
Screening, Symptom Recognition
and Referral to Treatment
for Eating Disorders in
Pediatric Primary Care Settings

Holly C. Gooding, MD, MSc
Physician - Division of Adolescent/Young Adult Medicine
Boston Children’s Hospital
Assistant Professor of Medicine and Pediatrics
Harvard Medical School
Course Instructors
Sara Forman, MD
Director of Outpatient Eating Disorders Program
Clinical Chief, Division of Adolescent/Young Adult Medicine
Boston Children’s Hospital
Assistant Professor of Pediatrics
Harvard Medical School

Disclosure Statement
• No one involved in creating this webinar has
any financial disclosures or conflicts of interest
to report

Webinar Orientation
• General chat questions/comments will be visible
only by webinar hosts and support staff
• If you need tech support:
1) Click on the Chat icon at the bottom of the webinar
screen
2) Click “Tech Support” from the drop down menu next
to “To:” and type your message
3) OR call Nick at 617-839-4162

Learning Goals
1. Describe eating disorders (EDs) and gaps in care among
youth in the United States
2. Discuss potential signs of EDs in youth as well as options
for ED screening within pediatric primary care
3. Describe treatment options for youth with EDs
4. Demonstrate a tool to help you refer patients to local
specialists when screening indicates concern

Academy for Eating Disorders:
“The Purple Brochure”
(Academy for Eating Disorders, 2016)

Question:
Who do you think of when you picture
the stereotype of someone with
an eating disorder?

Eating Disorders Overview
• Serious mental illnesses with a wide range of medical
complications
• Common across gender, sex, age, race/ethnicity,
socioeconomic status, and body shapes/sizes
• People of all weights can engage in unhealthy weight
control behaviors
• Disparities in diagnosis, treatment, health outcomes
• In children: failure to gain expected weight or height or
interruption of pubertal development should raise concern
(Academy for Eating Disorders, 2016)

Eating Disorders in
Diagnostic and Statistical Manual-5 (DSM)
• Anorexia nervosa (AN): Restriction + disturbance of body
image + fear of gaining weight
• Bulimia nervosa (BN): Binge eating +
purging/compensatory behavior + self-evaluation unduly
influenced by shape/weight
• Binge eating disorder (BED): Binge eating
without purging
(American Psychiatric Association, 2013)

• Avoidant/restrictive food intake disorder (ARFID):
Weight loss, nutritional deficiency without weight or
shape concerns; , food consumption is limited based on
the food's appearance, smell, taste, texture, or a past
negative experience
• Other specified feeding & eating disorder (OSFED): Does
not meet full criteria for other eating disorders, but has
specific disordered eating behaviors (e.g., restricting
intake, purging, binge eating)
(American Psychiatric Association, 2016)
Eating Disorders in
Diagnostic and Statistical Manual-5 (DSM)

Prevalence
Diagnosis Lifetime Prevalence
(13-18 year olds)
Anorexia Nervosa 0.3%
Bulimia Nervosa 0.9%
Binge Eating Disorder 1.6%
(Swanson et al., 2017)

Prevalence
(Swanson et al., 2017)
Boys of color > White boys
Lesbian, gay, bisexual youth
> Heterosexual youth
Transgender youth > Cisgender youth

Mortality
• EDs have among the highest mortality rates of any
psychiatric disorder
• Increased risk of suicide associated with all sub-types
of EDs
• Standardized mortality ratios (SMRs):
(Swanson et al., 2017)
(Arcelus et al., 2011)

Stereotypes & Access to Treatment
• EDs are underdiagnosed and undertreated
• Misleading stereotypes that only thin, white, affluent
females are affected by eating disorders can lead to under-
recognition in other groups
(Merikangas et al., 2011)
(Sonneville et al., 2018)

Disparities in Treatment
Perceived need
for ED treatment
ED diagnosis Past year ED
treatment
Males < Females Males < Females Males < Females
Non-affluent < Affluent Non-affluent < Affluent
(Sonneville et al., 2018)

Eating Disorders in Your Office?

