
1
INVERKEITHING PRIMARY SCHOOL
Medication in School policy
In accordance with Fife Council Medication in Schools Policy
Updated October 2019

2
CONTENTS
1.0 Purpose
2.0 Scope
3.0 Responsibilities
4.0 Procedure
Appendix 1 NHS Fife: School Health Service
Appendix 2 Staff Instruction Record
Appendix 3 Education Health Care Plan and Summary
Appendix 3.1 Education Health Care Plan and Summary - Example
Appendix 3.1.1 Education Health Care Plan and Summary - Template
Appendix 3.2 Parental Request for Administration of Medication
Appendix 3.3 Parental Request for Self Administration of Medication
Appendix 3.4 Notice to parent/carer that supply of medication needs replacing
Appendix 4 Related Circulars and Documents
3
1.0 PURPOSE
To ensure a consistent approach to the administration of, and arrangements for,
medication across Inverkeithing Primary School in line with Fife policy.
2.0 SCOPE
This procedure relates to all staff willing to assist in supervising or gaining skills in
the administration of medication or clinical tests. It also relates to support staff
who have a responsibility for meeting the health care needs of pupils as part of
their contractual duties.
Some health care needs will include a requirement for mediation. Common
examples include allergy, diabetes, asthma and epilepsy.
Specific policy circulars apply to diabetes and nut allergies (see appendix 4).
This procedure is to be read in conjunction with The Administration of
Medicines in Schools (2001) published by the Scottish Government.
3.0 RESPONSIBILITIES
Responsibilities of heads of service, heads of establishments, staff, parents/ carers
and pupils are covered in The Administration of Medicines in Schools (2001).
The role of the NHS Fife School Health Service Appendix 1.
Additional, specific responsibilities are as follows:
3.1 The Headteacher responsible for the premises has the following
responsibilities:
a) To develop, implement and administer a school policy for meeting the
health care needs of pupils based on this procedure and The
Administration of Medicines in Schools (2001).
b) To ensure that an Education Health Care Plan and Summary (Appendix 3)
is pulled together for all pupils along with Health Care Plans from other
identified Specialist Services, for whom action is required in relation to a
health issue, including those who may require emergency medicines, in
accordance with chapter 3 of the above document. This plan should be
reviewed and updated regularly and at least on an annual basis, or when
medication is changed in consultation with the parents/carers of the pupil
and relevant medical staff. Where appropriate, the pupil should also have
an involvement in this planning review. Staff from the specialist clinics
should complete a Health Care Plan/Emergency Plan when a child is seen
at the clinic. A copy of this Plan should be given to the school i.e. Asthma,
Cystic Fibrosis, Pupils with Allergies and Epilepsy.
4
c) To ensure that all relevant staff who have volunteered or are required to
work to this procedure are aware of the procedures’ requirements, notified
of any specific responsibilities they have been appointed to, and work to it.
d) To ensure that all staff involved in the administration or supervision of
medication are given the opportunity to gain skills and routinely update
skills and knowledge on a two-yearly basis or more often if required.
e) To ensure that all staff, including supply teachers, visiting teachers and
support staff receives general awareness raising instruction / guidance in
common medical conditions and that they are made aware of trained staff
within the school to whom they can refer if a pupil requires medication.
They should also be made aware of emergency procedures noted on any
pupil’s Education Health Care Plan and Summary.
f) To ensure that there is sufficient staff instructed to provide care at all
times, ie school hours, extra-curricular activities, school trips.
g) To ensure that records are kept appropriately including class lists being
clearly marked to indicate pupils with any medical condition which might
require action to be taken to ensure a pupil’s well-being, eg allergy,
asthma, diabetes, epilepsy.
h) To liaise with the parents/carers/pupil and the local Health Authority to
ensure that the health care needs of the pupil are met as far as the
resources of the staff and establishment allow.
i) To ensure that agreement is reached with all parties involved before the
release of any information on a pupil’s health care needs.
j) To ensure pupil confidentiality is maintained as appropriate.
k) To ensure that accommodation is available which offers adequate privacy
where necessary.
l) To ensure that adequate facilities for instruction purposes are made
available.
m) To ensure that parents are requested to replace “out of date “ medication,
remove any medication from the school at the end of session and replace
medication at the beginning of the new session
5
3.2 Staff have the following responsibilities:
a) To comply with this procedure, The Administration of Medicines in Schools
(2001) and the establishment’s policy on the administration of medicines.
