and determine if the criteria established needs to be updated to better
control Enrollee spending. These reports provide:
• An executive summary of claims and savings;
• Program activity at the drug class and drug levels; and
• Gross and net savings at the drug class and drug levels.
The reports specifically measure walkaways, claims reduced to quantity limits, and claims where therapy
paid over limit. The reports are available from your account team upon request.
Retrospective Safety Review Outcomes Report
The Retrospective Safety Review is used by clients to offer their Enrollees near-real-time claims review to
increase safety and capture savings earlier. It is important for actively enrolled clients to understand the
program’s effectiveness through tracking of the program’s outcomes and subsequent savings impact. The
Retrospective Safety Review acts as a safety net for situations that may have a negative clinical impact
on a Enrollee. Retail and mail service prescriptions are reviewed daily for serious drug-drug interactions,
and the prescriber is notified with an actionable Enrollee-specific communication within 72 hours of the
claim processing.
Safety and Monitoring Solution (SMS) Outcomes Report
SMS (Prescription Safety Management Identification, Intervention, and Investigation pillars) targets high-
risk drug classes, focusing on controlled substances and inappropriate use and misuse-related indicators
such as polypharmacy, provider shopping, and high total controlled-substance claims volume. The SMS
Outcomes Report provides the following information:
• Total Enrollees targeted
• Total case referrals
• Case summary
• Program savings
AD HOC REPORTING CAPABILITIES
We realize the positive edge that timely and insightful data and reporting can give you in shaping and
fine-tuning your pharmacy benefit to better serve your Enrollees. We also understand the need for this
type of reporting and personalized analytic consultation unique to your plan. We provide a comprehensive

Louisiana Medicaid Page 128
© 2022 Caremark. All Rights Reserved.
portfolio of automated reporting and business intelligence tools along with access to skilled Analytic
Consultants who are part of your account team.
Our Analytic Consultants and your designated client representatives have access to our electronic data
warehouse (EDW). The EDW facilitates storage, linkage, and rapid retrieval of prescription information
and other health data and advanced tools, such as statistical analysis system software, which allows
large amounts of data to be accessed faster than ever before. While traditional reporting gives the user a
historical perspective, we provide intelligent reporting—reports with built-in interactive features that
enable users to manipulate data with future projections and understand how to influence and shape those
developments.
In conjunction with your account team, your Analytic Consultant will provide you with specific data
analysis focusing on managing your organization’s pharmacy and total health care spending. This may
result in insights that promote appropriate utilization and minimize inappropriate usage. They will be
responsible for understanding your specific needs, working with your account team to coordinate
analysis, maintaining active contact with you to showcase and explain advanced analytic offerings, and
offering innovative solutions to manage your health care spending.
Using the data mined from our EDW and using additional resources from our Analytic Services staff as
necessary, our Analytic Consultants will work with LDH to help LDH make informed decisions related to
potential solutions and initiatives. Regardless of whether the decision results in a new plan design,
implementation of a safety program, trend management initiative, or change to your overall PBM
program, you can anticipate the expected results based on pre-implementation Enrollee impact and cost
estimates, and identify the achieved results based on post-implementation measurement of outcomes.
We strongly believe that most ad-hoc reporting needs LDH may have throughout the course of our
contract will be addressable through our user-friendly, online reporting tool, RxNavigator. If LDH requires
additional ad hoc reporting services, our Account Manager will work with LDH to be sure those reporting
requirements are met. CVS Health will complete requests for ad hoc reports by LDH or the MCOs within
two (2) business days of a request, unless an alternative response time is negotiated with LDH at the time
the request is made.
• Emergencies and disaster planning: Describe the proposed approach to meet the
requirements in Section 2.1.25.
In keeping with CVS Health’s commitment to provide the highest level of products, services and access to
care to our customers, CVS Health has in place comprehensive programs that support our business
operations and technology resiliency respectively.
ENTERPRISE RESPONSE AND RESILIENCY PROGRAM
The Enterprise Response and Resiliency (ERR) program is comprised of three core program areas: 1)
Program Governance, Risk and Compliance; 2) Business Continuity Management; and 3) Enterprise
Preparedness and Response. To drive the ERR strategy, CVS Health has an established Senior Director
and team dedicated to the program to ensure alignment with industry best practices and appropriate
priorities and capabilities are in place across the enterprise.
ERR is responsible for executing on the Enterprise Response Framework that includes response
recovery plans at the site, business and enterprise level.

Louisiana Medicaid Page 129
© 2022 Caremark. All Rights Reserved.
ENTERPRISE DISASTER RECOVERY PROGRAM
A full-time Corporate Information Technology (IT) Enterprise Disaster Recovery Director is responsible for
overall systems recovery planning, testing, measuring and reporting to the CIO any recommended
changes to systems recovery contracts, equipment, and procedures in order to meet changing recovery
needs. The Director has a team of analysts and advisors to assess architecture, compliance, metrics and
reporting and leverage new technology to improve recovery plans and capabilities. Additionally, the
Director manages IT-specific business continuity plans that follow the enterprise business continuity
standards.
BUSINESS CONTINUITY AND DISASTER RECOVERY OVERVIEW
CVS Health business units maintain lists of critical office locations and critical applications. These critical
locations and applications are those essential to our financial condition and/or ability to deliver core
products and services to customers, ensuring CVS Health can continue “helping people on their path to
better health.” ERR has site incident management plans to support all critical office location’s business
response and recovery operations as well as robust business continuity plans to ensure both physical and
technology recovery to continue their critical business operations and processes following a disaster or
crisis event. Critical customer services, such as claims and coverage verification, at multiple regional sites
back each other up.
Business impact analysis (BIA) is performed every 12, 24 and 36 months based on criticality and process
dependencies and are updated on an annual basis. During the BIA the maximum allowable downtime and
recovery time objectives are established for each business process. All process dependencies
(applications, vendors, etc.) and their requirements are captured. BIA’s are approved by two layers of

