
Infection Control
Manual
Revised: March 2023
Yale University
Table of Contents
Foreward .....................................................................................................................................iii
SECTION 1: Staff Orientation and Education Information ....................................................... 1
1.1
INTRODUCTION ................................................................................................................................................................................ 1
1.2
ROUTES OF TRANSMISSIONS ........................................................................................................................................................ 2
1.2.1
Contact Transmission ................................................................................................................... 2
1.2.2
Vehicle Route ............................................................................................................................... 2
1.2.3
Airborne Transmission .................................................................................................................. 2
1.2.4
Vector-Borne Transmission .......................................................................................................... 2
1.3
STANDARD PRECAUTIONS ............................................................................................................................................................ 2
1.4
TRANSMISSION-BASED PRECAUTIONS ...................................................................................................................................... 3
1.4.1
Airborne Precautions .................................................................................................................... 3
1.4.2
Droplet Precautions ...................................................................................................................... 3
1.4.3
Contact Precautions ...................................................................................................................... 3
1.4.4
Synopsis of Types of Precautions and Patients Requiring the Precautions* ..................................... 4
1.5
EMPIRIC USE OF TRANSMISSION-BASED PRECAUTIONS - PENDING CONFIRMATION OF DIAGNOSIS.......................... 5
1.6
TB EXPOSURE CONTROL PLAN ................................................................................................................................................ 22
Risk Assessment ................................................................................................................................. 22
Transmission and Pathogenesis ............................................................................................................ 22
Guidelines for TB Control ................................................................................................................... 23
TB Exposure Control Procedures for Suspected or Known Active TB Cases ......................................... 24
Evaluation of Health Care Workers Post Exposure to Active TB Cases ................................................. 24
Continuing Risk Assessment at Yale University ................................................................................... 25
1.7
GUIDELINES FOR VANCOMYCIN RESISTANT ENTEROCOCCUS (VRE) ..................................................... 25
1.8
MRSA INFECTION CONTROL GUIDELINES ........................................................................................................................... 26
SECTION 2: Medical Surveillance ............................................................................................ 29
2.1
RECOMMENDED IMMUNIZATIONS FOR HEALTH CARE WORKERS ............................................................................................29
2.2
TUBERCULOSIS TESTING............................................................................................................................................................. 34
2.3
COMMUNICABLE DISEASE WORK RESTRICTIONS FOR HEALTH CARE WORKERS ......................................................................34
2.4
GUIDELINES FOR PREGNANT HEALTH CARE PERSONNEL ............................................................................................... 39
2.5
EMERGENCY PROCEDURES FOR EXPOSURE TO BLOOD AND BODY FLUIDS ............................................................. 40
2.5.1
Needlestick Procedures ............................................................................................................... 41
2.6
POST EXPOSURE PROPHYLAXSIS GUIDELINES FOR EXPOSURE TO OTHER INFECTIOUS AGENTS .................................. 42
SECTION 3: Handling Waste ............................................................................................................. 45
3.1
MEDICAL WASTE MANAGEMENT ............................................................................................................................................. 45
3.2
GUIDELINES ON THE MANAGEMENT OF INFECTIOUS WASTE ........................................................................................ 46
3.3
TRASH HANDLING .......................................................................................................................................................................... 46
3.4
PROCEDURE FOR TRASH DISPOSAL ........................................................................................................................................ 46
3.5
DISPOSAL OF CHEMOTHERAPY WASTE ................................................................................................................................... 47
3.6
NEEDLES AND SYRINGES AND OTHER SHARP ITEM ............................................................................................................ 47
3.7
DRESSINGS AND TISSUES ...................................................................................................................................................................................48
3.8
AUTOCLAVES .................................................................................................................................................................................. 49
SECTION 4: Good Work Practices............................................................................................ 50
4.1
HAND WASHING ............................................................................................................................................................................. 50
4.2
GENERAL .......................................................................................................................................................................................... 50
4.3
EYEWASH STATION AND SPILL CLEAN-UP SUPPLIES ........................................................................................................ 51
4.4
REFRIGERATORS ............................................................................................................................................................................ 51
4.5
STORAGE OF STERILE SOLUTIONS ........................................................................................................................................... 51
4.6
STORAGE OF DISPOSABLE SUPPLIES ...................................................................................................................................... 52
4.7
PERISHABLE FOOD AND JUICES ............................................................................................................................................... 52
4.8
DIETARY ........................................................................................................................................................................................... 52
4.9
PRIVATE ROOMS ............................................................................................................................................................................ 52
4.10
ROOMMATES FOR PATIENTS ON TRANSMISSION BASED PRECAUTIONS .................................................................... 53
4.11
AIRBORNE PRECAUTION ROOMS ........................................................................................................................................... 53
General Considerations .............................................................................................................. 53
4.12
CLEANING PATIENT ROOMS .................................................................................................................................................... 53
SECTION 5: Personal Protective Equipment....................................................................................... 55
5.1
GLOVES ............................................................................................................................................................................................ 55
Policy and procedure for wearing gloves .............................................................................................. 55
Clean technique................................................................................................................................... 56
Sterile technique ................................................................................................................................. 56
5.2
GOWNS.............................................................................................................................................................................................. 57
Procedure for putting on a gown .......................................................................................................... 57
Procedure for removing a contaminated gown .............................................................................................. 58
5.3
FACE AND EYE PROTECTION ..................................................................................................................................................... 59
5.4
SURGICAL MASKS .......................................................................................................................................................................... 60
Procedure for Putting on a Mask .......................................................................................................... 60
5.5
NIOSH APPROVED PARTICULATE MASKS AND RESPIRATORS........................................................................................ 61
SECTION 6: Decontamination, Spill Response and Housekeeping .................................................... 62
6.1
STERILIZATION OR DISINFECTION OF REUSABLE MEDICAL INSTRUMENTS/DEVICES ...................................................... 62
Critical Items ...................................................................................................................................... 62
Semi-Critical Items ............................................................................................................................. 62
Non-Critical Items............................................................................................................................... 62
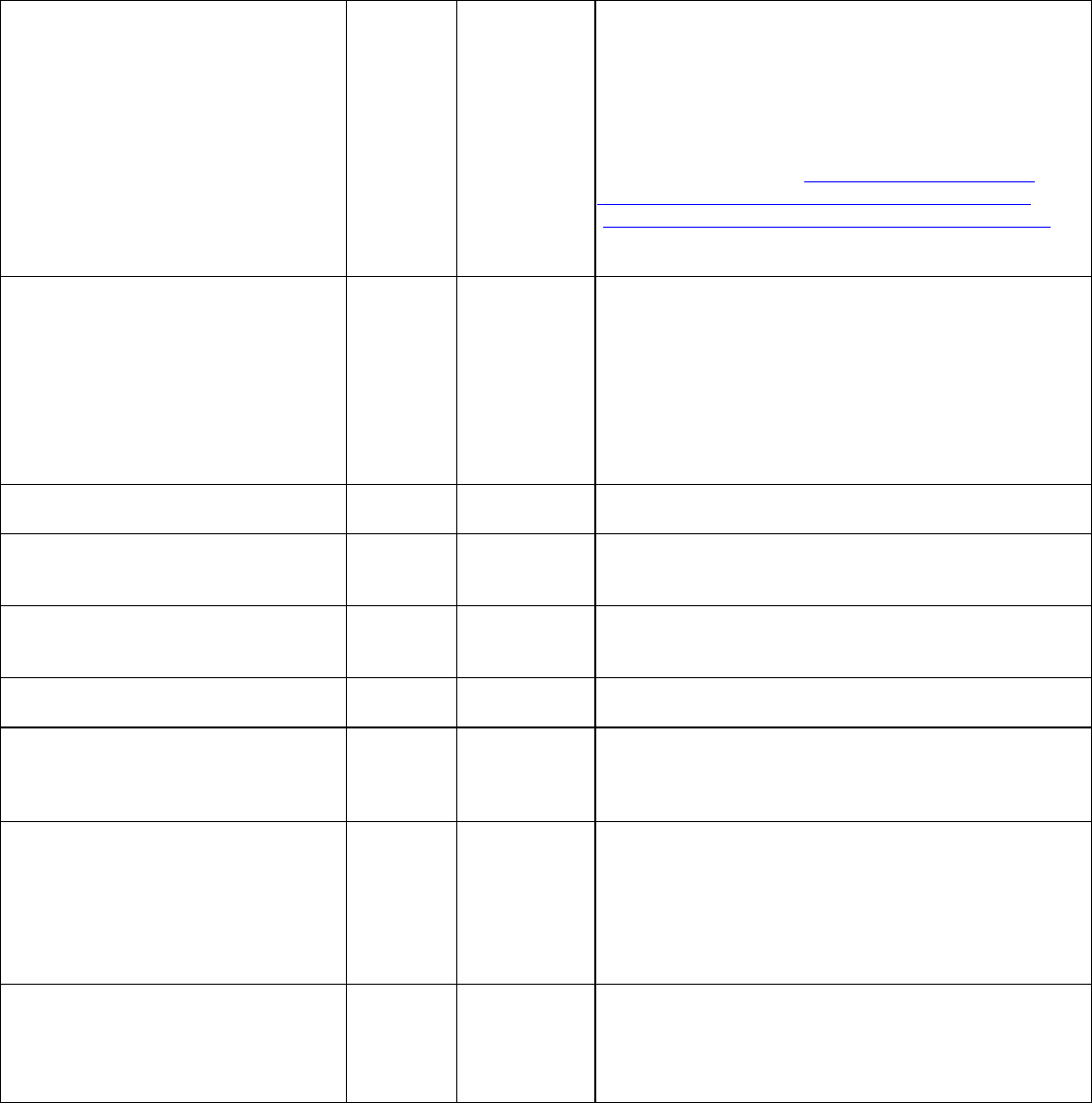
Table 1. Levels of Disinfection According to Types of Microorganism ................................................. 63
6.2
REUSABLE PATIENT-CARE EQUIPMENT ................................................................................................................................. 64
6.3
SPHYGMOMANOMETER AND STETHOSCOPE ......................................................................................................................... 64
6.4
SOILED LINEN & LAUNDRY ........................................................................................................................................................ 65
6.5
H
OUSEKEEPING........................................................................................................................................................................................................
65
6.6
CLEANING SPILLS OF BLOOD AND BODY FLUIDS ON ENVIRONMENTAL SURFACES ......................................................... 65
Prepare and maintain a spill response kit. ............................................................................................. 66
SECTION 7: Medications and Safety Injection Practices .................................................................. 67
7.1 Storage of Medications-Multi-Dose Vials/Single-Dose Vials………………………………………….…67
7.2 Fingerstick Devices………………………………………………………………………………………….…68
7.3 Blood Glucose Meter………………………………………………………………………………………..…68
SECTION 8: Storage and Transporting of Specimens ......................................................................... 69
8.1
HANDLING OF CLINICAL SPECIMENS ...................................................................................................................................... 69
8.2
PROTOCOL ON MANAGEMENT OF SPECIMENS ..................................................................................................................... 69
SECTION 9: Transportation of Patient ................................................................................................. 70
9.1
TRANSPORTATION PROCESS ....................................................................................................................................................... 70
9.2
GENERAL CONSIDERATIONS AND RESPONSIBILITIES ......................................................................................................... 70
Unit Receptionist ................................................................................................................................ 70
Nurse .................................................................................................................................................. 70
Transport Personnel: ........................................................................................................................... 70
9.3
INFECTION CONTROL CONSIDERATIONS FOR PERSONNEL TRANSPORTING PATIENT ...................................................... 70
9.4
GENERAL CONSIDERATIONS FOR PATIENTS .......................................................................................................................... 71
SECTION 10: Reporting Communicable Diseases to the State of Connecticut ................................. 72
SECTION 11: Serve and Assistance Animals… .................................................................................. 74
11.1
Guidelines for Service Animals Visiting Health Care Facilities ....................................... 74
11.2
Staff Responsibilities ...................................................................................................... 74
11.3
Permitted and Restricted Areas for Service Animals and Additional Info for Staff ........... 75
APPENDIX A: Needle Stick Procedure ................................................................................................................. 75
APPENDIX B: HIV Counseling Guidelines ........................................................................................................... 85
APPENDIX Yale Health 1: Quality Control of Multidose Vials/Sterile Solutions ................................................ 86
APPENDIX Yale Health 2: Laundry ...................................................................................................................... 88
APPENDIX Yale Health 3: Clean Up Spills ........................................................................................................... 89
APPENDIX Yale Health 4: Infection Control Protocol ......................................................................................... 91
APPENDIX Yale Health 5: TB Exposures at Yale Health ..................................................................................... 92
APPENDIX Yale Health 6: Universal Respiratory Etiquette ................................................................................ 94
APPENDIX Yale Health 7: Clinical Guidelines for SARS CoV Infection ........................................................... 95
APPENDIX Yale Health 8: VaricellaExposureatYale Health .................................................................................... 104
APPENDIX Yale Health 9: PnP for Visitors to ICF ............................................................................................. 106
APPENDIX Yale Health 10: PnP for Negative Pressure Rooms Inpatient Care and Use.................................. 107
APPENDIX Yale Health 11: Guidelines for the Infection Control Management & Prevention of
Norovirus Outbreaks… ...................................................................................................................................................... ….
109
iii
Foreword
In the mid 1990’s, concerns over the lack of uniformity of infection control practices across Yale
University’s clinical areas not monitored by the Yale-New Haven Hospital, prompted the Deputy
Provost to request the establishment of an Infection Control Work Group. Infection control
coordinators, nurses and doctors from various clinical locations as well as representatives from
Yale Environmental Health and Safety were selected to participate in the work group.
The group conducted an initial assessment of infection control programs in each University
clinical area. The Yale University Infection Control Work Group has prepared this manual to
inform the Yale clinical community of standard infection control issues and practices. This
manual will not replace established policy and procedure manuals that are in place at clinical
areas. However, this manual was established with the intent to provide consistent infection
control policies and programs that meet or exceed minimal acceptable standards, across Yale’s
clinical areas and satellite facilities. Areas lacking an established infection control manual can
use the manual as a framework and amend it with site specific information as required.
As this is a document in progress, all are encouraged to review this manual and contact Yale
Environmental Health and Safety concerning any infection control or safety issues.
In addition to preparing this manual, the Yale Infection Control Work Group is available to assist
your site with the following:
▪
help establish an infection control committee for your site;
▪
work with you to identify an on-site infection control coordinator;
▪
assist with the evaluation of new engineering controls designed to minimize occupational
exposures, such as sharps safety devices
Special thanks to those individuals who took time to review this manual and contributed
information and suggestions to improve the presentation. Every two years or as needed, this
manual will be reviewed and updated. The work group will continue to serve as a resource for
infection control, and will periodically monitor locations to ensure that the appropriate practices
are upheld.
1
SECTION 1: Staff Orientation and Education Information
1.1
Introduction
This manual has been prepared to provide current guidelines for the prevention and control of
infections among patients, employees and visitors. These guidelines provide a rational approach to
isolation and other infection control practices, balancing the theoretical with what is practical and
cost-effective.
All personnel (physicians, nurses, technicians, support staff and others) are responsible for
complying with isolation precautions and other infection control procedures, and for tactfully
calling observed infractions to the attention of offenders. Compliance with infection control
procedures cannot be effectively dictated and enforced by a committee or administration, but must
arise from a personal sense of responsibility to the patient and others in the health-care environment.
Unfortunately, infractions by some are sufficient to negate the conscientious efforts of others, so
constant vigilance is important.
Thus, professional responsibility is the key to detecting and correcting breaches in aseptic
techniques as well as setting an example of a philosophy of total patient care. Physicians, nurses
and others in leadership positions have an excellent opportunity to teach by example. Acting as role
models, they influence the practice of others a great deal.
Patients, as well as their visitors, also have a responsibility for complying with infection control
procedures. Physicians and nurses responsible for their care should inform them of appropriate
infection control procedures. Everyone in contact with patients must practice hand washing, the
single most effective procedure in preventing cross-infection. Even routine activities, such as
examining a patient or taking a blood pressure reading, can transfer organisms to the hands of the
health-care personnel. Hence, it is essential that hands be washed before touching a patient, during
patient care when going from one body site to another, after contact with infective material such as
blood, secretions and excretions, after handling articles and equipment contaminated with body
fluids, and before touching another patient. Patients must also be encouraged to wash their hands
at regular intervals.
Spread of infection requires three elements: a source of infecting organism, a susceptible host and
a means of transmission for the organism. The source of the infecting agent may be patients,
personnel, or, on occasion, visitors, and may include persons with acute diseases, persons in the
incubation period of a disease, or persons who are colonized by the infectious agent, but have no
apparent disease. Another source of infection can be the person’s own endogenous flora
(autogenous infection). Other potential sources are inanimate objects in the environment that have
become contaminated, including equipment and medications.
Patient’s resistance to pathogenic microorganisms varies greatly. Some patients may be immune
to, or able to resist colonization by an infectious agent; others exposed to the same agent may
establish a commensal relationship with the infecting organism and become asymptomatic carriers;
still others may develop clinical disease. Host resistance may be compromised by illness, as in
patients with diabetes mellitus, neoplasia, HIV-infection, leukemia and lymphoma, uremia,
traumatic injury or burns. Alternatively, resistance may be decreased by iatrogenic physical
intervention, most commonly urethral and intravenous catheters, respiratory tract manipulation and
surgical procedures, or medical measures, especially steroids and other immunosuppressive
medication.
Microorganisms are transmitted by various routes, and the same microorganism may be transmitted
by more than one route. For example, varicella-zoster virus (chicken pox) can be spread either by
the airborne route (droplet nuclei) or by direct contact. The differences in
2
infectivity and in the mode of transmission of the various agents form the basis for the differences
in isolation precautions recommended in this guideline.
1.2
Routes of Transmissions
There are four main routes of transmission — contact, vehicle, airborne, and vector-borne.
1.2.1
Contact Transmission
The most important and frequent means of transmission of nosocomial (hospital acquired)
infections can be divided into three subgroups: direct, indirect and droplet contact.
Direct contact: Direct physical transfer between a susceptible host and an infected or a
colonized person, as occurs when personnel turn patients, give baths, change dressings or
perform other procedures involving direct personal contact.
Indirect contact: This involves personal contact of the susceptible host with a contaminated
intermediate object, usually inanimate, such as bed linens, clothing, instruments and dressings.
Droplet contact: Infectious agents may come in contact with the conjunctiva, nose, or mouth of
a susceptible person as a result of coughing, sneezing or talking by an infected person who has
clinical disease or is a carrier of the organism. This is considered “contact” transmission rather
than airborne since droplets usually travel no more than about three feet.
1.2.2
Vehicle Route
The vehicle route applies in diseases transmitted through such contaminated items as:
Food (e.g., salmonellosis)
Water (e.g., giardiasis)
Drugs (e.g., bacteremia from an infusion of contaminated product)
Blood (e.g., Hepatitis B, Hepatitis C, HIV).
1.2.3
Airborne Transmission
Airborne transmission occurs by the inhalation of aerosols containing an infectious agent.
Organisms carried in this manner can be widely dispersed by air currents before being inhaled by
or deposited on a susceptible host. Tuberculosis is spread via airborne transmission.
1.2.4
Vector-Borne Transmission
Vector-borne transmission occurs when an infected vector bites a susceptible host, most commonly
arthropods (e.g., ticks, mosquitoes). World wide it is of special concern in tropical countries where
mosquito-transmitted malaria is endemic. In the United States, Lyme Disease and Rocky Mountain
Spotted Fever are examples of diseases transmitted by tick vectors, and Eastern Equine Encephalitis
(EEE) and West Nile Virus by mosquitoes.
1.3
Standard Precautions
Standard Precautions are a philosophy for providing medical care that assumes patients may be
infectious. It must be applied to all patients receiving care in University facilities regardless of
diagnostic or infection status. Standard Precautions apply to blood; all body fluids; secretions and
excretions (except sweat), regardless of whether or not they contain visible blood; non-intact skin;
and mucous membranes.
3
Standard Precautions state that gloves must be used whenever contact is anticipated, changed
between patients, and hands washed after gloves are removed. In addition, gowns (impermeable to
liquids) and shoe covers must be worn when splashes of body fluids or blood are anticipated in
order to reduce the risk of exposure to blood borne pathogens. Masks, face shields, or goggles must
also be worn during procedures that are likely to generate splashes or sprays of blood, body fluids,
or secretions.
1.4
Transmission-Based Precautions
These precautions are designed for patients who are documented or suspected to be infected with
highly transmissible or epidemiologically - important pathogens. These precautions are designed
to be implemented in addition to Standard Precautions:
1.4.1
Airborne Precautions
These precautions are designed for infections that are transmitted by airborne droplet nuclei (<5
microns in diameter) that can remain suspended in the air. Examples of infectious agents that fall
into this category include tuberculosis, Rubeola (measles), and Varicella (chickenpox).
In addition to Standard Precautions:
Patients should be placed in a private room with monitored negative air pressure in relation to
surrounding areas.
The room should have 6-12 air changes per hour with appropriate discharge of air outdoors or
through a high efficiency filtration system before the air is recirculated to other areas of the
building. The door must be kept closed with the patient kept in the room. If a private room is
not available, another patient with the same active infection may be placed in the room
(cohorting).
Personnel who enter the isolation room should be immune to the infection. Non-immune
personnel must wear a respirator (N-95 or better) before entering the room.
Patient transport should be limited to that which is absolutely necessary. Patients should wear
surgical masks if transported outside of the room.
Refer to TB Control Plan for additional information on this agent (see page 17).
1.4.2
Droplet Precautions
Droplet precautions are designed to prevent the transmission of organisms that are transmitted by
large droplet contact with conjunctiva or mucous membranes of the nose or mouth. Droplets greater
than 5 microns in diameter are usually generated with coughing, sneezing, talking, as well as during
procedures such as bronchoscopy or suctioning. These larger droplets generally travel only short
distances (3 feet or less). Examples of organisms in this category include influenza, mycoplasma,
strep pneumonia, mumps, and whooping cough.
Patients should be placed in a private room or, if not available, they may be placed in a room
with a patient who has an active infection with the same organism.
A surgical (or better) mask must be worn when working within 3 feet of the patient.
Patient transport should be limited to that which is absolutely necessary. A surgical mask
should be placed on the patient during transport.
1.4.3
Contact Precautions
These should be used for patients who are infected with organisms that are transmitted by direct
skin to skin contact or by indirect contact with environmental surfaces or patient care items.
4
These precautions are also used for patients who are colonized with organisms that are
epidemiologically-important. Examples of contact precaution organisms include herpes simplex,
scabies, streptococcus, and gastrointestinal colonization by drug resistant organisms.
In addition to Standard Precautions,
Patients must be placed in a private room or with another patient who has an active infection
with the same organism.
Gloves must be worn when entering the patient’s room. Gloves should be changed after
handling material that may have high concentrations of organisms. Gloves must be removed
before leaving the patient’s room and hands washed with an antimicrobial soap.
Caregivers must ensure that hands do not touch potentially contaminated environmental
surfaces after glove removal.
A gown should be worn if substantial contact with the patient or environmental surfaces is
anticipated or if the patient is incontinent, has diarrhea, an ostomy site, or other drainage not
contained by a dressing. The gown should be removed prior to leaving the room and care taken
to avoid touching surfaces after removing the gown.
Patient transport should be limited to that which is absolutely necessary. Care should be taken
during transport to minimize contact with other patients or environmental surfaces.
Non-critical patient care equipment should be used only for a single patient. If sharing of
common equipment is absolutely necessary, the equipment must be adequately cleaned and
disinfected before using it for another patient. (See sections on Sterilization of Reusable
medical Instruments/Devices and section on Housekeeping/Decontamination)
Note: Please see Guidelines for VRE and MRSA in addition to Contact Precautions.
1.4.4
Synopsis of Types of Precautions and Patients Requiring the Precautions*
Standard Precautions
Use Standard Precautions for the care of all patients
Airborne Precautions
In addition to Standard Precautions, use Airborne Precautions for patients known or suspected to
have serious illnesses transmitted by airborne droplet nuclei. Examples of such illnesses include:
Measles
Varicella (including disseminated zoster) +
Tuberculosis ++
Droplet Precautions
In addition to Standard Precautions, use Droplet Precautions for patients known or suspected to
have serious illnesses transmitted by large particle droplets. Examples of such illnesses include:
Invasive Haemophilus influenzae type b disease, including meningitis, pneumonia,
epiglottitis, and sepsis
Invasive Neisseria meningitidis disease, including meningitis, pneumonia, and sepsis
Other serious bacterial respiratory infections spread by droplet transmission, including:
Diphtheria (pharyngeal)
Mycoplasma pneumonia
Pertussis
Pneumonic plague

5
Streptococcal pharyngitis, pneumonia, or scarlet fever in infants and young children
Serious viral infections spread by droplet transmission, including: Adenovirus
+
Influenza Mumps
Parvovirus B19
Rubella
Contact Precautions
In addition to Standard Precautions, use Contact Precautions for patients known or suspected to have
serious illnesses easily transmitted by direct patient contact or by contact with items in the patient's
environment. Examples of such illnesses include:
Gastrointestinal, respiratory, skin, or wound infections or colonization with multidrug-
resistant bacteria judged by the infection control program, based on current state, regional,
or national recommendations, to be of special clinical and epidemiologic significance
Enteric infections with a low infectious dose or prolonged environmental survival,
including:
Clostridium difficile
For diapered or incontinent patients: enterohemorrhagic Escherichia coli
(O157:H7), Shigella, hepatitis A, or rotavirus
Respiratory syncytial virus, parainfluenza virus, or enteroviral infections in infants and
young children
Skin infections that are highly contagious or that may occur on dry skin, including:
Diphtheria (cutaneous)
Herpes simplex virus (neonatal or mucocutaneous) Impetigo
Noncontained abscesses, cellulitis, or decubiti
Pediculosis
Scabies
Staphylococcal furunculosis in infants and young children
Herpes or Varicella Zoster (disseminated or in the immunocompromised host) +
Viral/hemorrhagic conjunctivitis
Viral hemorrhagic infections (Ebola, Lassa, or Marburg) *
* See Appendix A for a complete listing of infections requiring precautions, including appropriate footnotes.
+ Certain infections require more than one type of precaution.
++ See CDC Guidelines for Preventing the Transmission of Tuberculosis in Health-Care Facilities.
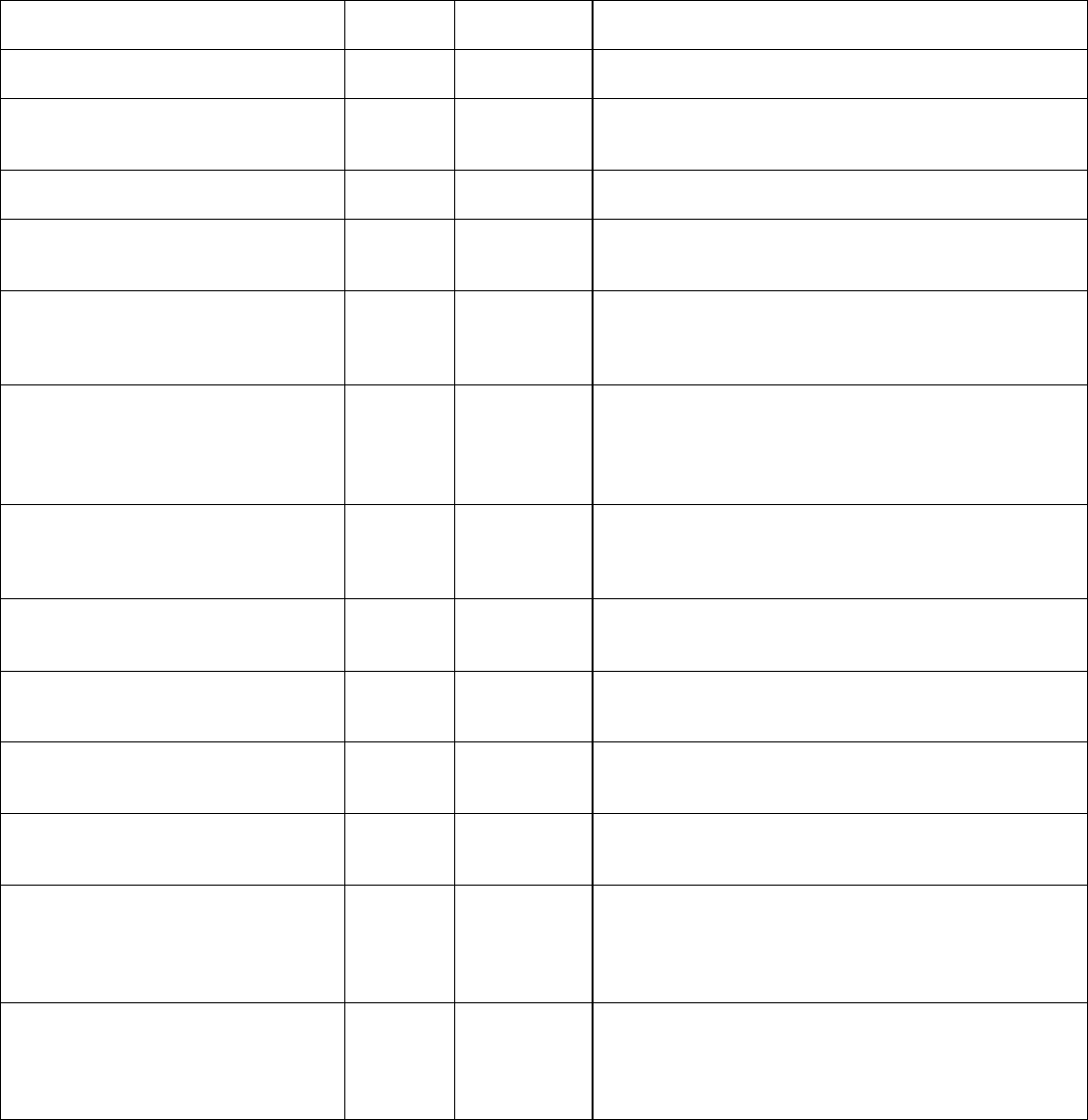
1.5
Empiric Use of Transmission-Based Precautions - Pending Confirmation of Diagnosis
Infection/Condition
Type of
Precaution
Duration of
Precaution
Precautions/Comments
Adenovirus infection (see agent-
specific guidance under gastroenteritis,
conjunctivitis, pneumonia)
Amebiasis
Standard
Person to person transmission is rare. Transmission
in settings for the mentally challenged and in a family
group has been reported [1045]. Use care when
handling diapered infants and mentally challenged
persons [1046].
Anthrax
Standard
Infected patients do not generally pose a
transmission risk.