Under no circumstances may any staff member dispense medication
to pupils on their own initiative.
b) Where there is involvement in the administration or supervision of the
taking of medicine on the part of education staff, staff involved must have
attended appropriate awareness raising sessions.
c) Staff are not to administer medication until they have completed
appropriate awareness raising sessions. Involvement is voluntary for the
majority of staff, though some support staff have meeting the health care
needs of pupils as part of their contractual duties.
d) Schools should update their knowledge of all common medical conditions,
ie allergy, asthma, diabetes, epilepsy, regularly using national and local
resources. A list of staff who have received instruction should be
displayed clearly in the school office. (Appendix 2).
e) Fife Council will provide indemnity to the member of staff administering
emergency medicines against claims arising from, or out of negligence
providing the member of staff has:
Completed appropriate awareness raising instruction
Shown competency in awareness to the medical professional conducting
awareness raising instruction
Followed agreed procedures and protocols
f) All staff who have direct responsibility for a pupil should be made aware of
any school Education Health Care Plan and Summary (Appendix 3) for
managing the condition.
g) Consideration of a pupil’s medical condition should be made with regard to
physical activities s illustrated in (h) and (i) below.
h) Pupils with asthma should be allowed to take time to use inhalers if
necessary but should be encouraged to resume participation as soon as
they feel able. Exercise triggers for asthmatic attacks should be pre-
empted by encouraging the pupil to use their inhaler prior to activity or if
any wheezy episode occurs during exercise.
i) Pupils with diabetes should be allowed access to blood testing facilities as
well as food and drink before and during exercise.
3.3 Pupils, parents or carers should:
a) Provide the Headteacher with sufficient information about the pupil’s
health care needs and treatments. This could include some written record
of their medical condition from i.e. GP, Hospital or Specialist Nurse.
6
b) In collaboration with relevant health professionals and the head of
establishment, reach an understanding on the education establishment’s
role in supporting their child’s, or in the case of a pupil their own, health
needs.
c) Where there is a need for ongoing or emergency medication, it is essential
that the parents/carers, Headteacher, relevant health professionals, and
the pupil if appropriate, meet to discuss the pupil’s health care needs.
One of the purposes of this meeting would be to formulate an Education
Health Care Plan and Summary (Appendix 3) which both outlines the
nature of the health care need and gives a clear indication of how these
needs will be met. The community paediatrician should be contacted
before the meeting and asked to assist in providing background
information from medical records. Following the completion of the health
care plan a copy should be sent to the community paediatrician for
information.
d) It is the responsibility of the parents/carers to ensure that all medication is
“in date” and is replaced as necessary. It is also their responsibility to
remove medication from the school at the end of the school session and
replace it at the beginning of the new session
3.4 Specialist Asthma Nurse
For pupils who have been identified by a specialist as having severe asthma,
the specialist asthma nurse at the Victoria Hospital, Kirkcaldy, will complete
an Asthma Record Card. This will be discussed with the school who should
keep a copy of this in the pupil’s PPR. GP practices will be encouraged to
complete a plan.
4.0 PROCEDURE
a) Many pupils will at some time need to take medication in schools, nurseries
or other education establishments. For the majority this will be short term
eg finishing a short course of antibiotics. However, others, who may suffer
from conditions such as asthma or diabetes, may require some form of daily
treatment or monitoring of their condition. Some pupils may require
emergency treatment for severe allergic reaction (anaphylaxis) or epilepsy.
Pupils with all such conditions are regarded as having health care needs,
and with suitable support from the school or education establishment can
take part in most normal school activities. A positive response by the
establishment to a pupil’s health care needs will not only support the pupil’s
health, but will be seen as allowing the pupil to gain the full benefit of their
education experience.
Headteachers are to follow guidance given in The Administration of
Medicines in Schools (2001).
b) Class registers should be clearly marked to indicate pupils with medical
conditions which might require medication, eg asthma, so that any teacher
taking the class will be aware of the need to be observant and reactive.
7
4.1 Additional Guidance
a) Storage of medication/test material
In cases where medication or tests are administered by staff, these
medicines or test materials should be:
stored in a secure area which is easily accessible to designated staff
members during the school day.