Importance of Early Detection & Intervention
• Early detection and intervention are critical to
reversing medical complications and improving
psychiatric outcomes
• Primary care providers can support patients in
accessing treatment and achieving recovery

• Significant weight changes/fluctuations
• Sudden changes in eating behaviors
• Sudden changes in exercise patterns,
excessive/compulsive exercise
(Academy for Eating Disorders, 2016)
Consider Screening for EDs
if You See Signs Including…

• Body image disturbance, drive to lose weight despite
low/normative weight
• Abdominal complaints in the context of weight loss
behaviors
• Use of appetite suppressants, laxatives, diuretics, etc
.
(Academy for Eating Disorders, 2016)
Consider Screening for EDs
if You See Signs Including…
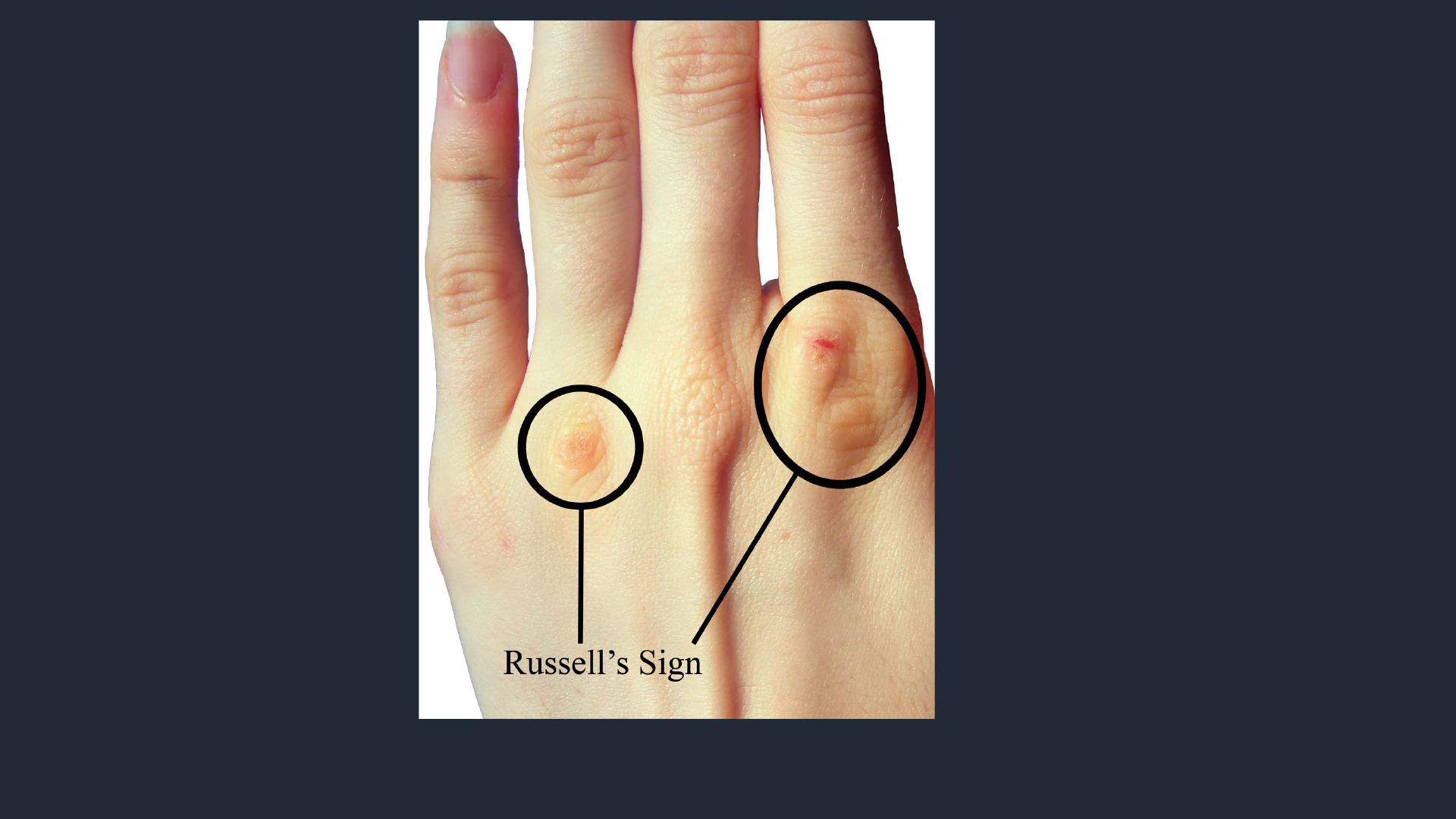
Source: https://commons.wikimedia.org/wiki/File:Russell%27s_Sign.png
Via Creative Commons. Author: “User:Kyukyusha”
Russell’s Sign