6
Anthrax
Cutaneous
Standard
Transmission through non-intact skin contact with
draining lesions possible, therefore use Contact
Precautions if large amount of uncontained drainage.
Handwashing with soap and water preferable to use of
waterless alcohol based antiseptics since alcohol does
not have sporicidal activity [983].
Anthrax
Pulmonary
Standard
Not transmitted from person to person
Anthrax
Environmental: aerosolizable
spore-containing powder or other
substance
Until
environment
completely
decontaminated
Until decontamination of environment complete [203].
Wear respirator (N95 mask or PAPRs), protective
clothing; decontaminate persons with powder on them
(Occupational Health Guidelines for Remediation
Workers at Bacillus anthracis-Contaminated Sites ---
United States, 2001--2002
(https://www.cdc.gov/mmwr/preview/mmwrhtml/mm51
3 5a3.htm))
Hand hygiene: Handwashing for 30-60 seconds with
soap and water or 2% chlorhexidene gluconate after
spore contact (alcohol handrubs inactive against
spores [983].
Post-exposure prophylaxis following environmental
exposure: 60 days of antimicrobials (either doxycycline,
ciprofloxacin, or levofloxacin) and post-exposure
vaccine under IND
Antibiotic-associated colitis (see
Clostridium difficile)
Arthropod-borne
viral encephalitides (eastern,
western, Venezuelan equine
encephalomyelitis; St Louis,
California encephalitis; West Nile
Virus) and
viral fevers (dengue yellow fever
Standard
Not transmitted from person to person except rarely by
transfusion, and for West Nile virus by organ
transplant, breastmilk or transplacentally [530, 1047].
Install screens in windows and doors in endemic
areas.
Use DEET-containing mosquito repellants and
clothing to cover extremities.
Blastomycosis, North American,
cutaneous or pulmonary
Standard
Not transmitted from person to person
Botulism
Standard
Not transmitted from person to person
Bronchiolitis (see respiratory infections
in infants and young children)
Contact +
Standard
Duration of
illness
Use mask according to Standard Precautions.
Brucellosis (undulant, Malta,
Mediterranean fever)
Standard
Not transmitted from person to person except rarely
via banked spermatozoa and sexual contact [1048,
1049]. Provide antimicrobial prophylaxis following
laboratory exposure [1050].
Campylobacter gastroenteritis (see
gastroenteritis)
Candidiasis, all forms including
mucocutaneous
Standard
Cat-scratch fever (benign inoculation
lymphoreticulosis)
Standard
Not transmitted from person to person
Cellulitis
Standard
Chancroid (soft chancre) (H. ducreyi)
Standard
Transmitted sexually from person to person
Chickenpox (see >varicella)
Chlamydia trachomatis
Conjunctivitis
Standard

7
Chlamydia trachomatis
Genital (lymphogranuloma
venereum)
Standard
Chlamydia trachomatis
age)
Standard
Chlamydia pneumoniae
Standard
Outbreaks in institutionalized populations
reported, rarely [1051, 1052].
Cholera (see gastroenteritis)
Closed-cavity infection
Open drain in place; limited or
minor drainage
Standard
Contact Precautions if there is copious
uncontained drainage
Closed-cavity infection
No drain or closed drainage
system in place
Standard
Clostridium botulinum
Standard
Not transmitted from person to person
Clostridium difficile (see gastroenteritis,
C. difficile)
Contact +
Standard
Duration of
illness
Clostridium perfringens
Food poisoning
Standard
Not transmitted from person to person
Clostridium perfringens
Gas gangrene
Standard
Transmission from person to person rare; one
outbreak in a surgical setting reported [1053]. Use
Coccidioidomycosis (valley fever)
Pneumonia
Standard
Not transmitted from person to person except under
extraordinary circumstances, (e.g., inhalation of
aerosolized tissue phase endospores during
necropsy, transplantation of infected lung) because
the infectious arthroconidial form of Coccidioides
immitis is not produced in humans [1054, 1055].
Colorado tick fever
Standard
Not transmitted from person to person
Congenital rubella
Contact +
Standard
Until 1 yr of age
Standard Precautions if nasopharyngeal and
urine cultures repeatedly neg. after 3 mos. of age
Conjunctivitis
Acute bacterial
Standard
Conjunctivitis
Acute bacterial
Chlamydia
Standard
Conjunctivitis
Acute bacterial
Gonococcal
Standard
Conjunctivitis
Acute viral (acute hemorrhagic)
Contact +
Standard
Duration of
illness
Adenovirus most common; enterovirus 70 [1056],
Coxsackie virus A24 [1057] also associated with
community outbreaks. Highly contagious; outbreaks in
eye clinics, pediatric and neonatal settings, institutional
settings reported. Eye clinics should follow Standard
Precautions when handling patients with conjunctivitis.
Routine use of infection control measures in the
handling of instruments and equipment will prevent the
occurrence of outbreaks in this and other settings.
[460, 814, 1058, 1059 461, 1060].
Corona virus associated with SARS
(SARS-CoV) (see severe acute
respiratory syndrome)
Coxsackie virus disease (see
enteroviral infection)

8
Creutzfeldt-Jakob disease (CJD, vCJD)
Standard
Use disposable instruments or special
sterilization/disinfection for surfaces, objects
contaminated with neural tissue if CJD or vCJD
suspected and has not been R/O; No special
burial procedures [1061]
Croup (see respiratory infections in
infants and young children)
Crimean-Congo Fever (see Viral
Hemorrhagic Fever)
Standard
Cryptococcosis
Standard
Not transmitted from person to person, except rarely
via tissue and corneal transplant [1062, 1063]
Cryptospor d os s (see gastroenter t s)
Diphtheria
Cutaneous
Contact +
Standard
Until off
antimicrobial
treatment and
culture-negative
Until 2 cultures taken 24 hours apart negative
Diphtheria
Pharyngeal
Droplet +
Standard
Until off
antimicrobial
treatment and
culture-negative
Until 2 cultures taken 24 hours apart negative
Ebola virus (see viral hemorrhagic
fevers)
Ebola Virus Disease for Healthcare
Workers [2014]: Update: Updated
recommendations for healthcare workers can
be found at Ebola: U.S. Healthcare Workers
and Settings
Echinococcosis (hydatidosis)
Standard
Not transmitted from person to person
Echovirus (see enteroviral infection)
Encephalitis or encephalomyelitis (see
specific etiologic agents)
Endometritis (endomyometritis)
Standard
Enterobiasis (pinworm disease,
oxyuriasis)
Standard
Enterococcus species (see multidrug-
resistant organisms if epidemiologically
significant or vancomycin resistant)
Enterocolitis, C. difficile (see C.
difficile, gastroenteritis)
Enteroviral infections (i.e., Group A
and B Coxsackie viruses and Echo
viruses) (excludes polio virus)
Standard
Use Contact Precautions for diapered or incontinent
children for duration of illness and to control
institutional outbreaks
Epiglottitis, due to Haemophilus
influenzae type b
Droplet +
Standard
Until 24 hours
after initiation of
effective
therapy
See specific disease agents for epiglottitis due to
other etiologies)
Epstein-Barr virus infection, including
infectious mononucleosis
Standard
Erythema infectiosum (also see
Parvovirus B19)
Escherichia coli gastroenteritis (see
gastroenteritis)
Food poisoning
Botulism
Standard
Not transmitted from person to person
Food poisoning
C. perfringens or welchii
Standard
Not transmitted from person to person

9
Gastroenteritis
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
Adenovirus
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
Campylobacter species
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
Cholera (Vibrio cholerae)
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
C. difficile
Contact +
Standard
Duration of
illness
Discontinue antibiotics if appropriate. Do not share
electronic thermometers [853], 854; ensure consistent
Gastroenteritis
Cryptosporidium species
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
E. coli
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
E. coli
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
Giardia lamblia
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
Noroviruses
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
Gastroenteritis
Salmonella species (including S.
typhi)
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
institutional outbreaks
Gastroenteritis
Shigella species (Bacillary
dysentery)
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
institutional outbreaks
Gastroenteritis
Vibrio parahaemolyticus
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
institutional outbreaks
Gastroenteritis
Viral (if not covered elsewhere)
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
institutional outbreaks
Gastroenteritis
Yersinia enterocolitica
Standard
Use Contact Precautions for diapered or incontinent
persons for the duration of illness or to control
institutional outbreaks
German measles (see rubella; see
congenital rubella)
Giardiasis (see gastroenteritis)
Gonococcal ophthalmia neonatorum
(gonorrheal ophthalmia, acute
conjunctivitis of newborn)
Standard
Gonorrhea
Standard
Granuloma inguinale (Donovanosis,
granuloma venereum)
Standard
Guillain-Barre' syndrome
Standard
Not an infectious condition
Haemophilus influenzae (see disease-
specific recommendations)
Hand, foot, and mouth disease (see
enteroviral infection)
Hansen's Disease (see Leprosy)
Hantavirus pulmonary syndrome
Standard
Not transmitted from person to person
Helicobacter pylori
Standard

10
Hepatitis, viral
Type A
Standard
Provide hepatitis A vaccine post-exposure as
recommended [1065]
Hepatitis, viral
Type A-Diapered or incontinent
patients
Contact +
Standard
Maintain Contact Precautions in infants and children <3
years of age for duration of hospitalization; for children
3-14 yrs. of age for 2 weeks after onset of symptoms;
>14 yrs. of age for 1 week after onset of symptoms
[833, 1066, 1067].
Hepatitis, viral
Type B-HBsAg positive; acute or
chronic
Standard
See specific recommendations for care of patients in
hemodialysis centers 778
Standard
See specific recommendations for care of patients
Herpangina (see enteroviral infection)
Hookworm
Standard
Herpes simplex (Herpesvirus hominis)
Encephalitis
Standard
Herpes simplex (Herpesvirus hominis)
Mucocutaneous, disseminated or
primary, severe
Contact
+
Standard
Until lesions dry
and crusted
Herpes simplex (Herpesvirus hominis)
Mucocutaneous, recurrent (skin,
oral, genital)
Standard
Herpes simplex (Herpesvirus hominis)
Neonatal
Contact
+
Standard
Until lesions dry
and crusted
Also, for asymptomatic, exposed infants delivered
vaginally or by C-section and if mother has active
infection and membranes have been ruptured for more
than 4 to 6 hours until infant surface cultures obtained at
24-36 hours. of age negative after 48 hours incubation
[1069, 1070]
Herpes zoster (varicella-zoster)
(shingles)
Disseminated disease in any
patient
Localized disease in
immunocompromised
patient until disseminated
infection ruled out
Airborne
+
Contact +
Standard
Duration of
illness
Susceptible HCWs should not enter room if immune
caregivers are available; no recommendation for
protection of immune HCWs; no recommendation for
type of protection, i.e. surgical mask or respirator; for
susceptible HCWs.
Herpes zoster (varicella-zoster)
(shingles)
Localized in patient with intact
immune system with lesions that
can be contained/covered
Standard
Duration of
illness (with
wound lesions,
until wounds
stop draining)
Susceptible HCWs should not provide direct patient
care when other immune caregivers are available.
Histoplasmosis
Standard
Not transmitted from person to person
Human immunodeficiency virus (HIV)
Standard
Post-exposure chemoprophylaxis for some blood
exposures [866].
Human metapneumovirus
Contact
+
Standard
Duration of
illness (with
wound lesions,
until wounds
stop draining)
HAI reported [1071], but route of transmission not
established [823]. Assumed to be Contact transmission
as for RSV since the viruses are closely related and
have similar clinical manifestations and epidemiology.
Wear masks according to Standard Precautions.
Impetigo
Contact
+
Standard
Until 24 hours
after initiation of
effective
therapy
Infectious mononucleosis
Standard
Influenza
Human (seasonal influenza)
-
See Prevention Strategies for Seasonal Influenza in
Hea thcare Sett ngs

11
Influenza
Avian (e.g., H5N1, H7, H9
strains)
-
See [This link is no longer active:
www.cdc.gov/flu/avian/professional/infect-control.htm.
Similar information may be found at Interim Guidance
for Infection Control Within Healthcare Settings When
Caring for Confirmed Cases, Probable Cases, and
Cases Under Investigation for Infection with Novel
Influenza A Viruses Associated with Severe Disease
(https://www.cdc.gov/flu/avianflu/novel-flu-infection-
control.htm), accessed May 2016.] for current avian
Influenza guidance.
Influenza
Pandemic Influenza (also a
human Influenza virus)
Droplet
See [This link is no longer active:
http://www.pandemicflu.gov. Similar information may be
found at Interim Guidance for Infection Control Within
Healthcare Settings When Caring for Confirmed Cases,
Probable Cases, and Cases Under Investigation for
Infection with Novel Influenza A Viruses Associated with
Severe Disease (https://www.cdc.gov/flu/avianflu/novel-
flu-infection- control.htm), accessed May 2016.] for
current pandemic Influenza guidance.
Kawasaki syndrome
Standard
Not an infectious condition
Lassa fever (see viral hemorrhagic
fevers)
-
Legionnaires' disease
Standard
Not transmitted from person to person
Leprosy
Standard
Leptospirosis
Standard
Not transmitted from person to person
Lice
Head (pediculosis)
Contact +
Standard
Until 24 hours
after initiation
of effective
therapy
See [This link is no longer active: http://www.cdc.gov/
ncidod/dpd/parasites/lice/default.htm.
Similar
information may be found at CDC’s Parasites - Lice
(https://www.cdc.gov/parasites/lice/index.html),
accessed May 2016.]
Lice
Body
Standard
Transmitted person to person through infested clothing.
Wear gown and gloves when removing clothing; bag
and wash clothes according to CDC guidance [This link
is no longer active: http://www.cdc.gov/ncidod/dpd/
parasites/lice/default.htm. Similar information may be
found at CDC’s Parasites - Lice
(https://www.cdc.gov/parasites/lice/index.html),
accessed May 2016.]
Lice
Pubic
Standard
Transmitted person to person through sexual contact.
See CDC’s [This link is no longer active:
http://www.cdc.gov/ncidod/dpd/parasites/lice/default.ht
m. Similar information may be found at CDC’s
Parasites - Lice
Malaria
Standard
Not transmitted from person to person except through
transfusion rarely and through a failure to follow
Standard Precautions during patient care 1076-1079.
Install screens in windows and doors in endemic areas.
Use DEET-containing mosquito repellants and clothing
to cover extremities.
Marburg virus disease (see viral
hemorrhagic fevers)
-

12
Measles (rubeola)
Airborne +
Standard
4 days after
onset of rash;
duration of
illness (with
wound lesions,
until wounds
stop draining)
in immune
compromised
Measles Update [November 2011]: Updated
recommendations can be found at Immunization
of Healthcare Personnel: Recommendations of
the Advisory Committee on Immunization
Practices (ACIP)
(https://www.cdc.gov/mmwr/pdf/rr/rr6007.pdf).
Susceptible HCWs should not enter room if immune
care providers are available; no recommendation for
face protection for immune HCW; no recommendation
for type of face protection for susceptible HCWs, i.e.,
mask or respirator [1027, 1028]. For exposed
susceptibles, post-exposure vaccine within 72 hours or
immune globulin within 6 days when available [17,
1032, 1034]. Place exposed susceptible patients on
Airborne Precautions and exclude susceptible
healthcare personnel.
Melioidosis, all forms
Standard
Not transmitted from person to person.
Meningitis
Aseptic (nonbacterial or viral;
also see enteroviral infections)
Standard
Contact for infants and young children.
Meningitis
Bacterial, gram-negative enteric,
in neonates
Standard
Meningitis
Fungal
Standard
Meningitis
Haemophilus Influenzae, type b
known or suspected
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
Meningitis
Listeria monocytogenes (See
Listeriosis)
Standard
Meningitis
Neisseria meningitidis
(meningococcal) known or
suspected
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
See meningococcal disease below.
Meningococcal disease: sepsis,
pneumonia, Meningitis
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
Postexposure chemoprophylaxis for household
contacts, HCWs exposed to respiratory secretions;
postexposure vaccine only to control outbreaks
15, 17
.
Molluscum contagiosum
Standard
Monkeypox
Airborne +
Contact +
Standard
Airborne-Until
monkeypox
confirmed and
smallpox
excluded
Contact-Until
lesions
See CDC’s Monkeypox website
(https://www.cdc.gov/poxvirus/monkeypox/)
[Current
version of this document may differ from original.] for
most current recommendations. Transmission in
hospital settings unlikely [269]. Pre- and post-exposure
smallpox vaccine recommended for exposed HCWs
Mucormycosis
Standard
13
Multidrug-resistant organisms
(MDROs), infection or colonization
(e.g., MRSA, VRE, VISA/VRSA,
ESBLs, resistant S. pneumoniae)
Contact +
Standard
MDROs judged by the infection control program, based
on local, state, regional, or national recommendations,
to be of clinical and epidemiologic significance. Contact
Precautions recommended in settings with evidence of
ongoing transmission, acute care settings with
increased risk for transmission or wounds that cannot
be contained by dressings. See recommendations for
management options in Management of Multidrug-
Resistant Organisms In Healthcare Settings, 2006
(https://www.cdc.gov/infectioncontrol/guidelines/mdro/)
[870]. Contact state health department for guidance
regarding new or emerging MDRO.
Mumps (infectious parotitis)
Droplet +
Standard
Until 9 days
After onset of swelling; susceptible HCWs should not
provide care if immune caregivers are available.
Note: (Recent assessment of outbreaks in healthy 18- 24
year olds has indicated that salivary viral shedding
occurred early in the course of illness and that 5 days of
isolation after onset of parotitis may be appropriate in
community settings; however the implications for
healthcare personnel and high-risk patient populations
remain to be clarified.)
Mycobacteria, nontuberculosis
(atypical)
Not transmitted person-to-person
Mycobacteria, nontuberculosis
(atypical)
Pulmonary
Standard
Mycobacteria, nontuberculosis
(atypical)
Wound
Standard
Mycoplasma pneumonia
Droplet +
Standard
Duration
of
Parainfluenza virus infection,
respiratory in infants and young
children
Contact +
Standard
Duration
of
illness
Viral shedding may be prolonged in immunosuppressed
patients [1009, 1010]. Reliability of antigentesting to
determine when to remove patients with prolonged
hospitalizations from Contact Precautions uncertain.
Parvovirus B19 (Erythema infectiosum)
Droplet +
Standard
Maintain precautions for duration of hospitalization when
chronic disease occurs in an immunocompromised
patient. For patients with transient aplastic crisis or red-
cell crisis, maintain precautions for 7 days. Duration of
precautions for immunosuppressed patients with
persistently positive PCR not defined, but transmission
has occurred [929].
Pediculosis (Lice)
Contact +
Standard
Until 24 hours
after initiation
of effective
therapy after
treatment

14
Pertussis (whooping cough)
Droplet +
Standard
Until 5 days
Single patient room preferred. Cohorting an option.
Post-exposure chemoprophylaxis for household
contacts and HCWs with prolonged exposure to
respiratory secretions [863]. Recommendations for
Tdap vaccine in adults under development.
Tdap Vaccine Recommendations [2011]
Update: Current recommendations can be found
at Tdap / Td ACIP Vaccine Recommendations
(www.cdc.gov/vaccines/hcp/acip-recs/vacc-
specific/tdap-td.html).
Pinworm infection (Enterobiasis)
Standard
Plague (Yersinia pestis)
Bubonic
Standard
Plague (Yersinia pestis)
Pneumonic
Droplet +
Standard
Until 48 hours
Antimicrobial prophylaxis for exposed HCW [207].
Pneumonia
Adenovirus
Droplet +
Contact +
Standard
Duration
of
illness
Outbreaks in pediatric and institutional settings reported
[376, 1084-1086]. In immunocompromised hosts, extend
duration of Droplet and Contact Precautions due to
prolonged shedding of virus [931]
Pneumonia
Bacterial not listed elsewhere
(including gram-negative
bacterial)
Standard
Pneumonia
B. cepacia in patients with CF,
including respiratory tract
colonization
Contact +
Standard
Unknown
Avoid exposure to other persons with CF; private room
preferred. Criteria for D/C precautions not established.
See CF Foundation guideline [20]
Pneumonia
Pneumonia
Haemophilus influenzae, type b
Adults
Standard
Pneumonia
Haemophilus influenzae, type b
Infants and children
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
Pneumonia
Legionella spp.
Standard
Pneumonia
Meningococcal
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
See meningococcal disease above
Pneumonia
Multidrug-resistant bacterial (see
multidrug-resistant organisms)
Pneumonia
Mycoplasma (primary atypical
Pneumonia)
Droplet
Duration
of
illness
Pneumonia
Pneumococcal pneumonia
Standard
Use Droplet Precautions if evidence of transmission
within a patient care unit or facility [196-198, 1087]
Pneumonia
Pneumocystis jiroveci
(Pneumocystis carinii)
Standard
Avoid placement in the same room with an
immunocompromised patient.
Pneumonia
Staphylococcus aureus
Standard
For MRSA, see MDROs

15
Pneumonia
Streptococcus, group A
Adults
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
See streptococcal disease (group A streptococcus)
below
Contact precautions if skin lesions present
Pneumonia
Streptococcus, group A
Infants and young children
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
Contact Precautions if skin lesions present
Pneumonia
Varicella-zoster (See Varicella-
Zoster)
Pneumonia
Viral
Adults
Standard
Pneumonia
Viral
Infants and young children
(see resp ratory nfect ous
Pressure ulcer (decubitus ulcer,
pressure sore) infected
Major
Contact +
Standard
Duration of
illness (with
wound
lesions, until
wounds stop
If no dressing or containment of drainage; until drainage
stops or can be contained by dressing
Pressure ulcer (decubitus ulcer,
pressure sore) infected
Minor or limited
Standard
If dressing covers and contains drainage
Prion disease (See Creutzfeld-Jacob
Disease)
Psittacosis (ornithosis) (Chlamydia
psittaci)
Standard
Not transmitted from person to person
Q fever
Standard
Rabies
Standard
Person to person transmission rare; transmission via
corneal, tissue and organ transplants has been reported
[539, 1088]. If patient has bitten another individual or
saliva has contaminated an open wound or mucous
membrane, wash exposed area thoroughly and
administer postexposure prophylaxis. [1089]
Rat-bite fever (Streptobacillus
moniliformis disease, Spirillum minus
disease)
Standard
Not transmitted from person to person
Relapsing fever
Standard
Not transmitted from person to person
Resistant bacterial infection or
colonization (see multidrug-resistant
organisms)
Respiratory infectious disease, acute
(if not covered elsewhere)
Adults
Standard
Respiratory infectious disease, acute
(if not covered elsewhere)
Infants and young children
Contact +
Standard
Duration of
illness (with
wound
lesions, until
wounds stop
Also see syndromes or conditions listed in Table 2

16
Respiratory syncytial virus infection, in
infants, young children and
immunocompromised adults
Contact +
Standard
Duration of
illness (with
wound
lesions, until
wounds stop
draining)
Wear mask according to Standard Precautions [24] CB
[116, 117]. In immunocompromised patients, extend the
duration of Contact Precautions due to prolonged
shedding [928]). Reliability of antigen testing to
determine when to remove patients with prolonged
hospitalizations from Contact Precautions uncertain.
Reye's syndrome
Standard
Not an infectious condition
Rheumatic fever
Standard
Not an infectious condition
Rhinovirus
Droplet +
Duration of
Droplet most important route of transmission [104
Ringworm (dermatophytosis,
dermatomycosis, tinea)
Standard
Rarely, outbreaks have occurred in healthcare settings,
(e.g., NICU [1093], rehabilitation hospital [1094]. Use
Contact Precautions for outbreak.
Ritter's disease (staphylococcal
scalded skin syndrome)
Contact +
Standard
Duration of
illness (with
wound
lesions, until
wounds stop
See staphylococcal disease, scalded skin syndrome
below
Rocky Mountain spotted fever
Standard
Not transmitted from person to person except through
transfusion,
rarely
Roseola infantum (exanthem subitum;
caused by HHV-6)
Standard
Rotavirus infection (see gastroenteritis)
Rubella (German measles) ( also see
congenital rubella)
Droplet +
Standard
Until 7 days
after onset
of rash
Susceptible HCWs should not enter room if immune
caregivers are available. No recommendation for
wearing face protection (e.g., a surgical mask) if
immune. Pregnant women who are not immune should
not care for these patients [17, 33]. Administer vaccine
within three days of exposure to non-pregnant
susceptible individuals. Place exposed susceptible
patients on Droplet Precautions; exclude susceptible
healthcare personnel from duty from day 5 after first
exposure to day 21 after last exposure, regardless of
post-exposure vaccine.
Rubeola (see measles)
Salmonellosis (see gastroenteritis)
Scabies
Contact
Until 24
Scalded skin syndrome,
staphylococcal
Contact
Duration of
illness (with
wound
lesions, until
wounds stop
See staphylococcal disease, scalded skin syndrome
below)
Schistosomiasis (bilharziasis)
Standard
Severe acute respiratory syndrome
Airborne +
Droplet +
Contact +
Duration of
illness (with
wound lesions,
until wounds
stop draining)
plus 10 days
after resolution
of fever,
provided
respiratory
Airborne preferred; D if AIIR unavailable. N95 or higher
respiratory protection; surgical mask if N95 unavailable;
eye protection (goggles, face shield); aerosol-
generating procedures and "supershedders" highest
risk for transmission via small droplet nuclei and large
droplets [93, 94, 96]. Vigilant environmental disinfection
(see [This link is no longer active:
www.cdc.gov/ncidod/sars. Similar information may be
found at CDC Severe Acute Respiratory Syndrome
(SARS) (https://www.cdc.gov/sars/index.html),
Sporotrichosis
Standard

17
Spirillum minor disease (rat-bite fever)
Standard
Not transmitted from person to person
Staphylococcal disease (S aureus)
Skin, wound, or burn
Major
Contact
Duration of
illness (with
wound
lesions, until
wounds stop
No dressing or dressing does not contain drainage
adequately
Staphylococcal disease (S aureus)
Skin, wound, or burn
Minor or limited
Standard
Dressing covers and contains drainage adequately
Staphylococcal disease (S aureus)
Enterocolitis
Standard
Use Contact Precautions for diapered or incontinent
children for duration of illness
Staphylococcal disease (S aureus)
Multidrug-resistant (see
multidrug-resistant organisms)
Staphylococcal disease (S aureus)
Pneumonia
Standard
Staphylococcal disease (S aureus)
Scalded skin syndrome
Contact
Duration of
illness (with
wound
lesions, until
wounds stop
Consider healthcare personnel as potential source of
nursery, NICU outbreak [1095].
Staphylococcal disease (S aureus)
Toxic shock syndrome
Standard
Streptobacillus moniliformis disease
(rat-bite fever)
Standard
Not transmitted from person to person
Streptococcal disease (group A
streptococcus)
Skin, wound, or burn
Major
Contact +
Droplet +
Standard
Until 24 hours
after initiation
of effective
therapy
No dressing or dressing does not contain drainage
adequately
Streptococcal disease (group A
streptococcus)
Skin, wound, or burn
Minor or limited
Standard
Dressing covers and contains drainage adequately
Streptococcal disease (group A
streptococcus)
Endometritis (puerperal sepsis)
Standard
Streptococcal disease (group A
streptococcus)
Pharyngitis in infants and young
children
Droplet
Until 24 hours
after initiation
of effective
therapy
Streptococcal disease (group A
streptococcus)
Droplet
Until 24 hours
after initiation
Streptococcal disease (group A
streptococcus)
Serious invasive disease
Droplet
Until 24 hours
after initiation
of effective
therapy
Outbreaks of serious invasive disease have occurred
secondary to transmission among patients and
healthcare personnel [162, 972, 1096-1098]
Contact Precautions for draining wound as above;
follow rec. for antimicrobial prophylaxis in selected
conditions [160].
Streptococcal disease (group B
streptococcus), neonatal
Standard
Streptococcal disease (not group A or
B) unless covered elsewhere
Multidrug-resistant (see
multidrug-resistant organisms)