This area should be locked/secured at the end of the school day.
All appropriate members of staff should be aware of where the keys for
this cabinet are held.
Schools should ensure that storage areas are kept below 25C
whenever possible.
In the event of medicines requiring to be kept under refrigeration,
storage is to be in a designated refrigerator authorised by the head of
establishment or in a locked and labelled container within a domestic
fridge.
Access to all medication must be controlled and refrigerators or
containers either secured firmly or be located in a room or area that can
be locked.
Particular care needs to be taken where an establishment stores controlled
drugs such as methylphenidate which is a class A drug. This may be more
easily recognised under the brand names Ritalin or Equasym. These
medicines should be kept in a locked cupboard allowing access only to
designed staff and being dispensed only by designated staff.
All medication, and in particular epi-pens, should be retained in the
original packaging.
Asthma inhalers should be readily accessible at all times. It is suggested
that –
In nursery classes/schools, Primary 1 to 3 and special schools inhalers
should be kept in a zipped “poly pocket” with the Emergency Care flow
diagram, in the pupil’s classroom
In Primary 4 to 7 and Secondary schools, inhalers will, in most cases,
be kept by the pupil in their bag or in the classroom with an additional
inhaler kept in a zipped “poly pocket”, with the Emergency Care flow
diagram, in a central, easily accessible place.
b) Recording
Establishments are to put in place a robust procedure for recording when
medicines are received, the expiry date and where appropriate, when
administered. The forms can be found in the Education Health Care Plan
and Summary (Appendix 3)
Schools should also ensure that parents are informed when medication
requires replacement.
8
Medication which is held within the school and is in date should be
collected by the parent/carer at the end of the term and returned to the
school on the first day of the next term.
c) Staff presence
While staff are acting with parental agreement and are in loco parentis, it
would be desirable for a second member of staff to be present during the
administration of medication both as a reassurance to staff and pupil. This
person will also be able to confirm that medication has been correctly
administered.
The need for privacy and reassurance should be kept in mind at all
times, particularly in the case of administration of rectal diazepam.
d) Disposal of medicines
Staff are not to dispose of medicines.
Parents/carers should be informed by the school that the
medication requires to be uplifted. This will be collected by the
parent/carer for disposal.
Parents/carers must provide replacement in-date medication to the
school if this is still required.
e) Collection and delivery of bins for disposal of needles
Sharp’s bins or clinical waste bins can be provided to schools on request
from the Estates Team. Arrangements will be made for delivery of bins
and frequency of uplift agreed dependent on requirements and agreed
protocols.
f) Hygiene/infection control
All staff should be familiar with normal precautions for avoiding infection
and must follow basic hygiene procedures. Where advice on infection
control is required, staff should request help from the NHS Board Infection
Control Nurse. Normal precautions include having access to protective
disposable gloves and taking care when dealing with spillage of blood or
other body fluids. Further guidance can be found in Appendix 5 and 5A to
Standard Circular No HSI 6 – First Aid.
g) Educational excursions and after school clubs
From time to time pupil(s) may take part in activities out with school.
These might include school trips, extra curricular activities, work
placements etc. Suitable arrangements for the administration of
medicines must be put in place to cover such activities so that designated
trained staff have access to necessary medication. Where an after school
activity takes place within the school premises a designated person should
have appropriate instruction and be given access to any medication stored
in the locked location within the school. Further guidance may be found in
Standard Circular No APG10 - Educational Excursions.
h) Refusal to take medicine
Where a pupil refuses to take medication or undergo a test, school staff
are not to put pressure on the pupil to take the medication or test and
9
should contact the parent/carer if the pupil is under 12 years of age or is
unable to advocate for him or her self. If parents/carers or emergency
contacts are unobtainable, the pupil’s GP should be contacted for advice.
In urgent cases the emergency services should be contacted.
i) Self management
It is good practice to allow pupils who can be trusted to manage their own
medication from a relatively early age and schools should encourage this.
If pupils can take their medication themselves, staff may only need to
supervise. An example would be inhalers for asthma. Some children with
diabetes may require to inject insulin during the school day. Appropriate
facilities should be provided to allow pupils to do this in private.