Louisiana Medicaid Page 130
© 2022 Caremark. All Rights Reserved.
leadership. Recovery strategy requirements are based on the outputs of the business impact and risk
assessment. Requirements are driven by resource and work load requirements over time.
Recovery strategies are developed for each business continuity plan to ensure:
• Protecting prioritized business processes, products and services;
• Ensuring sufficient recovery capability is in place based on pre-determined time frames;
• Stabilizing, recovery and resuming of critical processes and activities and their key dependencies;
• Mitigating, responding and managing impacts.
Business continuity plans (BCP) are in place for all critical lines of business. The BCP is developed and
includes the following, but is not limited to; activation procedures, notification procedures, loss of
locations, loss of technology, loss of staff, loss of vendor, loss of location, recovery strategy and
associated tasks, call lists, recovery teams, etc. Each BCP is approved by two layers of leadership
annually.
CVS Health documents its business continuity and disaster recovery plans using vendor-provided
continuity planning software. Periodic exercises test the contingency strategies identified in the plans.
CVS Health also maintains “on-demand” service contracts with reputable regional and national disaster
recovery specialty contractors who are familiar with our facilities, critical business operations, and
recovery priorities.
All IT applications have scheduled regular backups of key data. IT Infrastructure creates backups of
operating systems, programming products, databases, program and procedure libraries, and subsystems
such as IMS, CICS, DB2 tables, catalogs, and file system structures. Where backup media is in use, they
are transferred on a daily basis to a secure, climate-controlled, off-site storage location. Where media is
not used, data is replicated to an alternate site.
CVS Health maintains corporate data centers in Woonsocket, Rhode Island; Cumberland, Rhode Island;
and Scottsdale, Arizona that jointly support our computer systems and network. These data centers are a
critical part of day-to-day operations. An outage of one data center permits another to provide recovery of
critical applications and service to all CVS Health locations. The data center is a “hardened” facility
designed to protect the computer systems and minimize any disruption to normal processing.
DATA CENTERS RESILIENCY
CVS Health uses both an internal site and alternate site recovery strategy for the West data center,
located in Scottsdale, Arizona. Critical business functions running in the West data center are replicated
in real time to the data center in Woonsocket, Rhode Island. CVS Health also contracts with SunGard
Availability Services and Teradata for use of their hot sites during a disaster.
The Scottsdale, Arizona, data center is served by four 2,000 kva utility transformers fed from two separate
utility feeds via two utility automatic transfer switches. There are four 1,750 kw standby diesel generators;
each generator supports one of the four electrical systems: two 800 kva and two 1,000 kva UPS systems.
The Woonsocket, Rhode Island, data center is served by three 3,750 kva transformers fed from two
separate utility feeds via three utility static/transfer switches. There are four standby diesel generators:
two 1,750 kw CAT generators and two 2,000 kw CAT generators. The generators are supported by 10
450 kw UPS systems.
The Cumberland, Rhode Island, data center is served by two 3,750 kva transformers fed from two
separate utility feeds via two utility static/transfer switches. There are two standby diesel generators:
3,000 kw CAT generators. The generators are supported by six 700 kw UPS systems.

Louisiana Medicaid Page 131
© 2022 Caremark. All Rights Reserved.
The objective in the event of a disaster is to recover mission-critical business functions within four hours
of a declared disaster. Other noncritical but essential processes will be recovered within 24–96 hours of
the declaration. CVS Health achieves the four-hour recovery window by implementing a warm-standby
recovery solution that replicates critical production data from the West Coast data center systems to
redundant systems in the East Coast data center. The company also maintains contracts with vendor
recovery sites.
MAIL SERVICE PHARMACY CONTINUITY
Our mail service pharmacies are strategically located across the United States to minimize the impact of
any single event and to enhance delivery options. If one of our mail service pharmacies experience an
interruption in service, prescriptions can be diverted electronically to one of our other mail service
pharmacies for fulfillment. Our ability to shift volume is tested daily. Pharmacy workloads and staffing
levels are reviewed daily as part of normal business operations, and orders are moved between locations
as necessary if permitted by client contract.
SPECIALTY PHARMACY CONTINUITY
CVS Specialty pharmacies are strategically located across the United States and Puerto Rico. If one of
these pharmacies experience an interruption in service, prescriptions can be diverted electronically to one
of our other specialty pharmacies for fulfillment. The resulting prescription order is routed from the
alternate facility to the Enrollee using a courier or a means of transportation comparable to that used by
the mail service pharmacy.
CUSTOMER CARE CALL CENTER CONTINUITY
In addition to backup capabilities in CVS Pharmacy locations, we maintain redundant Customer Care call
center capabilities to ensure client support functions are not interrupted in the event of a disaster. CVS
Health operates several networked Customer Care call centers which are capable of transitioning calls
seamlessly—whether to adjust for continuous call management or to address an emergency situation at a
site.
INTERNET
Maintaining continuous operation of our information systems and Internet sites is critical to us and our
clients. We have comprehensive disaster prevention and recovery measures that are maintained at state-
of-the-art levels. These measures are focused on maintaining the integrity of our computer database,
claims processing system, telecommunications network, and Internet sites. To ensure our ability to re-
establish our Internet sites in the event of planned or unplanned outage, data is replicated in real time
from our primary data center to our recovery center for critical applications. Precautions and contingency
plans, in combination with disaster recovery analysis and business continuity staff and equipment plans,
ensure that Internet operations are always maintained at the highest possible levels.
TRAINING AND EDUCTION
CVS Health considers our business unit and IT resiliency to be a critical component and a market
differentiator. All CVS Health colleagues play a part in the recoverability of critical business processes. To
meet this challenge, CVS Health’s Resiliency teams have developed and maintain orientation training.
Specific training has been developed and maintained for key stakeholders, such as business continuity
administrators, recovery plan development, processes and procedures, ensuring preparedness for
exercising and crisis operations. Training is an annual requirement for identified key personnel and
recovery team members and highly recommended for all IT colleagues.
DATA SECURITY
Our backup and Disaster Recovery (DR) environments adhere to all the same security protocols as our
production environments. Annual DR tests help ensure systems and procedures are tested, including
features that prevent unauthorized access to Protected Health Information. This activity is included in our
annual SSAE 16 (formerly SAS 70) audit review. In the event of a disaster or emergency, CVS Health

