
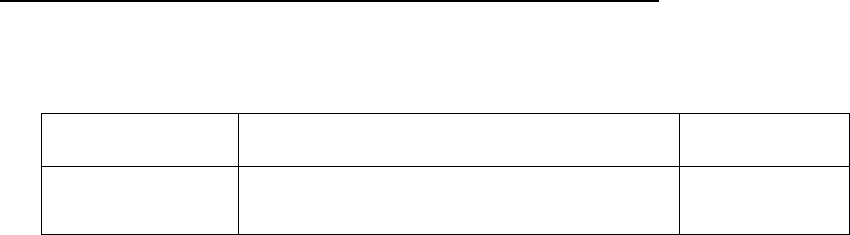
Medicare Claims Processing Manual
Chapter 32 – Billing Requirements for Special Services
Table of Contents
(Rev. 12683; Issued: 06-13-24)
Transmittals for Chapter 32
10- Diagnostic Blood Pressure Monitoring
10.1 - Ambulatory Blood Pressure Monitoring (ABPM) Billing Requirements
11 - Wound Treatments
11.1 – Electrical Stimulation
11.2 – Electromagnetic Therapy
11.3 – Autologous Platelet-Rich Plasma (PRP) for Chronic Non-Healing Wounds
11.3.1 – Policy
11.3.2 – Healthcare Common Procedure Coding System (HCPCS) Codes and
Diagnosis Coding
11.3.3 – Types of Bill (TOB)
11.3.5 - Place of Service (POS) for Professional Claims
11.3.6 – Medicare Summary Notices (MSNs), Remittance Advice Remark Codes
(RARCs), Claim Adjustment Reason Codes (CARCs) and Group Codes
12 - Counseling to Prevent Tobacco Use
12.1 - Counseling to Prevent Tobacco Use HCPCS and Diagnosis Coding
12.2 - Counseling to Prevent Tobacco Use A/B MAC (B) Billing Requirements
12.3 - A/B MAC (A) Billing Requirements
12.4 - Remittance Advice (RA) Notices
12.5 - Medicare Summary Notices (MSNs)
12.6 - Post-Payment Review for Counseling To Prevent Tobacco Use Services
12.7 - Common Working File (CWF) Inquiry
12.8 - Provider Access to Counseling To Prevent Tobacco Use Services Eligibility
Data
20 – Billing Requirements for Coverage of Kidney Disease Patient Education Services
20.1 – Additional Billing Requirements Applicable to Claims Submitted to Fiscal
Intermediaries (FIs)
20.2 - Healthcare Common Procedure Coding System (HCPCS) Procedure Codes and
Applicable Diagnosis Codes
20.3 - Medicare Summary Notices (MSNs) and Claim Adjustment Reason Codes
(CARCs)
20.4 - Advance Beneficiary Notice (ABN) Information
30 - Hyperbaric Oxygen (HBO) Therapy
30.1 – Billing Requirements for HBO Therapy for the Treatment of Diabetic Wounds
of the Lower Extremities
30.2 Hyperbaric Oxygen (HBO) Therapy (Section C, Topical Application of Oxygen)
40 – Sacral Nerve Stimulation
40.1 – Coverage Requirements
40.2 – Billing Requirements
40.2.1 – Healthcare Common Procedural Coding System (HCPCS)
40.2.2 – Payment Requirements for Test Procedures (HCPCS Codes 64585,
64590 and 64595)
40.2.3 – Payment Requirements for Device Codes A4290, E0752 and E0756
40.2.4 - Payment Requirements for Codes C1767, C1778, C1820, C1883 and
C1897
40.3 – Bill Types
40.4 – Revenue Codes
40.5 - Claims Editing
50 – Deep Brain Stimulation for Essential Tremor and Parkinson’s Disease
50.1 – Coverage Requirements
50.2 – Billing Requirements
50.2.1 – Part A Intermediary Billing Procedures
50.3 – Payment Requirements
50.3.1 - Part A Payment Methods
50.3.2 – Bill Types
50.3.3 – Revenue Codes
50.4 – Allowable Codes
50.4.1 – Allowable Covered Diagnosis Codes
50.4.2 - Allowable Covered Procedure Codes
50.4.3 – Healthcare Common Procedure Coding System (HCPCS)
50.5 – Ambulatory Surgical Centers
50.6 – Claims Editing for Intermediaries
50.7 – Remittance Advice Notice for A/B MACs (A)
50.8 – Medicare Summary Notices (MSN) Messages for Intermediaries
50.9 – Provider Notification
60 – Coverage and Billing for Home Prothrombin Time (PT/INR) Monitoring for Home
Anticoagulation Management
60.1 – Coverage Requirements
60.2 – Intermediary Payment Requirements
60.2.1 – Part A Payment Methods
60.3 – Intermediary Billing Procedures
60.3.1 – Bill Types
60.3.2 – Revenue Codes
60.4 – Intermediary Allowable Codes
60.4.1 – Allowable Covered Diagnosis Codes
60.4.2 – Healthcare Common Procedure Coding System (HCPCS) for
Intermediaries
60.5 – Carrier Billing Instructions
60.5.1 - HCPCS for Carriers
60.5.2 – Applicable Diagnosis Codes for A/B MACs (B)
60.6 – Carrier Claims Requirements
60.7 – Carrier Payment Requirements
60.8 – Carrier and Intermediary General Claims Processing Instructions
60.12 - Coverage for PET Scans for Dementia and Neurodegenerative Diseases
60.8.1 – Remittance Advice Notices
60.8.2 – Medicare Summary Notice (MSN) Messages
66 - National Coverage Determination (NCDs) services that are considered a
significant cost for Medicare Advantage.