Where the parent/carer is satisfied that the child is accustomed to
independent self-administration of medication, the head of establishment
may agree to a written request from the parent/carer that the child be
permitted to use the medication as required without permission. A
suitable Self-Administration consent form is given as Appendix 3.3.
j) Children losing an inhaler
Where an inhaler has been mislaid or lost within the school the pupil (or
member of staff) should alert the designated member of staff who should
thereafter inform the parent of the need to replace this as soon as
possible. In addition every effort should be made by the school to recover
this.
k) Nut allergies
Specific guidance on actions to take in the case of a reaction to peanut or
other nut allergies is to be found in Standard Circular No APG 11 – Policy
on Health Promotion - The Management of Nut Allergies in Fife Schools
(2005).
l) Non-prescription medication
Pupils sometimes ask for painkillers (analgesics) at school such as
paracetamol. School staff are not to give non-prescribed medication to
children. In the event of a child presenting in pain, school will contact the
parent/carer immediately. Should the emergency contact not be available,
in urgent cases school will contact the emergency services.
m) Buccal Midazolam, Intranasal Midazolam and Rectal Paraldehyde.
The administration of these medicines requires a measured dose
individualised for each child. Staff must have attended awareness raising
instruction in relation to a particular pupil. In the event of non availability of
a suitably trained member of staff, alternative measures may involve:
1. A request to the paediatrician to consider alternative medication
2. Consideration of alternative accommodation (possible move to another
educational establishment)
3. Case consultation that may result in alternative emergency
procedures.
10
n) The use of oxygen therapy in schools raises particular issues. It is
important to enable a child to take part in education and to minimise the
disruption oxygen therapy can cause. The use of oxygen should be fully
covered by the health care plan.
Note: Care must be taken in the storage, handling and use of
oxygen, e.g. adequate ventilation in the room in which oxygen is
used is essential, as oxygen supports combustion, increasing the
speed at which things burn. It is supplied in highly pressurised
containers.
Appropriate instruction will be required for any member of staff taking
responsibility for oxygen therapy.
Local guidelines and an individual care plan along with full safety
information and instruction will be made available on request to Pharmacy
Services. NHS Fife, Pentland House, Lynebank Hospital, Halbeath Road,
Dunfermline KY11 4UW (Telephone 01383565341, Fax 01383 741395).
11
Appendix 1
NHS Fife: School Health Service
1.0 Information for schools
1.1 Every school and early years’ establishment in Fife has a named community
paediatrician and school nurse or health visitor. These practitioners work in
partnership to enable each school child to gain maximum benefit from education
by reducing the consequences of disability through the early recognition of
problems and appropriate intervention/referral or signposting.
2.0 School entry
2.1 When a child enters school or early years’ establishment, a questionnaire is sent to
the parents requesting information about the child’s medical history and any
concerns about the child’s health or development that the parents may have. In
the case of early years’ establishments, the enrolment form provides the
opportunity for this essential information to be shared.
2.2 All children are offered a review of growth by the school nurse service. Parents are
offered the opportunity to discuss any problems or anxieties with the named school
nurse.
2.3 A medical examination may be considered for selected children where problems,
or potential problems, which could interfere with the ability to benefit from
education, have been identified. Parents are invited to attend for the medical
examination.
Pupils may be selected for referral:
A health concern has been identified on the parental questionnaire.
Parents have requested a medical examination.
School staff have identified a health concern.
A health concern is identified by the school nurse during the health review.
The child’s immunisation record is checked and advice is given to parents when this
is found to be incomplete.
3.0 Pre-school or P1 entry
3.1 Vision screening tests of visual acuity is offered to all pre-school children prior to
enrolment in P1 by NHS.
3.2 Height and weight measurements are taken and recorded to assess the pupils
growth. Following assessment of findings the school nurse service will discuss
any issues identified and take necessary action.
3.3 Primary 1 dental check as part of national dental inspection programme. Parents
will also be encouraged and assisted where necessary to register with a local NHS
dentist.
12
Appendix 1
4.0 Primary 7
4.1 A questionnaire is sent to all parents requesting update information on their child’s
health prior to entry to secondary schools.
4.2 A review of growth is offered by the school nursing service and appropriate
intervention offered if required.