Source: https://commons.wikimedia.org/wiki/File:Sinus_Bradycardia.jpg
Via Creative Commons. Artist: Andrewmeyerson.
Sinus Bradycardia

Changes in
Expected
Weight
Trajectory

Impact of Weight Stigma
• Can increase the risk for all eating disorders and can
deter individuals from seeking treatment
• Be aware of the unintended consequences of our
conversations about weight
• Focus on health behaviors and well-being

How to Screen for
Eating Disorders

Ways to Screen for EDs in Primary Care
• Validated tools: SCOFF, ESP, EDY-Q (recommended
for ARFID)
• As part of other health screening: PHQ-9
• Single questions about dieting and/or weight or
shape concerns
(Morgan et al., 2000) (Pfizer, 1999) (Cotton et al., 2003)
(Hilbert et al., 2016)

Specific Screening Questions
• “Are you on a diet?”
• “Are you dieting?”
• “Do you have any concerns about your weight or
body shape?”
(Gooding et al., 2016)

Video Vignette #1
Bulimia nervosa presenting in a young adult using a
single question:
“Do you have any weight or shape concerns?”

SCOFF
S
Do you make yourself sick (vomit) because you feel uncomfortably full?
C
Do you worry you have lost control over how much you eat?
O
Have you recently lost more than one stone (6.35 kg or 14 lbs) in a
three-month period?
F
Do you believe yourself to be fat when others say you are too thin?
F
Would you say food dominates your life?
(Morgan et al., 2000)

SCOFF
Yes to 2+ questions → need for a more comprehensive
assessment
Additional questions with high sensitivity and specificity for
bulimia nervosa:
1. Are you satisfied with your eating patterns?
2. Do you ever eat in secret?
(Morgan et al., 2000)

Eating Disorders Screen for Primary care (ESP)
• Are you satisfied with your eating patterns?
• Do you ever eat in secret?
• Does your weight affect the way you feel about
yourself?
• Have any members of your family suffered with an
eating disorder?
• Do you currently suffer with or have you ever suffered in
the past with an eating disorder?
(Cotton et al., 2003)

PHQ-9
(Pfizer, 1999)

Video Vignette #2:
Possible binge eating disorder identified via response
to question 5 on the PHQ9. Clinician conducts further
screening using the SCOFF.

When Screening
Indicates Concern:
What Next?

• Further evaluation, including lab tests
• Conversations with parents or guardians
• Follow-up appointments
• Referral to treatment
(Academy for Eating Disorders, 2016)
Next Steps May Include:

• Patients may not acknowledge their illness
• Important to trust the concerns of parents or
guardians
• Emphasize that no one chose or caused the
eating disorder
reduce stigma and promote
acceptance of treatment
(Academy for Eating Disorders, 2016)
Key Factors to Keep in Mind:

The Basics of Treatment

Goals of Treatment
• Nutritional rehabilitation
• Weight restoration
• Medical stabilization
• Resumption of menses
• Cessation of disordered eating behaviors
(Academy for Eating Disorders, 2016)
• Restore regular meal patterns
• Manage co-morbid conditions
• Avoid potential complications

Outpatient Treatment:
Multidisciplinary Approach
• Medical Provider
Vital signs, weight checks,
and blood testing as
needed
• Psychopharmacologist
Medications
• School Nurse/Counselor
Can add extra support
• Nutritionist
Meal planning, caloric
requirements,
micronutrients
• Psychotherapist
Individual and Family
Based Treatment

Levels of Care
• Outpatient
• Intensive outpatient
• Partial hospitalization
• Residential
• Inpatient
• Telehealth = promising new option to
increase access to care

Indications for Immediate
Hospitalization
• Severe dehydration or malnutrition
• Electrolyte disturbance
• Vital sign abnormality
• Serious comorbid diagnoses
• Acute refusal of food
• Suicidality
Video vignette #3
Anorexia nervosa presenting as a
change in an adolescent’s growth chart.