18
Strongyloidiasis
Standard
Syphilis
Latent (tertiary) and seropositivity
without lesions
Standard
Syphilis
Skin and mucous membrane,
including congenital, primary,
secondary
Standard
Tapeworm disease
Hymenolepis nana
Standard
Not transmitted from person to person
Tapeworm disease
Taenia solium (pork)
Standard
Tapeworm disease
Other
Standard
Tetanus
Standard
Not transmitted from person to person
Tinea (e.g., dermatophytosis,
dermatomycosis, ringworm)
Standard
Rare episodes of person-to-person transmission
Toxoplasmosis
Standard
Transmission from person to person is rare; vertical
transmission from mother to child, transmission through
organs and blood transfusion rare
Toxic shock syndrome (staphylococcal
disease, streptococcal disease)
Standard
Droplet Precautions for the first 24 hours after
implementation of antibiotic therapy if Group A
streptococcus is a likely etiology
Trachoma, acute
Standard
Transmissible spongiform
encephalopathy (see Creutzfeld-Jacob
disease, CJD, vCJD)
Trench mouth (Vincent's angina)
Standard
Trichinosis
Standard
Trichomoniasis
Standard
Trichuriasis (whipworm disease)
Standard
Tuberculosis (M. tuberculosis)
Pulmonary or laryngeal disease,
confirmed
Airborne
Discontinue precautions only when patient on effective
therapy is improving clinically and has three
consecutive sputum smears negative for acid-fast
bacilli collected on separate days (MMWR 2005; 54:
RR-17 Guidelines for Preventing the Transmission of
Mycobacterium tuberculosis in Health-Care Settings,
2005
(https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a
1.htm?s_cid=rr5417a1_e)) [12].
Tuberculosis (M. tuberculosis)
Pulmonary or laryngeal disease,
suspected
Airborne
Discontinue precautions only when the likelihood of
infectious TB disease is deemed negligible, and either
1.
there is another diagnosis that explains the clinical
syndrome or
2.
the results of three sputum smears for AFB are
negative. Each of the three sputum specimens
should be collected 8-24 hours apart, and at least
one should be an early morning specimen
Tuberculosis (M. tuberculosis)
Skin-test positive with no
evidence of current active
disease
Standard
Tularemia
Draining lesion
Standard
Not transmitted from person to person
19
Tularemia
Pulmonary
Standard
Not transmitted from person to person
Typhoid (Salmonella typhi) fever (see
gastroenteritis)
Typhus
Rickettsia prowazekii (Epidemic
or Louse-borne Typhus)
Standard
Transmitted from person to person through close
personal or clothing contact
Typhus
Rickettsia typhi
Standard
Not transmitted from person to person
Urinary tract infection (including
pyelonephritis), with or without urinary
catheter
Standard
Vaccinia
Only vaccinated HCWs have contact with active
vaccination sites and care for persons with adverse
vaccinia events; if unvaccinated, only HCWs without
contraindications to vaccine may provide care.
Vaccinia
Vaccination site care (including
autoinoculated areas)
Standard
Vaccination recommended for vaccinators; for newly
vaccinated HCWs: semi-permeable dressing over
gauze until scab separates, with dressing change as
fluid accumulates, ~3-5 days; gloves, hand hygiene for
dressing change; vaccinated HCW or HCW without
Vaccinia (adverse events following
vaccination)
Generalized vaccinia
Contact
Until lesions
dry and
crusted, scabs
separated
For contact with virus-containing lesions and exudative
material
Vaccinia (adverse events following
vaccination)
Progressive vaccinia
Contact
For contact with virus-containing lesions and exudative
material
Vaccinia (adverse events following
vaccination)
PostVaccinia encephalitis
Standard
Vaccinia (adverse events following
vaccination)
Blepharitis or conjunctivitis
Contact +
Standard
Use Contact Precautions if there is copious drainage
Vaccinia (adverse events following
vaccination)
Iritis or keratitis
Standard
Vaccinia (adverse events following
vaccination)
Vaccinia-associated erythema
multiforme (Stevens Johnson
Syndrome)
Standard
Not an infectious condition
Vaccinia (adverse events following
vaccination)
Secondary bacterial infection
(e.g., S. aureus, group A beta
hemolytic streptococcus)
Standard +
Contact
Follow organism-specific (strep, staph most frequent)
recommendations and consider magnitude of drainage

20
Varicella Zoster
Airborne +
Contact +
Standard
Until lesions
dry and
crusted
Susceptible HCWs should not enter room if immune
caregivers are available; no recommendation for face
protection of immune HCWs; no recommendation for type
of protection, i.e., surgical mask or respirator for
susceptible HCWs. In immunocompromised host with
varicella Pneumonia, prolong duration of precautions for
duration of illness. Post-exposure prophylaxis: provide
post-exposure vaccine ASAP but within 120 hours; for
susceptible exposed persons for whom vaccine is
contraindicated (immunocompromised persons, pregnant
women, newborns whose mother's varicella onset is
<5days before delivery or within 48 hours after delivery)
provide VZIG, when available, within 96 hours; if
unavailable, use IVIG, Use Airborne for exposed
susceptible persons and exclude exposed susceptible
healthcare workers beginning 8 days after first exposure
until 21 days after last exposure or 28 if received VZIG,
regardless of postexposure vaccination. [1036].
Viral hemorrhagic fevers due to Lassa,
Ebola, Marburg, Crimean-Congo fever
viruses
Standard +
Droplet +
Contact
Duration of
illness (with
wound
lesions, until
wounds stop
draining)
Ebola Virus Disease Update [2014]: Updated
recommendations for healthcare workers can be
found at Ebola: U.S. Healthcare Workers and
Settings
(https://www.cdc.gov/vhf/ebola/healthcare-us/).
Single-patient room preferred. Emphasize:
use of sharps safety devices and safe work
practices,
hand hygiene;
barrier protection against blood and body fluids
upon entry into room (single gloves and fluid-
resistant or impermeable gown, face/eye protection
with masks, goggles or face shields); and
appropriate waste handling.
Use N95 or higher respirators when performing
aerosol-generating procedures. Largest viral load in
final stages of illness when hemorrhage may occur;
additional PPE, including double gloves, leg and shoe
coverings may be used, especially in resource-limited
settings where options for cleaning and laundry are
limited. Notify public health officials immediately if
Ebola is suspected [212, 314, 740, 772]. Also see
Table 3 for Ebola as a bioterrorism agent.
Viral respiratory diseases (not covered
elsewhere)
Adults
Standard
Viral respiratory diseases (not covered
elsewhere)
Infants and young children (see
respiratory infectious disease,
acute)
Whooping cough (see pertussis)

21
Wound infections
Major
Contact +
Standard
Duration of
illness (with
wound
lesions, until
wounds stop
No dressing or dressing does not contain drainage
adequately
Wound infections
Minor or limited
Standard
Dressing covers and contains drainage adequately
Yersinia enterocolitica Gastroenteritis
(see gastroenteritis)
Zoster (varicella-zoster) (see herpes
Table 1. History of Guidelines for Isolation Precautions in Hospitals*
Year (Ref)
Document Issued
Comment
1970
Isolation Techniques for
Introduced seven isolation precaution categories with
color-coded cards: Strict, Respiratory, Protective,
Enteric, Wound and Skin, Discharge, and Blood
No user decision-making required
Simplicity a strength; over isolation prescribed for some
infections
1975
Isolation Techniques for
1100
Use in Hospitals, 2nd ed.
1983
CDC Guideline for Isolation
Provided two systems for isolation: category-specific
and disease- specific
Protective Isolation eliminated; Blood Precautions
expanded to include Body Fluids
Categories included Strict, Contact, Respiratory, AFB,
Enteric, Drainage/Secretion, Blood and Body Fluids
Emphasized decision-making by users
1985-88
Developed in response to HIV/AIDS epidemic
Dictated application of Blood and Body Fluid
precautions to all patients, regardless of infection status
Did not apply to feces, nasal secretions, sputum, sweat,
tears, urine, or vomitus unless contaminated by visible
blood
Added personal protective equipment to protect HCWs
from mucous membrane exposures
Handwashing recommended immediately after glove
removal
Added specific recommendations for handling needles
and other sharp devices; concept became integral to
OSHA’s 1991 rule on occupational exposure to blood-
borne pathogens in healthcare settings
1987
Emphasized avoiding contact with all moist and
potentially infectious body substances except sweat
even if blood not present
Shared some features with Universal Precautions
Weak on infections transmitted by large droplets or by
contact with dry surfaces
Did not emphasize need for special ventilation to

22
1996
Guideline for Isolation
Prepared by the Healthcare Infection Control Practices
Advisory Committee (HICPAC)
Melded major features of Universal Precautions and
Body Substance Isolation into Standard Precautions to
be used with all patients at all times
Included three transmission-based precaution
categories: airborne, droplet, and contact
Listed clinical syndromes that should dictate use of
empiric isolation until an etiological diagnosis is
established
Derived from Garner ICHE 1996
1.6
TB Exposure Control Plan
Yale University has a procedure in place to prevent and control tuberculosis (TB) in our patients,
employees and students. TB is a potentially severe, contagious disease that primarily affects the
lungs, but can also damage other parts of the body. It is usually transmitted by airborne droplets
containing TB bacteria that are spread by infected persons whenever they cough, speak, or sneeze.
On rare occasions, blood and body fluids may become contaminated with TB. Control measures
include understanding the mode of transmission, signs and symptoms of infection, medical
surveillance and therapy, and site-specific protocols.
In conjunction with the facility Infection Control Coordinator, area managers and supervisors must
conduct a risk assessment of their workplace to determine the risk for occupational transmission of
TB and implement an appropriate exposure control plan. Yale Environmental Health and Safety
and the Employee Health can assist with TB risk assessments.
Risk Assessment
The number of reported TB cases in Connecticut has continued to decline for the past several years.
These rates are monitored by the Connecticut Department of Public Health Tuberculosis Control
Program.
Transmission and Pathogenesis
Tuberculosis is an airborne communicable disease caused by Mycobacterium tuberculosis, the
tubercle bacillus. It is spread primarily by tiny airborne particles (1 - 5 microns in diameter), known
as droplet nuclei, that are generated when a person with infectious TB (pulmonary or laryngal)
sneezes, coughs, speaks, or sings. If another person inhales these droplet nuclei, transmission may
occur. Infection begins with multiplication of tubercle bacilli in alveolar macrophages, some of
which spread through the bloodstream; however, the immune system response usually prevents the
development of disease. Persons infected with TB but who do not develop active TB are often
asymptomatic and not infectious; such persons usually have a positive reaction to the tuberculin
skin test. Only about 10% of infected persons develop active TB disease at some time in their lives,
but the risk is considerably higher for persons who are immunosuppressed, especially those with
HIV infection. Although the majority of TB cases are pulmonary, TB can occur in almost any
anatomical site or as disseminated disease. Extrapulmonary TB can be transmitted through blood
and body fluids.
An extremely serious aspect of TB that has developed over the past two decades is multidrug
resistant strains (MDR TB) that are usually resistant to at least isoniazid and rifampin. Infection
with MDR-TB has a 50 to 80% mortality rate. MDR-TB can usually be prevented by initially
23
treating TB patients with four drugs and by administering TB medications on a directly observed
basis. Persons at higher risk for MDR-TB include those: recently exposed to MDR-TB, especially
the immunocompromised; TB patients who failed to take medications as prescribed; TB patients
who were prescribed an ineffective treatment regimen; and persons previously treated for TB.
Guidelines for TB Control
Employees at risk should be tested for TB exposure by a tuberculin skin test (PPD) or
QuantiFERON serum test at least annually. New employees will be referred to the Employee
Health office (Yale Health, 55 Lock Street, (432-0071) upon being hired for baseline PPD
testing. Employees with potential exposure must be tested within 2 weeks of hire. Employees
with a history of a previous positive PPD or serum test will not be retested but should provide
documentation of a negative chest x-ray as part of their evaluation. Employees exempt from
the tuberculin skin test must be informed about symptoms of TB and the need for immediate
evaluation of any pulmonary symptoms suggestive of TB by their health care provider to
determine if active disease has developed.
University employees and students in contact with patients or clients in hospitals, clinics, or
long term facilities must be tested for TB exposure by a tuberculin skin test (PPD) or
QuantiFERON serum test on an annual basis. This includes students who deliver care, conduct
research or consult individuals. In addition, students who volunteer in correctional facilities,
hospices, shelters for the homeless, or drug/alcohol treatment facilities should be tested on an
annual basis.
Employees and students who test positive on PPD or blood testing will be referred for a chest
x-ray and evaluated for signs of active TB infection. If no signs of active infection (such as
fatigue, fever, chills, night sweats, loss of appetite, weight loss, productive sputum, coughing
up blood (hemoptasis), chest pain, hoarse voice) are present, the employees will be referred for
prophylactic treatment as appropriate following established CDC recommendations.
Health care providers, employees and students (as designated in the above statements) should
be educated through infection control staff about the transmission of TB and appropriate
methods of protection. OSHA compliant TB training will be provided to those in covered risk
groups. Awareness level training will be provided periodically to students and volunteers
working in a health care setting.
Health care providers should concentrate on identifying TB infection among our patient
population.
The following guidelines are recommended for testing groups of patients at high risk for TB
infection:
Patients with history of combined cough, fever, weight loss, night sweats, hemoptysis for
greater than 2 weeks.
Patients with radiographic abnormalities suggestive of TB infection.
Recent contacts with infectious TB cases.
Patients infected with HIV.
Groups at high risk for TB infection such as foreign born persons who arrived within the past
5 years from Asia, Africa, Latin America and Caribbean, medically underserved populations,
long term residents of hospitals, nursing homes, homeless shelters, and correctional facilities.
Patients with underlying medical conditions that increase the risk of TB such as silicosis,
diabetes mellitus, long term corticosteroid therapy, immunosuppressive therapy, injecting
24
drug use, underlying malignancies, end stage renal disease, post gastrectomy, or intestinal by
pass. In addition, anergy testing should also be performed on any patient suspected of being
immunocompromised.
Patients who are identified as having a positive skin test should have a chest x-ray and be
evaluated for signs of active TB by their health care provider. Patients should be referred when
appropriate for curative or prophylactic treatment under CDC guidelines.
TB Exposure Control Procedures for Suspected or Known Active TB Cases
Ask the person/patient presenting symptoms to cover their nose and mouth.
Provide a surgical mask for the person to wear to contain droplets. Recognize the signs and
symptoms of active TB - these include: fatigue, fever, chills, night sweats, loss of appetite and
weight loss. The advanced stages of TB disease include: sputum-producing cough, coughing up
blood, chest pain, and hoarseness of voice.
Isolate patient from other visitors and employees
If available, place any patient strongly suspected of active TB in a room with:
negative air pressure in relation to the surrounding areas that can be monitored,
6 to 12 room air exchanges per hour,
air discharged directly outdoors or through monitored high efficiency particulate aerosol
(HEPA) filters before recirculation to other areas in the facility.
In facilities without an available negative pressure isolation room, post a sign at the entrance of the
room. The sign will have a red and white stop sign with the statement “No Admittance without
Wearing a Type N95 or More Protective Respirator”.
If a facility does not have a negative air flow room
Provide a surgical mask for patient to wear to contain droplets. Any patient who is strongly
suspected of having active TB should be given a molded surgical mask, instructed to keep it on,
and escorted to a private exam room. These areas are not appropriate for strict isolation but can be
used as a separate waiting area for a short duration until transport can be arranged. Post a sign at
the entrance of the room. The health care provider evaluating the patient should make arrangements
to transfer the patient to a facility with an appropriate isolation room to complete the remainder of
the TB work up (i.e. Yale-New Haven Hospital). Ambulance as well as emergency room personnel
at the admitting facility must be notified of the suspected diagnosis so that appropriate precautions
can be taken.
Immediately notify your supervisor and infection control nurse
Any known case of tuberculosis in a patient or employee must be reported to the Infection
Control Nurse for appropriate reporting to local and state health departments.
The examining room used as a holding area should be closed and terminally cleaned after the
patient has left and then disinfected with an institutionally approved disinfectant.
Wear a respirator for close or prolonged contact
When in close contact with a suspected active TB case, wear a NIOSH certified N-95 mask or a
HEPA respirator. The employee must be fit tested before using N-95 or HEPA respirator, before
wearing a respirator, personnel must be evaluated by Employee Health (432-0071) at the Yale
Health (55 Lock Street) and must contact Yale Environmental Health and Safety (785- 3550) at
135 College Street for training regarding respirator selection, fit testing, and use.
Evaluation of Health Care Workers Post Exposure to Active TB Cases
Health care workers who have been exposed to active TB cases are recommended to have an
initial baseline TB test at time of exposure and a follow up test at 3 months post-exposure.
25
Health care workers with PPD or blood test conversion from negative to positive post-exposure
will be advised to have a chest x-ray and referred for appropriate prophylactic therapy.
Continuing Risk Assessment at Yale University
TB test conversion rates among employees as well as active TB cases among patients will be
reviewed annually by Employee Health and Infection Control Staff for the purpose of risk
assessment. Any evidence of TB test conversion clusters or patient to patient transmission of
TB will be the impetus for further investigation to maintain compliance with TB control
guidelines. Yale Environmental Health and Safety will be responsible to provide training and fit
testing (respiratory protection) to employees who may be at risk of occupational exposure to TB.
The Yale Health –Dept. of Employee Health will provide the medical surveillance of employees
at risk of occupational exposure to tuberculosis for screening and post-exposure follow-up.
The facility Infection Control Committee will coordinate risk assessment and compliance.
Human Resources will notify OEHS & UHS of potential occupationally exposed newly hired
employee.
1.7
Guidelines for Vancomycin Resistant Enterococcus (VRE) and Multi Resistant
Staphylococcal Aureus (MRSA) Management
The source patient colonized or infected with VRE should immediately be placed on Contact
Precautions in a private room (or in the same room as another VRE infected patient).
Contact Precautions for VRE require that gloves be worn when entering the room; gowns
should also be worn if substantial contact with the patient or environmental surfaces (including
furniture, bed rails, etc.) is anticipated or if the patient is incontinent.
Hands should be washed with antimicrobial soap containing chlorhexidine (i.e., Hibiclens)
after removal of gloves and gowns.
Non-critical patient care items such as stethoscopes, thermometers or sphygmomanometers
should be dedicated for the exclusive use of the patient on Contact Precautions.
Items (i.e., wheel chairs, stretchers,) that cannot be specially dedicated to the source patient
should be first cleaned and then disinfected with an institutionally-approved disinfectant after
each use.
Patient(s) on Contact Precautions who need to be transported outside of the ICF but within the
building should be accompanied by a staff member who can inform the receiving department
of the Contact Precautions. Any contaminated surfaces in the receiving department should be
disinfected as above) after use by the affected patient(s).
The charge nurse should insure that any outside facility or agency (including ambulance) is
notified of Contact Precautions prior to receiving the patient.
The Infection Control Nurse may order follow up stool cultures on the source patient for VRE
to determine when Contact Precautions may be discontinued. The guidelines for
discontinuation of Contact Precautions pertaining to VRE are 3 sequential negative specimens
from multiple body sites taken at least one week apart.
Contact Precautions may not be discontinued until it has been discussed with and approved by
the Infection Control Nurse or their designee.
If any evidence of transmission of VRE to other patients is detected, such as finding a positive
culture in the roommate of the source patient, the Infection Control Nurse will do further
investigation in collaboration with the ICF staff.
The Infection Control Nurse with the primary providers’ assistance may order a stool culture
(or rectal swab) for VRE on the roommate of a patient who has been newly found to have VRE.
Additional screening of patients on the unit may be performed at the discretion of the Infection
Control Nurse.

26
After discharge of a patient with VRE, housekeeping should be instructed to clean and
disinfect all environmental surfaces in the room (including phones, doorknobs etc.) using the
institutionally-approved disinfectant. It is the responsibility of the ICF charge nurse to ensure
that this step is completed and that the Infection Control Nurse is notified. The Infection Control
Nurse may elect to perform routine environmental surveillance cultures at his or her discretion.
1.8
Infection Control MRSA Program
1.
Clinical Staff
a.
CDC handouts on MRSA to clinical staff to increase education and awareness
b.
Health care worker education done at safety fair
c.
Work with pharmacy to look at programs to foster and monitor
appropriate use of antimicrobials
d.
Include history of MRSA infection or current colonization on electronic medical record
problem list
e.
Suspect MRSA infection when clinical picture is consistent, culture any open, draining or
suspect wounds to look for MRSA as well as other bacterial pathogens.
f.
Focus on communication - inform all transferring or receiving agencies or facilities of
patient’s MRSA status
2.
Transmission precautions
Contact precautions are recommended for treatment of patients with MRSA infections. This
includes:
Inpatient
•
Private room (if not available may have patients with same MRSA
infection housed in the same room)
•
Glove use when entering room
•
Change gloves after contact with material that might have high concentration of
organisms
•
Remove gloves before leaving room and wash with antimicrobial soap
•
Gowns should be worn if substantial contact with patient or environmental
surfaces is expected and removed prior to leaving the room.
•
Patients should remain in their private rooms and should only be transported
when absolutely necessary, minimizing contact between patient and
environmental surfaces. Patients should be escorted by a staff member for all
transportation within the facility.
•
Non-critical patient care items should only be used for that patient. If sharing of
equipment is necessary, the equipment must be cleaned and disinfected before
using it on another patient.
•
Masks should be used for any splash generating procedures.
Ambulatory
•
Standard precautions are used for patients infected or colonized with MRSA.
•
Gloves and gowns must be used for contact with any secretions or drainage.

27
Environmental Measures:
Inpatient
•
Clean and disinfect surfaces and equipment that may be contaminated, especially
those that are close to the patient such as bed rails, over the bed tables and other
frequently touched surfaces such as door knobs, bed pans, bathrooms on a more
frequent schedule than routine cleaning
•
Upon discharge of patient, terminally clean the room with special focus on
frequently touched areas.
Ambulatory
•
Clean exam tables after use by patient with open wound or drainage as well as
any other environmental surfaces in exam room where patient may have had
contact between surfaces and wound
3.
Tracking
Laboratory reports will be analyzed to track the incidence of MRSA in our facility.
Categories to be tracked will be: total number of infections (this will separated by patient to
avoid duplication of reporting), antibiotic susceptibility data for MRSA infections, and site
information for MRSA infections. If analysis shows a significant upward trend in the
incidence of new MRSA infections or if there is any evidence of a health care associated
infection or outbreak, prevention efforts will be intensified (see below)
4.
Prevention of transmission
a.
Follow CDC hand hygiene recommendations, stress hand washing in all clinical areas
b.
Patient education programs - Educational posters in residential and athletic areas,
education directed at patients who are infected or colonized prior to discharge.
5.
Intensified Prevention Efforts in setting of increased transmission
Intensify efforts if any evidence of increased transmission or health care associated
outbreaks, including one or more of the measures below in addition to those previously
outlined:
•
Consider obtaining active surveillance cultures from at risk inpatient populations, obtain
cultures on roommates of patients subsequently diagnosed with MRSA, and obtain cultures
on patients previously infected or colonized with MRSA. Cultures should be obtained from
areas of skin breakdown or draining wounds, plus anterior nares. Continue surveillance
on a weekly basis until transmission ceases or frequency decreases.
•
If surveillance data points to a health care worker as a possible ongoing source of
transmission, consider obtaining health care worker cultures or consultation with an expert
in Infectious Disease.
•
Consider assignment of dedicated nursing and ancillary staff, including environmental staff
to infected patients. Use either disposable or patient dedicated equipment for the infected
patients.
•
Intensify training and monitoring of the use of contact precautions and on the proper use of
environmental measures.
28
•
Obtain environmental cultures of equipment or other surfaces if evidence points to an
environmental source of ongoing transmission.
•
Consider consultation with an expert in Infectious Disease or Epidemiology for further
recommendations and discussion of decolonization options for patients or staff.
29
SECTION 2: Medical Surveillance
2.1
Recommended Immunizations for Health Care Workers
Adopted from AJIC Vol. 26 No 3June 1998 CDC Personnel Health Guideline: Guideline for Infection
Control in Health Care Personnel and current CDC Adult Immunization Guidelines:
All health care workers should be immunized against the following diseases that may be encountered in
their workplace: hepatitis B, measles, mumps, rubella, and diphtheria-tetanus. In addition, non-immune
workers should be vaccinated against Varicella-zoster. Health care workers should also receive the
influenza vaccine on a yearly basis to prevent transmission of the disease to their high-risk patients. Table
1 outlines the recommended vaccinations along with their indications and contraindications. There are
some additional vaccinations listed in the table which may be indicated in certain situations for health care
workers, but which are not routinely recommended. Health Care workers are also recommended to receive
one adult tetanus-diphtheria-pertussis booster as an adult and repeat diphtheria-tetanus boosters as
recommended by CDC.

30
Table 1. Immunobiologics and schedules for health care personnel: Immunizing agents strongly recommended for health care personnel
Generic name
Primary booster
Dose schedule
Indications
Major precautions
and contraindications
Special considerations
Hepatitis B-
recombinant vaccine
Two doses IM in the
deltoid muscle 4 wk
apart; 3rd dose 5 mo.
after 2nd; booster
doses not necessary if
titer is positive
Health care personnel at risk of
exposure to blood and body fluids
No apparent adverse effects to
developing fetuses, not
contraindicated in pregnancy;
history of anaphylactic reaction to
common bakers yeast
No therapeutic or adverse effects on HBV-
infected persons; cost-effectiveness of
prevaccination screening for susceptibility
to HBV depends on costs of vaccination and
antibody testing and prevalence of immunity
in the group of potential vaccines;
health care personnel who have ongoing
contact with patients or blood should be
tested 1-2 mo. after completing the
vaccination series to determine serologic
response
Influenza vaccine
(inactivated whole or
split virus)
Annual single-dose
vaccination IM with
current (either whole-
or split-virus) vaccine
All health care workers
History of anaphylactic
hypersensitivity after egg ingestion
No evidence of maternal or fetal risk when
vaccine was given to pregnant women with
underlying conditions that render them at
high risk for serious influenza
complications.
Measles live-virus
vaccine
One dose SC; 2
nd
dose
at least 1 mo. later
All health care workers must have
either two doses of live vaccine on or
after their 1st birthday, (b) physician-
diagnosed measles, or (c) laboratory
evidence of immunity.
Pregnancy; immunocompromised*
state; (including HIV-infected
persons with severe
immunosuppression) history of
anaphylactic reactions after gelatin
ingestion or receipt of neomycin; or
recent receipt of immune globulin
MMR is the vaccine of choice if recipients
are also likely to be susceptible to rubella
and/or mumps; persons vaccinated between
1963 and 1967 with (a) a killed measles
vaccine alone, (b) killed vaccine followed
by live vaccine, or (c) a vaccine of unknown
type should be revaccinated with two doses
of live measles vaccine
Mumps live- virus
vaccine
Two dose of live
mumps virus vaccine
Susceptible health care workers should
receive 2 doses of live mumps vaccine
unless they have laboratory evidence of
immunity, or physician diagnosed
mumps.
Pregnancy; immunocompromised*
state; history of anaphylactic
reaction after gelatin ingestion or
receipt of neomycin
MMR is the vaccine of choice if recipients
are also likely to be susceptible to measles
and rubella
HDCV, Human diploid cell rabies vaccine; rabies vaccine absorbed; IPV, inactivated poliovirus vaccine; OPV, oral poliovirus vaccine; ID, intradermally. *Persons immunocompromised because of
immune deficiencies, HIV infection, leukemia, lymphoma, generalized malignancy, or immunosuppressive therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation.