4.3 Dental checks may be carried out as part of national dental inspection programme.
5.0 Secondary S2
5.1 All girls in S2 will be offered the HPV (human Papilloma Virus) vaccine which gives
some protection against cervical cancer.
6.0 Secondary S3
6.1 Booster vaccination against Diphtheria, Tetanus and Polio will be offered in school
for those not routinely immunised by their family GP.
6.2 Dental checks may be carried out as part of national dental inspection programme.
7.0 At all ages
7.1 Any health needs identified will be managed by the relevant agency with onward
referral to appropriate specialist if indicated. In line with the principles of GIRFEC
senior school staff are notified when those problems are of educational
significance and likely to be other than of a temporary nature after discussion with
the pupil and parents/carers.
7.2 Referral to the Audiology Department is available at the request of pupils, parents
or teachers whenever there is doubt about a pupil’s hearing.
7.3 The community paediatrician and the school nurse are available at any time for
discussion with school staff where health concerns exist about pupils.
7.4 Advice is always available from the school nurse, when there is anxiety about
cases of infectious disease or parasitic infestation in a school, eg scabies, lice
7.5 Managing infectious diseases in schools document
8.0 Health promotion
8.1 Involvement of the school nurse service may include:
Supporting the head teacher to draw up the Education Health Care Plan and
Summary (Appendix 3)
Signposting/supporting classroom teachers to deliver aspects of curriculum for
excellence
Signposting/supporting staff to develop health initiatives identified by the
school, e.g. healthy lifestyle
13
Appendix 1
9.0 Raising awareness for administration of emergency medicines in school
9.1 Some pupils may have medication prescribed for use in an emergency situation
e.g. epileptic convulsion, acute allergic reaction (anaphylaxis).
9.2 Community paediatricians will be responsible for the Initial instruction to staff
members in the administration of these medicines. Updates are offered two yearly
across Fife. It is advised that schools be proactive in identifying a member of staff
to receive this instruction whether or not there are pupils who, at that time, require
medication.
14
Appendix 2
Instruction of staff on Medication in Schools
Pupils who may require emergency medication to be administered
A half day Initial instruction for the management of Allergy, Anaphylaxis and Epilepsy
is offered on a number of occasions throughout the school year. These sessions are
delivered by Community Paediatricians and can be booked through CPD online.
When instruction takes place a register of those present is kept and a copy sent to
the CPD office and Rothesay house. A signature of attendance by the attendee is
essential and this must be completed at the instruction session
Staff should update their knowledge at least every 2 years and Update sessions will
be offered locally by Community Health Practitioners (school nurses). These can also
be booked through CPD online. When instruction takes place a register of those
present is kept and a copy sent to the CPD office. A signature of attendance by the
attendee is essential and this must be completed at the instruction session
Where specific instruction is required for procedures other than those offered on the
centrally held courses, this will be carried out on an individual basis with staff and the
community paediatrician or specialist nurse. Such sessions should be noted by staff
on their individual CPD record and a note of the specific instruction with the trainer’s
name, sent to Rothesay House for noting in central records.
Sessions in Special Schools are often organised for whole departments and it is
essential that this information is included in CPD records. This can be done by
ensuring that when instruction takes place a register of those present is kept and a
copy sent to the CPD office. A member of that team will then enter the information in
the records of the people named on the register.
Pupils with severe asthma
Specific instruction will be offered by the Asthma Specialist Nurses for school staff
who work with pupils
Pupils with mild asthma
General awareness raising instruction for all staff may be requested from the Asthma
Specialist Nurses
Pupils with diabetes
Specific instruction will be offered by the Diabetes Specialist Nurses for school staff
who work with pupils and more general instruction for all staff may also be possible.
Pupils with epilepsy
General awareness raising sessions for all staff and pupil specific instruction may be
requested from the Epilepsy Specialist Nurse.
Pupils with allergies
General advice for all staff may be requested from the Specialist Allergy Nurse.