Louisiana Medicaid Page 132
© 2022 Caremark. All Rights Reserved.
ensures all security protocols remain in tact at our fail over sites and call centers. We monitor who at CVS
Health, beyond assigned CVS Health Louisiana staff, have access to Louisiana data and ensure that only
those who are a part of the Disaster Recovery or emergency efforts can access the bare minimum
amount of data they need to perform their functions. As we recover from the event and return to normal
operations, our security team disables any access to Louisiana data from CVS Health Staff that were
used as a part of the recovery effort who are not a part of the CVS Health Louisiana team.
COMMUNICATION METHODS
Your Account Director will be your central point of contact for the most up-to-date information. The CVS
Health Enterprise Response and Resiliency team provides monitoring of potential events that could affect
Enrollee care and coordinates response. We coordinate response in the following ways:
When an emergency is declared, we have processes in place to cascade information to inform clients of
these situations. CVS Health has a program called SCC13 which is designed to help ensure Enrollees
have quick and easy access to their prescription medications when they are affected by a weather or
other emergency, or when they require an early fill of medication for certain common reasons.
Functionality is now available that eliminates the need for a pharmacist to contact the CVS Health
Pharmacy Help Desk (and/or the Health Plan Customer Care), or for the Enrollee to call Customer Care,
to obtain an override in certain situations. LDH can choose to implement this capability during initial
implementation and this would be available during any event where normal operations are impacted.

Louisiana Medicaid Page 133
© 2022 Caremark. All Rights Reserved.
CVS Health has a robust suite of resources and tactics to help Enrollees that are affected by disaster.
Some examples are shown below:

Louisiana Medicaid Page 134
© 2022 Caremark. All Rights Reserved.
CVS Health has established a coordinated communication method, integrated with all appropriate
government agencies/authorities, including CDC, FEMA, and DHS, who will be on the front lines if a
pandemic or emergency is declared. We will proactively interact with all impacted state boards of
pharmacy as we utilize our dedicated cross functional team established within our organization. Our
internal team will reach out in a preplanned, coordinated manner to all stakeholders (including MCOs and
LDH) in our national pandemic/emergency response efforts, providing strategic direction and information
to our organization and impacted customers to limit disruption and maintain continuity of prescription
services.
In addition to comprehensive recovery planning, we have several linked, regional call centers and
pharmaceutical distribution centers (both PBM and specialty) across the U.S. In the case of a pandemic –
or a disruption due to other factors – that would cause either regional isolation or quarantine, we would be
in a position to seamlessly redistribute our work to another part of the country through electronic means
without significant disruption to our clients or their Enrollees. Through this process, we will work with our
vendor partners to ensure the security of our supply chain of essential medications and other critical
supplies.
EXERCISES AND TESTING
Exercises of recovery plans and capabilities are performed annually. Recovery of all critical functions is
performed at least annually. Exercises include testing of applications, network connectivity, and claims
transmission. Issues identified during these exercises are recorded and tracked until resolved. Our
backup facility has the processing capacity to performing all production processing.
Maintenance of the data center recovery plan is performed frequently, with disaster recovery and
business continuity plans reviewed, updated and tested annually. After action reports are developed

Louisiana Medicaid Page 135
© 2022 Caremark. All Rights Reserved.
following each exercise, included is a summary of successes, opportunities and a detailed action plan. A
copy will be made available to LDH.
Annually, IT validates the ability to perform a fully integrated alternate site recovery of critical IT
applications and services. The scope of the disaster recovery exercise is to activate the recovery systems
at our disaster recovery site and validate full functionality of the recovery systems and data. We conduct a
full integration test of our data center. The team recovers all critical applications and data under the
RTOs. The IT Telecommunications team maintains special equipment, circuits, and plans that will allow
them to connect a defined subset of critical offices.
Disaster recovery testing is performed throughout the year, with the latest test performed July 11, 2020.
There were no significant disaster recovery findings. Recovery exercises include identifying test
objectives, dates, location, participants, along with management approval of both pre and post exercising
objectives and results. Any deviations, issues or problems identified during exercising are documented
and seen through to resolution. Process improvements are implemented on an ongoing basis.
Business continuity testing’s is performed throughout the year. The Enterprise Response and Resiliency
team performed a functional test of alternate workplace capabilities (desktop, network, voice, resource
planning, call recording, etc.) utilizing the Mobile Recovery Unit (trailer) at our Customer Care Call Center
location. The purpose of this exercise was to demonstrate CVS Health’s capability to relocate to an
alternate location and continue work operations. The test occurred over a three (3) day period including
one (1) pretest day and two (2) user testing days. Call Center agents participated in the test and
successfully tested the capability of performing inbound/outbound calls in the Mobile Recovery Unit with
no impact to operations.
• Continuity of Operations Plan (COOP): Describe the proposed approach to meet the
requirements in Section 2.1.26.
As a critical infrastructure organization which millions of Enrollees depend upon to obtain needed
medication, we have a responsibility to ensure minimum disruption in providing Enrollees access to their
medication in the event of an emergency and/or disruption. We have comprehensive incident
management and business recovery plans in place to respond to potential disasters or service
interruptions in order to ensure continued operations to serve our clients and their Enrollees. We have
implemented these plans on a number of occasions over the past several years as a result of natural
disasters, emergency situations, etc.
CVS Health will work directly with LDH to collaborate with you on initiatives for an emergency/disaster
solution. Your CVS Health Account team discusses and engages with internal business areas (that
include regulatory affairs, operational areas, etc.) to take suggestions back to LDH and the MCOs as
options to mitigate any disruption of pharmacy services in the event of a disaster or other emergency
event . We work collaboratively with all parties to determine an appropriate course of action based on the
outcomes from our initial meeting with LDH and the MCOs. CVS Health will provide daily updates to LDH
and the MCOs on the current status of recovery, discuss what measures have been implemented, how
effective they have been and share pharmacy processing statistics . As changes are needed to the
agreed upon mitigation, CVS Health works with LDH and the MCOs in daily meetings to suggest
alternative approaches and will implement them as requested by the State.
The CVS Health Enterprise Response and Resiliency (ERR) team is a critical, centralized resource to
lead enterprise efforts during disruptions such as hurricanes and help the organization return to normalcy
by managing risk. The work of this team translates directly into support for Enrollees, customers, and
clients throughout rapidly developing weather events, power outages, etc. Companywide, colleagues
from dozens of departments (such as retail, network, IT, etc.) work around the clock to ensure colleague
and Enrollee safety, monitor structural soundness, and ensure customers’ medication needs are met.