31
Table 1. Continued
Generic name
Primary booster
Dose schedule
Indications
Major precautions
and contraindications
Special considerations
Rubella live- virus
vaccine
One dose SC; no
booster
Health care personnel, both male and
female, who lack documentation of
receipt of live vaccine on or after their
1
st
birthday, or of laboratory evidence
of immunity.
Pregnancy; immunocompromised*
state; history of anaphylactic
reaction after receipt of neomycin
Women pregnant when vaccinated or who
become pregnant within 3 mo. of
vaccination should be counseled on the
theoretic risks to the fetus, the risk of
rubella vaccine-associated malformations in
these women is negligible; MMR is the
vaccine of choice if recipients are also
likely to be susceptible to measles or
mumps
Varicella-zoster live-
virus vaccine
Two 0.5 ml doses SC
4-8 wk apart if 13 yr.
Health care personnel without
laboratory evidence of Varicella
immunity or evidence of previous
vaccination.
Pregnancy, immunocompromised*
state, history of anaphylactic
reaction after receipt of neomycin or
gelatin; salicylate use should be
avoided for 6 wk after vaccination
Because 71%-93% of persons without a
history of varicella are immune, serologic
testing before vaccination may be cost-
effective
Hepatitis A Vaccine
Two doses of vaccine
IM, either
(HAVRIX
TM
) 6-12
mo. apart or
(VAQTA
TM
) 6 mo.
apart
Not routinely indicated for U.S. health
care personnel; however, persons who
work with HAV-infected primates or
with HAV in a laboratory setting
should be vaccinated
History of anaphylactic reaction to
alum or the preservative 2-phenoxy-
ethanol; vaccine safety in pregnant
women has not been evaluated, risk
to fetus is likely low and should be
weighed against the risk of hepatitis
A in women at high risk
Health care personnel who travel
internationally to endemic areas should be
evaluated for vaccination
HDCV, Human diploid cell rabies vaccine; rabies vaccine absorbed; IPV, inactivated poliovirus vaccine; OPV, oral poliovirus vaccine; ID, intradermally. *Persons immunocompromised because of
immune deficiencies, HIV infection, leukemia, lymphoma, generalized malignancy, or immunosuppressive therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation.

32
Table 1. Continued
Generic name
Primary booster
Dose schedule
Indications
Major precautions
and contraindications
Special considerations
Meningo-coccal
One dose in volume
Not routinely indicated for health care
Vaccine safety in pregnant women
May be useful in certain outbreak
(MCV4 or MPSV)
and by route specified
workers in the United States except to
has not been evaluated; vaccine
situations
by manufacturer; need
microbiologists who are routinely
should not be given during
for boosters is
exposed to isolates
pregnancy unless risk of infection is
unknown
high.
Polio vaccine
IPV, two doses SC
given 4-8 wk apart
followed by 3rd dose
6-12 mo. after
Health care personnel in close contact
with persons who may be excreting
wild virus and laboratory personnel
handling specimens that may contain
wild poliovirus
History of anaphylactic reaction
after receipt of streptomycin or
neomycin; because safety of vaccine
has not been evaluated in pregnant
women, it should not be given
during pregnancy
Use only IPV for immunosuppressed
persons or personnel who care for
immunosuppressed patients.
Tetanus and
Two doses IM 4 wk
All adults; tetanus prophylaxis in
First trimester of pregnancy; history
Diphtheria
apart; 3
rd
dose 6-12
wound management
of a neurologic reaction or
(Td)
mo. after 2nd dose;
immediate hypersensitivity reaction;
booster every 10 yr.
individuals with severe local
(Arthus-type) reaction after
previous dose of Td vaccine should
not be given further routine or
emergency doses of Td for 10 yr.
*The term immunocompromised includes persons who are immunocompromised from immune deficiency diseases, HIV infection, leukemia, lymphoma, or generalized malignancy, or
immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation.

33
Table 1. Continued
Generic name
Primary booster
Dose schedule
Indications
Major precautions
And contraindications
Special considerations
Tetanus-diphtheria
acellular pertussis
One dose as an adult
Adults should have one dose in place of
regular diphtheria-tetanus booster at
greater than or equal to 10 years after
last Td booster. Adults who have
contact with children under 12 months
old and health care workers are
recommended to get one Tdap if more
than 2 years have passed since last
tetanus booster.
Anyone with unstable neurological
condition should defer, see other
precautions under Adult diphtheria-
tetanus
Typhoid vaccines:
oral
Four oral doses on
alternate days;
(Ty21a) vaccine
manufacturer’s
recommendation is
revaccination with the
entire four-dose series
every 5 yr.
Personnel in laboratories who
frequently work with Salmonella typhi
History of severe local or systemic
reaction to a previous dose of
typhoid vaccine; Ty2la vaccine
should not be given to
immunocompromised* personnel or
those currently taking antibiotocs
Vaccination should not be considered
as an alternative to the use of proper
procedures when handling specimens
and cultures in the laboratory
Typhoid vaccines:
Inactivated
one injection with
booster needed every 2
years
Vaccinia vaccine
One dose administered
with a bifurcated
needle; boosters every
10 yr.
Personnel who directly handle cultures
of or animals contaminated with
recombinant Vaccinia viruses or
orthopox viruses (monkeypox, cowpox,
Vaccinia, etc.) that infect human beings
Pregnancy, presence or history of
eczema, or immunocompromised’
status in potential vaccines or in
their household contacts
Vaccination may be considered for
health care personnel who have direct
contact with contaminated dressings or
other infectious material from
volunteers in clinical studies involving
recombinant Vaccinia virus
*The term immunocompromised includes persons who are immunocompromised from immune deficiency diseases, HIV infection, leukemia, lymphoma, or generalized malignancy, or
immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation.
2.2
Tuberculosis Testing
Employees and students at risk should be tested for TB exposure by a tuberculin skin test (PPD) or
a QuantiFERON serum test on an annual basis. New employees will be referred to the Employee
Health Department upon being hired for baseline PPD testing. A 2-step PPD will be done on
employees who are at higher risk for previous TB infection as defined by the CDC and who do not
have a history of a previous negative PPD within the last 2 years. Employees with a history of a
previous positive PPD test will not be retested but should provide documentation of a negative
chest x-ray as part of their evaluation for the positive PPD. Employees exempt from the tuberculin
skin test must be informed about symptoms of TB and the need for immediate evaluation of any
pulmonary symptoms suggestive of TB by a primary or trained health care provider to determine if
symptoms of TB disease have developed.
All University employees and students in contact with patients or clients in hospitals, clinics or long
term facilities must be tested for TB exposure by a tuberculin skin test (PPD) or QuantiFERON
serum on an annual basis. This includes students who deliver care conduct research or consult
individuals. In addition, any student who volunteers in correctional facilities, hospices, shelters for
the homeless or drug/alcohol treatment facilities should be retested on an annual basis.
Employees and students who test positive on PPD testing will be referred for a chest x-ray and will
be evaluated for any signs of active TB infection. If no signs of active infection (such as fatigue,
fever, chills, night sweats, loss of appetite, weight loss, sputum production, coughing up blood —
hemoptysis. chest pain, hoarse voice) are present the employees will be referred for prophylactic
treatment when appropriate following established CDC recommendations.
If an employee is exposed to someone with active TB through their job, they should contact the
Employee Health Department at 432-7978 at Yale Health to arrange for a tuberculosis skin test
now and again at 3 months. If the employee’s skin test remains negative, they can return for annual
skin testing if they are in a job category which has potential exposure. If the skin test shows
evidence of recent infection, they will be referred for a Chest X-ray and a discussion of appropriate
treatment or prophylaxis.
2.3
Communicable Disease Work Restrictions for Health Care Workers
Adopted from the AJIC Vol. 26 No 3June 1998 CDC Personnel Health Guideline: Guideline for Infection Control in Health Care
Personnel
Table 2 summarizes the suggested work restrictions for health care workers who are infected with
infectious diseases of importance in health care settings. In some cases, state and local regulations
may regulate the restrictions in a given area. Employees who are suffering from any of these listed
infections should report it to their supervisor, who should then report it to the infection control
coordinator and the Department of Employee Health for further guidance or advice on the
restrictions and return to duty.
34

35
Table 2. Summary of suggested work restrictions for health care personnel exposed to or infected with infectious diseases of importance in health
care setting (modified from ACIP recommendations).
Disease/Problem
Work Restriction
Duration
Conjunctivitis
Restrict from patient contact and contact with
the patient’s environment
Until discharge ceases
Cytomegalovirus infections
No restriction
Diarrheal diseases
Acute stage (diarrhea with other symptoms)
Convalescent stage, Salmonella spp.
Norovirus – restrict from work while
symptomatic and until 48-72 hours after
resolution
Restrict from patient contact, contact with the
patient’s environment, or food handling
Restrict from care of high-risk patients
Until symptoms resolve
Until symptoms resolve; consult with local and
state health authorities regarding need for
negative stool cultures
Diphtheria
Exclude from duty
Until antimicrobial therapy completed and 2
cultures obtained 24 hours apart are negative
Enterovial infections
Restrict from care of infants, neonates, and
immunocompromised patients and their
environments
Until symptoms resolve
Hepatitis A
Restrict from patient contact, contact with
patient'’ environment, and food handling
Until 7 days after onset of jaundice
Hepatitis B
Personnel with chronic hepatitis B surface
antigemia who do not perform exposure
prone procedures
Personnel with acute or chronic hepatitis B e
antigenemia who perform exposure-prone
procedures
No restriction; refer to state regulations;
standard precautions should always be
observed
Do not perform exposure-prone invasive
procedures until counsel from an expert review
panel has been sought; panel should review and
recommend procedures the worker can
perform, taking into account specific procedure
as well as skill and technique of worker;
refer to state regulations
Until hepatitis B e antigen is negative
Hepatitis C
No recommendation
†Those susceptible to Varicella and who are at increased risk of complications of Varicella, such as neonates and immunocompromised persons of any age.
‡ High-risk patients as defined by the ACIP for complications of influenza.

36
Table 2 Continued
Disease/Problem
Work Restriction
Duration
Herpes simplex
Genital
Hands (herpetic whitlow)
Oralfacial
No restriction
Restrict from patient contact and contact with
the patient’s environment
Evaluate for need to restrict from care of high-
risk patients
Until lesions heal
Human immunodeficiency virus
Do not perform exposure-prone invasive
procedures until counsel from an expert review
panel has been sought; panel should review and
recommend procedures the worker can
perform, taking into account specific
procedures as well as skill and technique of the
worker; standard precautions should always be
observed; refer to state regulations
Measles
Active
Postexposure (susceptible personnel)
Exclude from duty
Exclude from duty
Until 7 days after the rash appears
From 5
th
day after 1
st
exposure through 21
st
day
after last exposure and/or 7 days after rash
appears
Meningococcal infections
Exclude from duty
Until 24 hours after start of effective therapy
Mumps
Active
Postexposure (susceptible personnel)
Exclude from duty
Exclude from duty
Until 9 days after onset of parotitis
From 12
th
day after 1
st
exposure through 26
th
day after last exposure or until 9 days after
onset of parotitis
Pediculosis
Restrict from patient contact
Until treated and observed to be free of adult
and immature lice

37
Table 2 Continued Revised: 10/29/01
Disease/Problem
Work Restriction
Duration
Pertussis
Active
Postexposure (asymptomatic personnel)
Postexposure (symptomatic personnel)
Exclude from duty
No restriction, prophylaxis recommended
Exclude from duty
From beginning of catarrhal (inflammation of
mucous membranes) stage through 3
rd
wk after
onset of paroxysms or until 5 days after start of
effective antimicrobial therapy
Until 5 days after start of effective
antimicrobial therapy
Rubella
Active
Postexposure (susceptible personnel)
Exclude from duty
Exclude from duty
Until 5 days after rash appears
From 7
th
day after 1
st
exposure through 21
st
day
after last exposure
Scabies
Restrict from patient contact
Until cleared by medical evaluation
Staphylococcus aureus infection
Active, draining skin lesions
Carrier state
Restrict from contact with patients and
patient’s environment or food handling
No restriction, unless personnel are
epidemiologically linked to transmission of the
organism
Until lesions have resolved
Streptococcal infection,
Group A
Restrict from patient care, contact with
patient’s environment, or food handling
Until 24 hours after adequate treatment started
Tuberculosis
Active disease
PPD converter
Exclude from duty
No restriction
Until proved noninfectious
Varicella
Active
Postexpsoure (susceptible personnel)
Exclude from duty
Exclude from duty
Until all lesions dry and crust
From 10
th
day after 1
st
exposure through 21
st
day (28
th
day if VariZIG given) after last
exposure

38
Table 2 Continued
Disease/Problem
Work Restriction
Duration
Zoster
Localized, in healthy person
Generalized or localized in
immunosuppressed person
Postexposure (susceptible personnel)
Cover lesions; restrict from care of high-risk
patients†
Restrict from patient contact
Restrict from patient contact
Until all lesions dry and crust
Until all lesions dry and crust
From 8
th
day after 1
st
exposure through 21
st
day
(28
th
day if VariZIG given) after last exposure
or, if Varicella occurs, until all lesions dry and
crust
Viral respiratory infections, acute febrile
Consider excluding from the care of high risk
patients‡ or contact with their environment
during community outbreak of RSV and
influenza
Until acute symptoms resolve
*Unless epidemiologically linked to transmission of infection
†Those susceptible to Varicella and who are at increased risk of complications of Varicella, such as neonates and immunocompromised persons of any age.
‡ High-risk patients as defined by the ACIP for complications of influenza.

2.4
Guidelines for Pregnant Health care Personnel
Adopt from AJIC Vol. 26 No 3June 1998 CDC Personnel Health Guideline: Guideline for Infection Control in Health Care Personnel
Pregnant health care workers are at no greater risk than other personnel for acquiring an infectious
disease as a result of caring for patients. However, since some infections can pose a risk
to the fetus due to perinatal transmission, pregnant workers should adhere to Standard and
Transmission Based Precautions regardless of their individual immune status with respect to
certain diseases. Pregnant workers should also be aware of their own immune status with respect
to communicable diseases and be up–to-date on vaccinations that are available for these diseases.
Table 3. Pregnant health care personnel: Pertinent facts to guide management of
occupational exposures to infectious agents
Agent
Potential Effect
on Fetus
Rate of
Perinatal
Transmission
Maternal
Screening
Prevention
1. Cytomegalo-
virus
Hearing loss;
congenital
syndrome*
15% after
primary maternal
infection;
symptomatic 5%
Antibody provides
some but not
complete protection
against clinical
disease; routine
screening not
recommended
Standard precautions
2. Hepatitis B
Hepatitis;
development of
chronic
infection in
infant
HBeAg
seropositive 90%;
HBeAg negative
0-25%
HBsAg routine
screening
recommended
Vaccine and HBIG to
infant; standard
precautions
3. Hepatitis C
Hepatitis
2% - 5%
Anti-HCV; HCV
RNA in reference
labs; routine
screening not
recommended
Standard precautions
4. Herpes
simplex
Mucocutaneous
lesions, sepsis,
encephalitis;
congenital
malformations
(rare)
Unlikely from
nosocomial
exposure;
primary 33%-
50%, recurrent
4%
Antibody testing
not useful;
inspection for
lesions at delivery
Standard precautions
5. Human
immunodefici-
ency virus
(HIV)
AIDS by 2-3 yr.
8%-30%
Antibody by
enzyme
immunoassay,
Western blot
Avoid high-risk behaviors;
consider postexposure
prophylaxis after high-risk
needlestick exposure;
intrapartum and postnatal
zidovudine for HIV-
seropositive mothers and
their babies; standard
precautions
6. Influenza
Inconsistent
Rare
None
Vaccine (safe during
pregnancy); droplet
precautions
39

Table 3 Continued
Agent
Potential
Effect on
Fetus
Rate of Perinatal
Transmission
Maternal
Screening
Prevention
7. Measles
Prematurity;
abortion
Rare
History, antibody
Vaccine†; airborne
precautions
8. Parovirus
B19
Hydrops,
stillbirth
Rare, 3% - 9%
maximum adverse
outcome
IgM and IgG
antibody
prepregnancy;
antibody protection
Droplet precautions
9. Rubella
Congenital
syndrome*
45% - 50% overall;
90% in 1
st
12 wk
Antibody
Vaccine†; droplet
precautions for acute
infection; contact
precautions for
congenital rubella
10.
Tuberculosis
Hepatomegaly
, pulmonary,
CNS
Rare
Skin test
Isoniazid ethambutol
for disease; airborne
precautions
11. Varicella-
zoster
Malformations
(skin, limb,
CNS, eye);
chickenpox
Total 25%;
congenital
syndrome (0-4%)
Antibody
Vaccine†; VariZIG
within 10 days of
exposure if
susceptible; airborne
and contact
precautions
Modified from Siegel JD. Risk and exposure for the pregnant health-care worker. In: Olmatead RN, editor. APIC
infection control and applied epidemiology; principles and practices. St Louis: Mosby; 1996. p. 22-2-22-3 (table
22-1). HBeAg, Hepatitis Be antigen; CNS, central nervous system.
*Congenital syndrome: varying combinations of jaundice, hapatospienomegaly, microcephaly, ONS
abnormalities, thrombocytopenia, anemia, retinopathy, and skin and bone lesions.
†Live-virus vaccines are given routinely before pregnancy.
2.5
Emergency Procedures for Exposure to Blood and Body Fluids
Employees exposed to blood or body fluids by a needlestick, cut, bite, or splash to a mucous
membrane or non-intact skin should immediately wash the affected area with soap and water
for 15 minutes. If the splash is to the eyes or mucous membrane, the area should be flushed
with water for 15 minutes.
Employees should immediately report the exposure incident to their supervisor and seek
medical attention.
Employees or students should immediately report for medical care at Yale Health Plan
(Employee Health Office 432-7978, Student Medicine 432-0312 or Acute Care 432-0123).
It is important to begin any recommended treatment within 1 to 2 hours after exposure.
If the exposure occurs at the Yale-New Haven Hospital and the employee wishes to be seen on
site, they should report to Personnel Health Service (7:30 A.M. to 4:30 P.M., Monday through
Friday) or the Yale-New Haven Hospital Emergency Room if the episode occurs outside of
regular daytime working hours.
40
41
2.5.1 Needlestick Procedures
The exposed employee/student should immediately be tested for baseline HIV, Hepatitis B
Surface Ab, and Hepatitis C Ab following established testing guidelines.
The exposed person will be counseled regarding the risk of seroconversion for HIV; symptoms
of disease (acute retroviral syndrome), precautions to prevent secondary spread, and possible
indication for antiviral prophylaxis. See needlestick PnP for current prophylaxis
recommendations (Appendix B)
Workers who receive antiviral prophylaxis should also have baseline CBC and renal and
hepatic function tests drawn.
The suspected source patient for the exposure should be immediately approached to give
consent for a baseline HIV, Hepatitis B S Ag, Hepatitis B S Ab, Hepatitis B core Ab, and
Hepatitis C Ab. The attending primary care provider for the source patient should be notified
to obtain this testing. The Yale Health Plan or Personnel Health providers can assist with this
process. If the source patient does not give consent for testing, the institution’s needlestick
committee should convene as soon as possible to take the necessary steps to obtain testing.
If antiviral prophylaxis for HIV is indicated, the employee/student will be given a 96-hour
packet of prophylactic medication that is available at each institution.
The exposed person will then be instructed to follow up with the appropriate department (either
Employee Health at 432-7978 or Student Medicine at 432-0312) on the next business day to
receive further instructions.
Anyone receiving antiviral prophylaxis should be reevaluated at 2 weeks and 4 weeks post-
exposure for CBC, LFT’s, and renal function to check for any symptoms of drug toxicity that
might indicate the need for reduction of dosage or change in medication. Expert consultation
with an infectious disease specialist should be obtained for situations that might require a
change in the protocol.
Exposed person should be retested for HIV antibody at 6 weeks, 12 weeks and 6 months post-
exposure. Testing may be extended for a year if recommended by the medical provider on a
case-by-case basis.
Appropriate prophylaxis for Hepatitis B exposure should be included in all evaluations where
indicated. If the source patient has evidence of HepC infection, the employee should have
follow up testing for HepC including a HepC viral RNA at 4 weeks and HepC Ab at 3 and 6
months.
If the source patient’s HIV status subsequently becomes known, the decision about antiviral
prophylaxis can be modified as clinically indicated.
Those exposed to blood or bodily fluids should make sure an incident report is filed within 24
hours; employees should also make sure a Supervisor’s Report of Injury is filed.
See appendix for information concerning HIV Counseling Guidelines and Risk Categories.
42
2.6 Post Exposure Prophylaxis guidelines for exposure to other infectious agents
Adopt from AJIC Vol. 26 No 3June 1998 CDC Personnel Health Guideline: Guideline for Infection Control in Health Care Personnel
The following table outlines prophylactic regimens that may be prescribed in situations where a
health care worker is exposed to an infectious agent or communicable disease. Health care workers
who are exposed to any of these infections through their work should notify their supervisor, who
will then refer them to the Department of Employee Health for evaluation and discussion of
prophylaxis.

43
Table 4. Immunobiologics and schedules for health care personnel: Diseases for which postexposure prophylaxis may be indicated for
health care personnel
Disease
Prophylaxis
Indications
Major precautions
contraindications
and
Special
considerations
Diphtheria
Benzathine penicillin, 1.2 mU IM, single
For health care personnel exposed
Also administer one
dose, or erythromycin (1 gm/day) PO x 7
to diphtheria or identified as
dose Td to previously
days
carriers
immunized if no Td
has been given in 5
yr.
Hepatitis A
Begin Hepatitis A vaccination serioes for
persons 1-40 years old (If < 1 year or >
40 years old, can use IgG 0.02mg/kg
within 2 weeks)
May be indicated for health care
personnel exposed to feces of
infected persons during outbreaks
Hepatitis B
HBIG 0.06 ml/kg IM as soon as possible
(and within 7 days) after exposure (with
dose 1of hepatitis B vaccine given at
different body site); complete doses #2
and #3 of HepB series
HBV-susceptible health care
personnel with percutaneous or
mucous-membrane exposure to
blood known to be HBsAg
seropositive
Meningococc
al disease
Rifampin, 600 mg PO every 12 hours for
2 days, or ceftriaxone, 250 mg IM, single
dose, or ciprofloxacin, 500 mg PO, single
dose
Personnel with direct contact with
respiratory secretions from infected
persons without the use of proper
precautions (e.g., mouth-to-mouth
resuscitation, endotracheal
intubation, endotracheal tube
management, or close examination
of oropharynx
Rifampin and ciprofloxacin
not recommended during
pregnancy
Pertussis
Azithromycin, 500mg x1, then 250mg
x 4 days
Erythromycin, 500 mg qid PO, or
trimetho-prim-sulfamethoxazole, 1 tablet
bid PO, for 14 days after exposure
Personnel with direct contact with
respiratory secretions or large
aerosol droplets from respiratory
tract of infected persons.
PO, Orally; Td, tetanus-diphtheria toxoid; IG, immune globulin; IgA, immunoglobulin A; qid, four times daily; bid, twice daily; HRIG, human rabies immunoglobulin; HDCV, human diploid cell rabies
vaccine; RVA, rabies vaccine absorbed.
*Persons immunocompromised because of immune deficiencies, HIV infection, leukemia, generalized malignanacy, or immunosuppressive therapy with corticosteroids, alkylating drugs, antimetabolites, or
radiation.
†Some persons have recommended 125 U/10 kg regardless of total body weight.
Table 4. Continued

44
Disease
Prophylaxis
Indications
Major
precautions
contraindications
and
Special considerations
Rabies
For those never vaccinated: HRIG 20
Personnel who have been bitten by
human being or animal with rabies or
have had scratches, abrasions, open
wounds, or mucous membranes
contaminated with saliva or other
potentially infective material (e.g.,
brain tissue)
Personnel who have
IU/kg, half infiltrated around wound, and
previously been
HDCV or RVA vaccine, 1.0 ml, IM
vaccinated, give HDCV
(deltoid area), 1 each on days 0, 3, 7, 14.
or RVA vaccine, 1.0
ml, IM, on days 0 and
3; no HRIG is
necessary
Varicella
If within 3-5 days immediate vaccination
Personnel known or likely to be
Serologic testing may
zoster virus
with Varicella vaccine series.
susceptible to Varicella and who have
help in assessing
Alternatively for high risk patients,
close and prolonged exposure to an
whether to administer
VZIG for persons 50 kg: 125 U/10kg
IM; for persons 50 kg: 625 U†
infectious health care worker or
patient, particularly those at high risk
for complications, such as pregnant or
VZIG; if Varicella is
prevented by the use of
VZIG, vaccine should
immunocompromised persons
be offered later
PO, Orally; Td, tetanus-diphtheria toxoid; IG, immune globulin; IgA, immunoglobulin A; qid, tour times daily; bid, twice daily; HRIG, human rabies immunoglobulin; HDCV, human diploid cell rabies vaccine;
RVA, rabies vaccine absorbed, VZIG Varicella Zoster Immune globulin.
*Persons immunocompromised because of immune deficiencies, HIV infection, leukemia, generalized malignanacy, or immunosuppressive therapy with corticosteroids, alkylating drugs, antimetabolites, or
radiation.
†Some persons have recommended 125 U/10 kg regardless of total body weight.

45
SECTION 3: Handling Waste
3.1
Medical Waste Management
The purpose of this section is to provide practical guidelines for employees who handle, manage,
transport and dispose of waste.
There is no epidemiological evidence that clinical waste, when properly disposed, is more infective
to the community than residential waste. However, it does present a greater risk to waste-handlers
until it reaches the final disposal location. Medical waste must always, therefore, be handled
carefully. Infection capability is dependent on:
the presence of a human pathogen
a pathogen with sufficient virulence in sufficient dose to cause disease
the availability of a potential host’s portal of entry
the resistance of the host
The following waste shall be declared as medical waste and shall be subject to the special waste-
handling described below
contaminated sharps
unused, discarded hypodermic needles, suture needles, scalpel blades and syringes
used intravenous equipment
isolation wastes from patients infected with these viruses
Kyasanur Forest Disease
Junin
Marburg
Russian spring-summer encephalitis
Congo-Crimean Hemorrhagic fever
Omsk hemorrhagic fever
Lassa
Machupo
Ebola
cultures and stocks of infectious agents
human blood and blood products
dressings, paper tissues and other disposable items saturated or dripping with blood or items
caked with dried blood
pathological wastes
Medical waste must be collected and transported in leak proof and impervious bags or containers
prior to autoclaving or incineration. Items other than the infective waste described, even if the item
has had contact with blood, exudates or secretions, may be disposed of with all other trash. All trash
must be collected and transported to the collection bin in leak proof, impervious bags. Bulk blood,
suctioned fluids, excretions and secretions must be carefully poured down a drain connected to a
sanitary sewer, and bleach must be poured into the drain before disposing of contaminated fluid and
also after disposing of contaminated fluid.

46
3.2
Guidelines on the Management of Infectious Waste
Medical Waste
Wearing gloves place contaminated dressings, tissues and other articles soiled by respiratory,
oral, blood or wound secretions in a receptacle lined with an impervious plastic bag. Double-
bag in a red plastic bag for disposal.
Place waste in the designated area for Medical waste removal.
Dispose of urine, feces, secretions and excretions into the patient’s toilet or hopper sink.
Do not dispose of wastes in the patient’s sink.
Blood and Blood Products
Wash hands (See section on hand washing).
Follow standard precautions.
Clean up any spillage of blood immediately with a solution of 5.25 sodium hypochlorite
(bleach) and water. Use one part bleach to nine parts water, or another EPA registered
disinfectant.
These recommendations are for the protection of patient care personnel, specimen transporting
personnel, laboratory personnel, and everyone who works in the institution. When handling blood,
employees should be aware the potential exists for the acquisition of Hepatitis B, Hepatitis C, HIV,
Cytomegalovirus (CMV), other viruses and biological agents which are blood borne.
3.3
Trash handling
All material for disposal, except material designated as “infectious,” will be disposed of using
the ordinary trash removal system which terminates with the trash removal from facility and
off-loading at an approved municipal landfill.
Gross liquid content found in various containers to be discarded should be eliminated by the
individual, generating the waste, prior to the introduction of the container into the trash disposal
system.
Containers (e.g., bed pans, emesis basins, urinals, urinal hats, respiratory suction tubing, suction
canister liners & tubing) holding urine, feces, vomitus or nasogastric drainage are discarded in
regular trash after emptying fluids into sanitary sewer system, and rinsing container.
All trash shall be placed in a high tensile strength, impervious, liquid-tight bag prior to being
sent down a trash chute.
3.4
Procedure for Trash Disposal
Use plastic liners in all wastebaskets.
Discard paper and disposable items into the plastic liner in the wastebasket. When full, the
plastic liner should be sealed and disposed of into another larger bag, and not reused.
Do not discard needles and syringes into the wastebasket.
Close bag tightly and secure with tie or tape.