15
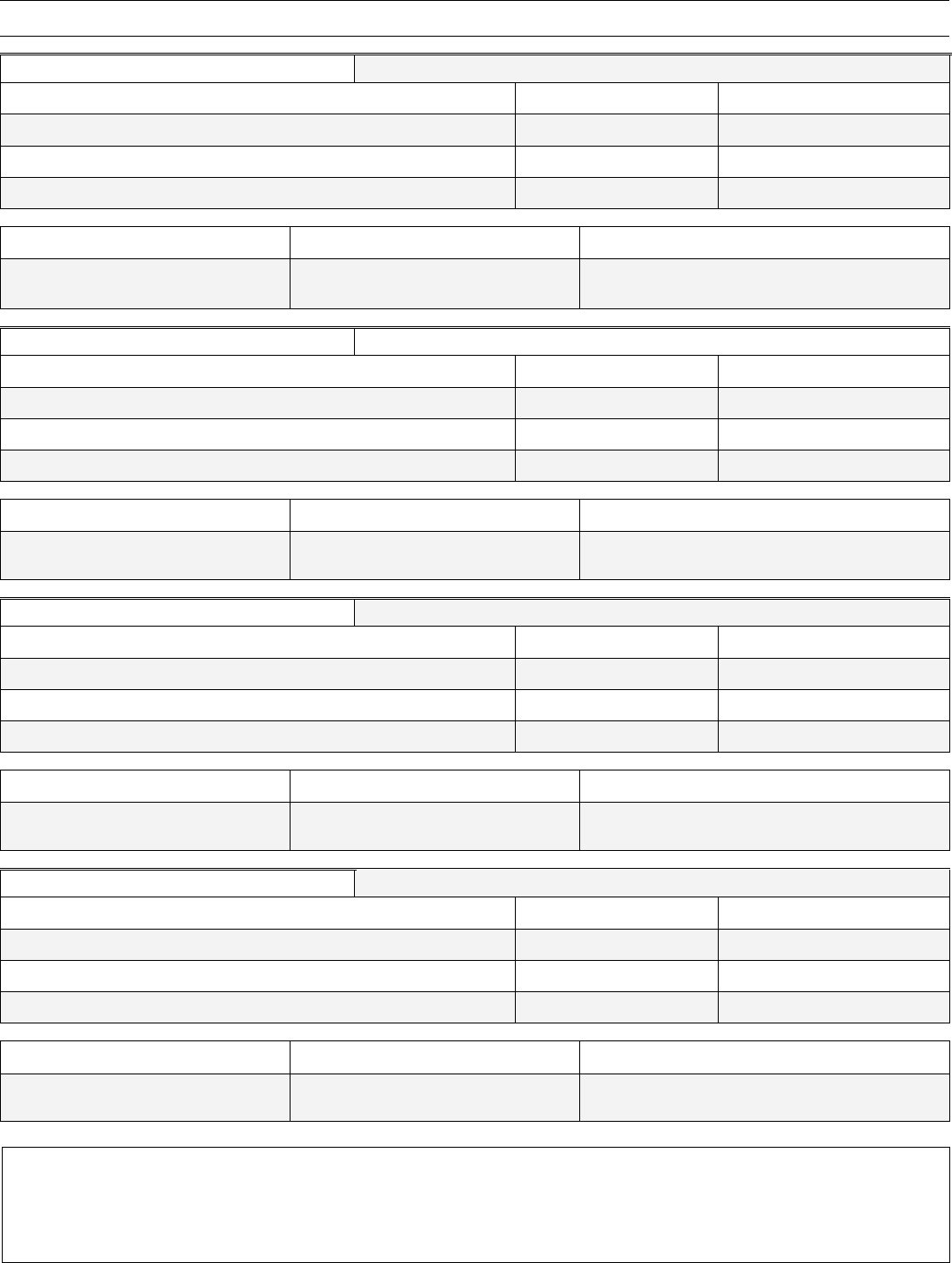
Staff Instruction Record Appendix 2
Record of staff who have volunteered to administer emergency medication as and when
required and who have attended instruction on the management of SEVERE ALLERGIES,
ASTHMA AND EPILEPSY
(N.B. Staff should attend an update at least every 2 years)
NAME
Initial
Attendance
Update
Update
Update
Update

16
Education Health Care
Plan and Summary
HSI2 – Appendix 3
Please enter name and date of birth of pupil here
Please enter
photograph of pupil here
Please enter name of school here
17

18
Emergency Medication in Schools for Pupils
Education Health Care Plan for a Pupil with Medical Needs
(Please enter details requested in shaded boxes)
HSI 2
Appendix 3
Pupil’s details (Enter all the requested information below)
Name of Pupil:
Date of Birth:
Year Group
Class
Medical Information (Enter name of medical condition(s))
Family Contact Information (Please enter all requested details as fully as possible)
Name of family member
Relationship to pupil
Contact telephone no.