Louisiana Medicaid Page 136
© 2022 Caremark. All Rights Reserved.
CASE STUDIES – DISASTER RECOVERY AND BUSINESS CONTINUITY
The following include some case studies of CVS Health’s ability to activate and execute its DR/BC plan:
In 2017, our ERR Command Center worked for several weeks to keep enterprise-wide areas informed of
the hurricane situation (Irma and Maria). Twice-daily situation reports included weather, at-risk facilities,
action planning by businesses, store operations, logistics, facilities, and loss prevention.
Hundreds of our facilities and thousands of our colleagues across our enterprise in Texas, Florida, and
Puerto Rico were impacted by the 2017 storms; however, we remained committed to providing continued
care to our Enrollees and clients. Highlights of our support included:
• Approving one-time emergency refills of a 10-day supply of medication for PBM Enrollees in affected
areas and availability of our Pharmacy Help Desk for immediate overrides;
• Sending CVS Pharmacy reminders to fill prescription medications in advance of storm impacts via
automated calls and mobile app and text alerts;
• Shifting dispensing and Customer Care to alternative facilities, expanding operating hours and shift
coverage, and when possible coordinating shipping to safer alternative addresses;
• Stationing Mobile Rx, our mobile pharmacy trailer, in impacted areas, where customers could pick up
their prescriptions, purchase over-the-counter medications, and receive recommended vaccines;
• Working with local, state, and federal partners to coordinate critical needs for our business, including
arranging for a jet to deliver emergency medications to long-term care facilities in Houston,
coordinating delivery of specialty medicines by ambulance to a hospital for a Enrollee with pulmonary
arterial hypertension in Florida;
• Collaborating with local officials and recovery organizations to assess products we could donate (e.g.,
food, water, medical supplies) to help with immediate needs; and
• Donating upwards of $10 million via CVS Health Foundation to support first responders, disaster
relief, American Red Cross, and our employee relief fund.

Louisiana Medicaid Page 137
© 2022 Caremark. All Rights Reserved.

Louisiana Medicaid Page 138
© 2022 Caremark. All Rights Reserved.
These examples demonstrate how CVS Health has the ability to recover from an emergency event or
disaster and continue to serve Enrollees in getting their prescriptions filled. We bring the same level of
expertise and rigor to Louisiana as a part of this engagement.
1.8.9 Innovative Concepts and Value-Added Services
LDH is interested in exploring value added services the Proposer may offer. The Proposer is
encouraged to work with LDH as well as the MCOs to identify and propose value-added services
that may apply to MCO-specific populations. LDH may approve the provision of value-added
services offered by the Proposer throughout the term of the Contract. The provision of value-
added services shall be subject to the explicit written approval of LDH.
The Proposer may present innovative concepts for consideration. The Proposer may present
value-added benefits for LDH approval.
We’re challenging the status quo of the health care industry with new technologies, business models and
partnerships. CVS HealthHUB® locations allow us to bring care close to home — right to the communities
where your members live and work. They’re another unique touchpoint that allows us to engage with
members more frequently, so we can help them take the right healthy actions.

Louisiana Medicaid Page 139
© 2022 Caremark. All Rights Reserved.
CVS HealthHUB locations create a new health engagement model. The CVS HealthHUB location format
combines the best of today’s CVS Pharmacy with the future of accessible, lower-cost health services and
more trusted advice.
CVS HealthHUB locations are the first- of-their-kind, community-based stores focused on helping consumers
get well and stay well. They offer a broader range of health care services, wellness products, trusted advice
and personalized care — all conveniently located within a local CVS Pharmacy.
A care concierge acts as a one-stop shop for your members, helping them understand benefits, access care,
fill prescriptions, seek follow-up care, and identify other types of care. The care concierge helps members and
their families get started on their paths to better health.
Expanded pharmacy services
We’re amplifying the success of CVS pharmacy solutions to offer the following expanded services at CVS
HealthHUB locations:
• Pharmacist diabetes education sessions — Program designed to help patients with diabetes better
manage their condition through education. Patients are offered a 30-minute in-person consultation to offer
disease education and support.
• Personalized patient counseling — Patients who may benefit from additional smart glucometer counseling
are offered this service by pharmacists.
• Blood pressure screening and coaching — Diabetic patients are offered a blood pressure screening by a
CVS pharmacist with follow-up to their PCP or prescriber for out of range readings.
• Key points in care — Pharmacist-driven educational outreach for patients having been identified as being
at a critical juncture in care, for example starting insulin. Patients can receive additional counseling in-
store or by phone.
• Lifestyle modifications – smoking cessation — Patients or caregivers can engage with pharmacists to
help them develop a plan to quit smoking.
• Personalized Rx support — Pharmacists, with Pharmacy Tech support, to manage a panel of high-risk
and cost patients to engage the patient to better manage disease state and drive behavior change to
reduce medical cost.
• Electronic medical record integration — Electronic medical records provide the pharmacy team additional
visibility into the patient records to make clinical decisions, document interventions, communicate with
their PCP, and provide a means for future billing of services.
Care Concierge
CVS Health’s HealthHub locations include a unique store colleague, the Care Concierge, to better assist your
members on their path to better health. The Care Concierge will engage with members across the acuity
spectrum to provide education and navigation to care, either within the HUB or in-network, that best fits their
needs. This engagement can take place either in-person or digitally
Some of these activities include assisting members in locating a health care provider in-network, scheduling
appointments for MinuteClinic check-ins, and helping members engage with our full suite of care