47
3.5
Disposal of chemotherapy waste
The following procedures are recommended for laboratory and clinic personnel for the safe
handling and disposal of chemotherapy drugs and related waste.
Under laws enacted by the federal government, criteria were developed by which wastes could be
determined hazardous. Chemotherapy drugs have been listed as hazardous wastes.
Because of similarity of structure, mode of action, and toxicity all chemotherapy drugs should be
handled and disposed of as hazardous waste. The University Environmental Health and Safety
Department has detailed recommendations for the handling of hazardous waste. These
recommendations can be found on the EHS web site or by contacting the department at 203-785-
3550.These recommendations must be followed since Yale is considered a large generator of
hazardous waste and, as such, is highly regulated by the EPA and Connecticut DEP. The law allows
for civil and criminal penalties to be assessed against institutions and/or individuals that improperly
dispose of hazardous wastes.
Empty syringes, vials, etc. should be placed in the appropriate sharps disposal container. A
container is considered empty if it contains no more than 3 percent by weight of the total
capacity of the container. This definition is important since containers of chemotherapy drugs
do not have to be disposed of as hazardous waste if they meet this definition.
Syringes are always considered biological waste. Any chemotherapy drugs in the syringe
should be emptied into a waste container. The empty syringe is then placed into the appropriate
sharps disposal container.
Waste containers for prepared excess chemotherapy drugs should be kept in each lab, clinic or
office. The container should be compatible with the drug, have a secure lid, and a label
identifying the contents. More than one type of excess drug can be put into each container if a
log sheet is kept on the type of drug and the amount put in. This is important for the final
disposal of this material since unknown material is very expensive to dispose of and these costs
would be charged back to the doctor or department.
Vials that are not empty (>3 percent by weight of the capacity of the container) should be placed
into a plastic lined box. When the box is full, tape the top shut, tag with a hazardous waste tag,
and call Environmental Services Section (5-3551) to arrange for disposal.
Vials containing sterile water should be emptied into the sink and the bottles should be placed
in the appropriate sharps disposal container.
3.6
Needles and Syringes and Other Sharp item
Personnel should use caution when handling all used needles and syringes because it is usually not
known which patient’s blood is contaminated with the hepatitis virus, HIV or other blood borne
diseases. To prevent needle-stick injuries, used needles should not be recapped; bent,
broken, or removed. Place used needle and syringes into an appropriate sharps disposal container
after use. The sharps disposal container used for needles/syringes or other intravascular sharps must
be a rigid puncture-resistant, leak proof on sides and bottom, the container lid opening must be a
one way system to prevent spillage and retrieval of items from container, and appropriately labeled
with the international biohazard symbol and word biohazard
(see figure below).

48
BIOHAZARD
Procedures for Used Needles, Syringes, Knife Blades and other intravascular Sharps -- These
guidelines should be followed by all personnel:
Sharp instruments and disposable items:
Only safety needles should be used unless ICC has approved an exception for a particular
procedure.
Needles must not be recapped, purposely bent or broken by hand, removed from disposable
syringes, or otherwise manipulated by hand.
Needles, syringes and other sharps must have the facility-approved protective safety
mechanism employed immediately after use.
After syringes and needles, scalpel blades and other sharp items are used they must be placed
in appropriate sharps disposal containers for disposal.
Such containers must be easily accessible to personnel needing them and located in all areas
where sharps are commonly used. Sharps containers must be constructed so that they will not
spill their contents and will not themselves allow injuries when handled.
These containers must also be located in patient’s examination or treatment rooms and any
other setting where blood is drawn and needles are used.
Disposal of knife blades:
Safety scalpels with disposable handles must be used unless a department hs been granted and
exception by ICC.
Deposit blade or blade with disposable handle in the sharps container.
Other Sharps
Non-intravascular sharp items ( e.g., glass slides, glass tubes, vacutainers, glass medication
vials, vaccine vials) are deposited into the designated puncture-resistant medical waste
containers.
3.7
Dressings and Tissues
Wound dressings are to be disposed of in a manner so as to “confine and contain” any blood and
body fluid that may be present.
Small dressings can be enclosed in the disposable glove used by the caregiver removing the
dressing. While holding the dressing, the glove should be pulled off inside out over the dressing.
The dressing will be contained in the inverted glove. The dressing and glove can be safely
discarded into the regular trash container located in the patient/clinic room.
Larger dressings should be removed using gloves on both hands. The gloves, dressings and
other trash from the dressing change procedure should be placed directly into an impervious
plastic bag located at the bedside. The bag should be zipped or tied closed and deposited into
the regular trash.

49
Dressings, paper tissues and other disposable items saturated or dripping with blood or items
caked with dried blood must be placed in red biohazard bag and disposed as regulated medical
waste.
Any waste item that is caked, dried, soaked or dripping with blood is deposited into red
biohazard bag, if the item is capable of puncturing the bag then place the item in a puncture
resistant red medical waste container.
Other body fluids (semen, vaginal secretions, cerebrospinal fluids, synovial fluids, pleural fluid,
pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid
that is visibly contaminated with blood, and all body fluids in situations where it is difficult or
impossible to differentiate between body fluids) are empty from container when feasible, by
patient care area staff, by pouring into the sanitary sewer system (soiled utility room or toilet
facility) and deposit containers and/or sealed units in red medical waste container: Containers
that cannot be emptied are stoppered to prevent leakage and placed in red medical waste
container.
3.8
Autoclaves
Autoclaves can sterilize all items that are heat stable (not damaged by steam or high temperature)
or used to decontaminate waste items. In gravity autoclaves, cycles of 250°F (121°C), 15 to 18 lbs.
pressure for one hour may be required for decontamination. In the newer vacuum autoclaves,
decontamination may require 270°F (132°C), 27 to 30 lbs. pressure for 45 minutes. Use chemical
and biological indicators to verify your autoclave technique and sterilization. Contact Yale
Environmental Health and Safety (785-3550) for more information on the Biological Indicator test
kit. Personal protection equipment (PPE) such as rubberized aprons, full-face shields and heat and
liquid resistant gloves must be worn when operating autoclaves.
When autoclaves cannot be used, an alternative method such as chemical decontamination may be
employed. Items must be soaked in a tuberculocidal disinfectant or a 10% bleach (sodium
hypochlorite) solution for at least 30 minutes. Heavily soiled items must be cleaned first.
Whatever the temperature and time requirement for decontamination, the contents of each load
must be positioned so that steam penetrates into, or heated air flows freely among all items to be
decontaminated. Tightly sealed or stoppered materials may not be effectively decontaminated and
may become dangerously pressurized causing injury when removed
A routine autoclave maintenance program is recommended. Regular chemical "tape" monitoring of
temperature and periodic monitoring with a biological indicator should be performed to evaluate
the effectiveness of the autoclave. Place biological indicators at locations inside the load, the area
slowest to heat up, throughout the autoclave are the best indication of sterilization. Biological
indicators may be processed by either in-office biological monitoring (use of an incubator) or mail-
in spore testing (processed by a lab vendor). Autoclaves should be tested periodically. Contact Yale
Environmental Health and Safety for assistance in testing your autoclave.
Items containing chemicals (such as phenol-chloroform) should not be placed in an autoclave or a
hot air oven (remove chemicals first).
Autoclave records should be kept on-hand for at least three years.
Questions should be addressed to Yale Environmental Health and Safety — 785-3550

50
SECTION 4: Good Work Practices
This section contains information essential to understanding and properly using Standard
Precautions. These techniques and recommendations should be applied to all patient care
procedures. For example, gowns are appropriate for patient-care personnel when soiling with bodily
fluids is likely, whether or not the patient is known or suspected to be infected.
4.1
Hand washing
Hand washing is the single most important means of preventing the spread of infection. Personnel
should always wash their hands, even when gloves are used, before and after taking care of any
patient.
YUHS Policy and Procedure is to wash hands before and after each patient contact.
Basic Hand Washing
Start with acceptable antimicrobial liquid hand soap. Turn water on and wet hands
thoroughly.
Vigorously lather with soap, covering well beyond areas of contamination.
Use friction, one hand upon the other with fingers interlaced for at least 15 seconds.
Rinse hands thoroughly under running water, holding elbows higher than hands to allow
water to flow to the fingertips.
Dry hands with a clean, dry paper towel.
Use a paper towel to turn off the water faucet.
4.2
General
Eating, drinking, application of cosmetics or lip balm, and handling of contact lenses is
prohibited in work areas where there is reasonable likelihood of occupational exposure to
blood, body fluids, chemicals, radioactive materials, and all other hazardous materials.
Personal food and drink are prohibited from storage in refrigerators, freezers, cabinets, or on
shelves or countertops in the areas designated for patient care.
Use protective covering on chairs, wheelchairs, stools, and exam tables that have direct
contact with patient’s skin.
Cover stretchers and exam/treatment tables with a clean sheet and/or disposable exam table
paper before each patient use. Wipe the surface with an institutionally-approved disinfectant
(such as, tuberculocidal disinfectant or a 10% bleach solution) daily and when visibly soiled
with blood or body fluids.
Clean non-patient specific portable equipment (blood pressure cuffs) with an approved
disinfectant-detergent in accordance with the manufacturer's instructions when visibly soiled
and according to the equipment cleaning policy.
Place contaminated reusable instruments in designated containers before removal to another
area for cleaning.
Family/visitors of Inpatient Care patients will be advised to check with the patient’s nurse
before bringing gifts of food or drink, as some patients are on special diets.

51
Due to infection control considerations, plants and flowers are not allowed in patient care
areas or in clean and dirty utility rooms.
Dispose of sharps in the designated sharps container. Contaminated needles must not be bent,
recapped, broken, or removed by hand from the syringe. Always engage the sharp safety
mechanism before disposal immediately after use.
Check all sterile supplies weekly for inventory rotation. Supply delivery will follow first in
first out procedure.
Prepare fresh solutions of disinfectant according to manufacturer’s instructions. Place a date on
the container as to when the solution was prepared. If using bleach solution, (10% in water) it
must be prepared daily.
Minimize splashing, spraying, or generation of droplets during procedures involving blood or
other potentially infectious materials.
Keep goggles, gowns, and gloves available and easily accessible in all exam rooms and other
direct patient care areas.
Label and date all patient food items.
Do not store clean supplies on the floor, in the soiled utility room, or next to sinks where
splashing of water or soiling may occur. Designate and maintain areas for clean and dirty
supplies.
Medical supplies must not be stored in corrugated boxes.
4.3
Eyewash Station and Spill Clean-Up Supplies
Employees need to know where the emergency eyewash, chemical and biological spill supplies,
and other safety equipment is located. Eyewash stations will be tested according to policy by
clinical personnel to be certain that water flows through it.
4.4
Refrigerators:
There must be separate refrigerators for food, specimens and medications, each with a cleaning
schedule. Signs must be affixed to indicate its designated use. A biohazard label must be affixed to
the outside of refrigerators used to store specimens. Refrigerators must be monitored for
temperature and cleanliness, which includes daily or twice daily temperature checks, weekly and
as needed cleaning, and routine inspection of contents. Laboratory specimens requiring
refrigeration while awaiting transport may not be stored in the same refrigerator as medications,
juices or water stored for the purpose of dispensing with medication.
4.5
Storage of Sterile Solutions:
Upon opening sterile solutions, staff may write the date on the label. All open solutions will be
discarded on the first working day of the month or upon expiration date, whichever is the earliest.
Sterile stock solutions should be checked prior to use for turbidity, leaks, cracks, particle matter,
discoloration, and expiration date.
When pouring from a container of sterile solution, first pour and then discard a small amount.
Unused remaining sterile solutions must be discarded after 24 hours or as per explicit instructions
of the pharmacist.
YUHS Personnel refer to policy Quality Control of Multidose Vials - Appendix # 1

52
4.6
Storage of Disposable Supplies
Single-use disposable type sterile and non-sterile supplies must be inspected upon receipt and again
just prior to use for intact packaging, evidence of water damage or other contamination or
tampering.
Store supplies in a clean, dry, enclosed area (e.g., cupboard, closet) in their original cartons. Never
store clinical supplies under the sink since they may receive moisture damage/contamination during
routine cleaning procedures and from water leakage. Disposable supplies may only be used once
and not reprocessed, re-sterilized, or reused. After use, promptly dispose items in the appropriate
waste container.
4.7
Perishable Food and Juices
Cans of juices or milk must be checked for expiration date and discarded at expiration date. Before
opening a can, wipe the surface with a moistened paper towel to avoid introducing contaminants.
A dedicated refrigerator is required for the storage of patient food and juices, and must be monitored
at least daily for temperature and cleanliness.
4.8
Dietary
No special dishes or other precautions are necessary when visiting, serving or interviewing
patients, except when those patients are on Transmission Based Precautions.
Disposable dishware and trays are not required for any patient except those on Transmission
Based Precautions.
No special precautions are needed when passing or collecting menus (except for those patients
on Transmission Based Precautions), unless the menus are visibly soiled. If soiled, wear gloves
to handle and dispose of the soiled menus. Promptly wash hands.
No special precautions are needed when passing trays or delivering nourishment to patients
(except those on Transmission Based Precautions). For collecting trays, gloves should be worn.
All disposable items should be removed from trays and discarded into the appropriate waste
receptacle in the patient’s room. Only reusable items should be returned to the Food Service.
▪
Because it is unsanitary to mix clean and contaminated materials, bedpans and urinals
must be removed from patient bed tables prior to mealtime. The table will be washed
with facility approved disinfectant.
▪
In order for food trays to be collected by Food Service Personnel, they must be free of
direct patient care items.
▪
Employees in the dish-room must wear gloves, discard them and wash their hands before
working in “clean” food areas.
▪
See specific policies related to dietary services.
4.9
Private Rooms
Private rooms are required for all patients who soil the room with body substances, as well as for
patients who are likely to have an infectious disease transmissible by the airborne route. Few
patients require private rooms, so in choosing roommate combinations, nurses should assess the
risk of transmission between patients. When practicing Standard Precautions, roommate selection
should be based on the likelihood of soiling of articles in the room.

53
4.10
Roommates for Patients on Transmission Based Precautions
If infected or colonized patients are not placed in private rooms, they should be placed with
appropriate roommates. Infected patients should not share a room with a patient who is likely to
become infected or in whom consequences of infection are likely to be severe (e.g.,
immunosuppressed patient).
In general, patients infected by the same microorganism may share a room. Such grouping (or
cohorting) of patients is especially useful during outbreaks when there is a shortage of private
rooms.
4.11
Airborne Precaution Rooms
General Considerations
Any patient requiring airborne precaution rooms will be masked, placed in a private room and if
appropriate be admitted to Inpatient Care isolation rooms or immediately transferred to Yale New
Haven Hospital.
4.12
Cleaning Patient Rooms
1.
Routine Cleaning
Patient rooms and other treatment area must be cleaned and disinfected prior to the introduction of
a new patient. This cleaning and disinfecting must be in compliance with established housekeeping
policies using only approved cleaning and disinfecting agents. Cleaning equipment used in rooms
of patients whose infection requires a private room should be disinfected before being used in other
patient rooms, i.e. dirty water should be discarded, wiping cloths and mop heads should be
laundered. If cleaning cloths and mop heads are contaminated with infective material or blood, they
should be bagged and sent to the laundry.
Environmental surfaces such as walls, floors and other surfaces are not associated with transmission
of infections to patients or health-care workers. Therefore, extraordinary attempts to disinfect or
sterilize these environmental surfaces are not necessary. However, cleaning and removal of soil
should be done routinely.
Cleaning schedules and methods vary according to the department, the type of surface to be cleaned
and the amount and type of soil present. Horizontal surfaces (e.g. bedside tables and hard-surfaced
flooring) in patient-care areas are usually cleaned on a regular basis, when soiling or spills occur,
and when a patient is discharged. Cleaning of walls, blinds and curtains is performed semi-annually
and when they are visibly soiled.
Disinfectant-detergent formulations registered by the Environmental Protection Agency (EPA) can
be used for cleaning environmental surfaces, but the actual physical removal of microorganisms
by scrubbing is probably as important as any antimicrobial effect of the cleaning agent used.
The manufacturer’s instructions for appropriate use should be followed.
2.
Staff Responsibilities in Terminal Cleaning of the Isolation Room or Cubicle
Clean, bag and remove all supplies from the room before Housekeeping arrives to terminally
clean the room.
Empty all non-disposable receptacles such as drainage bottles into the toilet. If the receptacles
are disposable, empty and discard them according to facility’s policy.
Housekeeping will clean other patient care supplies such as reusable equipment according to
facility policy.

54
Discard all opened or unopened disposable items into trash receptacle.
3.
Terminal Cleaning
Although microorganisms may be present on walls, floors and tabletops in rooms used for patients
on isolation precautions, these environmental surfaces, unless visibly contaminated, are rarely
associated with transmission of infections to other patients when such equipment is not
appropriately decontaminated and reprocessed. Therefore, terminal cleaning should primarily be
directed toward those items that have been in direct contact with the patient or in contact with the
patient’s infective material (excretions, secretions, blood or body fluids). The disinfectant-
detergent solution used during terminal cleaning should be facility approved. Terminal cleaning of
rooms (or cubicles) consists of the following:
Housekeeping personnel should use the same precautions to protect themselves during terminal
cleaning that they use if the patient were still in the room.
All disposable items should be discarded. Articles grossly contaminated with infective material
should be bagged and disposed of in accordance with Yale University’s policy on disposal of
infectious wastes.
All equipment not sent for sterilization or discarded should be cleaned according to facility policy.
All surfaces of furniture and mattress covers should be cleaned according to facility policy.
All floors should be mopped with a disinfectant- detergent solution. Routine washing of walls,
blinds and curtains is not indicated; however, these should be washed if they are visibly soiled.
Cubicle curtains should be changed if visibly soiled or according to facility policy.
Airing a room from which a patient has been discharged is not an effective terminal disinfection
procedure and is not necessary.

55
SECTION 5: Personal Protective Equipment
Personal protective equipment (PPE) also known as barrier protection, is used to prevent blood and
other potentially infectious materials from making direct contact with an employee’s clothing or
body. The type and amount of PPE required depends upon the task to be performed and the
anticipated exposure.
5.1
Gloves
Gloves reduce the possibility personnel will become infected with microorganisms that are
infecting patients; gloves reduce the likelihood personnel will transmit their own endogenous
microbial flora to patients; gloves reduce the possibility personnel will become transiently
colonized with microorganisms which can be transmitted to other patients.
When gloves are indicated, disposable single-use gloves (sterile or non-sterile, depending on the
purpose for use) should be worn. Use sterile gloves for procedures involving contact with normally
sterile areas of the body. Use examination gloves for procedures involving contact with mucous
membranes, unless otherwise indicated, and for other patient care or diagnostic procedures that do
not require the use of sterile gloves.
Since no one glove can provide protection against all hazards, the gloves selected must be of
appropriate material, usually intact vinyl or nitrile, of appropriate quality for the procedures
performed, and of appropriate size for each health-care worker. Employers must not wash or
disinfect surgical or examination gloves for reuse. Washing with surfactants may cause “wicking,”
i.e. the enhanced penetration of liquids through undetected holes in the glove. Direct glove contact
with disinfecting agents (i.e., bleach, ethanol or isopropanol, gluturaldehyde) will cause glove
deterioration and must be avoided. General-purpose utility (rubber) gloves worn by maintenance,
housekeeping, laundry or other non-medical personnel may be decontaminated and reused. Do not
use gloves if they are peeling, cracked, or discolored, or if they have punctures, tears, or other
evidence of deterioration.
Used gloves should be discarded into an appropriate receptacle. When there is direct contact with
a patient’s secretions or excretions, gloves should be changed if care of the patient has not been
completed.
Policy and procedure for wearing gloves
Wear gloves on both hands for touching blood and body fluids, mucous membranes, or non-
intact skin of all patients, for handling items or surfaces soiled with blood or body fluids.
Change gloves immediately if they are torn or punctured.
Change gloves after contact with each patient’s blood or body fluids or after contact with
items or surface soiled with blood or body fluids.
Remove gloves before leaving the exam/patient room, dirty utility areas or other work areas.
Change gloves and wash hands between patient contact.
Wash hands after removing gloves.
Using gloves is essential in the following circumstances
During phlebotomy, injections, intravenous administration, wear gloves on both hands. Gloves
will reduce the incidence of blood contamination of hands, but they cannot prevent penetrating
injuries caused by needles or other sharp instruments.
Any time the health-care worker has cuts, abraded skin, chapped hands, dermatitis or the
like. Workers with chapped or abraded skin must contact their supervisor before initiating work
with potentially infectious materials. Waterproof bandages and double gloving

56
should be employed to protect the employee. If the employee cannot provide adequate
protection, she/he should not work with potentially infectious materials. This restriction should
remain in effect until the condition is resolved.
During instrumental examination of oropharynx, gastrointestinal tract and genitourinary tract.
When examining abraded or non-intact skin or patients with active bleeding.
During invasive procedures.
During all cleaning of body fluids and decontaminating procedures.
Clean technique
a.
Slip the gloves onto the right hand first and then the left, making sure they fit securely over
the cuffs of the isolation gown.
b.
Take an extra pair of gloves, protected by a clean paper towel, into the isolation room. The
extra gloves can be used in case the original pair tears or becomes soiled.
Sterile technique
Remove all jewelry, including rings (a plain wedding band is permitted)
Wash hands thoroughly with an antiseptic and dry them off with a paper towel. Use a paper
towel to turn off the faucet. (refer to page 49 for handwashing technique).
Open the package containing the sterile gloves.
Carefully open the inner wrapper, maintaining aseptic technique, being careful not to
contaminate the gloves by touching them (see diagram below).
Grasp the folded edge (inside surface) of the right glove’s cuff with the left hand (see
diagram below).
•
Slip the right hand inside the glove. To avoid contamination, the fingers on the left hand should
touch only the inside of the glove. If the glove becomes contaminated, discard it and obtain a
new one

57
Slip the fingers of the gloved hand under the cuff (touching only the outer surfaces) of the
glove, as shown below.
Insert the left hand into the glove and pull the glove on with the right hand. Avoid touching
the skin with the gloved hand.
Keep thumb
up and back
Adjust both gloves so they fit properly. Make sure no gaps exist between the fingertips and
the ends of the gloves.
Inspect the gloves for nicks and tears before and during the procedure. Obtain a new pair of
sterile gloves if a break in technique, nick or tear occurs.
5.2
Gowns
In general, gowns are recommended to prevent soiling of clothing when taking care of patients.
Gowns, aprons or lab coats are required when splashes to the skin or clothing with body fluid are
likely to occur. Gowns, including surgical gowns, shall be made of or lined with impervious
material and shall protect all areas of exposed skin. Gowns will also be worn when arms come into
contact with a patient’s blood or body fluids or non-intact skin.
When gowns are indicated, they should be worn only once and then discarded in an
appropriate receptacle.
Clean, freshly laundered or disposable gowns may be worn in most circumstances.
In some instances, as with extreme burns or extensive wounds, sterile gowns should be worn
when changing dressings.
Supplies of gowns are to be readily available.
The gown should be large enough to cover the clothing entirely and protect all areas of
exposed skin.
Procedure for putting on a gown
Slide the gown over the hands and arms by holding arms forward and slightly above head.

58
Fasten the gown at the back of the neck; then grasp the gown at the waistline in the back and
overlap the edges as much as possible. While holding the overlapping edge with one hand,
grasp one end of the belt with the other hand and pull it around the back and fasten.
Procedure for removing a contaminated gown
Untie belt in the back of the gown, and remove gloves if applicable. Wash and dry hands using
sink inside room. Unfasten the neck of the gown and pull off the first sleeve by slipping the
fingers under the cuff.
Do not
touch
Do not touch outside surface of cuff; the outside is contaminated and the hands are now clean.

59
Remove the second sleeve by grasping it through the first sleeve like this:
Without touching the outer surface of the gown, fold it with the outer contaminated surfaces
together. Then, roll the gown into a ball, being careful to touch only the inner uncontaminated
surface of the gown. If gown is non-disposable, place it into the patient’s linen hamper. If gown
is disposable, discard it into the patient’s covered waste receptacle. Always remember to hold
the contaminated gown away from the uniform.
Wash hands before leaving room and use a paper to turn off the faucets.
5.3
Face and Eye Protection
Face and eye protection must be worn whenever there is potential for the generation of splashes,
spray, splatter or droplets of blood or other potentially infectious material in the eyes, nose, mouth,
or other facial areas. Eye protection may prevent damage to the eye in addition to preventing
exposure to infectious materials. Certain disinfectants and other chemical can damage the eye or
cause blindness if splashed in the eye.
One or more devices may provide face and eye protection. Remember that the nose and mouth
must be protected if eye protection is worn, and vice-versa.
Product selection should be based upon acceptability to the wearer and the protection afforded. Eye
protection may be provided by safety glasses or normal glasses with side shields, goggles or chin
length face shields. Nose and mouth protection may be provided by surgical masks and face shields.

60
Face shields provide full-face protection against splashes and sprays to the face.
Some face shields are strong enough to provide protection against impact injuries.
Note that face shields do not offer mucous membrane protection from infectious
aerosols.
Goggles are another alternative for eye protection. Goggles form a face seal and
provide protection on the sides and top of the eyes
Safety glasses with side shields provide protection against splashes and sprays.
Note that splashes may reach the eye because glasses are not flush with the
user’s face. Also safety glasses do not offer eye protection from infectious
aerosols.
5.4
Surgical Masks
Surgical masks protect the mucous membranes of the mouth and nose. Surgical
masks are generally protective against droplets, splashes and sprays. Masks must
cover both the nose and the mouth, and fit the face closely, so that air passes through
the mask before being inhaled. Some surgical masks are available with attached eye
shields.
Moisture from expired air may eventually saturate the mask, making breathing difficult or fogging
eyeglasses. If this occurs, change the mask, discarding it as medical waste if contaminated with
human blood or other potentially infectious materials. Uncontaminated masks may be discarded in
the general trash. Surgical masks offer limited protection from infectious aerosols.
The use of masks and protective eye wear or face shields is required when contamination of
mucosal membranes (eyes, mouth or nose) with body fluid splashes or aerosolization is likely to
occur, such as during suctioning, surgical or dental procedures.
Procedure for Putting on a Mask
If the mask has a metal strip, position it over the nose with the metal strip facing outward; if
the mask does not have a metal strip, position it properly covering the mouth and nose.
Tie the mask’s top strings just above the top of the ears or place ties behind ears.
Pull down the lower part of the mask over the mouth and chin.
Tie the bottom strings around the neck.
Press the metal strip over the nose so the mask fits comfortably and snugly.
Change mask when it becomes moist, difficult to breath through or damaged.
Wash hands before touching mask and/or removing it. Discard mask in waste receptacle in
room before leaving room.
If both gown and mask are worn, remove gown first, wash hands, remove mask and discard
mask in waste receptacle in room. Wash hands prior to leaving room and use a paper towel to
turn off the faucets.
61
5.5
NIOSH Approved Particulate Masks and Respirators
Different respirators offer different levels of protection by varying their aerosol filter efficiency:
95%, 99% and 99.97%. NIOSH approved particulate masks and respirators for airborne precaution
use are the N95, N99 or N100. All respirator wearers must complete a medical surveillance
questionnaire. Training and fit testing is also required for all respirator wearers prior to use. A
respirator wearer would need to be refitted with the respirator if the wearer has a weight change of
20 pounds or more, significant facial scarring in the area of the facepiece seal, significant dental
changes (such as multiple extractions without prosthesis or acquiring dentures), reconstructive or
cosmetic surgery or any other condition that may interfere with facepiece sealing. Fit testing is
required initially and annually on all respirators with tight fitting face pieces. Respirator
information, training, and fit testing is available through the Yale Office of Environmental Health
and Safety; medical questionnaires are administered through the Employee Health office.
Respirators should be put on before entering the room of the patient on airborne precautions and
taken off, placed in a protective labeled bag in the anteroom. Discarded at the end of shift.
Employees who perform duties that may require respirator use must be trained and fit tested as per
the Yale University Respiratory Protection Program.
62
SECTION 6: Decontamination, Spill Response and Housekeeping
6.1
Sterilization or Disinfection of Reusable Medical Instruments/Devices:
Medical devices, equipment, and surgical materials are divided into three general categories,
1.critical items, 2. Semi-critical items, and 3. Non-critical items, based on the potential risk of
infection involved in their use.
Critical Items
Critical items are instruments or objects that are introduced directly into the bloodstream or into
other normally sterile areas of the body. Examples of critical items are surgical instruments, cardiac
catheters, implants, pertinent components of the heart-lung oxygenator, and the blood compartment
of a hemodialyzer. Sterility at the time of use is required for these items; consequently, one of
several accepted sterilization procedures is generally recommended.
Semi-Critical Items
Items in the second category are classified as semi-critical in terms of the degree of risk of infection.
Examples are noninvasive flexible and rigid fiber-optic endoscopes, endotracheal tubes, anesthesia
breathing circuits, and cystoscopes. Although these items come in contact with intact mucous
membranes, they do not ordinarily penetrate body surfaces. If steam sterilization can be used, it is
often cheaper to sterilize many of these items, but sterilization is not absolutely essential; at a
minimum, a high-level disinfection procedure that can be expected to destroy vegetative
microorganisms, most fungal spores, tubercle bacilli, and small non-lipid viruses is recommended.
In most cases, meticulous physical cleaning followed by an appropriate high-level disinfection
treatment gives the user a reasonable degree of assurance that the items are free of pathogens.
Non-Critical Items
Non-critical items are those that either do not ordinarily touch the patient or touch only intact skin.
Such items include crutches, bed boards, blood pressure cuffs, and a variety of other medical
accessories. These items rarely, if ever, transmit disease. Consequently, depending on the particular
piece of equipment or item, washing with a detergent may be sufficient.
The level of disinfection achieved depends on several factors, principally contact time, temperature,
type and concentration of the active ingredients of the chemical germicide, and the nature of the
microbial contamination. Some disinfection procedures are capable of producing sterility if the
contact times used are sufficiently long; when these procedures are continued long enough to kill
all but resistant bacterial spores, the result is high-level disinfection. Other disinfection procedures
that can kill many types of viruses and most vegetative microorganisms (but cannot be relied upon
to kill resistant microorganisms such as tubercle bacilli, bacterial spores, or certain viruses) are
considered to be intermediate- or low-level disinfection.
The tubercle bacillus, lipid and non-lipid viruses, and other groups of microorganisms in Table I
are used in the context of indicator microorganisms that have varying degrees of resistance to
chemical germicides and not necessarily because of their importance in causing nosocomial
infections. For example, cells of M. tuberculosis or M. bovis, which are used in routine efficacy
tests, are among the most resistant vegetative microorganisms known and, after bacterial
endospores, constitute the most severe challenge to a chemical germicide. Thus, a tuberculocidal
chemical germicide may be used as a high or intermediate-level disinfectant targeted to many types
of nosocomial pathogens but not specifically to control respiratory tuberculosis.