66.1 – Institutional Billing for National Coverage Determination (NCDs)
services that are considered a significant cost for Medicare Advantage
66.2 – Services Identified as having Significant Cost for Medicare Advantage
67 - No Cost Claims
67.1 - Practitioner Billing for No Cost Items
67.2 - Institutional Billing for No Cost Items
67.2.1 - Billing No Cost Items Due to Recall, Replacement, or Free Sample
68 - Investigational Device Exemption (IDE) Studies
68.1 - Billing Requirements for Providers Billing for Routine Care Items and Services
in Category A IDE Studie
68.2 - Billing Requirements for Providers Billing for Category B IDE Devices and
Routine Care Items and Services in Category B IDE Studies
68.4 – Billing Requirements for Providers Billing Routine Costs of Clinical Trials
Involving a Category B IDE
69 - Qualifying Clinical Trails
69.1 - General
69.2 - Payment for Qualifying Clinical Trial Services
69.3 - Medical Records Documentation Requirements
69.4 - Local Medical Review Policy
69.5 - Billing Requirements - General
69.6 - Requirements for Billing Routine Costs of Clinical Trials
69.7 - Reserved for Future Use
69.8 - Handling Erroneous Denials of Qualifying Clinical Trial Services
69.9 - Billing and Processing Fee for Service Claims for Covered Clinical Trial
Services Furnished to Managed Care Enrollees
69.10 - CWF Editing Of Clinical Trial Claims For Managed Care Enrollees
69.11 - Resolution of CWF UR 5232 Rejects
70 - Billing Requirements for Islet Cell Transplantation for Beneficiaries in a National
Institutes of Health (NIH) Clinical Trial
70.1 - Healthcare Common Procedure Coding System (HCPCS) Codes for Carriers
70.2 - Applicable Modifier for Islet Cell Transplant Claims for Carriers
70.3 - Special Billing and Payment Requirements for Carriers
70.4 - Special Billing and Payment Requirements for A/B MACs (A)
70.5 - Special Billing and Payment Requirements Medicare Advantage (MA)
Beneficiaries
80 – Billing of the Diagnosis and Treatment of Peripheral Neuropathy with Loss of Protective
Sensation in People with Diabetes
80.1 - General Billing Requirements
80.2 - Applicable HCPCS Codes
80.3 - Diagnosis Codes
80.4 - Payment
80.5 - Applicable Revenue Codes
80.6 - Editing Instructions for A/B MACs (A)
80.7 - CWF General Information
80.8 - CWF Utilization Edits
90 - Stem Cell Transplantation
90.1 - General
90.2 - HCPCS and Diagnosis Coding - ICD-9-CM Applicable
90.2.1 - HCPCS and Diagnosis Coding for Stem Cell Transplantation - ICD-
10-CM Applicable
90.3 - Non-Covered Conditions
90.4 - Edits
90.5 - Suggested MSN and RA Messages
90.6 - Clinical Trials for Allogeneic Hematopoietic Stem Cell Transplantation
(HSCT) for Myelodysplastic Syndrome (MDS)
100 – Billing Requirements for Expanded Coverage of Cochlear Implantation
100.1 –A/B MACs (Part A) Billing Procedures
100.1.1 – Applicable Bill Types
100.1.2 – Special Billing Requirements for A/B MACs (A) for Inpatient
Billing
100.2 – A/B MACs (Part A) Payment Requirements
100.3 – A/B MACs (Part B) Billing Procedures
100.4 – Healthcare Common Procedural Coding System (HCPCS)
100.5 – Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark
Codes (RARCs), Group Codes, and Medicare Summary Notice (MSN) Messages
110 - Coverage and Billing for Ultrasound Stimulation for Nonunion Fracture Healing
110.1 - Coverage Requirements
110.2 - Intermediary Billing Requirements
110.3 - Bill Types
110.4 - Carrier and Intermediary Billing Instructions
110.5 - DMERC Billing Instructions
120 - Presbyopia-Correcting (P-C IOLS) and Astigmatism-Correcting Intraocular Lenses (A-
C IOLs) (General Policy Information)
120.1 - Payment for Services and Supplies
120.2 - Coding and General Billing Requirements
120.3 - Provider Notification Requirements
120.4 - Beneficiary Liability
130 - External Counterpulsation (ECP) Therapy
130.1 - Billing and Payment Requirements
130.2 - Special Intermediary Billing and Payment Requirements
140 140 - Cardiac Rehabilitation (CR) Programs,
Intensive Cardiac Rehabilitation (ICR) Programs, and
Pulmonary Rehabilitation (PR) Programs On or After
January 1, 2024
140.1 – CR Program Services Furnished On or Before Dec. 31, 2009
140.1.1 - Coding Requirements for CR Services Furnished On or Before Dec.