Louisiana Medicaid Page 140
© 2022 Caremark. All Rights Reserved.
management programs, including Transform Diabetes Care, AccordantCare skilled nurses, or simply helping
the member navigate to our Point Solutions Management partners.
Additionally, the Care Concierge at each HealthHub manages an event calendar, hosting group space events,
providing your members with free educational group classes and community partner programs.
Additional MinuteClinic offerings
MinuteClinic locations feature additional clinical services at CVS HealthHUB locations to help members with
certain chronic conditions, including disease identification, condition education and treatment guidance.
MinuteClinic locations offer:
• Chronic obstructive pulmonary disease services — Improve patient breathing with expanded services,
offering COPD patients nebulizer treatments in clinic for optimal assessment, treatment, and triage if
needed.
• Congestive heart failure patient assessment — Heart failure monitoring support, including ordering labs,
helping to manage comorbidities, guiding psychosocial care, providing education, and collaborating with
primary prescribers.
• Diabetic retinopathy screening services — Currently available in all locations. Clinical testing protocol to
screen patients with known diabetes using digital retinal photography in partnership with a third-party eye
care professional reading center.
• Phlebotomy services — In-house phlebotomy services allow for improved workflow efficiency for
providers and patients, avoids having the patient go elsewhere such as community reference lab and
mitigates clinical quality compliance drop-off.
• Chronic disease screening suite of services — Comprehensive chronic condition care offerings including
ordering labs, helping to manage comorbidities, guide psychosocial care, provide education, and
collaborate with primary prescribers.
• Obstructive sleep apnea screenings — Connection of patients through an innovative diagnostic pathway
to a Home Sleep Test (HST) vendor that ships the testing device to the patient’s home.
Innovative health services
CVS HealthHUB locations provide health care services in a more convenient, accessible and holistic manner.
Our expanded suite of health care services includes:
• Digital nutrition partnership — Noom, a CVS digital nutrition partner, is a behavior change and wellness
app that is available for customer enrollment.
• Sleep apnea end-to-end solution — Durable Medical Equipment specialists and HHC associates conduct
patient education, assist with mask fittings and initial set up consultation, facilitate product selection and
resupply, and provide follow-up phone calls, troubleshooting and compliance support related to sleep
apnea products.
Engaging product experiences

Louisiana Medicaid Page 141
© 2022 Caremark. All Rights Reserved.
In addition to offering personalized health and wellness services, we’re providing our customers with carefully
curated products. CVS HealthHUB locations will feature the following health and wellness product categories:
• Fitness — Fitness, physical therapy and yoga products targeting customers who believe that exercise is
part of a healthy lifestyle
• Cleanse and detox — Supplements, teas and related products targeting customers that aim to re-achieve
balance and/or remove toxins
• Personal emergency response — Technology targeting seniors to reduce risks associated with
independent living
• Trending nutrition — Supplements and consumables targeting customers that are facilitating their healthy
lifestyle through trending diet themes such as paleo and keto
• Honey and bee products — Honey and pollen products targeting customers that want drug-free solutions
to a variety of acute health needs such as sore throat and acid reflux
• Energy and performance — Fuel for athletes including electrolytes, glucosamine, BCAAs, caffeine and
protein
• Performance braces — Wrist, elbow, back, knee and ankle braces for customers that want a higher end,
performance-focused support product
• Calm — Products and supplements targeting stress and anxiety, for the 60% of customers that believe
being emotionally stable is part of a healthy lifestyle
• Diabetic compression — Compression garments focused on improving extremity circulation for people
with diabetes
• Memory and focus — Combination of new and existing products merchandised together to create a
destination for products that enhance cognitive performance
• Sleep apnea — Prescription full-solution apnea devices, accessories and kits for customers managing
sleep apnea
The following offerings can help member plans manage Medicaid drug benefit needs.
CLINICAL PROGRAMS
CONFIDENTIAL
HEALTHTAG
We can help health plans extend their reach to engage and retain members through our HealthTag program,
which offers better coordination and more comprehensive member care. Our channels can be used to
promote positive member behavior change and address opportunities to reduce health care costs. We have
industry-leading data and targeting algorithms that provide a near-real-time view into member behavior,
allowing us to better identify members who are most likely to positively respond to interventions.

Louisiana Medicaid Page 142
© 2022 Caremark. All Rights Reserved.
• Face-to-face delivery of health care improvement messages at CVS Pharmacy can effectively increase
member engagement and promote positive behavior change.
• Identifying health improvement opportunities through our real-time pharmacy data and clinical targeting
provides health plans with important information that can be used to better coordinate and improve
member care.
• Messages delivered at CVS MinuteClinic or the pharmacy prompt members to obtain necessary health
care such as screenings, vaccinations, and chronic condition monitoring. CVS MinuteClinic can also
provide convenient and low-cost acute care.
• Providing physicians with real-time pharmacy claims data can give them a more complete picture of the
member’s health.
CONFIDENTIAL
PHARMACY ADVISOR COUNSELING
that can improve adherence to chronic medications to manage the most common conditions in your
Medicaid population, including asthma, bipolar disorder, cardiovascular disease, depression, diabetes, and
schizophrenia, to reduce associated adverse events and total health care costs. We do this through
proactive one-on-one member counseling in person at retail or by phone. Our bilingual pharmacists, who
interact with members frequently, can bridge the knowledge gap by educating and promoting positive
behavior change among your population. Pharmacists counsel on the importance of taking medication as
prescribed and encourage enrollment in the plan’s disease management program, if appropriate. This
outreach targets members who are nonadherent or new-to-drug therapy—which is especially important for
those who are covered for the first time.
These interventions are delivered by retail pharmacists in store or by specially trained pharmacists at our call
centers for members who use other retail pharmacies. Pharmacy Advisor Counseling targets chronic, costly
conditions that drive the majority of health care costs. The program may also support HEDIS and/or state
quality measures related to asthma, behavioral health, and diabetes. Pharmacy Advisor is accredited and
recognized by URAC for best practices in engaging and influencing member health through positive behavior
change. Pharmacy Advisor Counseling draws insights from 1.5 million member interactions and ongoing
behavioral research to further improve quality. To demonstrate results, we provide clients with regular
member activity reports. By maximizing opportunities to interact with members, Pharmacy Advisor
Counseling is a powerful complement to existing programs.
HEALTH ADVISOR OVERVIEW
Chronic conditions continue to drive cost at increasing rates. Patients with a chronic conditions need help
managing their health outside of the traditional office visit; when they don’t receive that help, their clinical
outcomes are lower and their cost higher. And Health Plans recognize that they need to help. Moreover,
chronic care solutions in the market today are largely telephonic care management in nature and focus on
support, patient education, coordination of resources and self-management. Patients need more help when
the critical parts of their visit with a doctor are so short and very infrequent:
• Average American visits the doctor 4 x / year (http://info.wellframe.com/ebook-fight-point-solution-
fatigue.html)
• Average visit includes only 2 minutes average talk time on major topics
(http://info.wellframe.com/ebook-fight-point-solution-fatigue.html)
As a result patients leave the office confused or unsure what they need to do next. And the vast majority of
patients are asking for more help and/or resources to better manage their condition. Clients need a way to