63
Table 1. Levels of Disinfection According to Types of Microorganism
Bacteria
Fungi
1
Viruses
Levels
Vegetative
Tubercle
Bacillus
Spores
Lipid &
Medium size
Non-lipid &
small
High
+
2
+
+
3
+
+
+
Intermediate
+
+
±
4
+
+
±
5
Low
+
-
-
±
+
-
1
Includes asexual spores but not necessarily chlamydospores or sexual spores.
2
Plus sign indicates that a killing effect can be expected when the normal use-concentrations of chemical disinfectants or pasteurization
are properly employed; a negative sign indicates little or no killing effect.
3
0nly with extended exposure times are high-level disinfectant chemicals capable of actual sterilization.
4
Some intermediate-level disinfectants can be expected to exhibit some sporicidal action.
5
Some intermediate-level disinfectants may have limited virucidal activity
In general, reusable medical devices or patient-care equipment that enters normally sterile tissue or
the vascular system or through which blood flows should be sterilized before each use. Sterilization
means the use of a physical or chemical procedure to destroy all microbial life, including highly
resistant bacterial endospores. The major sterilizing agents used in hospitals are
a) moist heat by steam autoclaving, b) ethylene oxide gas, and c) dry heat. However, there are a
variety of chemical germicides (sterilants) that have been used for purposes of reprocessing
reusable heat-sensitive medical devices and appear to be effective when used appropriately, i.e.,
according to manufacturer's instructions. These chemicals are rarely used for sterilization, but
appear to be effective for high-level disinfection of medical devices that come into contact with
mucous membranes during use (e.g., flexible fiber-optic endoscopes).
Disinfection means the use of a chemical procedure that eliminates virtually all recognized
pathogenic microorganisms but not necessarily all microbial forms (e.g., bacterial endospores) on
inanimate objects. There are three levels of disinfection: high, intermediate, and low. High-level
disinfection kills all organisms, except high levels of bacterial spores, and is effected with a
chemical germicide cleared for marketing as a sterilant by the Food and Drug Administration.
Intermediate-level disinfection kills mycobacterium, most viruses, and bacteria with a chemical
germicide registered as a "tuberculocide" by the Environmental Protection Agency (EPA). Low-
level disinfection kills some viruses and bacteria with a chemical germicide registered as a hospital
disinfectant by the EPA.
Heat stable reusable medical devices that enter the blood stream or enter normally sterile tissue
should always be reprocessed using heat-based methods of sterilization (e.g., steam autoclave or
dry heat oven).
Laparoscopic or arthroscopic telescopes (optic portions of the endoscopic set) should be subjected
to a sterilization procedure before each use; if this is not feasible, they should receive high-level
disinfection. Heat stable accessories to the endoscopic set (e.g., trocars, operative instruments)
should be sterilized by heat-based methods (e.g., steam autoclave or dry heat oven).
Reusable devices or items that touch mucous membranes should, at a minimum, receive high- level
disinfection between patients. These devices include reusable flexible endoscopes, endotracheal
tubes, anesthesia breathing circuits, and respiratory therapy equipment.
Medical devices that require sterilization or disinfection must be thoroughly cleaned to reduce
organic material or bio-burden before being exposed to the germicide, and the germicide and the
device manufacturer's instructions should be closely followed.
Except on rare and special instances (as mentioned below), items that do not ordinarily touch the
patient or touch only intact skin are not involved in disease transmission, and generally do not
necessitate disinfection between uses on different patients. These items include crutches, bed
boards, blood pressure cuffs, and a variety of other medical accessories. Consequently, depending
on the particular piece of equipment or item, washing with a detergent or using a low-

64
level disinfectant may be sufficient when decontamination is needed. If non-critical items are
grossly soiled with blood or other body fluids:
In patient-care areas, visibly soiled areas should first be cleaned and then chemically
decontaminated. For disinfection, the pre-cleaned areas should be moistened with the
appropriate germicide and allowed to air dry.
In the laboratory, large spills of cultured or concentrated infectious agents should be flooded
with a liquid germicide before cleaning, then decontaminated with fresh germicidal chemical
after organic material has been removed. It is not necessary to flood spills of blood or other
body fluids with germicide before cleaning.
Gloves should always be worn during cleaning and decontaminating procedures. Eye and face
protection may be needed if spraying or splattering is likely to occur to the face. Eye protection
may prevent damage to the eye in addition to preventing exposure to infectious materials. Certain
disinfectants and other chemical can damage the eye or cause blindness if splashed in the eye. Use
goggles or safety glasses and mask or full face shield to protect the mucous membranes of the face.
Exceptional circumstances that require non-critical items to be either dedicated to one patient or
patient cohort, or subjected to low-level disinfection between patient uses are those involving
Patients infected or colonized with vancomycin-resistant enterococci or other drug-resistant
microorganisms judged by the infection control program, based on current state, regional, or
national recommendations, to be of special or clinical or epidemiologic significance or
Patients infected with highly virulent microorganisms, e.g., viruses causing hemorrhagic fever
(such as Ebola or Lassa).
If you have questions about a low- or intermediate-level disinfectant, contact the manufacturer,
your local or state health department, or the Antimicrobial Program Branch, Registration Division,
Environmental Protection Agency (EPA), (703) 308-6411. Or, you may call the EPA disinfectant
hotline at 1-800-447-6349. The EPA is the federal regulatory agency for low- or intermediate-level
disinfectants.
If you have questions about high-level disinfectants (sterilants), or how to clean, disinfect or
sterilize a particular medical device, first contact the manufacturer of the product. If you are unable
to obtain sufficient information in this manner, contact the Food and Drug Administration (FDA)
regional office or the FDA Center for Devices and Radiological Health in Hartford at (860) 240-
4289/90 in Bridgeport at (203) 579-5822/3. FDA is the federal regulatory agency for safe and
effective use of medical devices and is now also responsible for regulation of chemical sterilants.
6.2
Reusable Patient-Care Equipment
Yale Health Personnel refer to Central Sterile Department Policy and Procedures located in the
Located in the Endoscopy Suite, 4
th
floor, Room 4277 (Decontamination) and room 4275
(Sterilization), for equipment reprocessing.
6.3
Sphygmomanometer and Stethoscope
No special precautions are indicated unless this equipment is contaminated (or likely to be
contaminated) with infective material. If soiled, wipe the stethoscope, cuff, gauge, bulb, and other
component parts with a cloth moistened with a disinfectant solution. See Contact Precautions for
additional information.

65
6.4
Soiled Linen & Laundry
It is the responsibility of the Housekeeping staff to remove all soiled/dirty linen and all trash from
the unit.
There is a method for disposal of linen soiled with blood and body secretions to reduce risk of staff
contact with the soiled linen. In accordance with standard precautions, employees are required to
wear gloves and gowns if necessary, while handling all soiled linen. All patient laundry is
considered to be soiled with blood or body fluids and should be handled using Standard Precautions.
All soiled linen is placed in the linen hampers
The risk of disease transmission from soiled linen is negligible. However, soiled linens may carry
large numbers of organisms that may contaminate the air and immediate environment if they are
“fluffed” or agitated.
All linen will be handled as potentially infectious. Linen will be transported in high tensile strength,
impervious bags. Soiled linen should be handled as little as possible and with minimum agitation
in order to prevent microbial dissemination into the air and onto employees handling the linen.
Soiled linen should not come into contact with attire. Hold the soiled linen away from your clothes.
If linen saturated wear a gown and booties to prevent further transmission. It should be placed in
bags as close as possible as the location it was used. It should not be sorted or rinsed in patient care
areas. Soiled linen must be collected and transported in impervious bags to prevent leakage. Bags
must be secured when filled (not overfilled) to prevent spillage during transportation. Soiled
laundry must be collected in covered hampers in patient care areas. Gloves must be worn when
handling linen.
YUHS Personnel refer to policy Laundry - Appendix # 2
6.5
Housekeeping
All waste baskets in the rooms of patients shall be lined with plastic liners. When full these bags
shall be removed, using gloves, closed (placed in a second plastic bag that is closed), and
transported to the dumpster.
Bathrooms shall be cleaned in the usual manner using gloves and germicide/disinfectant solution.
Gloves shall be worn when cleaning showers and bathtubs, using the germicidal disinfectant
solution once each day. Tub cleaning with germicidal disinfectant solution will be followed by
scrubbing with a cleaner and rinsed thoroughly.
Housekeeping Staff shall wear gloves when removing all trash. The trash in the specially
marked waste containers in the treatment rooms is to be double bagged and removed by
Housekeeping Staff wearing gloves.
All horizontal surfaces shall be cleaned in accordance with a germicidal solution in
accordance with manufacturer's recommendations daily and as required.
Floors shall be mopped thoroughly and cleaned with germicidal solution once a week and as
required.
Wall shall be spot cleaned with detergent and germicide solution when soiled and shall be
periodically cleaned according to prescribed housekeeping routine.
Institutionally approved germicide can be obtained through the Purchasing department.
6.6
Cleaning Spills of Blood and Body Fluids on Environmental Surfaces
All spilled blood and other body fluids are handled and managed safely to maintain a safe
environment. Household bleach (5.25 sodium hypochlorite) or an appropriate tuberculocidal
disinfectant shall be used to clean all spills of human blood and other potentially infectious
materials.

66
YUHS Personnel refer to policy Clean Up of Spills - Appendix # 3
If spill response /mess kits are unavailable in facility, either obtain prepared spill kit or assemble
your own spill response kit.
Prepare and maintain a spill response kit.
Basic equipment is some disinfect and solidifying agent, paper towels, household rubber gloves,
biohazard bags, and forceps to pick up broken glass and PPE. The contents of the kit are kept in a
plastic container. There are commercial available spill kits for cleaning blood and body fluids.
References:
Favero MS, Bond WW. Sterilization, disinfection, and antisepsis in the hospital. In: Manual of
Clinical Microbiology, 1991; chapter 24:183-200. American Society for Microbiology.
Washington, DC.
Garner JS, Favero MS. Guidelines for handwashing and hospital environmental control, 1985.
MMWR, 1987;36(25 Supplement). MMWR 1988;37(24)
Rutala WA. APIC guideline for selection and use of disinfectants. Am J Infect Control
1996;24:313-342.

67
SECTION 7: Medications and Safe Injection Practices
7.1 Storage of Medications – Multi-Dose Vials/Single-Dose Vials
Single-dose vials: Approved for use on a single patient for a single procedure or injection.
Multi-dose vials: Use a new sterile needle and syringe each time entering the vial. Do not keep multi-dose
vials in the immediate patient treatment area.
The rubber stopper should be wiped with alcohol each time the vial is entered. If multiple-dose
vials are used, the date and time of opening should be written on the label with the initials of the
person who opened it. Multi-dose vials must be examined for precipitate matter and evidence of
discoloration prior to each use. Vials are stored in accordance with manufacturer recommendations.
YUHS Personnel refer to policy Quality Control of Multi-dose Vials - Appendix Yale Health #1
Medications should be stored in areas with restricted access and secured in a locked cabinet.
Medications should not be stored on counter tops next to the sink. The person administering unit
dose medications should always check to be certain that the package is sealed and that the expiration
date has not passed.
Only supplies used for medication and patient treatment shall be stored in the treatment room or
dedicated refrigerator. The medication refrigerator must be checked for outdated medications and
kept clean. The temperature (36 F –40F) of the medication refrigerator must be monitored daily. A
log must be maintained to include daily temperature checks, weekly and as needed cleaning and
routine inspection of contents.
Horizontal surfaces in the treatment room shall be wiped with a germicide solution weekly and as
needed and sinks shall be scoured and germicide solution applied daily.
Sterile water and saline for irrigation should be labeled with the date and time it was opened. The
bottles should be discarded at the end of 24 hours.
Hydrogen peroxide must be dated when opened and discarded at the end of the week. Contact
Environmental Affairs (203-432- 6545) for information on disposal procedures.
Note: Controlled Substances must be kept in a secured locked area. Clinics who utilize controlled
substances must have an updated license with the State and Federal Drug Enforcement Agency.
An Inventory must be kept of all controlled substances. A copy of this inventory must be sent to
the State DEA by May 1
st
of each year.
7.2 Fingerstick Devices
68
• Two types of devices:
• Auto-disabling single use
• Reusable
• Single use, auto-disabling devices are disposable and, by design, prevent re-use
• Use in settings where assisted BGM is performed.
• Reusable devices cannot be adequately cleaned and disinfected.
• Never use for more than one person.
• Even when not visibly soiled, have been responsible for transmitting hepatitis when stored with other
devices.
• Use new pair of gloves for each new test.
• Perform hand hygiene before and after glove use.
• Avoid handling test strip containers with soiled gloves to avoid contamination.
• If a new test strip is needed, discard soiled gloves and perform hand hygiene before obtaining a new test
strip.
7.3 Blood Glucose Meter
• When possible, should be assigned to an individual person and should not be shared.
• If the meter must be shared, clean and disinfect after every use, per manufacturer’s instructions:
• Use the disinfectant recommended by the manufacturer.
• Typically, an EPA approved disinfectant (effective against Human HIV-1 and Hepatitis B Virus)
• Follow recommended dwell time (or contact time) specified on label.
• If manufacturer does not specify how the device should be cleaned and disinfected, it should not be shared.
• Always maintain aseptic technique:
• Hand hygiene and glove use
• Separate clean and dirty
• Cleaning of environment

69
SECTION 8: Storage and Transporting of Specimens
8.1
Handling of Clinical Specimens
All clinical specimens, regardless of patient origin, will be subject to the application of Standard
Precautions and handled as potentially infectious.
All specimens will be packaged in a lab provided approved sealable plastic bag prior to
transportation to the lab so that lab slips will not come in direct contact with specimen
container. *This bag must be sealed when delivered to the lab.
Urine, vomitus and feces from patients can be safely flushed down the toilet into the
municipal sewage system.
Care should be taken when collecting specimens to avoid contamination of the outside of the
container. Contaminated materials used in laboratory tests should be decontaminated before
reprocessing or be placed in bags and disposed of in accordance with institutional policies for
disposal of infectious waste. Bagging is intended to prevent inadvertent exposure of laboratory
or transport personnel to infective material and prevent contamination of the environment.
All blood or body fluid specimens must be transported from one area to another using
appropriate leak proof specimen transport container or placed in the specimen refrigerator or
specimen pick-up container that are labeled with the biohazard label.
8.2
Protocol on Management of Specimens
Wear gloves when collecting and handling specimens.
Collect specimens in appropriate container following specimen requirements (spinning,
freezing, etc.)
Close container tightly. Leakage leads to contamination of specimen and personnel.
Label specimen container including all appropriate information. All specimens must be
labeled in the presence of the patient utilizing 2 identifiers
Fill out laboratory requisition form completely.
Contact appropriate Lab (Yale, Quest)
Place container in the lab specific sealable plastic bag.
Attach requisition to bagged specimen.
Transport specimens in an upright in the YUHS approved transport container/cooler.
Deliver specimen promptly to the appropriate pick-up storage container or specimen
refrigerator that is labeled with the Biohazard label.
Wash hands with soap and water after contact with secretions, excretions, blood and articles
contaminated with bodily fluids. See Section 2.5 Emergency Procedures for Exposure to Blood
and Body Fluids for additional information concerning exposures to potentially infectious
materials.
For spills, disinfect area promptly with tuberculocidal disinfectant or 10% household bleach
(1:10 dilution: 1 part bleach to 9 parts water). Wear gloves for clean up. Refer to spill policy.

70
SECTION 9: Transportation of Patient
9.1
Transportation Process
Patient infected with virulent or epidemiologically important microorganisms should leave their
room only for essential purposes. When special studies are ordered, the individual requesting the
study should indicate on the requisition the patient is on transmission based precautions. The patient
and transport personnel should use acquisition barriers (masks, impervious dressings, etc.) to
prevent transmission. Personnel in the area to which the patient is to be taken should be notified
of the impending arrival of the patient and of precautions to be used to Prevent transmission of
infection. Patient should be alerted to the potential spread of their disease and informed as to how
they can assist in maintaining a barrier against transmission of their infection to others.
9.2
General Considerations and Responsibilities
The preparation of transportation of patient to other departments or institutions and the notification
concerning the impending arrival of the patient is a multi-disciplinary responsibility that requires
collaboration and teamwork. The nurse, the unit receptionist and transport personnel are jointly
responsible for the following actions:
Unit Receptionist:
Notify the department to which the patient is being transported (e.g. Diagnostic Imaging,
Physical Therapy, etc.) that the patient is on transmission based precautions.
Nurse:
Instruct the transporter in transmission based precautions when the transporter arrives on the
patient-care unit to transport the patient to another area of the hospital. Before entering the
room, put on essential protective barriers as indicated by the transmission based precautions
(such as gloves, gown, face shield, mask or respirator). Explain to the patient what special
precautions will be taken before he/she leaves the room. Put the mask on the patient if required
under the specific transmission based precautions. Assist the patient into wheelchair or
stretcher.
Transport Personnel:
Receive instructions from the nurse when he/she arrives on site. Bring clean wheelchair or
stretcher to the patient’s room. The vehicle should be protected by a clean sheet. Before
entering the room, put on essential protective barriers. Assist the patient into wheelchair or
stretcher. Remove gloves and wash hands with an antiseptic solution when transportation is
complete. Push transport vehicle outside room and transport patient to designated area as
expeditiously as possible.
9.3
Infection Control Considerations for Personnel Transporting Patients on Contact
Precautions Only
During the transportation process, the following infection control procedures should be
considered:
When transporting the patient to another department, if soiling of the uniform is likely to occur,
wear a gown to protect clothing and wear gloves for touching infective material; if soiling is
not likely, no special precautions are required other than GOOD HAND WASHING.

71
Transport patient to area of destination as expeditiously as possible utilizing the service
elevator when possible, limiting contact with others.
Wash hands after direct contact with the patient, contaminated equipment and before
touching another patient.
Discard the sheet in contaminated laundry in patient’s room.
Spray and wipe the chair, stretcher, or wheelchair and wipe with a disinfectant according to
cleaning and reprocessing of non-critical patient care equipment and medical devices.
9.4
General Considerations for Patients
Help the patient to bed.
Push wheelchair or stretcher to door.
Wash hands upon leaving the isolation area.

72
SECTION 10: Reporting Communicable Diseases to the State of Connecticut
REPORTABLE DISEASES, EMERGENCY ILLNESSES and HEALTH CONDITIONS - 2017
The Commissioner of the Department of Public Health (DPH) is required to declare an annual list of Reportable Diseases,
Emergency Illnesses and Health Conditions. The Reportable Disease Confidential Case Report form (PD-23) or other disease
specific form should be used to report the disease, illness, or condition. Reports (mailed, faxed, or telephoned into the DPH) should
include the full name and address of the person reporting and attending physician, name of disease, illness or condition, and full
name, address, date of birth, race/ethnicity, gender and occupation of the person affected. Forms can be found on the DPH website.
See page 4 for a list of persons required to report Reportable Diseases, Emergency Illnesses and Health Conditions. Mailed reports
must be sent in envelopes marked “CONFIDENTIAL.” Changes for 2017 are noted in bold and with an asterisk (*).
Category 1 Diseases: Report immediately by telephone on the day of recognition or strong suspicion of disease for those
diseases marked with a telephone (). Also mail a report within 12 hours.
Category 2 Diseases: Diseases not marked with a telephone are Category 2 diseases. Report by mail within 12 hours of
recognition or strong suspicion of disease.
Acquired Immunodeficiency Syndrome (1,2) HIV-1 / HIV-2 infection in: (1) Rotavirus
Acute flaccid myelitis ▪ persons with active tuberculosis disease Rubella (including congenital)
Anthrax ▪ persons with a latent tuberculous Salmonellosis
Babesiosis infection (history or tuberculin skin test SARS-CoV
Botulism >5mm induration by Mantoux technique) Shiga toxin-related disease (gastroenteritis)
Brucellosis ▪ persons of any age Shigellosis
California group arbovirus infection ▪ pregnant women Silicosis
Campylobacteriosis HPV: biopsy proven CIN 2, CIN 3 or AIS Smallpox
Carbon monoxide poisoning (3) or their equivalent (1) St. Louis encephalitis virus infection
Chancroid Influenza-associated death (7) Staphylococcal enterotoxin B pulmonary
Chickenpox
Influenza-associated hospitalization (7) poisoning
Chickenpox-related death Lead toxicity (blood level ≥ 15 µg/dL) Staphylococcus aureus disease, reduced or
Chikungunya Legionellosis
resistant susceptibility to vancomycin (1)
Chlamydia (C. trachomatis) (all sites) Listeriosis Staphylococcus aureus methicillin-
Cholera Lyme disease resistant disease, invasive, community
Cryptosporidiosis Malaria acquired (4*,10)
Cyclosporiasis Measles Staphylococcus epidermidis disease,
Dengue Melioidosis reduced or resistant susceptibility
Diphtheria Meningococcal disease to vancomycin (1)
Eastern equine encephalitis virus infection Mercury poisoning Syphilis
Ehrlichia chaffeensis infection Mumps Tetanus
Escherichia coli O157:H7 gastroenteritis Neonatal bacterial sepsis (8) Trichinosis
Gonorrhea Neonatal herpes (≤ 60 days of age) Tuberculosis
Group A Streptococcal disease, invasive (4*) Occupational asthma Tularemia
Group B Streptococcal disease, invasive (4*) Outbreaks: Typhoid fever
Haemophilus influenzae disease, invasive (4*) ▪ Foodborne (involving ≥ 2 persons) Vaccinia disease
Hansen’s disease (Leprosy) ▪ Institutional Venezuelan equine encephalitis virus infection
Healthcare-associated Infections (5) ▪ Unusual disease or illness (9) Vibrio infection (parahaemolyticus,
Hemolytic-uremic syndrome (6) Pertussis vulnificus, other)
Hepatitis A Plague Viral hemorrhagic fever
Hepatitis B: Pneumococcal disease, invasive (4*) West Nile virus infection
3.
acute infection (2) Poliomyelitis Yellow fever
4.
HBsAg positive pregnant women Q fever
Zika virus infection Hepatitis C: Rabies
5.
acute infection (2) Ricin poisoning
6.
positive rapid antibody test result Rocky Mountain spotted fever
FOOTNOTES:
1.
Report only to State.
6. On request from the DPH and if adequate serum is available, send serum from
2.
As described in the* CDC case definition.
patients with HUS to the DPH Laboratory for antibody testing.
3.
Includes persons being treated in hyperbaric chambers for suspected CO
7. Reporting requirements are satisfied by submitting the Hospitalized and Fatal
poisoning.
Cases of Influenza-Case Report Form in a manner specified by the DPH.
4.
Invasive disease: from sterile fluid (blood, CSF, pericardial, pleural,
8. Clinical sepsis and blood or CSF isolate obtained from an infant ≤ 72 hours of age.
peritoneal, joint, or vitreous) bone, internal body sites, or other normally
9. Individual cases of “significant unusual illness” are also reportable.
sterile site including muscle. *
10. Community-acquired: infection present on admission to hospital, and person has
5.
Report HAIs according to current CMS pay-for-reporting or pay-for-
no previous hospitalizations or regular contact with the health-care setting.
performance requirements. Detailed instructions on the types of HAIs, facility types
and locations, and methods of reporting are available on the DPH website: www.ct.
gov/dph/HAI.

73
How to report: The PD-23 is the general disease reporting form and should be used if other specialized forms are not available. The PD-23 can be found on the DPH
website (www.ct.gov/dph/forms). It can also ordered by writing the Department of Public Health, 410 Capitol Ave., MS#11EPI, P.O. Box 340308, Hartford, CT 06134-0308 or
by calling the Epidemiology and Emerging Infections Program (860-509-7994). Specialized reporting forms are available on the DPH website or by calling the following
programs: Epidemiology and Emerging Infections Program (860-509-7994) - Hospitalized and Fatal Cases of Influenza, Healthcare Associated Infections (860-509-7995) -
National Healthcare Safety Network, HIV/AIDS Surveillance (860-509-7900) - Adult HIV Confidential Case Report form, Immunizations Program (860-509-7929) -
Chickenpox Case Report (Varicella) form, Occupational Health Surveillance Program (860-509-7740) - Physician’s Report of Occupational Disease, Sexually Transmitted
Disease Program (860-509-7920), and Tuberculosis Control Program (860-509-7722).
Telephone reports of Category 1 disease should be made to the local Director of Health for the town in which the patient resides, and to the Ep idemiology and
Emerging Infections Program (860-509-7994). Tuberculosis cases should be directly reported to the Tuberculosis Control Program (860-509-7722). For the name, address,
or telephone number of the local Director of Health for a specific town contact the Office of Local Health Administration (860-509-7660).
For public health emergencies on evenings, weekends, and holidays call 860-509-8000.