31, 2009
140.2 – – CR Program Services Effective for Dates of Service On or After January 1,
2024
140.2.1 – Coding Requirements for CR Services Furnished On or After
January 1, 2010
140.2.2 - Claims Processing Requirements for Cardiac Rehabilitation (CR) and
Intensive Cardiac Rehabilitation (ICR) Services Furnished On or After January
1, 2010
140.2.2.1 – Correct Place of Service (POS) Codes for CR and ICR
Services on Professional Claims
140.2.2.2 – Requirements for CR and ICR Services on Institutional
Claims
140.2.2.3 – Frequency Edits for CR and ICR Claims
140.2.2.4 – Edits for CR Services Exceeding 36 Sessions
140.2.2.5 – Edits for ICR Services Exceeding 126 Days and 72
Sessions
140.2.2.6 – Supplier Specialty Code 31 Requirements for ICR Claims
140.3 – ICR Program Services Effective for Dates of Service On or After January 1,
2024
140.3.1 – Coding Requirements for ICR Services Furnished On or After
January 1, 2010
140.4 – PR Program Services Effective for Dates of Service On or After January 1,
2024
140.4.1 – Coding Requirements for PR Services Furnished On or After
January 1, 2010
140.4.2 - Claims Processing Requirements for Pulmonary Rehabilitation (PR)
Services Furnished On or After January 1, 2010
140.4.2.1 – Correct Place of Service (POS) Codes for PR Services on
Professional Claims
140.4.2.2 – Requirements for PR Services on Institutional Claims
140.4.2.3 – Daily Frequency Edits for PR Claims
140.4.2.4 – Edits for PR Services Exceeding 36 Sessions
140.4.2.5 – Edits for PR Services Exceeding 72 Sessions
150 - Billing Requirements for Bariatric Surgery for Morbid Obesity
150.1 - General
150.2 - HCPCS Procedure Codes for Bariatric Surgery
150.3 - ICD Procedure Codes for Bariatric Surgery for Treatment of Co-Morbid
Conditions Related to Morbid Obesity (A/MACs only)
150.4 - ICD Diagnosis Codes for Bariatric Surgery
150.5 - ICD Diagnosis Codes for BMI ≥35
150.5.1 – ICD Codes for Type II Diabetes Mellitus Complication
150.6 - Claims Guidance for Payment
150.7 - Medicare Summary Notices (MSNs) and Claim Adjustment Reason Codes
150.8 - B/MAC Billing Requirements
150.9 - Advance Beneficiary Notice and HINN Information
160 – PTA for Implanting the Carotid Stent
160.1 – Category B Investigational Device Exemption (IDE) Study Coverage
160.2 – Post-Approval Study Coverage
160.2.1 – Carotid Artery Stenting (CAS) Post-Approval Extension Studies
160.3 – Carotid Artery Stenting (CAS) With Embolic Protection Coverage
160.4 – 510k Post-Approval Extension Studies using 510k-Cleared Embolic
Protection Devices during Carotid Artery Stenting (CAS) Procedures
161 - Intracranial PTA With Stenting
170 - Billing Requirements for Lumbar Artificial Disc Replacement
170.1 - General
170.2 - Carrier Billing Requirements
170.3 - A/B MAC (A) Billing Requirements
170.4 - Reasons for Denial and Medicare Summary Notice (MSN), Claim Adjustment
Reason Code Messages and Remittance Advice Remark Code
170.5 - Advance Beneficiary Notice (ABN and Hospital Issued Notice of
Noncoverage (HINN) Information
180 – Cryosurgery of the Prostate Gland
180.1 – Coverage Requirements
180.2 – Billing Requirements
180.3 – Payment Requirements
180.4 - Claim Adjustment Reason Codes, Remittance Advice Remark Codes, Group
Codes, and Medicare Summary Notice Messages
180.5 – Additional CWF and Contractor Requirements
190 – Billing Requirements for Extracorporeal Photopheresis
190.1 - Applicable Intermediary Bill Types
190.2 - Healthcare Common Procedural Coding System (HCPCS), Applicable
Diagnosis Codes and Procedure Code
190.3 - Medicare Summary Notices (MSNs), Remittance Advice Remark Codes
(RAs) and Claim Adjustment Reason Coded
190.4 - Advance Beneficiary Notice and Hospital Issued Notice of Noncoverage
Information
200 - Billing Requirements for Vagus Nerve Stimulation (VNS)
200.1 - General
200.2 - ICD-9 Diagnosis Codes for Vagus Nerve Stimulation (Covered since DOS on
and after July 1, 1999)
200.3 - Carrier/MAC Billing Requirements
200.4 - Fiscal Intermediary Billing Requirements
200.5 - Medicare Summary Notice (MSN), Remittance Advice Remark Code (RARC)
and Claims Adjustment Reason Code (CARC) Messages
200.6 - Advance Beneficiary Notice and HINN Information
210 – Billing Requirements for Continuous Positive Airway Pressure (CPAP) for Obstructive
Sleep Apnea (OSA)
220 – Billing Requirements for Thermal Intradiscal Procedures (TIPs) Claims
220.1 - General
220.2 - Contractors, A/B Medicare Administrative Contractors (MACs)
220.3 - Medicare Summary Notice (MSN), Claim Adjustment Reason Code (CARC),
and Remittance Advise Remark Code (RARC)
220.4 - Advanced Beneficiary Notice (ABN)
230 - Billing Wrong Surgical or Other Invasive Procedures Performed on a Patient, Surgical
or Other Invasive Procedures Performed on the Wrong Body Part, and Surgical or Other
Invasive Procedures Performed on the Wrong Patient
240 – Special Instructions for Certain Claims with a Gender/Procedure Conflict
240.1 - Billing Instructions for Institutional Providers
240.2 – Billing Instructions for Physicians and Non-Physician Practitioners
250 – Pharmacogenomic Testing for Warfarin Response
250.1 – Coverage Requirements
250.2 – Billing Requirements
250.3 – Payment Requirements
260 – Dermal Injections for Treatment of Facial Lipodystophy Syndrome (FLS)
260.1 – Policy
260.2 – Billing Instructions
260.2.1 – Hospital Billing Instructions
260.2.2. – Practitioner Billing Instructions
260.3 – Claims Processing System Editing
270 - Claims Processing for Implantable Automatic Defibrillators
270.1 - Coding Requirements for Implantable Automatic Defibrillators
270.2 - Billing Requirements for Patients Enrolled in a Data Collection System
280 – Autologous Cellular Immunotherapy Treatment of Metastatic Prostate Cancer
280.1 - Policy
280.2 – Healthcare Common Procedure Coding System (HCPCS) Codes and
Diagnosis Coding