Louisiana Medicaid Page 143
© 2022 Caremark. All Rights Reserved.
improve or even replace their current solution(s) with a cost-effective stepwise approach to substantially
improve care and reduce costs.
CONFIDENTIAL
To address this,
that empowers smarter care decisions by delivering
individualized next best actions through digital channels, provider outreach, 1:1 pharmacist counseling and
our unique CVS Health assets, including CVS HealthHUB locations to improve health outcomes and reduce
medical costs. Health Advisor leverages enterprise capabilities and medical claims, pharmacy claims and lab
data to drive higher engagement and better care delivery through a comprehensive behavior change
platform.
Based on a member’s risk profile, low-touch and high-touch channels are used to deliver next best actions.
Next best actions target key behaviors:
• Shifting site of care through avoidable emergency room
(ER) visits, using alternative sites of care where appropriate
[urgent care, telemedicine, primary care physician (PCP)],
adopting preferred labs and low-cost radiology centers and
using office/ambulatory surgery centers (ASCs) for low-
acuity procedures
• Improving non-emergent health outcomes and reducing
complications through preventive screenings, vaccinations,
reducing waste by using surgical best practices, reducing
readmissions and increasing usage of in-network providers
• Closing clinical care gaps through stop/modify a drug,
add/intensify medical therapy, condition/drug monitoring,
drug-drug interaction and medication adherence
Low-touch channels include provider fax, direct mail, email, SMS/text, interactive voice response (IVR), CVS
Pharmacy
®
prescription bag messaging (HealthTag
®
), and MinuteClinic
®
messaging (HealthTag).
High-touch channels include Pharmacist Panel – The high-touch delivery channel intensifies outreach for the
top 5 percent of high-risk members by providing proactive, ongoing support by a CVS pharmacist to deliver
better outcomes. Pharmacist Panel leverages behavioral insights and analytics to provide tailored education
to members. Intervenes proactively, up to 6 health interviews/consultations annually (face-to-face and/or
telephonically) for those high-risk members filling at CVS retail.
Note: Regular CVS visits are not required for the Health Advisor product to be effective. All campaigns are omni-channel, integrating a
handful of core member outreach channels with additional capabilities like Pharmacist Panel to engage with high-risk members who fill
at CVS Pharmacy.
Health Advisor may not be available in all states or for all lines of business; pending final legal review.
Health Advisor goes beyond adherence to impact behavior change and improve health outcomes:
• 15% improvement in positive behavior change improvement
• 12% reduction in unnecessary ER visits
• 18% reduction in high cost lab usage
• 8% reduction in out-of-network and non-preferred facility utilization.
Vulnerable Patient Index (VPI)

Louisiana Medicaid Page 144
© 2022 Caremark. All Rights Reserved.
The VPI tool targets interventions to the elements of excess medical spending that are responsive to
pharmacy-based interventions. The VPI stratifies members and determines a single risk result based on
safety score, adherence risk, and projected total cost. It identifies superutilizers—complex patients with or
without behavioral health issues as well as general needs. Interventions are based on the VPI result.
Members with a lower result are offered a targeted medication review (TMR) and adherence support.
Members with a medium result are offered a comprehensive medication reconciliation (CMR) and/or
behavioral health solutions. Those members with the highest result can receive coordination of care,
pharmacy home services, and medication management.
POINT-OF-SALE EDITS
Point-of-sale edits identify safety issues. Our system flags potential medication safety concerns at the point
of sale for quick action. Any time a prescription triggers safety issues, a real-time safety alert is delivered to
the dispensing pharmacy. Our pharmacists review claims not addressed at the point of sale within 72 hours
of adjudication to determine an appropriate course of action. Based on Medi-Span, more than 100 alerts are
covered within this program.
SPECIALTY DRUG PROGRAM
Our specialty drug program provides injectable and biotech drugs efficiently and cost-effectively through one
full-service source, offers member support and education, integrates drug utilization and compliance
programs, and offers PBM-based electronic claims processing. Our specialty management capabilities
address drug spending under both the pharmacy and medical benefits. We are the only specialty pharmacy
that integrates rare disease management—critical in controlling overall costs related to this small but high-
cost population. We are also the only company to provide specialty pharmacy access through our retail
stores—a program we call Specialty Connect.
Specialty Connect creates seamless access through any of our more than 9,000 CVS Pharmacy locations or
e-prescribing to any CVS Health pharmacy, within state restrictions. Once the prescription is ready, the
patient is alerted that our disease-specific CareTeam will call them, generally within hours. The CareTeam
includes pharmacy coordinators who deal with much of the administrative requirements for filling the
prescription. The CareTeam also includes pharmacists to manage the medication-specific discussions
including side effect management, injection training, and options for delivery. The patient can choose to have
the medication delivered to their home, or they can pick it up at their neighborhood CVS Pharmacy. The
clinicians on our Specialty CareTeam include disease management nurses and Coram nurses who support
those patients on infused medications.
With all of this additional clinical expertise, we have added to the clinical team available to help patients and
providers promote member health. NovoLogix gives clients greater visibility into claims under the medical
benefit for specialty drugs and provides a means to evaluate those claims for appropriate use and pricing.
Accordant Health Services offers care management for 17 rare, progressive conditions that have
approximately 1% prevalence, with average per member per year (PMPY) costs of about $23,000. No one
else offers the suite of condition management that Accordant has.
1.8.10 Proposed Staff Qualifications
Proposers should state job responsibilities, workload and lines of supervision for both Key
Personnel and General Staff. An organizational chart identifying individuals and their job titles
and major job duties should be included. The organizational chart should show lines of
responsibility and authority.