74
SECTION 11: Service and Assistance Animals
In compliance with the Americans with Disabilities Act and other applicable state and federal law,
the purpose of this policy is to establish guidance for Yale University employees in a clinical setting.
For the policy statement please refer to the Yale University policy for service and assistance animals.
https://your.yale.edu/policies-procedures/policies/4400-service-and-assistance-animals
11.1 Guidelines for Service Animals Visiting Heath Care Facilities.
1. Require that all patients, visitors and health care workers practice hand hygiene both before
and after each animal contact.
2. Require that animal handlers carry an alcohol based hand rub product with them, and that
they offer the product to anyone who wishes to touch the animal.
3. Require that animal handlers practice personal hand hygiene in accordance with Yale
University policy for employees.
4. Service animals must be harnessed, leashed or tethered unless these devices interfere with
the animal's work or the person's disability prevents using these devices.
5. The handler must carry supplies sufficient to clean up the animal’s excreta (feces, urine,
vomitus). If the animal has an elimination accident, gloves should be worn to remove the
debris and clean up the area and hand hygiene performed after glove removal. Any organic
debris and paper towels should be placed in a plastic bag and discarded in an outdoor trash
receptacle. After the area is cleaned, it must be disinfected with the facility's approved
product, following the label instructions for appropriate concentration and contact time.
6. Patients must make arrangements to take care of the pet if they cannot physically do so.
7. Access cannot be denied to a person with a service animal because of allergies or fear of
dogs. If a person has allergies to dog dander or is afraid of a dog, accommodations should be
made by assigning them to different locations in the room or different rooms in the facility.
11.2 Staff Responsibilities
1. When encountering an individual with a disability, it is acceptable to ask if they need
assistance. If yes, ask how you can best assist them.
2. Allow a service animal to accompany the partner at all times and everywhere on campus
except where service animals are specifically prohibited.
3. A person with a disability cannot be asked to remove his or her service animal from the
premises unless the dog is not housebroken, is out of control, or if the handler/owner does
not take effective action to control the service animal.
4. When encountering an individual with a service animal, treat the individual and the service
animal with respect and do not treat the animal like a pet (e.g. pat the animal or otherwise
distract it from its duties).
5. With regard to those with animals that appear to be service animals, staff may not ask about
the person’s disability; require medical documentation, a special identification card, or
training documentation for the dog; or ask the dog to demonstrate its ability to perform the
work or task. When it is not obvious what task is being performed by a service animal, staff
may ask only two questions:
• Is the dog a service animal required because of a disability?
• What work or task has the dog been trained to perform?
6. Staff is not required to provide care or food for a service animal.
75
11.3 Permitted and Restricted Areas for Service Animals and Additional Information for Staff
Areas Where Service Animals Are Permitted:
A service animal is permitted in areas of Yale University clinics that are unrestricted to inpatients,
outpatients or visitors, provided the presence of the animal does not compromise patient care subject
to the following:
Areas Where Service Animals Are Not Permitted:
Restricted areas where a service animal generally cannot be permitted include:
1. Areas that employ greater than general infection-control measures
2. Other restricted areas include:
• Food preparation areas
• Central sterile processing
• Operating rooms (and other invasive treatment/procedure rooms)
• Post anesthesia areas
• Heart and vascular procedure rooms
• Intensive care units and/or other locations with immunocompromised patients.
Individualized (case-by-case) assessment should be made to determine whether animal
visitation is appropriate for immunocompromised patients.
• Diagnostic areas
• Family birthing areas
• Nurseries
• Medication rooms
• Pharmacy
• Playrooms
• Oncology transplant unit
• Areas, facilities, or rooms where a patient(s) have
o altered mental status
o had a splenectomy
o open wounds
o behavior or psychiatric disorders

75
APPENDIX A: Needle Stick Procedure
Standard:
Yale Health will have a policy to define the sequence of events which needs to take place
after a health care worker sustains a needlestick, or other injury involving exposure to
human blood or body fluids. This policy conforms to the requirements set forth by
OSHA.
Policy:
The Yale Health needlestick policy has been developed by the Department of Employee
Health and applies to all health care workers of the facility. Any health care worker
(HCW) who sustains a needlestick or exposure to human blood or body fluids during the
course of his or her job duties must follow the steps outlined in the following procedure.
The policy’s aim is to provide the optimum care to the injured HCW and attempt to
prevent or identify infections caused by blood borne pathogens that the employee might
be exposed to in the course of the injury.
Procedure:
1. Employees or students who sustain a needlestick should Immediately report to
receive medical care at Yale Health (Employee Health Department 432-7978,
Student Health 432-0312, or Acute Care 432-0123). It is important to begin any
recommended treatment within 1 to 2 Hours after exposure.
2. If the exposure occurs at the Yale New Haven Medical Center and the HCW
wishes to be seen on site, he/she should report to the Occupational Health Service
(7:30 a.m. to 4:30 p.m., Monday through Friday) at 203-688-2462 or to Yale New
Haven Hospital Emergency Room (203-688-2222) if the episode occurs outside
of regular daytime working hours.
3. The source patient for the exposure should be immediately approached to give
consent for a baseline HIV, Hepatitis B Surface Ag, Hepatitis B Surface Ab,
Hepatitis B core Ab, and Hepatitis C Ab. Rapid HIV testing on the source patient
should be requested for all needlestick cases. Rapid HIV testing can be done at the
Yale-New Haven Hospital Laboratory. The attending physician for the source
patient should be notified to obtain this testing. The Yale Health or YNHH
Occupational Health providers can assist with this process. If the source patient
has no medical provider to perform testing and consents to testing, the treating
M.D. can order the tests through Yale Health and bill to Employee Health. The
Employee Health provider must be informed of the testing and of a means to
follow up with source patient to communicate the results. If the source patient
does not give consent for testing, the institution's needlestick committee should
convene as soon as possible to take the necessary steps to obtain testing. If the
source is known to be HIV positive or is on antiretroviral therapy, then the
attending physician should be questioned about known HIV resistance patterns.
76
This should be considered when prescribing anti-viral treatment. Do not delay
treatment pending the information however.
4. Consider requesting expert Infectious Disease Consult for exposures to known
HIV source cases that are currently receiving treatment for HIV. The CDC Post
Exposure Prophylaxis Hotline at 1-888-448-4911 is available for consultation 24
hours a day.
5. The exposed employee/student should immediately be tested for a baseline HIV,
Hepatitis B Surface Ab, Hepatitis C Ab following the institution's established
testing guidelines.
6. Post Exposure Prophylaxis ( PEP) should be offered to any health care provider
who has been exposed to blood or body fluids from an HIV positive source, or
from a source with reasonable suspicion of HIV infection. PEP is not justified for
situations where there is negligible risk of transmission. Expert consultation
should be sought if needed to determine the need for PEP.
7. Any health care provider who is prescribed PEP should receive a 3 drug regimen.
The preferred regimen is:
a.
Truvada once daily plus Raltegrvir (Isentress) 400 mg bid for 4
weeks.
b.
This should be started as soon as possible, using the starter packets
available in the Pharmacy or Pyxis in Acute Care. If treatment has been
delayed but the exposure is subsequently found to be high risk, it may be
started up to 72 hours later (this could change the effectiveness).
8. If the source patient is subsequently found to be HIV negative, any PEP that was
prescribed should be discontinued and no further follow up is indicated.
9. Workers who receive antiviral prophylaxis should also have baseline CBC, renal
and hepatic function tests drawn.
10. If antiviral prophylaxis for HIV is indicated, the HCW should be given a 96 hour
packet of prophylactic medication, which is available at each institution in the
Pharmacy or Pyxis in Acute Care.
11. The health care worker should then be instructed to follow up with the appropriate
department (either Employee Health at 432-7978 or Student Health 432-0312) on
the next business day by phone to receive further instructions within 72 hours.
12. All HCWs taking antiviral prophylaxis should be reevaluated at 2 weeks for a
CBC, LFT's and renal functions to check for any symptoms of drug toxicity,
which may necessitate a reduction of dosage or change in medication. Expert
consultation with an infectious disease specialist should be obtained for situations
which might require a change in the protocol or for cases where the source HIV
strain is known to be resistant to one or more drugs.
13. If the health care worker follow up testing is done using a 4th generation HIV p24
Ag/HIVAb test, they should receive follow up testing at 6 weeks and 4 months,
77
after which follow up can be considered complete. (Testing should be extended to
6 months if a standard HIV Ab test is used).
14. See Appendix 1 for situations where expert consultation for PEP is recommended.
15. The exposed worker should be advised to use precautions (e.g., use of barrier
contraception and avoidance of blood or tissue donations, pregnancy, and, if
possible, breast-feeding) to prevent secondary transmission, especially during the
first 6–12 weeks after exposure. They should be counseled about symptoms of
acute retroviral syndrome, possible drug interactions, the need to adhere to the
PEP regimen and possible drug toxicities and rashes.
16. Appropriate prophylaxis for Hepatitis B exposure should be included in all
evaluations where indicated. (See Table 3)
17. The employee should be evaluated for exposure to Hepatitis C if the source
patient is infected with Hepatitis C or has risk factors for infection. Testing for
Hep C should include a viral RNA for Hep C and Hep C AB at 4-6 weeks, and a
Hep C Antibody at 3-4 months, and 6 months.
18. All employees/students who sustain a potential exposure to blood or bodily fluids
should make certain an incident report is filed within 24 hours (at Yale-New
Haven Hospital or Yale Medical School, this is done at the Medical-Legal Affairs
Office, 203 Clinic Building). Employees should also make certain a Yale
University Report of Injury is filed.
19. All record of testing and treatment of HCW should follow established
confidentiality guidelines and should be forwarded to the physician who will be
following the patient (either in Employee Health or Student Health).
20. Employees who refuse to get initial HIV testing may choose to have their initial
serum drawn and stored in the laboratory. They must be informed that their
refusal to submit to HIV testing within 72 hours post accident will make it
impossible to order testing of the source patient without consent.
21. Please see Table A1 for alternative PEP regimens and Table B1 for side effects
information.
Reference: “JSTOR: Infection Control and Hospital Epidemiology, Vol. 34, No. 9 (September 2013)

78
Needle Stick Procedure Appendix 1
Situations for Which Expert Consultation for Human Immunodeficiency Virus (HIV)
Post exposure Prophylaxis (PEP) Is Recommended
Delayed (i.e., later than 72 hours) exposure report
• Interval after which benefits from PEP are undefined
Unknown source (e.g., needle in sharps disposal container or laundry)
• Use of PEP to be decided on a case-by-case basis
• Consider severity of exposure and epidemiologic likelihood of HIV exposure
• Do not test needles or other sharp instruments for HIV
Known or suspected pregnancy in the exposed person
• Provision of PEP should not be delayed while awaiting expert consultation
Breast-feeding in the exposed person
• Provision of PEP should not be delayed while awaiting expert consultation
Known or suspected resistance of the source virus to antiretroviral agents
• If source person’s virus is known or suspected to be resistant to 1 or more of the
drugs considered for PEP, selection of drugs to which the source person’s virus is
unlikely to be resistant is recommended
• Do not delay initiation of PEP while awaiting any results of resistance testing of
the source person’s virus
Toxicity of the initial PEP regimen
• Symptoms (e.g., gastrointestinal symptoms and others) are often manageable
without changing PEP regimen by prescribing antimotility or antiemetic agents
• Counseling and support for management of side effects is very important, as
symptoms are often exacerbated by anxiety
Serious medical illness in the exposed person
• Significant underlying illness (e.g., renal disease) or an exposed provider already
taking multiple medications may increase the risk of drug toxicity and drug-drug
interactions
Expert consultation can be made with local experts or by calling the National Clinicians’
Post-Exposure Prophylaxis Hotline (PEPline) at .
79
Needle Stick Procedure Appendix 2
Counseling of Healthcare Personnel (HCP) Exposed to Known or Suspected Human
Immunodeficiency Virus (HIV)–Positive Sources
Counseling (at the time of exposure and at follow-up appointments). Exposed HCP
should be advised to use precautions (e.g., use of barrier contraception and avoidance of
blood or tissue donations, pregnancy, and, if possible, breast-feeding) to prevent
secondary transmission, especially during the first 6–12 weeks after exposure.
For exposures for which post exposure prophylaxis (PEP) is prescribed, HCP should be
informed regarding the following:
• Possible drug toxicities (e.g., rash and hypersensitivity reactions that could imitate
acute HIV seroconversion and the need for monitoring)
• Possible drug interactions
• The need for adherence to PEP regimens

TABLE 3. Postexposure management of health-care personnel after occupational
percutaneous and mucosal exposure to blood and body fluids, by health-care personnel
HepB vaccination and response status
Postexposure testing
Postexposure prophylaxis
Source patient
(HBsAg)
HCP testing
(anti-HBs)
HBIG*
Vaccination
Documented
responder
§
after complete
series (≥3 doses)
No action needed
Positive/unknown
—**
HBIG x2
separated
by 1 month
—
No
Negative
No action needed
Positive/unknown
<10mIU/mL
**
HBIG x1
Negative
<10mIU/mL
None
Any result
≥10mIU/mL
No action needed
Positive/unknown
—**
HBIG x1
Complete
vaccination
Yes
Negative
—
None
Complete
vaccination
Yes
Abbreviations: HCP = health-care personnel; HBsAg = hepatitis B surface antigen; anti-HBs = antibody to hepatitis B surface
antigen; HBIG = hepatitis B immune globulin.
* HBIG should be administered intramuscularly as soon as possible after exposure when indicated. The effectiveness of HBIG when
administered >7 days after percutaneous, mucosal, or nonintact skin exposures is unknown. HBIG dosage is 0.06 mL/kg.
†
Should be performed 1–2 months after the last dose of the HepB vaccine series (and 4–6 months after administration of HBIG to avoid
detection of passively administered anti-HBs) using a quantitative method that allows detection of the protective concentration of anti-HBs (≥10
mIU/mL).
§
A responder is defined as a person with anti-HBs ≥10 mIU/mL after ≥3 doses of HepB vaccine.
¶
A nonresponder is defined as a person with anti-HBs <10 mIU/mL after ≥6 doses of HepB vaccine.
** HCP who have anti-HBs <10mIU/mL, or who are unvaccinated or incompletely vaccinated, and sustain an exposure to a source patient who
is HBsAg-positive or has unknown HBsAg status, should undergo baseline testing for HBV infection as soon as possible after exposure, and
follow-up testing approximately 6 months later. Initial baseline tests consist of total anti-HBc; testing at approximately 6 months consists of
HBsAg and total anti-HBc.
80

81

82

83

84
85
APPENDIX B: HIV Counseling Guidelines
Risks
The risk of HIV infection after percutaneous exposure to human blood and body fluids is estimated to be 0.3%
on average. The risk is estimated to be higher in cases where the exposure involves a deep injury with a hollow
bore instrument from a patient that has end stage AIDS or an early retro viral syndrome. The risks of a mucous
membrane or skin exposure to HIV infected material is estimated to be lower.
Symptoms
Patients who are exposed to material that is potentially infected with HIV should be counseled about the
symptoms of the acute retroviral syndrome. Symptoms include
fever
sore throat
nausea
headache
enlarged lymph nodes
rash
The symptoms will generally appear within six weeks after an exposure to HIV. The symptoms may be similar
to a viral illness due to other agents, so that patients should be told not to assume the worst if they experience
symptoms after an exposure. Patients should be encouraged to report any suspicious symptoms to their primary
care provider in order to have them evaluated.
Precautions to prevent infection
All patients who have had a potential exposure to HIV should take precautions to avoid possible secondary
transmission. These precautions are the following:
use a condom when engaging in sexual activities
refrain from open mouth kissing
avoid sharing shaving instruments
refrain from donating blood, organs, or other tissues
avoid breast-feeding or becoming pregnant.
Patients should be encouraged to come back for follow up testing at 6 weeks, 3 months, and 6 months. Patients
should continue these precautions until testing at 6 months post exposure confirms lack of seroconversion.
Antiviral Drugs
Patients should be prescribed anti viral drugs based on the needlestick protocol guidelines and risk categories.
Patients should be instructed to begin taking the drugs immediately since the greatest potential benefit results
when the drugs are taken within the first one to two hours post exposure. Patients may be given an initial 72-
hour supply of anti-HIV medications at the time of evaluation. They must contact their clinician and arrange
for further medication without interruption, for a total treatment course of four weeks.

86
APPENDIX Yale Health 1: Quality Control of Single and Multi-dose Vials/Sterile Solutions
Subject:
Quality control of single dose and multidose vials, non-preservative irrigation solutions,
dated and undated items and topicals
Standard:
Sterility of multidose medication vials/containers will be maintained.
Quality control of multidose medication vials, single use vials, non-preservative irrigation
solutions, non-dated items (alcohol, H
2
O
2
, and green soap), dated items (Betadine), and
topicals will be documented.
Policy
1.
All single and multidose vials/medications will be discarded after single patient use.
•
Medications will be ordered and stocked as single dose vials when possible.
•
Medications only available as multidose vials will still only be used for single patient
administration.
•
Injectable medication administered in the department are basic medical treatment. There
is no charge to the patient.
•
Medications supplied in the department include but are not limited to:
▪
Anesthetics (i.e. Lidocaine 1%, 2% with and without Epinephrine, Benzocaine,
Sodium Bicarbonate).
▪
Steroids (i.e. Kenalog, Celestone, Depo-Medrol, etc.)
2.
Non-preservation irrigation solutions must be discarded at the end of single patient procedure or at
the end of each clinic day. (Normal Saline Irrigation or Sterile Water Irrigation).
3.
Opened solutions i.e., alcohol, peroxide, green soap, betadine will have an expiration sticker
applied when opened. The expiration date will reflect the 1st day of the next month. (Example:
Betadine opened August 15th will have expiration date September 1) All open solutions must be
discarded on the first clinic day of each month.
•
Solutions will be ordered and stocked in the smallest volume when possible.
4.
Expensive allergy extract (single patient use) and multidose vials for vaccines unavailable in
single-dose vial/syringe will expire per manufacturer's expiration date (i.e., meningococcal
vaccine and certain insulin solutions). Exceptions are: "Vial Open Expires..." stickers are
available through the Purchasing Department and should be used to document date opened and
expiration date. Lot number and manufacturers expiration date must not be occluded by sticker.
Exceptions are outlined in the compliance with the Connecticut DPH recommendations.
5.
Manufacturer recommendation must be followed for the storage of multidose vials/containers.
6.
Any exceptions must be approved by the Yale Health Center's Pharmacy and Therapeutic
Committee and Infection Control.

87
7.
Control testing solutions for CLIA waived tests (HCG, Strep A , glucose, ISTAT, Bianox, A1C,
etc.) are exempt from the monthly discard policy. The solutions are of known consistency and
deliver an expected result. Abnormal results result in removal from service of the testing
device/cartridges/strips. The solutions are not used in direct patient care but rather in calibration of
direct patient care devices. In all cases the manufacturer's instructions for use, retention and
discarding of testing solutions will be followed.
8.
Aseptic technique must be maintained when accessing multidose vials/containers.
9.
Sterile products must be accessed and prepared in areas functionally separate from general work
area.
10.
Eating and drinking must not be allowed in the prep area.
11.
Multidose vials/containers must be inspected for defects, manufacturers expiration date and
product integrity before use. If the product is defective or has expired, it MUST NOT BE USED.
Defective products should be promptly reported to Yale Health Center's Pharmacy.
12.
The rubber stopper of the container must be wiped with 70% alcohol before entry.
13.
Personnel should avoid touch contamination of sterile supplies.
Procedure:
1.
Identify patient, use 2 identifiers (name, DOB).
2.
Assess for allergies.
3.
Medication is verified against physician or PA order.
4.
Expiration date is checked.
5.
Medication is prepared and administered as per MD or PA order by the MD/PA/APRN/RN using
aseptic technique. (See Policy: Intra Articular Injections )
6.
All medication is discarded after single patient use.
88
APPENDIX Yale Health 2: Laundry
Standard:
Appropriate laundry procedures are followed to minimize potential nosocomial and
occupations risks associated with soiled linen.
Policy & Procedure:
A.
Collection
1.
Soiled linen will be collected in a manner that minimizes agitation to prevent
contamination of the environment and personnel and will be bagged at the site of
use.
2.
Linens are placed in white plastic bags. Linens are double bagged when leakage
onto the environment or contamination of transporting personnel is expected.
3.
All linen is transported to a collection area via linen carts located in the dirty
utility room. Laundry bags will not be overfilled to prevent mechanical
obstruction.
4.
In situations in which laundry is heavily soiled with blood or body fluids,
standard precautions will be followed.
B.
Transportation
1.
Soiled linen will be picked up daily in the morning, Monday, Wednesday and
Friday by Unitex Corporation.
2.
Clean linen is pressed, folded, and delivered to the fifth floor, Inpatient Care
Facility Monday, Wednesday and Friday. it is covered and wrapped for
protection. The laundry staff places laundry on the shelves of the linen closet, the
housekeeping staff assist in keeping the linen neat and monitor the cleanliness of
the closet.
C.
Linen Supply
1.
The Director of Nursing and/or the purchasing department, with the assistance of
the housekeeping department will maintain sufficient levels of linens for three (3)
times the licensed capacity of the facility.
D.
Infection Control
1.
Standard isolation procedures will be followed.
2.
The Infection Control Committee will monitor laundry procedures for
compliance with this policy.
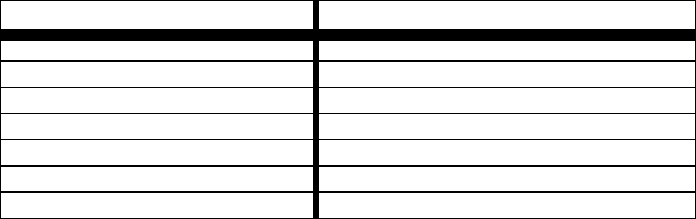
89
APPENDIX Yale Health 3: Clean Up Spills
Standard:
Clean-up of Spills with Potential for Staff and Patient Exposure to Bloodborne Pathogens.
Policy:
Provide a safe and clean environment for staff and patients while minimizing the risk of
exposure to bloodborne pathogens: for staff members assigned to decontaminate and clean
spills, and for patients and staff by the timely decontamination and clean-up of spills
posing a risk of exposure to bloodborne pathogens.
Procedure:
1.
Person discovering or receiving report of a spill must, immediately cover spill with
"Red Z", spray with Cavicide and cover spill utilizing supplies and directions located
in all spill kits (available through Building Services, Monday - Friday, 8:30a.m. -
5:00p.m.). Managers or persons responsible for ordering supplies should be sure
enough spill kits are readily available in their department.
2.
Clean-up of spills occurring in a clinic area are the responsibility of the personnel of
that specific clinic, utilizing the supplies and step-by-step directions located in the
spill kit.
3.
Contact Yale Health Building Services Emergency phone at 2-0276 to have the day
housekeeping staff continue the disinfecting process. Yale Health Day Housekeeping
Staff is available: Monday through Friday 7:30 a.m. to 5:00p.m., Saturday at 8:30 a.m.
and Sunday 8:30 a.m. to 5:00 p.m.
4.
Report Incident into the Report Tracker system.
5.
Spills occurring at any time in elevator interiors will be reported to the main desk.
The main desk personnel will shut down the elevator and notify the building Services
Manger of the spill.
6.
Cleaning up of spills occurring in a non-clinical area will be the responsibility of the
following departments for their respective floors, utilizing the supplies and step-by-
step directions located in the spill kit.
Non-Clinical Area
Responsible Department
Lower Level
Building Services
First Floor
Acute Care
Second Floor
Surgical Specialties
Third Floor
Pediatrics
Fourth Floor
Inpatient Care
Elevator Interiors
Building Services
90
7.
During weeknights 5:00p.m.to 12:00a.m., and weekend hours, Acute Care will be
responsible for any spills ocurring on the First floor and Inpatient Care will be
responsible for spills occurring on the Fourth floor. If a spill occurs on any other floor
during weeknights, 5:00p.m. to 8:30a.m. or weekends due to after hours clinic,
seminars, classes, or special arrangements to see a patient in a clinci area, the person
responsible for the clinic, seminar, class or provider seeing a patient is responsible for
the clean-up of any spill related to persons attending these sessions or patient seen after
hours. These spills must be decontaminated and cleaned up immediately, not left for
housekeeping upon their return to duty.
8.
Spill kits are available through Building Services and include all supplies and the
written protocol to be used in the clean-up of any spill with potential for exposure to
bloodborne pathogens. Be sure enough spill kits are available in your department
since Building Services is not accessible after 5:00p.m. on weekdays and is closed on
weekends/holidays.
9.
Assure that all members of your staff, including per diem, casual and off-hours staff,
with risk for exposure to bloodborne pathogens receive their annual bloodborne
Pathogens Training when yearly sessions are scheduled. These training sessions are
mandated by OSHA and address the issues required to afford staff members the
information they need to maintain a safe environment for both patients and employees
and proper handling of materials with potential for risk of exposure to bloodborne
pathogens. Training sessions are given throughout the year for all new Yale Health
employees.
10.
Assure that all staff members are instructed in the location and use of the spill kits and
spill protocol including all per diem, casual and off-hour staff.
91
APPENDIX Yale Health 4: Infection Control Protocol
Section II. Infection Control/Quality Assurance Rounds
Protocol and Procedure:
I.
Primary function is to measure compliance of each individual Yale Health Department to
the procedures and protocols outlined in the Yale Health Infection Control Manual and
Standards of Care.
A.
During unannounced walking rounds by the Infection Control Practitioner and
surveillance team, use a check list and document non-compliance.
B.
A form will be utilized to communicate any recommendations by the infection
control practitioner and surveillance team to the responsible Department
Manager/Chief to correct or improve department compliance.
C.
A form will be utilized by the responsible departmental staff to communicate to
the Infection Control Practitioner the action taken to improve or correct
compliance with set criteria.
II.
Surveillance Information is used as a teaching tool and guideline for responsible
departmental staff to meet and maintain compliance.
III.
The responsible departmental manager/chief will be sent a copy of the surveillance
information with the Infection Control Practitioner's recommended action for correction
of non-compliance, when appropriate, or comments. The responsible departmental
manager/chief will receive the completed report after the inspection is completed.
IV.
The responsible departmental manager/chief will respond in writing when cited for non-
compliance with set criteria. Infection Control Practitioner /Surveillance Team must
receive this response within two (2) weeks of date of report. The response must include
the department action taken to improve or correct the area of non-compliance cited. The
copy of the report sent by the Infection Control Practitioner /Surveillance Team includes
a column for department action. The responsible departmental manager/chief will utilize
this system for the department response.
V.
The surveillance team will re-visit a department cited for non-compliance following the
initial visit to assess action taken.
Non-compliance with the potential for serious risk of injury or safety to patients or staff
members will require immediate action and reassessment.

92
APPENDIX Yale Health 5: TB Exposures at Yale Health
Standard:
Yale Health will follow up on any potential exposure to infectious TB in our facility.
Procedure:
The following steps are to be taken if a case of active TB is diagnosed in the Yale Health patient
population.
1.
The clinician who diagnoses or who is first notified of the diagnosis of active TB in one
of their Yale Health patients must immediately notify the Infection Control practitioner
for the facility with the name of the patient, dates that patient was seen in the facility for
the evaluation of potential TB and names of any other clinicians or staff members known
to have contact with the patient during the visit.
2.
The Infection Control Practitioner will obtain the medical record of the index patient,
verify the diagnosis of active TB and begin a list of staff members that had contact with
the patient during the visits where the patient was symptomatic and/or diagnosed with
TB. The managers of any department involved in the care of the patient may need to be
consulted in order to identify additional exposed staff members. The chart will also be
reviewed to determine whether the appropriate infection control practices were used in
caring for the patient once the diagnosis of active TB was suspected. This review of the
infection control practices will be reported at the Infection Control committee. The
Infection control practitioner will report the index TB case to the State of Connecticut if
the diagnosis was made by a Yale Health clinician as per the Reportable Disease policy.
3.
The Infection Control Practitioner, in conjunction with the Chief of Employee Health will
inform all staff members who had contact with the index case that they need to have a
baseline ppd now (unless one has been placed within the past 3 months) and a follow up
ppd in 3 months time to identify any potential secondary cases. Any staff member who is
determined to have evidence of new TB infection as a result of this testing will be
evaluated as per the facility TB control plan. Any exposed staff who have a previous
history of a past positive ppd will notified to be alert and report any signs or symptoms
consistent with TB disease to employee health.
4.
The Infection Control practitioner will check the computerized department clinic
schedules for the days that the index patient was seen in the facility in the respective
department and begin a list of patients who were likely to have been in the waiting room
in close proximity to the index patient along with their primary providers.
5.
The Infection control staff and/or employee health staff will forward a notice to the
patients who may have been exposed to the index case to alert them of this fact and
recommend that they contact their primary physician for a ppd or evaluation. The primary
physicians will also be notified so that they will be aware of the case. If any exposed
patient subsequently is discovered to be infected with TB by way of a skin test
conversion, their primary physician will notify the Infection control and employee health
staff.
93
6.
At the end of the follow up period, the employee health chief will report to the Infection
Control committee about the outcome of the monitoring period including any evidence of
secondary spread of TB from the index case by identification of new ppd conversions.
7.
The Infection Control Committee will review the entire infection control practices
surrounding the case as well as the outcome from the monitoring period to document
adherence to the facility TB control plan and to make any recommendations for future
cases.
94
APPENDIX Yale Health 6: Universal Respiratory Etiquette
Standard:
Many respiratory pathogens are transmitted in health care settings (examples: influenza,
mycoplasma, coronaviruses, adenoviruses). Respiratory etiquette practices can decrease the rate
of transmission of these pathogens to patients, visitors, and staff.
Policy:
Yale Health will implement Universal Respiratory Etiquette practices in the clinical areas of the
facility.
Procedure:
1.
Patients and visitors with fever, cough or other respiratory symptoms will be offered a
surgical mask to wear while waiting for their health care appointments.
2.
Patients who have the above respiratory symptoms and cannot wear a surgical mask will be
advised to use a tissue to cover their nose or mouth while coughing or sneezing.
3.
Hand hygiene materials will be available in clinical waiting areas. Patients with respiratory
symptoms will be encouraged to perform frequent hand washing using these products.
4.
Clinical staff will be educated about respiratory hygiene and encouraged to wear surgical
masks when assessing patients who have respiratory symptoms. Clinical staff will perform
frequent hand washing when caring for patients with respiratory symptoms.
5.
Clinical managers will be responsible for ensuring that their respective departments keep the
supplies on hand in order to implement this respiratory etiquette policy.
95
APPENDIX Yale Health 7: Clinical Guidelines for Severe Acute Respiratory Syndrome -
Corona Virus (SARS CoV) Infection
The following guidelines should be used as clinical guidance for evaluating patients with
community-acquired illness for possible SARS-CoV Disease.
In the absence of SARS-CoV transmission anywhere in the world, the diagnosis of SARS-
CoV disease should be considered only in patients who require hospitalization for
radiographically confirmed pneumonia and who have an epidemiologic history that raises the
suspicion of SARS-CoV disease. The suspicion for SARS-CoV disease is raised if, within 10
days of symptom onset, the patient:
▪
Has a history of recent travel to mainland China, Hong Kong, or Taiwan (see Figure 1,
footnote 3) or close contact with ill persons with a history of recent travel to such areas,
or
▪
Is employed in an occupation at particular risk for SARS-CoV exposure, including a
healthcare worker with direct patient contact or a worker in a laboratory that contains live
SARS-CoV, or
▪
Is part of a cluster of cases of atypical pneumonia without an alternative diagnosis
Persons with such a clinical and exposure history should be evaluated for possible SARS CoV
disease as per CDC guidelines.
Once SARS-CoV transmission has been documented in the world, the diagnosis should still
be considered in patients who require hospitalization for pneumonia and who have the
epidemiologic history described above. In addition, all patients with fever or respiratory
symptoms should be questioned about whether within 10 days of symptom onset they have had:
▪
Close contact with someone suspected of having SARS-CoV disease, OR
▪
A history of foreign travel (or close contact with an ill person with a history of travel) to a
location with documented or suspected SARS-CoV, OR
▪
Exposure to a domestic location with documented or suspected SARS-CoV (including a
laboratory that contains live SARS-CoV), or close contact with an ill person with such an
exposure history.
Persons with such an exposure history should be evaluated for SARS-CoV disease according to
established CDC guidelines ( See CDC web site for most current guidelines)
See attached matrix for CDC recommendations for Outpatient Facilities.