280.3 - Types of Bill (TOB) and Revenue Codes
280.4 - Payment Method
280.5 - Medicare Summary Notices (MSNs), Remittance Advice Remark Codes
(RARCs), Claims Adjustment Reason Codes (CARCs), and Group Codes
290 - Transcatheter Aortic Valve Replacement (TAVR) Furnished on or After May 1, 2012
290.1 - Coding Requirements for TAVR Furnished on or After May 1, 2012, through
December 31, 2012
290.1.1- Coding Requirements for TAVR Services Furnished On or After January 1,
2013
290.2 - Claims Processing Requirements for TAVR Services on Professional Claims
290.3 - Claims Processing Requirements for TAVR Services on Inpatient Hospital
Claims
290.4 - Claims Processing Requirements for TAVR Services for Medicare Advantage
(MA) Plan Participants
300 - Billing Requirements for Ocular Photodynamic Therapy (OPT) with Verteporfin
300.1 - Coding Requirements for OPT with Verteporfin
300.2 - Claims Processing Requirements for OPT with Verteporfin Services on
Professional Claims and Outpatient Facility Claims
300.3 - Claims Processing Requirements for OPT with Verteporfin Services on
Inpatient Facility Claims
300.4 - Medicare Summary Notice (MSN) and Remittance Advice (RA)
Messages
310 - Transesophageal Doppler Used for Cardiac Monitoring
310.1 – Coding Requirements for Transesophageal Doppler Cardiac Monitoring
Furnished Before October 1, 2012
310.2 – Coding Requirements for Transesophageal Doppler Monitoring Furnished On
or After October 1, 2012
310.3 – Correct Place of Service (POS) Code for Transesophageal Doppler Cardiac
Monitor Services on Professional Claims
320 - Artificial Hearts and Related Devices
320.1 – Coding Requirements for Artificial Hearts Furnished Before May 1, 2008
320.2 – Coding Requirements for Artificial Hearts Furnished After May 1, 2008
320.3 – Ventricular Assist Devices (VADs)
320.3.1 – Postcardiotomy
320.3.2 – Bridge- to-Transplantation (BTT)
320.3.3 – Other
320.3.4 – Replacement Accessories and Supplies for External VADs or Any
VAD
330 – Percutaneous Image-guided Lumbar Decompression (PILD) for Lumbar Spinal
Stenosis (LSS)
330.1 – Claims Processing Requirements for Percutaneous Image-guided Lumbar
Decompression (PILD) for Lumbar Spinal Stenosis (LSS) on Professional Claims
330.2 - Claims Processing Requirements for PILD for Outpatient Facilities
340 – Transcatheter Mitral Valve Repair (TMVR)
340.1 – Coding Requirements for TMVR for Mitral Valve TEER Claims Furnished
on or After August 7, 2014
340.2 – Claims Processing Requirements for Mitral Valve TEER Services on
Professional Claims
340.3 - Claims Processing Requirements for Mitral Valve TEER Services on
Inpatient Hospital Claims
340.4 - Claims Processing Requirements for Mitral Valve TEER Services for
Medicare Advantage (MA) Plan Participants
350 - Emergency and Foreign Hospital Services
350.1 - Services Rendered By Nonparticipating Providers
350.2 - Establishing an Emergency
350.3 - Qualifications of an Emergency Services Hospital
350.4 - Coverage Requirements for Emergency Hospital Services Furnished Outside
of the United States
350.5 - Services Furnished in a Foreign Hospital Nearest to Beneficiary's U.S.
Residence
350.6 - Coverage of Physician and Ambulance Services Furnished Outside U.S.
350.7 - Claims for Services Furnished in Canada to Qualified Railroad Retirement
Beneficiaries
350.8 - Claims from Hospital-Leased Laboratories Not Meeting Conditions of
Participation
350.9 - Nonemergency Part B Medical and Other Health Services
350.10 - Elections to Bill for Services Rendered By Nonparticipating Hospitals
350.11 - Processing Claims
350.11.1 - Contractors Designated to Process Foreign Claims
350.11.2 - Contractor Processing Guidelines
350.11.3 - Medicare Approved Charges for Services Rendered in Canada or
Mexico
350.11.4 - Accessibility Criteria
350.11.5 - Medical Necessity
350.11.6 - Time Limitation on Emergency and Foreign Claims
350.11.7 - Payment Denial for Medicare Services Furnished to Alien
Beneficiaries Who Are Not Lawfully Present in the United States
350.12 - Appeals on Claims for Emergency and Foreign Services
360 - Payment for Services Received By Nonparticipating Providers
360.1 - Payment for Services from Foreign Hospitals
360.1.1 - Attending Physician's Statement and Documentation of Medicare
Emergency
360.2 - Designated Contractors
360.3 - Model Letters, Nonparticipating Hospital and Emergency Claims
360.3.1 - Model Letter to Nonparticipating Hospital That Elected to Bill For
Current Year
360.3.2 - Model Letter to Nonparticipating Hospital That Did Not Elect to Bill
for Current Year
360.3.3 - Model Letter to Nonparticipating Hospital That Requests to Bill the
Program
360.3.4 - Full Denial - Hospital-Filed or Beneficiary-Filed Emergency Claim
360.3.5 - Partial Denial - Hospital-Filed or Beneficiary-Filed Emergency
Claim
360.3.6 - Denial - Military Personnel/Eligible Dependents
360.3.7 - Full Denial - Shipboard Claim - Beneficiary filed
360.3.8 - Full Denial - Foreign Claim - Beneficiary Filed
370 - Microvolt T-wave Alternans (MTWA)
370.1 - Coding and Claims Processing for MTWA
370.2 - Messaging for MTWA
380--Leadless Pacemakers
380.1 - Leadless Pacemaker Coding and Billing Requirements for Professional
Claims
380.1.1 - Leadless Pacemaker Place of Service Restrictions
380.1.2 - Leadless Pacemaker Modifier
380.1.3 - Leadless Pacemaker Additional Claim Billing Information
380.2 - Leadless Pacemaker Claim Adjustment Reason Codes (CARC), Remittance
Advice Remark Codes (RARC) and Medicare Summary Notice (MSN) Messages
390 – Supervised exercise therapy (SET) of Symptomatic Peripheral Artery Disease
390.1 - General Billing Requirements
390.2 - Coding Requirements for SET
390.3 - Special Billing Requirements for Institutional Claims
390.4 - Common Working File (CWF) Requirements
390.5 - Applicable Medicare Summary Notice (MSN), Remittance Advice Remark
Codes (RARC) and Claim Adjustment Reason Code (CARC) Messaging