Home:
Work:
Mobile:
Name of family member
Relationship to pupil
Contact telephone no.
Home:
Work:
Mobile:
NHS contact details
Name of GP
Telephone no.
Surgery Name
Name of Consultant/Specialist
Name of hospital/clinic
Telephone no.
This plan was prepared by (please add name and designation of everyone involved in preparing this plan)
Copies of this plan have been given to (please add name and designation of everyone who received a copy of this plan)

19
Medication in Schools for Pupils – contd.
Name of Pupil
Page 2 of Appendix 3
Name of pupil’s medical condition(s) and details of pupil’s individual symptoms
1. Name of medical condition
Give brief descriptions of symptoms associated with this medical condition
Name of medication taken for this medical condition
2. Name of medical condition
Give brief descriptions of symptoms associated with this medical condition
Name of medication taken for this medical condition:
Daily care requirements (e.g. before sport, dietary needs, therapy input, nursing needs)
Action to be taken in an emergency (this will be the agreed procedures shown in The Summary Form)
Follow up care (add details of any after care required for this pupil)
Members of staff in school trained to administer medication for this pupil
(add name and designation of staff member – also state if different staff are trained for off-site activities)
Signature of Parent or Guardian
School representative’s signature
Sign above and print name below
Sign above and print name below
Relationship to pupil
Designation
Education Health Care Summary Prepared
Yes
No
Date

20
FIFE COUNCIL
EDUCATION HEALTH CARE PLAN SUMMARY – EXAMPLE ONLY
Name of Pupil:
JOHN SMITH
Date of Birth:
01/08/99
Address:
77 Anywhere Street, Kirkcaldy KY2 6SS
In the event of
an emergency
phone:
Mum on 01592 555555
DIABETES MELLITIS
Hypoglycaemia is a complication of diabetes where the blood glucose levels fall too low – BELOW 4.
Each child has their own signs and symptoms of Hypo.
Hypogel Insulin Lucozade
All kept in box in cupboard in classroom
Symptom 1
Feeling lethargic, generally unwell
Treatment/Procedure
Test blood
If reading is below 4 treatment is required
Symptom 2
Treatment/Procedure
Symptom 3
Treatment/Procedure
Symptom 4
Treatment/Procedure
Nominated people within
school:
Signatures of agreeing parties:
Parental contact details:
GP details:
Health
Professional
Nurse Jones
Name
Deborah Smith
Name:
Dr Drake
Parent/Carer
Deborah Smith
Tel:
01592 555555
Tel:
01592 222222
Headteacher
Mrs Trunchbull
Mobile:
n/a
Address:
Health Centre
Anywhere
Date Completed
Appendix 3.1 - Example

21
FIFE COUNCIL
EDUCATION HEALTH CARE PLAN SUMMARY
Name of Pupil:
Date of Birth:
Address:
In the event of
an emergency
phone:
.
Symptom 1
Treatment/Procedure
Symptom 2
Treatment/Procedure
Symptom 3
Treatment/Procedure
Symptom 4
Treatment/Procedure
Nominated people within
school:
Signatures of agreeing parties:
Parental contact details:
GP details:
Health
Professional
Name
Name:
Parent/Carer
Tel:
Tel:
Headteacher
Mobile:
Address:
Date Completed
Appendix 3.1.1 - Template

22
Parental Request for Administration of Medication
(Please enter information into the shaded areas)
HSI 2
Appendix 3.2
To:
The Head teacher
School:
I request that my son/daughter is given the following medication or clinical test by school staff as indicated below:
Name of pupil
Date of Birth
Class/Teacher
Date request made
Name of medical condition
(a) Details of medicine(s) and/or test(s)
Name of medicine(s) or test(s)
Dosage
Time to be administered (am/pm)
Only as required (tick)
(b) Please indicate the circumstances in which the medicine(s) or test(s) should be administered
(c) Dose of medicine(s) to be given and means of administration and/or technique for undertaking the test
(d) Length of time current supply of medicine(s) will cover
Monday
Tuesday
Wednesday
Thursday
Friday
Ongoing
Medication and/or test kit to be replenished/updated regularly
Name address and telephone number of GP or Paediatric Consultant
Name address and telephone number of parent/carer
I undertake to deliver the medicine(s) and/or test materials personally to school, and to replace them whenever
necessary. I also undertake to advise you immediately of any changes in treatment prescribed by doctor or hospital.