96
Matrix 1: Recommendations for Inpatient Facilities and Emergency Departments
Level of SARS
activity
Suggested actions
No cases of SARS
in the facility
Triage activities/facility access controls
Notify the SARS coordinator or designee of any transfers from facilities that have SARS
cases.
In accordance with recommendations for respiratory hygiene/cough etiquette, instruct all
patients with respiratory illnesses to perform hand hygiene and cover the nose/mouth
when coughing or sneezing. Manage these patients with Droplet Precautions until
determined that they are not needed.
In the presence of person-to person SARS-CoV transmission in the world but no
known transmission in the area around the facility:
Place signs at all entry points detailing symptoms of and current epidemiologic risk
factors for SARS and directing persons meeting these criteria to an appropriate area for
evaluation.
Initiate screening of patients on entry to the emergency department for symptoms and
epidemiologic links suggesting SARS. Patients with fever or lower respiratory
symptoms and SARS risk factors should perform hand hygiene, wear a surgical mask (if
possible), and be isolated in accordance with the recommendations in Supplement I. If
airborne isolation is not possible, consider cohorting, with all patients wearing surgical
masks. Evaluate patients according to the algorithm (Figure 2) in Clinical Guidance on
the Identification and Evaluation of Possible SARS-CoV Disease among Persons
Presenting with Community-Acquired Illness
(www.cdc.gov/ncidod/sars/clinicalguidance.htm).
If a patient’s risk of exposure to SARS-CoV is high (e.g., close contact with a
laboratory-confirmed case of SARS-CoV disease), the clinical criteria should be
expanded to include other early symptoms of SARS-CoV disease.
In the presence of SARS-CoV transmission in the area around the facility:
All persons should perform hand hygiene on entry.
Actively screen all persons entering the facility for fever and lower respiratory
symptoms. All patients presenting with fever or lower respiratory symptoms should
perform hand hygiene, wear a surgical mask (if possible), and be isolated for SARS in
accordance with the recommendations in Supplement I. If airborne isolation is not
possible, consider cohorting, with all patients wearing surgical masks. Evaluate patients
according to the algorithm (Figure 2) in Clinical Guidance on the Identification and
Evaluation of Possible SARS-CoV Disease among Persons Presenting with Community-
Acquired Illness (www.cdc.gov/ncidod/sars/clinicalguidance.htm).
If a patient’s risk of exposure to SARS-CoV is high (e.g., close contact with a
laboratory-confirmed case of SARS-CoV disease), the clinical criteria should be
expanded to include other early symptoms of SARS-CoV disease.
Intake/triage staff should follow SARS infection control and PPE guidance, as specified
in Supplement I.
Limit visitors (e.g., one per patient per day).
Screen all visitors for SARS risk factors and symptoms.
Limit elective admissions and procedures.
Consider designating an area as a “SARS evaluation center” and sending all patients
presenting with fever or respiratory symptoms to the center for evaluation.

97
Matrix 1: Recommendations for Inpatient Facilities and Emergency Departments
(continued)
Level of SARS
activity
Suggested actions
No cases of SARS
in the facility
(continued)
Patient placement
In the presence of person-to-person SARS-CoV transmission in the world but NO
known transmission in the area around the facility:
Patients presenting with fever or lower respiratory symptoms and epidemiologic risk
factors for SARS should perform hand hygiene, wear a surgical mask (if possible), and
be isolated for SARS in accordance with the recommendations in Supplement I. If
airborne precautions are not possible, consider cohorting, with all patients wearing
surgical masks. Evaluate patients according to the algorithm (Figure 2) in Clinical
Guidance on the Identification and Evaluation of Possible SARS-CoV Disease among
Persons Presenting with Community-Acquired Illness
(www.cdc.gov/ncidod/sars/clinicalguidance.htm).
If a patient’s risk of exposure is high (e.g., close contact with a laboratory-confirmed
case of SARS-CoV disease), the clinical criteria should be expanded to include, in
addition to fever or lower respiratory symptoms, the other early symptoms of SARS-
CoV disease.
In the presence of person-to-person SARS-CoV transmission in the world but NO
known transmission in the area around the facility:
Patients presenting with fever or lower respiratory symptoms should perform hand
hygiene, wear a surgical mask (if possible), and be isolated in accordance with the
recommendations in Supplement I. If airborne isolation is not possible, consider
cohorting, with all patients wearing surgical masks. Evaluate patients according to the
algorithm (Figure 2) in Clinical Guidance on the Identification and Evaluation of
Possible SARS-CoV Disease among Persons Presenting with Community-Acquired
Illness (www.cdc.gov/ncidod/sars/clinicalguidance.htm).
If a patient’s risk of exposure is high (e.g., close contact with a laboratory-confirmed
case of SARS-CoV disease), the clinical criteria should be expanded to include, in
addition to fever or lower respiratory symptoms, the other early symptoms of SARS-
CoV disease.
3)
Designated personnel
Assign only selected, trained, and fit-tested emergency department staff to evaluate
possible SARS cases. Staff should follow SARS infection control and PPE guidance, as
specified in Supplement I.
4)
Surveillance
Depending on directives from local/state health departments, consider reporting of
patients requiring hospitalization for unexplained pneumonia who have risk factors for
SARS, as specified in Supplement B.
5)
Healthcare worker restrictions
Healthcare workers should notify the SARS coordinator at each facility where they work
and have at least daily symptom checks if:
They are caring for a SARS patient in another facility.
They are also working in another facility that has reported nosocomial SARS-CoV
transmission.
They have close contact with SARS patients outside the hospital.

98
Matrix 1: Recommendations for Inpatient Facilities and Emergency Departments
(continued)
Level of SARS
activity
Suggested actions
A few cases in the
facility, but all
cases are imported
(NO nosocomial
transmission)
Triage activities/facility access controls
Same as for “No cases of SARS in the facility.” Add:
No visitors to SARS patients unless necessary (e.g., parents, translators); visitors must
receive infection control training.
Designate specific SARS patient-flow routes (e.g., emergency department to designated
elevator to AIIR; AIIR to radiology).
Clean rooms housing SARS patients in accordance with current recommendations (see
Supplement I).
Patient placement
Same as for “No cases of SARS in the facility.” Add:
Place admitted known or potential SARS patients in AIIRs if available.
Consider cohorting admitted patients in private rooms on designated SARS units,
depending on personnel and availability of AIIRs. Modify designated floors/rooms as
possible.
Designated personnel
Same as for “No cases of SARS in the facility.” Add:
Assign only selected, trained, and fit-tested staff to SARS patient care (includes
designated ancillary personnel).
Assign a selected, trained, and fit-tested team with access to appropriate respiratory
protection (see Supplement I) for emergency resuscitation or respiratory procedures in
known or potential SARS patients.
Surveillance
Conduct active surveillance targeted to healthcare workers providing care to SARS
patients (e.g., symptom monitoring).
Healthcare worker restrictions
Same as for “No cases of SARS in the facility.” Add:
No eating or drinking in SARS patient-care areas.
Furlough healthcare workers with unprotected exposures to SARS patients during high-
risk procedures, and institute checks to evaluate possible symptoms.
Healthcare workers with other (non-high-risk) unprotected exposures to a SARS patient
should undergo checks for possible symptoms. Furlough of these workers could be
considered.

99
Matrix 1: Recommendations for Inpatient Facilities and Emergency Departments
(continued)
Level of SARS
activity
Suggested actions
A larger number of
SARS cases in the
facility OR
nosocomial
transmission with
all cases linked to a
clearly identified
source
Triage activities/access controls
Same as for “A few cases in the facility but all cases are imported.” Add:
Regardless of the level of SARS activity in the community around the facility:
Limit visitors (e.g., one per patient per day).
Maintain a log of all visitors to SARS patients to aid in contact tracing.
Limit elective admissions/procedures.
All healthcare workers and visitors should have a fever check and perform hand
hygiene on entry.
Patient placement
Same as for “A few cases in the facility but all cases are imported.” Add:
Designated personnel
Same as for “A few cases in the facility but all cases are imported.”
Surveillance
Implement active healthcare worker surveillance (symptom monitoring) throughout the
facility.
Monitor all healthcare worker absenteeism and illnesses (e.g., through the occupational
medicine clinic); evaluate for links to known SARS cases.
Monitor for and evaluate all new fevers and lower respiratory illnesses among patients.
Place any patient with unexplained fever or lower respiratory symptoms on SARS
precautions, and evaluate in accordance with the algorithm (Figure 2) in Clinical
Guidance on the Identification and Evaluation of Possible SARS-CoV Disease among
Persons Presenting with Community-Acquired Illness
(www.cdc.gov/ncidod/sars/clinicalguidance.htm).
If a patient’s risk of exposure is high (e.g., close contact with a laboratory-confirmed
case of SARS-CoV disease), the clinical criteria should be expanded to include, in
addition to fever or lower respiratory symptoms, the other early symptoms of SARS-
CoV disease.
Healthcare worker restrictions
Same as for “A few cases in the facility but all cases are imported.”

100
Matrix 1: Recommendations for Inpatient Facilities and Emergency Departments
(continued)
Level of SARS
activity
Suggested actions
Cases attributed to
nosocomial
transmission with
NO clearly
identified source
Triage activities/access controls
Same as for “A larger number of cases or linked transmission.” Add:
No visitors allowed in hospital unless necessary (e.g., parents, translators); visitors
must receive infection control training.
Close emergency department and facility to admissions and transfers.
Patient placement
Same as for “A larger number of cases or linked transmission.” Add:
Consider cohorting patients and staff to care for patients in the following categories:
Afebrile patients with no close SARS contact -- discharge as soon as medically
indicated
Afebrile patients with close SARS contact -- discharge as soon as medically indicated,
with contact restrictions and health department follow-up per recommendations in
Supplement D
Febrile or symptomatic patients not meeting case definition
Patients meeting case definition
Designated personnel
Same as for “A larger number of cases or linked transmission.” Add:
All persons in the facility should wear a surgical mask when not providing patient care
(this is not meant to serve as SARS PPE but to limit potential SARS-CoV transmission
from someone who develops SARS). When in contact with SARS patients, all persons
should continue to follow SARS infection control guidance and PPE as specified in
Supplement I.
Surveillance
Same as for “A larger number of cases or linked transmission.” Add:
Place any patient with new fever or lower respiratory illness (not just unexplained) on
SARS precautions and evaluate in accordance with the SARS clinical algorithm.
If a patient’s risk of exposure is high (e.g., close contact with a laboratory-confirmed
case of SARS-CoV disease), the clinical criteria should be expanded to include, in
addition to fever or lower respiratory symptoms, the other early symptoms of SARS-
CoV disease.
Healthcare worker restrictions
Same as for “A larger number of cases or linked transmission.” Add:
Depending on staffing issues, either:
Implement home/work restrictions for all healthcare workers in the facility, or
Restrict movement to work and home for all healthcare workers who worked in an
area of the facility where nosocomial transmission may have occurred.

101
Matrix 2: Recommendations for Outpatient Facilities/Areas
Level of SARS
activity
Suggested actions
No person-to-
person SARS
transmission
reported anywhere
in the world
Patient screening and precautions
In accordance with recommendations for respiratory hygiene/cough etiquette, instruct
all patients with symptoms of a respiratory infection to perform hand hygiene and
cover the nose/mouth. Manage these patients with Droplet Precautions until it is
determined that they are not needed. If there are likely to be delays in moving patients
out of the waiting area, consider dividing the area so that patients with respiratory
illnesses do not sit near others.
Healthcare worker precautions
Healthcare workers seeing patients with respiratory illness should use Droplet
Precautions.
During respiratory illness season, intake/triage staff should practice frequent hand
hygiene and could be given the option of wearing surgical masks.
Infrastructure issues
The facility will need a supply of waterless hand-hygiene products, surgical masks,
and other applicable PPE and will need to consider the logistics of implementing a
respiratory hygiene/cough etiquette strategy.

102
Matrix 2: Recommendations for Outpatient Facilities/Areas (continued)
Level of SARS
activity
Suggested actions
Presence of
person-to-person
SARS
transmission
worldwide but no
known
transmission in the
area around the
facility
Patient screening and precautions
Screen all patients and visitors with fever or lower respiratory symptoms for SARS
epidemiologic links (e.g., travel to endemic areas or contact with known cases).
Instruct anyone with fever or lower respiratory symptoms and epidemiologic risks for
SARS to wear a surgical mask (if tolerated) and to perform hand hygiene. Place these
patients immediately in a private room. Transfer these patients as soon as possible to a
facility where they can be isolated appropriately during the evaluation. Notify receiving
facilities that the patient is being sent for evaluation of SARS.
If a patient’s risk of exposure is high (e.g., close contact with a laboratory-confirmed
case of SARS-CoV disease), the clinical criteria should be expanded to include, in
addition to fever or lower respiratory symptoms, the other early symptoms of SARS-
CoV disease.
Manage outpatients in accordance with Clinical Guidance on the Identification and
Evaluation of Possible SARS-CoV Disease among Persons Presenting with Community-
Acquired Illness (www.cdc.gov/ncidod/sars/clinicalguidance.htm).
Healthcare worker precautions
Healthcare workers who are in direct contact with patients who might have SARS should
wear full SARS PPE (see Supplement I).
Infrastructure issues
The facility will need a supply of PPE (e.g., gowns, gloves, eye protection, respirators
[N-95 or higher level]).
Known
transmission in
the area around
the facility
1) Patient screening and precautions
Screen all patients and visitors for fever and lower respiratory symptoms both
when appointments are made and when they arrive at the clinic. Refer persons
with these symptoms to a facility where they can be isolated appropriately during
evaluation. Warn receiving facilities that the patient is being sent for evaluation
of SARS.
If a patient’s risk of exposure is high (e.g., close contact with a laboratory-
confirmed case of SARS-CoV disease), the clinical criteria should be expanded
to include, in addition to fever or respiratory symptoms, the other early
symptoms of SARS-CoV disease.
Healthcare worker precautions
Same as for “Person-to-person SARS transmission worldwide but no known
transmission in the area around the facility.”
Infrastructure issues
Same as for “Person-to-person SARS transmission worldwide but no known
transmission in the area around the facility.”

103
Matrix 3: Recommendations for Long-Term Care Facilities
Level of SARS
activity
Suggested actions
No person-to-
person SARS
transmission
reported anywhere
in the world
Patient precautions
In accordance with recommendations for respiratory hygiene/cough etiquette, patients
who develop symptoms of a respiratory infection should be placed on Droplet
Precautions until determined that they are not needed.
Healthcare worker precautions
Healthcare workers seeing patients with respiratory illness should use Droplet
Precautions and practice frequent hand hygiene.
Infrastructure issues
The facility will need supplies for Droplet Precautions (masks, gloves and gowns) and
hand hygiene.
Presence of
person-to-person
SARS
transmission
worldwide, but
no known
transmission in
the area around
the facility
Patient precautions
Same as for “No person-to-person SARS transmission reported anywhere in the
world.” Add:
Screen all potential admissions for symptoms and epidemiologic links to SARS.
Healthcare worker precautions
Same as for “No person-to-person SARS transmission reported anywhere in the
world.”
Infrastructure issues
Same as for “No person-to-person SARS transmission reported anywhere in the
world.”
Access controls
Visitors should be screened for symptoms and epidemiologic links to SARS
cases. Visitors with symptoms and epidemiologic links should not be allowed
into the facility.
Known
transmission in
the area around
the facility
1)
Patient precautions
Same as for “No person-to-person SARS transmission reported anywhere in the world.”
All new admissions should be evaluated at an acute-care facility (no direct admissions).
Patients with fever or lower respiratory symptoms should be evaluated according to the
algorithm (Figure 2) in Clinical Guidance on the Identification and Evaluation of
Possible SARS-CoV Disease among Persons Presenting with Community-Acquired
Illness (www.cdc.gov/ncidod/sars/clinicalguidance.htm) before being admitted. Patients
who are asymptomatic but had exposures should be observed for 10 days for the
development of symptoms before they are admitted.
If there is significant transmission in the community around the facility, initiate
surveillance for nosocomial lower respiratory illness, and transfer all patients who
develop such illness to an acute-care facility for evaluation. Acute-care facilities should
be notified that the patients are being transferred for evaluation of SARS.
2)
Healthcare worker precautions
Same as for “No person-to-person SARS transmission reported anywhere in the world.”
Healthcare workers should undergo symptom monitoring. Symptomatic healthcare
workers should be furloughed and evaluated according to the algorithm (Figure 2) in
Clinical Guidance on the Identification and Evaluation of Possible SARS-CoV Disease
among Persons Presenting with Community-Acquired Illness
(www.cdc.gov/ncidod/sars/clinicalguidance.htm).
3)
Infrastructure issues
4)
Access controls
Visitors should be actively screened for symptoms.
Visitors with symptoms should not be allowed into the facility.

104
APPENDIX Yale Health 8: Varicella Exposure at Yale Health
Standard:
Yale Health Center will prevent the spread of Varicella when it is diagnosed in a patient or staff
member.
Policy:
Yale Health Center staff will identify, report and use appropriate transmissions based precautions
and personal protective measures to prevent further transmission when a patient is diagnosed with
varicella in our facility.
Procedure:
1.
Patients who call with symptoms of fever and a pruritic vesicular rash should be referred to a
nurse or a CLINICIAN for phone triage. Obtain the name and telephone number of the
patient. Before advising them to come into the facility, Varicella should be considered as a
diagnosis. Please note that varicella requires airborne isolation.
a.
Patients with possible varicella who are severely ill or at risk for complications
(immunocompromised patients, pregnant women) should be referred to Yale-New
Haven Hospital (YNHH) for further evaluation and treatment. The ED at YNHH
should be notified so that the patient can be evaluated with the appropriate airborne
precautions.
b.
Patients who are not severely ill or at risk for complications should speak with a
clinician to make arrangements to have the patient come to the facility wearing a
surgical mask at a specific time or be given a surgical mask at the door. The
ambulance enters should be used. The patient should be immediately escorted into the
airborne isolation room in the Inpatient Care. The patient should only be cared for by
immune staff. If an advance notice is possible, please notify the charge nurse in the
Inpatient Care to confirm availability of the isolation room.
c.
If the patient is well enough to be discharged to home, they must be informed that they
are infectious until all lesions are crusted over (generally about 7 days) and that they
must stay out of work or school and avoid contact with anyone who is not immune to
Varicella.
e. If an undergraduate who lives in the dormitory is diagnosed with varicella, they may
not be sent back to the dormitory and should be offered admission to the isolation room
in the Inpatient Care if available. The policy Managing Students
With VaricellaChickenpox Or Other Potentially Serious Communicable
Diseases will be followed.
g. Any exam room used for a Varicella patient can be cleaned according to the regular
room cleaning procedure.
2.
The clinician who makes the diagnosis of varicella will notify the Infection Control
Practitioner, who will then report it to the State of Connecticut as per the Reportable Disease
policy. The Infection Control practitioner will review the infection control practices used in
caring for the index patient and report on this to the Infection Control committee. In off-
105
hours cases, the clinician of record for the case is responsible for instituting appropriate
Infection Control precautions.
3.
The Infection control practitioner will identify any staff members who were directly
exposed to the index patient and either contact each of them or consult the employee health
clinician to determine the staff members’ varicella immunity status.
4.
Any staff member who is determined not to have an immunity to varicella will be required to
get a varicella titer immediately under the direction of the employee health clinician. A staff
member with a history of the varicella vaccination only (not natural immunity) will also be
required to get a varicella titer.
5.
Any staff member whose varicella titer is negative will be placed on mandatory furlough or
removed from patient care from day 10 to 21(the incubation period) post exposure to the index
case to prevent possible varicella transmission to immunocompromised patients. At this time,
the staff member can be offered the varicella vaccination (up to 72 hrs post exposure) if not
previously vaccinated, which might help prevent a severe infection should they develop
varicella. If they develop varicella during this incubation period, they must report it to the
employee health department as well as notifying their primary provider to seek treatment. If
they do not develop varicella beyond the incubation period, they are unlikely to become ill
.Upon their return to duty, staff members who were not previously vaccinated should be
encouraged to receive the vaccine.
6.
Any exposed non –immune staff member who is immunocompromised or pregnant should
be evaluated for possible administration of varicella-zoster immune globulin by a clinician
with expertise in this area.
7.
The Infection Control practitioner will also determine a list of potential patient contacts who
may have shared the waiting room with the index case. The records of these patients will be
reviewed if available to determine if any of them were immunocompromised or currently
pregnant. All potentially exposed patients will be notified either by phone or letter if
unavailable, that they may have been exposed to varicella. The patients will be advised that if
they had a history of chicken pox, a positive varicella titer, or the varicella vaccine, they are
unlikely to become ill. They will be advised to contact their own doctor immediately if they
do not have a history of immunity, or if they are pregnant or immunocompromised. The
primary physicians of any identified immunocompromised or pregnant patient will also be
notified.
8.
An asymptomatic patient who worries about exposure can be seen to have a baseline
Varicella titer drawn and be offered the Varicella vaccine (if clinically appropriate).
9.
At the end of the incubation period (post day 21), the Infection control committee will
review the exposure history, along with any evidence of secondary transmission and review
the infection control practices to make any recommendations for handling of future cases.
106
APPENDIX Yale Health 9: PnP for Visitors to Inpatient Care
Standard:
Yale Health’s visitor policy balances the needs of patients and their families with heightened
awareness of infectious disease control.
Policy:
It is important to have a policy for visitors to the IC that both protects visitors from infectious
risks from patients and protects patients from infections that might be brought into the facility by
visitors.
Procedure:
1.
All visitors to patients in IC must check in at the nursing station before entering the patient’s
room. Visitors are encouraged to speak with the charge nurse for any questions or concerns.
2.
Visitors who are suffering from cold or flu symptoms or other illness that may be contagious
such as chicken pox, diarrhea, fever, cough, draining uncontained skin wounds, should refrain
from visiting patients in the IC so as not to transmit a potentially contagious illness to patients
who are already ill with other conditions. You should be free of any symptoms for 48 hours
before coming to IC.
3.
Visitors must observe all procedures related to transmission based precautions that pertain to
the patients with whom they are visiting. The nursing staff will instruct visitors on the steps to
observe the proper precautions including items such as the use of gowns, gloves, or masks, as
well as proper hand washing and respiratory etiquette.
4.
For patients on enhanced precautions, do not sit on the bed or use the patients’ toilets, share
patient toiletries, tissues, etc. or handle items of hospital equipment such as intravenous
tubing or drains.
5.
The nursing staff on duty and the administrators of Yale Health reserve the right to deny
visitors permission to visit if it is determined that the visitors pose a potential increased threat
of communicable disease, or if the visitors are unable or unwilling to follow the transmission
based precautions.
6.
Visitors may be asked to leave at any time if a patient’s condition is judged to be
deteriorating, if the patient is becoming fatigued or a clinical intervention is necessary.
107
APPENDIX Yale Health 10: PnP for Negative Pressure Rooms Inpatient Care and Use
Standard:
To provide a negative air pressure environment to safely care for persons requiring respiratory
isolation.
Policy:
Patients admitted to Inpatient Care who require respiratory isolation will be placed in one of the
two negative pressure rooms. Negative pressure will be maintained and monitored at all times.
Procedure:
1.
The Inpatient Care charge nurse is alerted to the admission of a patient requiring
respiratory isolation.
2.
The room, either 10 or 11, is checked for all appropriate furniture and equipment
required. Any unnecessary equipment is removed from the room.
3.
The door to the room is shut and appropriate the signage is placed on the door.
4.
The nurse will set the room to negative pressure by turning the key to the control switch
at the nurse's station.
5.
The monitoring box outside the room is checked by the nurse to assure negative pressure
is attained.
6.
After negative pressure is attained, the door is opened to test that the alarm sounds when
the pressure is no longer negative.
7.
The door is closed again and the nurse verifies that the pressure monitor goes back to the
negative and the alarm stops.
8.
Staff entering the room will open the door after donning PPE and will close the door
immediately after entering the room.
a.
Traffic in and out of the room will be held to a minimum.
b.
No visitors will be allowed unless they have been authorized by the attending
clinician, have been fit tested for a respirator, and have been instructed by staff
on the proper use of personal protective equipment (PPE).
9.
PPE will be removed by staff immediately after exiting the room and disposed of in the
designated waste container outside of the room. Staff will take care to avoid
contaminating themselves while removing the personal protective equipment and will
wash hands immediately upon completion of this step.
10.
When negative pressure rooms are in use, the pressure monitor outside the room will be
checked by the nurse hourly.

108
11.
If the negative pressure cannot be maintained, the patient will don an molded surgical
mask and will be transported to the hospital via AMR as soon as possible.
. The receiving facility as well as the ambulance services will be informed of the need to
use respiratory protection while caring for this patient.
12.
The patient will remain in the room for the duration of their inpatient stay. Only transport
within the building that is absolutely necessary for procedures will be authorized
and the patient will wear a molded surgical mask during any required transport.
The attending clinician can discontinue respiratory protection procedures after a
diagnosis is established that does not require these procedures or once the patient is
deemed noninfectious. Consultation with the Infection Control Staff or Medical Director
is encouraged if there is any doubt about continuation of respiratory isolation.
13.
Internal and external appointments for patients who are on isolation must be approved by
the attending clinician.
Attached: Negative Pressure Weekly Monitoring Log

109
APPENDIX Yale Health 11: Guidelines for the Infection Control management and Prevention
of Norovirus outbreaks
Noroviruses are the most common cause of epidemic gastroenteritis. These viruses are of
particular importance in gastroenteritis outbreaks in long term care and other health care settings
as well as the food service industry.
Noroviruses can cause gastroenteritis in patients of all ages. The incubation period is 12-48 hours
and symptoms are characterized by acute onset of diarrhea (usually nonbloody), vomiting, nausea
and abdominal cramps as well as occasional low grade fever and myalgias. Most cases resolve
without treatment in 1-3 days. The virus is shed in the stool and vomitus and peak shedding is for
2-5 days, although the virus can be detected for up to 4 weeks. Norovirus is extremely contagious
and is generally transmitted by person to person transmission, foodborne or waterborne
transmission. Indirect exposure by contaminated fomites has also been implicated.
The following guidelines from the CDC are recommended as a response to suspected norovirus
outbreaks and as prevention for the spread of the virus:
1.
Report suspected norovirus outbreaks (defined as an unusually large number of cases in a
patient population who either live or work in close proximity to each other) promptly to
Infection Control in order that an investigation can be started to attempt to identify the
source and prevent further transmission.
2.
Enforce good hand hygiene by washing hands with soap and running water for at least 20
seconds. Note that alcohol-based hand sanitizers may not be as effective in the setting of
norovirus outbreaks.
3.
Institute contact precautions for any patients admitted to the infirmary or when caring for
patients that might be incontinent or wearing diapers. In settings with widespread illness,
consider assigning exposed staff members only to care for patients admitted with
norovirus symptoms and re-assign non exposed staff to other patient areas.
4.
During times of widespread illness, visitors to the infirmary will be screened for
symptoms of gastrointestinal illness and not be admitted to the unit if they have
symptoms. Visitors to patients with norovirus symptoms will be kept to the minimal
number necessary for patient comfort and must adhere to strict contact precautions.
5.
Employees or students who are ill with a norovirus like illness will remain home for 48-
72 hours after symptom resolution.
6.
Environmental surfaces will be first cleaned to remove any soiled material and then
disinfected with either a 1:10 solution of bleach or the institutionally approved
disinfectant for norovirus.
7.
Attempt to collect specimens for testing from at least 5 acutely ill patients to test for
norovirus. (whole stool specimens can be sent for PCR testing)
8.
Report all suspected norovirus outbreaks to the local and state health departments using
our standard reportable disease policy and procedure.
110
APPENDIX Yale Health 12: Yale Health Procedure for Discontinuation of Airborne
Isolation for rule out Tuberculosis patients
1.
All suspected or known patients with tuberculosis who are admitted to the ICF must be
admitted to the airborne isolation room according to airborne transmission based
precautions outlined in the Infection Control manual.
2.
Airborne precautions may be discontinued when infectious TB disease is considered
unlikely and either 1) another diagnosis is made that explains the clinical syndrome or 2)
the patient has three consecutive, negative AFB sputum smear results. Each of the three
sputum specimens should be collected in 8–24-hour intervals, and at least one specimen
should be an early morning specimen.
Yale Health Infection Control Committee