400 - Chimeric Antigen Receptor (CAR) T- cell Therapy
400.1 - Coverage Requirements
400.2 - Billing Requirements
400.2.1- A/B Medicare Administrative Contractor (MAC) (A) Bill Types
400.2.2 - A/B MAC (A) Revenue Codes
400.2.3 - A/B MAC Billing Healthcare Common Procedural Coding System
(HCPCS) Codes
400.2.3.1 – A/B MAC (B) Places of Service (POS)
400.2.4 - A/B MAC Diagnosis Requirements
400.2.5 – Billing Information for Professional Claims
400.3 - Payment Requirements
400.4 - Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes
(RARCs),Group Codes, and Medicare Summary Notice (MSN) Messages
400.5 - Claims Editing
410 - Acupuncture for Chronic Low Back Pain (cLBP)
410.1 - Coverage Requirements
410.2 - Claims Processing General Information
410.3 - Institutional Claims Bill Type and Revenue Coding Information
410.4 – Messaging
410.5 – Common Working File (CWF) Editing
411 – Home Infusion Therapy Services
411.1 – Policy
411.2 – Coverage Requirements
411.3 – Home Infusion Drugs: Healthcare Common Procedural Coding System
(HCPCS) Drug Codes
411.4 – Billing and Payment Requirements
411.5 – Return as Un-Processable, Claim Adjustment Reason Codes, Remittance
Advice Remark Codes, Group Codes, and Medicare Summary Notice Messages
411.6 – CWF and MCS Editing Requirements
412 - Monoclonal Antibodies Directed Against Amyloid for the Treatment of Alzheimer’s
Disease (AD)
412.1 - Coding Information
412.2 - Claim Processing Instructions
412.3 - Messaging

10 - Diagnostic Blood Pressure Monitoring
(Rev. 109, 02-27-04)
10.1 - Ambulatory Blood Pressure Monitoring (ABPM) Billing
Requirements
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
A. Coding Applicable to A/B MACs (A and B)
Effective April 1, 2002, a National Coverage Decision was made to allow for Medicare
coverage of ABPM for those beneficiaries with suspected "white coat hypertension"
(WCH). ABPM involves the use of a non-invasive device, which is used to measure blood
pressure in 24-hour cycles. These 24-hour measurements are stored in the device and are
later interpreted by a physician. Suspected "WCH" is defined as: (1) Clinic/office blood
pressure >140/90 mm Hg on at least three separate clinic/office visits with two separate
measurements made at each visit; (2) At least two documented separate blood pressure
measurements taken outside the clinic/office which are < 140/90 mm Hg; and (3) No
evidence of end-organ damage. ABPM is not covered for any other uses. Coverage policy
can be found in Medicare National Coverage Determinations Manual, Chapter 1, Part 1,
§20.19. (http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp).
The ABPM must be performed for at least 24 hours to meet coverage criteria. Payment is
not allowed for institutionalized beneficiaries, such as those receiving Medicare covered
skilled nursing in a facility. In the rare circumstance that ABPM needs to be performed
more than once for a beneficiary, the qualifying criteria described above must be met for
each subsequent ABPM test.
Effective dates for applicable Common Procedure Coding System (HCPCS) codes
for ABPM for suspected WCH and their covered effective dates are as follows:
HCPCS Definition Effective
Date
93784
ABPM, utilizing a system such as magnetic tape and/or
computer disk, for 24 hours or longer; including
recording, scanning analysis, interpretation and report.
04/01/2002
93786 ABPM, utilizing a system such as magnetic tape and/or
computer disk, for 24 hours or longer; recording only.
04/01/2002
93788 ABPM, utilizing a system such as magnetic tape and/or
computer disk, for 24 hours or longer; scanning analysis
with report.
01/01/2004
HCPCS Definition Effective
Date
93790
ABPM, utilizing a system such as magnetic tape and/or
computer disk, for 24 hours or longer; physician review
with interpretation and report.
04/01/2002

In addition, one of the following diagnosis codes must be present:
Diagnosis
Code
Description
If ICD-10-
CM
is
applicable
R03.0
Elevated blood pressure reading without diagnosis of
hypertension
B. A/B MAC (A) Billing Instructions
The applicable types of bills acceptable when billing for ABPM services are 13X, 23X,
71X, 73X, 75X, and 85X. Chapter 25 of this manual provides general billing instructions
that must be followed for bills submitted to A/B MACs (A). The A/B MACs (A) pay for
hospital outpatient ABPM services billed on a 13X type of bill with HCPCS 93786 and/or
93788 as follows: (1) Outpatient Prospective Payment System (OPPS) hospitals pay based
on the Ambulatory Payment Classification (APC); (2) non-OPPS hospitals (Indian Health
Services Hospitals, Hospitals that provide Part B services only, and hospitals located in
American Samoa, Guam, Saipan and the Virgin Islands) pay based on reasonable cost,
except for Maryland Hospitals which are paid based on a percentage of cost. Effective
4/1/06, type of bill 14X is for non-patient laboratory specimens and is no longer applicable
for ABPM.
The A/B MACs (A) pay for comprehensive outpatient rehabilitation facility (CORF)
ABPM services billed on a 75x type of bill with HCPCS code 93786 and/or 93788
based on the Medicare Physician Fee Schedule (MPFS) amount for that HCPCS code.
The A/B MACs (A) pay for ABPM services for critical access hospitals (CAHs) billed on a
85x type of bill as follows: (1) for CAHs that elected the Standard Method and billed
HCPCS code 93786 and/or 93788, pay based on reasonable cost for that HCPCS code; and
(2) for CAHs that elected the Optional Method and billed any combination of HCPCS
codes 93786, 93788 and 93790 pay based on reasonable cost for HCPCS 93786 and 93788
and pay 115% of the MPFS amount for HCPCS 93790.
The A/B MACs (A) pay for ABPM services for skilled nursing facility (SNF) outpatients
billed on a 23x type of bill with HCPCS code 93786 and/or 93788, based on the MPFS.