Louisiana Medicaid Page 145
© 2022 Caremark. All Rights Reserved.
Job descriptions, including the percentage of time allocated to the project and the number of
personnel should be included indicating minimum education, training, experience, special skills
and other qualifications for each staff position as well as specific job duties identified in the
proposal. Job descriptions should indicate if the position will be filled by a Subcontractor.
The Proposer should identify the individuals serving as key personnel, the resources proposed
for Key Personnel roles in Section 2.1.4, and the percentage of time directly assigned to the
project, should be identified.
Include full resumes of all proposed key personnel identified for key roles. Each person
identified for a role above should be included in the resume section. Each resume should
demonstrate the qualifications and experience relevant to the position proposed. Each resume
should include work history, the specific functions performed, and how the experience relates to
the assigned role. Résumés of all known personnel working or overseeing the LDH Pharmacy
Program should be included. Résumés of proposed personnel should include, but not be limited
to:
• Experience with Proposer.
• Previous experience in projects of similar scope and size.
• Educational background, certifications, licenses, special skills, etc.
Provide three (3) references for each proposed Key Personnel candidate demonstrating
experience in a similar role on one or more projects similar to Section 2. Scope of Work
requirements. Each reference should include:
• Name of the person to be contacted.
• Contact phone number.
• Client name and address.
• Brief description of work.
• Dates (month and year) of employment.
These references should be able to attest to the candidate’s specific qualifications.
If Subcontractor personnel will be used, the Proposer should clearly identify these persons, if
known, and provide the same information requested for the Proposer’s personnel, if requested
by LDH.
If any of the Proposer's named personnel is a current or former Louisiana State employee,
indicate the Agency where employed, position, title, termination date, and (in the redacted
proposal ONLY) the last four digits of the social security number.
CVS Health agrees in concept with the staffing requirements as noted in the RFP. At present we are not
including names and resumes. Given the highly competitive nature of this procurement and the Louisiana
state-based requirement, the hiring pool may be greatly reduced. Once the award is announced bidders will
have an opportunity to assemble a team with the best talent. As we work closely with the state during
subsequent stages of the project and begin to better understand in full scope the needed resources to fully
align objectives, we will add individuals with mutually agreeable backgrounds and experience to ensure the
business outcomes are delivered.
1.8.11 Veteran and Hudson Initiative Programs Participation

Louisiana Medicaid Page 146
© 2022 Caremark. All Rights Reserved.
The State of Louisiana Veteran and Hudson Initiatives are designed to provide additional
opportunities for Louisiana-based small entrepreneurships (sometimes referred to as LaVet's
and SE's respectively) to participate in contracting and procurement with the State. A certified
Veteran-Owned and Service-Connected Disabled Veteran-Owned small entrepreneurship (LaVet)
and a Louisiana Initiative for Small Entrepreneurships (Hudson Initiative) small entrepreneurship
are businesses that have been certified by the Louisiana Department of Economic Development.
All eligible vendors are encouraged to become certified. Qualification requirements and online
certification are available at:
https://smallbiz.louisianaeconomicdevelopment.com.
If a Proposer is not a certified small entrepreneurship as described herein, but plans to use
certified small entrepreneurship(s), Proposer shall include in their proposal the names of their
certified Veteran Initiative or Hudson Initiative small entrepreneurship Subcontractor(s), a
description of the work each will perform, and the dollar value of each subcontract.
During the term of the contract and at expiration, the Contractor will also be required to report
Veteran-Owned and Service-Connected Disabled Veteran-Owned and Hudson Initiative small
entrepreneurship Subcontractor or distributor participation and the dollar amount of each.
In RFPs requiring the compliance of a good faith subcontracting plan, the State may require
Proposers to submit information on their business relationships and arrangements with certified
LaVet or Hudson Initiative Subcontractors at the time of proposal review. Agreements between a
Proposer and a certified LaVet or Hudson Initiative Subcontractor in which the certified LaVet or
Hudson Initiative Subcontractor promises not to provide subcontracting quotations to other
Proposers shall be prohibited.
If performing its evaluation of proposals, the State reserves the right to require a non-certified
Proposer to provide documentation and information supporting a good faith subcontracting
plan. Such proof may include contracts between Proposer and certified Veteran Initiative and/or
Hudson Initiative Subcontractor(s).
If a contract is awarded to a Proposer who proposed a good faith subcontracting plan, the using
agency, the Louisiana Department of Economic Development (LED), or the Office of State
Procurement (OSP) may audit Contractor to determine whether Contractor has complied in good
faith with its subcontracting plan. The Contractor must be able to provide supporting
documentation (i.e., phone logs, fax transmittals, letter, e-mails) to demonstrate its good faith
subcontracting plan was followed. If it is determined at any time by the using agency, LED, or
the OSP Director that the Contractor did not in fact perform in good faith its subcontracting plan,
the contract award or the existing contract may be terminated.
The statutes (La. R.S. 39:2171 et. seq.) concerning the Veteran Initiative may be viewed at:
http://www.legis.la.gov/Legis/Law.aspx?d=671504.
The statutes (La. R.S. 39:2001 et. seq.) concerning the Hudson Initiative may be viewed at:
http://www.legis.la.gov/Legis/Law.aspx?d=96265.
The rules for the Veteran Initiative (LAC 19:VII. Chapters 11 and 15) and for the Hudson Initiative
(LAC 19:VIII
Chapters 11 and 13) may be viewed at:

Louisiana Medicaid Page 147
© 2022 Caremark. All Rights Reserved.
https://www.doa.la.gov/doa/osp/vendor-resources/hudson-se-veteran-initiatives/.
A current list of certified Veteran-Owned and Service-Connected Disabled Veteran-Owned and
Hudson Initiative small entrepreneurships may be obtained from the Louisiana Economic
Development Certification System at: https://smallbiz.louisianaeconomicdevelopment.com
Additionally, a list of Hudson and Veteran Initiative small entrepreneurships, which have been
certified by the Louisiana Department of Economic Development and who have opted to register
in the State of Louisiana LaGov Supplier Portal:
https://lagoverpvendor.doa.louisiana.gov/irj/portal/anonymous?guest_user=self_reg.
This may be accessed from the State of Louisiana Procurement and Contract (LaPAC) Network:
https://wwwcfprd.doa.louisiana.gov/OSP/LaPAC/vendor/VndPubMain.cfm.
When using this site, determine the search criteria (i.e. alphabetized list of all certified vendors,
by commodities, etc.) and select SmallE, VSE, or DVSE.
CVS Health's Supplier Diversity program, established in 2000, actively seeks diverse suppliers of products
and services to meet our operational needs. One of our primary means of recruiting and identifying diverse
suppliers is through active participation and membership with nationally recognized advocacy groups. The
program is designed to complement our commitment to providing outstanding service to our customers and to
recognize the critical role diverse suppliers have in our continued success.
At CVS Health, our Supplier Diversity Program helps us identify diverse suppliers of products and services
that support the needs of our clients and health plan participants. This program exemplifies our company’s
commitment both to sound business practices and to the communities we serve.
Our Supplier Diversity Program embraces Minority-and-Women-Owned Enterprises (M/WBEs), Veteran and
Disabled
Veteran Business Enterprises (V/DVBEs), Small Business Enterprises (SBEs), Disability-Owned Business
Enterprises (DOBEs), Disadvantaged Business Enterprises (DBEs), Historically Underutilized Business
Enterprises Zones (HUBZone), and Lesbian, Gay, Bisexual and/or Transgender Business Enterprises
(LGBTBE). As part of this program, we have a Diverse Retail Pharmacy Initiative that encourages diverse-
owned, independent retail pharmacies to become part of our network.
Diverse suppliers provide outstanding service and effective solutions in helping us achieve our company
mission to “improve the lives of those we serve by making innovative and high-quality health and pharmacy
services safe, affordable and easy to access.” We recognize that this program is essential to the continued
growth, development and success of our company and look forward to working closely with diverse suppliers
in all aspects of our business.
Our Supplier Diversity Program consists of two tiers. Tier I focuses on monitoring our purchases to help
ensure we have diverse suppliers providing quality goods and services. Tier II takes the program to a new
level by monitoring our large valued suppliers to help ensure diverse suppliers are included in their supply
chains. This two-tiered program further demonstrates our commitment to both the use of diverse direct
suppliers and to doing business with suppliers who are embedding diversity in their own supply chains.
Corporate Supplier Diversity partners with CVS Health business units as advocates for the integration of
supplier diversity into strategic procurement activities. In addition, we partner with national organizations to

Louisiana Medicaid Page 148
© 2022 Caremark. All Rights Reserved.
identify and develop diverse businesses and emerging entrepreneurs to strengthen the business communities
we serve. Organizations such as:
• National Minority Supplier Development Council - NMSDC
• Women’s Business Enterprise National Council - WBENC
• Disability:IN
• National Gay and Lesbian Chamber of Commerce - NGLCC
• United States Hispanic Chamber of Commerce - USHCC
• United States Pan Asian American Chamber of Commerce- USPAACC
• National Veteran Business Development Council - NVBDC
To learn more about our program, please visit, https://cvshealth.com/about/diversity/ supplier-diversity-
program.
ECONOMIC IMPACT
THROUGH OUR SUPPLIER DIVERSITY PROGRAM IN 2020
• $6.3 Billion production impact of our program
• $2.3 Billion wages supported
• 46,238 jobs supported
• $3.4 Billion in small and diverse purchase
SUPPLIER DIVERSITY SPENDING IN 2020
• $727 Million in Minority Businesses
• $415 Million in Women Businesses
• $44 Million in Veteran Businesses
• $2.8 Billion in Small Businesses.
OUR 2020 IMPACT IN LOUISIANA
State
CVS Health
Purchases
Total Output
Total
Wages
Total
Jobs
Jobs at Small &
Diverse
Suppliers
Taxes
Supported
Louisiana
$23 Million
$38 Million
$13 Million
287
170
$13 Million
Please refer to Section V Tab 5 for CVS Health’s 2021 list of diverse suppliers certified by the Louisiana
Economic Development Department.
1.8.12 Additional Information
As an appendix, Proposers should include a copy of the Continuity of Operations Plan.
Please refer to Section V Tab 4 for a copy of CVS Health’s Business Continuity Plan.
1.8.13 Cost Proposal

Louisiana Medicaid Page 149
© 2022 Caremark. All Rights Reserved.
Proposers shall complete a cost proposal in format of the cost template form (See Attachment III)
for each year of the contract to demonstrate how cost was determined. Proposers must
complete a cost proposal to be considered for award. Failure to complete will result in the
disqualification of the proposal.
CVS Health confirms. Please refer to Section IV for CVS Health’s Cost Proposal.
1.8.14 Certification Statement
The Proposer must submit a Certification Statement (See Attachment I) signed by the company
official or agent duly authorized to sign proposals or contracts on behalf of the organization. A
certified copy of a board resolution granting such authority shall be submitted with the
Certification Statement if the Proposer is a corporation. The Proposer represents and agrees
that in reviewing and completing this response it has accurately disclosed - and in the future will
accurately disclose – all interests of Proposer. Proposer also represents and agrees that it has
disclosed - and will disclose - any activity, policy, or practice of which Proposer is aware that
presents a conflict of interest with the performance of its obligations hereunder.
CVS Health confirms. Please refer to Section V Tab 6 and Section V Tab 7 for the Officer’s Certificate of
Authority.