OPENPediatrics.org Group Site
3
1
2
https://www.openpediatrics.org
Follow the steps to create a new account:

OPENPediatrics.org Group Site
3
4
5

• Eating disorders affect many people, including many
who do not fit common stereotypes
• Screening in primary care can help patients get into
appropriate treatment and increase chances of recovery
• There are accessible, free resources available to find
appropriate specialists for your patients
Summary

Webinar Creators
Katelyn Ferreira, MPH
Sara Forman, MD
Holly Gooding, MD, MSc
❖
Suman Ambwani, PhD
S. Bryn Austin, ScD
Erin Gibson, MPH
Megan Kipp, MEd
Jordan Levinson, BA

Webinar Vignette Actors
❖
Suman Ambwani, PhD
Courtney Brown, BA
Danielle Ferreira
Jessica Lin, MD
Cameron Nereim, MD
Frinny Polanco Walters, MD

U.S. Department of Health and Human Services Offices and Agencies:
• Office on Women’s Health
• Agency for Health Care Quality and Research
• Centers for Disease Control and Prevention
• Food and Drug Administration
• Health Resources and Services Administration
• Substance Abuse and Mental Health Services Administration
• National Institute of Mental Health
Federal Supporters

Community Partners

Funders
• Ellen Feldberg Gordon Challenge Fund for Eating
Disorders Prevention Research
• Jennifer Perini Fund for Eating Disorders Prevention
Research
• Office on Women’s Health
• MCHB/HRSA training grants T71-MC-00009, T76-MC-
00001

References
• Academy for Eating Disorders. (2016). Eating Disorders: A Guide to Medical Care (3rd Ed.).
Retrieved from Academy for Eating Disorders Website:
https://www.aedweb.org/learn/publications/medical-care-standards
• American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders
(5th ed.). Arlington, VA: American Psychiatric Publishing.
• Arcelus, J., Mitchell, A. J., Wales, J., & Nielsen, S. (2011). Mortality Rates in Patients With Anorexia
Nervosa and Other Eating Disorders. Archives of General Psychiatry, 68(7), 724-731.
• Cotton, M.-A., Ball, C., & Robinson, P. (2003). Four Simple Questions Can Help Screen for Eating
Disorders. Journal of General Internal Medicine, 18(1), 53–56.
• Gooding, H.C., Cheever, E., Forman, S.F., Hatoun, J., Jooma, F., Touloumtzis, C., & Vernacchio, L.
(2017). Implementation and Evaluation of Two Educational Strategies to Improve Screening for
Eating Disorders in Pediatric Primary Care. Journal of Adolescent Health, 60(5), 606-611.
• Hilbert, A., & van Dyck, Z. (2016). Eating Disorders in Youth-Questionnaire. English version.
University of Leipzig: http://nbn-resolving.de/urn:nbn:de:bsz:15-qucosa-197246.

References
• Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a Brief Depression
Severity Measure. Journal of General Internal Medicine, 16(9), 606–613.
• Merikangas, K.R., He, J., Burstein, M., Sendsen, J., Avenevoli, S., Case, B., Georgiades, K., et al.
(2011). Service Utilization for Lifetime Mental Disorders in U.S. Adolescents: Results of the
National Comorbidity Survey Adolescent Supplement (NCS-A). Journal of the American Academy
of Child & Adolescent Psychiatry, 50 (1), 32-45.
• Morgan, J.F., Reid, F., & Lacey, J.H. (1999). The SCOFF Questionnaire: A New Screening Tool for
Eating Disorders. The BMJ, 319, 1467-1468.
• Sonneville, K.R. & Lipson, S.K. (2018). Disparities in Eating Disorder Diagnosis and Treatment
According to Weight Status, Race/Ethnicity, Socioeconomic Background, and Sex among College
Students. International Journal of Eating Disorders, 51(6), 518-526.
• Swanson, S.A., Crow, S.J., Le Grange, D., Swendsen, J., & Merikangas, K.R. (2011). Prevalence and
Correlates of Eating Disorders in Adolescents: Results From the National Comorbidity Survey
Replication Adolescent Supplement. Archives of General Psychiatry, 68(7), 714-723.
• The Alliance for Eating Disorders Awareness. Treatment Center & Practitioner Directory. Retrieved
from https://www.findedhelp.com.

Thank you!

Questions?

Thank you!
Please email erin.gibson@childrens.harvard.edu with
any questions.