The A/B MACs (A) accept independent and provider-based rural health clinic (RHC) bills
for visits under the all-inclusive rate when the RHC bills on a 71x type of bill with revenue
code 052x for providing the professional component of ABPM services. The A/B MACs
(A) should not make a separate payment to a RHC for the professional component of
ABPM services in addition to the all-inclusive rate. RHCs are not required to use ABPM
HCPCS codes for professional services covered under the all-inclusive rate.
The A/B MACs (A) accept free-standing and provider-based federally qualified health
center (FQHC) bills for visits under the all-inclusive rate when the FQHC bills on a 73x
type of bill with revenue code 052x for providing the professional component of ABPM
services.
The A/B MACs (A) should not make a separate payment to a FQHC for the professional
component of ABPM services in addition to the all-inclusive rate. FQHCs are not required
to use ABPM HCPCS codes for professional services covered under the all-inclusive rate.
The A/B MACs (A) pay provider-based RHCs/FQHCs for the technical component of
ABPM services when billed under the base provider’s number using the above
requirements for that particular base provider type, i.e., a OPPS hospital based RHC would
be paid for the ABPM technical component services under the OPPS using the APC for
code 93786 and/or 93788 when billed on a 13x type of bill.
Independent and free-standing RHC/FQHC practitioners are only paid for providing the
technical component of ABPM services when billed to the A/B MAC (B) following the
MAC’s instructions.
•
A/B MAC (B) Claims
A/B MACs (B) pay for ABPM services billed with ICD-10-CM diagnosis code R03.0 (if
ICD-10 is applicable) and HCPCS codes 93784 or for any combination of 93786, 93788
and 93790, based on the MPFS for the specific HCPCS code billed.
•
Coinsurance and Deductible
The A/B MACs (A and B) shall apply coinsurance and deductible to payments for ABPM
services except for services billed to the A/B MAC (A) by FQHCs. For FQHCs only co-
insurance applies.
11 - Wound Treatments
(Rev 124a, 03-19-04)
11.1 - Electrical Stimulation
(Rev. 371, Issued 11-19-04, Effective: 04-01-05, Implementation: 04-04-05)
A. Coding Applicable to Carriers & Fiscal Intermediaries (FIs)
Effective April 1, 2003, a National Coverage Decision was made to allow for Medicare
coverage of Electrical Stimulation for the treatment of certain types of wounds. The type of
wounds covered are chronic Stage III or Stage IV pressure ulcers, arterial ulcers, diabetic
ulcers and venous stasis ulcers. All other uses of electrical stimulation for the treatment of
wounds are not covered by Medicare. Electrical stimulation will not be covered as an initial
treatment modality.
The use of electrical stimulation will only be covered after appropriate standard wound care
has been tried for at least 30 days and there are no measurable signs of healing. If electrical
stimulation is being used, wounds must be evaluated periodically by the treating physician but
no less than every 30 days by a physician. Continued treatment with electrical stimulation is
not covered if measurable signs of healing have not been demonstrated within any 30-day
period of treatment. Additionally, electrical stimulation must be discontinued when the
wound demonstrates a 100% epithelialzed wound bed.
Coverage policy can be found in Pub. 100-03, Medicare National Coverage Determinations
Manual, Chapter 1, Section 270.1
(http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp)
The applicable Healthcare Common Procedure Coding System (HCPCS) code for Electrical
Stimulation and the covered effective date is as follows:
HCPCS Definition Effective Date
G0281 Electrical Stimulation, (unattended), to one
or more areas for chronic Stage III and
04/01/2003

HCPCS Definition Effective Date
Stage IV pressure ulcers, arterial ulcers,
diabetic ulcers and venous stasis ulcers not
demonstrating measurable signs of healing
after 30 days of conventional care as part
of a therapy plan of care.
Medicare will not cover the device used for the electrical stimulation for the treatment of
wounds. However, Medicare will cover the service. Unsupervised home use of electrical
stimulation will not be covered.
B. FI Billing Instructions
The applicable types of bills acceptable when billing for electrical stimulation services are
12X, 13X, 22X, 23X, 71X, 73X, 74X, 75X, and 85X. Chapter 25 of this manual provides
general billing instructions that must be followed for bills submitted to FIs. FIs pay for
electrical stimulation services under the Medicare Physician Fee Schedule for a hospital,
Comprehensive Outpatient Rehabilitation Facility (CORF), Outpatient Rehabilitation Facility
(ORF), Outpatient Physical Therapy (OPT) and Skilled Nursing Facility (SNF).
Payment methodology for independent Rural Health Clinic (RHC), provider-based RHCs,
free-standing Federally Qualified Health Center (FQHC) and provider based FQHCs is made
under the all-inclusive rate for the visit furnished to the RHC/FQHC patient to obtain the
therapy service. Only one payment will be made for the visit furnished to the RHC/FQHC
patient to obtain the therapy service. As of April 1, 2005, RHCs/FQHCs are no longer
required to report HCPCS codes when billing for these therapy services.
Payment Methodology for a Critical Access Hospital (CAH) is on a reasonable cost basis
unless the CAH has elected the Optional Method and then the FI pays115% of the MPFS
amount for the professional component of the HCPCS code in addition to the technical
component.
In addition, the following revenues code must be used in conjunction with the HCPCS code
identified:
Revenue Code Description
420 Physical Therapy
430 Occupational Therapy
520 Federal Qualified Health Center *
521 Rural Health Center *
977, 978 Critical Access Hospital- method II
CAH professional services only
* NOTE: As of April 1, 2005, RHCs/FQHCs are no longer required to report HCPCS codes
when billing for these therapy services.
C. Carrier Claims

Carriers pay for Electrical Stimulation services billed with HCPCS codes G0281 based on the
MPFS. Claims for Electrical Stimulation services must be billed on Form CMS-1500 or the
electronic equivalent following instructions in chapter 12 of this manual
(http://www.cms.hhs.gov/manuals/104_claims/clm104c12.pdf).