Signed by:
Relationship to child:
Date:
23
Appendix 3.2 – page 2
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff member
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff member
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff member
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff member
Please note that medication stored in schools will not be available outwith normal school hours.
Parents and carers must contact their GPs within normal hours for the replacement
of medication outwith normal school hours and terms

24
Parental Request for Self-Administration of Medication
HSI 2
Appendix 3.3
To:
The Head teacher
School:
I wish my son/daughter, when necessary, to be permitted to take the following
medicine(s) and/or perform the following clinical test(s)
Name of pupil
Date of Birth
Class/Teacher
Date request made
Name of medical condition
(a) Details of medicine(s) and/or test(s)
Name of medicine(s) or test(s)
Dosage
Time to be administered (am/pm)
Only as required (tick)
(b) Please indicate the circumstances in which the medicine(s) or test(s) should be administered
(c) Dose of medicine(s) to be given and means of administration and/or other details of test
(d) Length of time current supply of medicine(s) will cover
Monday
Tuesday
Wednesday
Thursday
Friday
Ongoing
Medication and/or test kit to be replenished/updated regularly
(e) It is/It is not necessary for a member of staff to record each dose of medicine and/or each test performed
My son/daughter will carry the above medicine(s) at all times, for taking as required. I undertake to advise you
immediately of any change of treatment prescribed by my doctor or hospital.
Name address and telephone number of GP or Paediatric Consultant
Name address and telephone number of parent/carer
I undertake to deliver the medicine(s) and/or test materials personally to school, and to replace them whenever
necessary. I also undertake to advise you immediately of any changes in treatment prescribed by doctor or hospital.
Signed by:
Relationship to child:
Date:

25
Appendix 3.3 – page 2
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff
member
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff
member
RECEIPT OF MEDICATION FOR PUPIL
Name of medicine
Date received in school
Expiry Date
Total amount of drug received (in mls, no. of tablets or units)
Name of school:
Signature of staff member
Countersignature of 2
nd
staff
member
Please note that medication stored in schools will not be available outwith normal school hours.
Parents and carers must contact their GPs within normal hours for the replacement
of medication outwith normal school hours and terms

26
Notice to parent/carer that supply of medication needs replacing
HSI 2
Appendix 3.4
To the parent/carer of:
Enter name of pupil and date of birth in row below
Supply of medication – replacement
The emergency medication held in school for your daughter/son requires to be replaced because
it is out of date/has been used.
Name of medication
Dose prescribed
Time(s) to be given
If your son/daughter still requires this medication please ensure you send a further supply into school as soon as
possible.
Please make sure that this medication is given to the school in the container in which it was dispensed, clearly labeled
and indicating contents, dosage and child’s name in full.
Please return this form with the medication
I request that the medication stated above continue to be administered to:
(Enter name and date of birth of pupil)
I accept full responsibility for informing the school if my child has been given a dose of this medication before coming to
school.
I accept responsibility for ensuring that the medicine has not expired and that there will be enough medicine supplied to
the school for my child’s needs. I will collect all unused medicine from the school when informed it needs uplifted.
Parent’s Name and address: (enter below)
Contact details:
Home
Work
Mobile
E-mail
Signature of parent/guardian
Date
Note: The school will not accept medication unless this form is completed and
signed by the parent or legal carer of the child and the headteacher agrees to the
administration of the medication.
27
RELATED CIRCULARS AND DOCUMENTS APPENDIX 4
1. The Administration of Medicines in Schools 2001 (Scottish Executive)
2. Standard Circular No APG 10 – Educational Excursions
3. Standard Circular No HSI 6 – First Aid (Appendices 5 & 5A)
4. Standard Circular No APG 11 – Policy on Health Promotion (Appendix 8: The
Management of Nut Allergies in Fife Schools)
5. Standard Circular HSI 9 – Policy for the Management of Diabetes in Schools