D. Coinsurance and Deductible
The Medicare contractor shall apply coinsurance and deductible to payments for these therapy
services except for services billed to the FI by FQHCs. For FQHCs, only co-insurance
applies.
11.2 - Electromagnetic Therapy
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
A. HCPCS Coding Applicable to A/B MACs (A and B)
Effective July 1, 2004, a National Coverage Decision was made to allow for Medicare
coverage of electromagnetic therapy for the treatment of certain types of wounds. The type of
wounds covered are chronic Stage III or Stage IV pressure ulcers, arterial ulcers, diabetic
ulcers and venous stasis ulcers. All other uses of electromagnetic therapy for the treatment of
wounds are not covered by Medicare. Electromagnetic therapy will not be covered as an
initial treatment modality.
The use of electromagnetic therapy will only be covered after appropriate standard wound
care has been tried for at least 30 days and there are no measurable signs of healing. If
electromagnetic therapy is being used, wounds must be evaluated periodically by the treating
physician but no less than every 30 days. Continued treatment with electromagnetic therapy
is not covered if measurable signs of healing have not been demonstrated within any 30-day
period of treatment. Additionally, electromagnetic therapy must be discontinued when the
wound demonstrates a 100% epithelialzed wound bed.
Coverage policy can be found in Pub. 100-03, Medicare National Coverage Determinations
Manual, Chapter 1 section 270.1.
(http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp)
The applicable Healthcare Common Procedure Coding System (HCPCS) code for Electrical
Stimulation and the covered effective date is as follows:
HCPCS Definition Effective Date
G0329 ElectromagneticTherapy, to one or more
areas for chronic Stage III and Stage IV
pressure ulcers, arterial ulcers, diabetic
ulcers and venous stasis ulcers not
demonstrating measurable signs of healing
after 30 days of conventional care as part
of a therapy plan of care.
07/01/2004
Medicare will not cover the device used for the electromagnetic therapy for the treatment of
wounds. However, Medicare will cover the service. Unsupervised home use of
electromagnetic therapy will not be covered.
B. A/B MAC (A) Billing Instructions

The applicable types of bills acceptable when billing for electromagnetic therapy services are
12X, 13X, 22X, 23X, 71X, 73X, 74X, 75X, and 85X. Chapter 25 of this manual provides
general billing instructions that must be followed for bills submitted to A/B MACs (A). A/B
MACs (A) pay for electromagnetic therapy services under the Medicare Physician Fee
Schedule for a hospital, CORF, ORF, and SNF.
Payment methodology for independent (RHC), provider-based RHCs, free-standing FQHC
and provider based FQHCs is made under the all-inclusive rate for the visit furnished to the
RHC/FQHC patient to obtain the therapy service. Only one payment will be made for the
visit furnished to the RHC/FQHC patient to obtain the therapy service. As of April 1, 2005,
RHCs/FQHCs are no longer required to report HCPCS codes when billing for the therapy
service.
Payment Methodology for a CAH is payment on a reasonable cost basis unless the CAH has
elected the Optional Method and then the A/B MAC (A) pays pay 115% of the MPFS amount
for the professional component of the HCPCS code in addition to the technical component.
In addition, the following revenues code must be used in conjunction with the HCPCS code
identified:
Revenue Code Description
420 Physical Therapy
430 Occupational Therapy
520 Federal Qualified Health Center *
521 Rural Health Center *
977, 978 Critical Access Hospital- method II
CAH professional services only
* NOTE: As of April 1, 2005, RHCs/FQHCs are no longer required to report HCPCS codes
when billing for the therapy service.
C. A/B MAC (B) Claims
A/B MACs (B) pay for Electromagnetic Therapy services billed with HCPCS codes G0329
based on the MPFS. Claims for electromagnetic therapy services must be billed using the
ASC X12 837 professional claim format or Form CMS-1500 following instructions in chapter
12 of this manual (www.cms.hhs.gov/manuals/104_claims/clm104index.asp).
Payment information for HCPCS code G0329 will be added to the July 2004 update of the
Medicare Physician Fee Schedule Database (MPFSD).
D. Coinsurance and Deductible
The Medicare contractor shall apply coinsurance and deductible to payments for
electromagnetic therapy services except for services billed to the A/B MAC (A) by FQHCs.
For FQHCs only co-insurance applies.
11.3 – Autologous Platelet-Rich Plasma (PRP) for Chronic Non-Healing
Wounds
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)

11.3.1 – Policy
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)
Effective for claims with dates of service on or after April 13, 2021, contractors shall accept
and pay for autologous platelet-rich plasma (PRP) for the treatment of chronic non-healing
diabetic wounds for a duration of 20 weeks, when prepared by devices whose Food and Drug
Administration-cleared indications include the management of exuding cutaneous wounds,
such as diabetic ulcers, in accordance with the coverage criteria outlined in Publication 100-
03, chapter 1, section 270.3, of the National Coverage Determinations (NCD) Manual.
NOTE: Coverage of PRP services for the treatment of chronic non-healing diabetic wounds
that are performed more than 20 weeks after the date of the first PRP service shall be
determined by the local Medicare Administrative Contractor (MAC).
Coverage of autologous PRP for the treatment of all other chronic non-healing wounds (non-
diabetic) will be determined by local MACs under section 1862(a)(1)(A) of the Social
Security Act.
11.3.2 – Healthcare Common Procedure Coding System (HCPCS) Codes
and Diagnosis Coding
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)
Healthcare Common Procedure Coding System (HCPCS) Code
Effective for claims with dates of service on or after April 13, 2021, Medicare providers shall
report HCPCS code G0460 for PRP services for the treatment of chronic non-healing non-
diabetic wounds.
Effective for claims with dates of service on or after April 13, 2021, Medicare providers shall
report HCPCS code G0465 for PRP services for the treatment of chronic non-healing diabetic
wounds under the conditions and criteria outlined in NCD Manual Section 270.3.
If ICD-10 Diagnosis coding is applicable
For claims with dates of service on or after April 13, 2021, PRP, for the treatment of chronic
non-healing diabetic wounds must be billed reporting both an ICD-10 diagnosis code for
diabetes mellitus and an ICD-10 diagnosis code for chronic ulcers.
- Two diagnosis codes are required- Diabetic Mellitus plus Chronic Ulcer
Diabetes Mellitus
E08.621
Diabetes mellitus due to underlying condition with foot ulcer
E08.622
Diabetes mellitus due to underlying condition with other skin ulcer
E09.621
Drug or chemical induced diabetes mellitus with foot ulcer
E09.622
Drug or chemical induced diabetes mellitus with other skin ulcer
E10.621
Type 1 diabetes mellitus with foot ulcer
E10.622
Type 1 diabetes mellitus with other skin ulcer
E11.621
Type 2 diabetes mellitus with foot ulcer
E11.622
Type 2 diabetes mellitus with other skin ulcer
E13.621
Other specified diabetes mellitus with foot ulcer
E13.622
Other specified diabetes mellitus with other skin ulcer

Chronic Ulcer
L97.111
Non-pressure chronic ulcer of right thigh limited to breakdown of skin
L97.112
Non-pressure chronic ulcer of right thigh with fat layer exposed
L97.113
Non-pressure chronic ulcer of right thigh with necrosis of muscle
L97.115
Non-pressure chronic ulcer of right thigh with muscle involvement without evidence of
necrosis
L97.116
Non-pressure chronic ulcer of right thigh with bone involvement without evidence of
necrosis
L97.118
Non-pressure chronic ulcer of right thigh with other specified severity
L97.114
Non-pressure chronic ulcer of right thigh with necrosis of bone
L97.121
Non-pressure chronic ulcer of left thigh limited to breakdown of skin
L97.122
Non-pressure chronic ulcer of left thigh with fat layer exposed
L97.123
Non-pressure chronic ulcer of left thigh with necrosis of muscle
L97.124
Non-pressure chronic ulcer of left thigh with necrosis of bone
L97.125
Non-pressure chronic ulcer of left thigh with muscle involvement without evidence of
necrosis
L97.126
Non-pressure chronic ulcer of left thigh with bone involvement without evidence of necros
L97.128
Non-pressure chronic ulcer of left thigh with other specified severity
L97.211
Non-pressure chronic ulcer of right calf limited to breakdown of skin
L97.212
Non-pressure chronic ulcer of right calf with fat layer exposed
L97.213
Non-pressure chronic ulcer of right calf with necrosis of muscle
L97.214
Non-pressure chronic ulcer of right calf with necrosis of bone
L97.215
Non-pressure chronic ulcer of right calf with muscle involvement without evidence of
necrosis
L97.216
Non-pressure chronic ulcer of right calf with bone involvement without evidence of necros
L97.218
Non-pressure chronic ulcer of right calf with other specified severity
L97.221
Non-pressure chronic ulcer of left calf limited to breakdown of skin
L97.222
Non-pressure chronic ulcer of left calf with fat layer exposed
L97.223
Non-pressure chronic ulcer of left calf with necrosis of muscle
L97.224
Non-pressure chronic ulcer of left calf with necrosis of bone
L97.225
Non-pressure chronic ulcer of left calf with muscle involvement without evidence of necros
L97.226
Non-pressure chronic ulcer of left calf with bone involvement without evidence of necrosis
L97.228
Non-pressure chronic ulcer of left calf with other specified severity
L97.315
Non-pressure chronic ulcer of right ankle with muscle involvement without evidence of
necrosis
L97.316
Non-pressure chronic ulcer of right ankle with bone involvement without evidence of
necrosis
L97.318
Non-pressure chronic ulcer of right ankle with other specified severity
L97.321
Non-pressure chronic ulcer of left ankle limited to breakdown of skin
L97.322
Non-pressure chronic ulcer of left ankle with fat layer exposed
L97.323
Non-pressure chronic ulcer of left ankle with necrosis of muscle
L97.324
Non-pressure chronic ulcer of left ankle with necrosis of bone
L97.325
Non-pressure chronic ulcer of left ankle with muscle involvement without evidence of
necrosis
L97.326
Non-pressure chronic ulcer of left ankle with bone involvement without evidence of
necrosis
L97.328
Non-pressure chronic ulcer of left ankle with other specified severity
L97.411
Non-pressure chronic ulcer of right heel and midfoot limited to breakdown of skin
L97.412
Non-pressure chronic ulcer of right heel and midfoot with fat layer exposed
L97.413
Non-pressure chronic ulcer of right heel and midfoot with necrosis of muscle
L97.414
Non-pressure chronic ulcer of right heel and midfoot with necrosis of bone
L97.415
Non-pressure chronic ulcer of right heel and midfoot with muscle involvement without

evidence of necrosis
L97.416
Non-pressure chronic ulcer of right heel and midfoot with bone involvement without
evidence of necrosis
L97.418
Non-pressure chronic ulcer of right heel and midfoot with other specified severity
L97.421
Non-pressure chronic ulcer of left heel and midfoot limited to breakdown of skin
L97.422
Non-pressure chronic ulcer of left heel and midfoot with fat layer exposed
L97.423
Non-pressure chronic ulcer of left heel and midfoot with necrosis of muscle
L97.424
Non-pressure chronic ulcer of left heel and midfoot with necrosis of bone
L97.425
Non-pressure chronic ulcer of left heel and midfoot with muscle involvement
without evidence of necrosis
L97.426
Non-pressure chronic ulcer of left heel and midfoot with bone involvement
without evidence of necrosis
L97.428
Non-pressure chronic ulcer of left heel and midfoot with other specified severity
L98.411
Non-pressure chronic ulcer of buttock limited to breakdown of skin
L98.412
Non-pressure chronic ulcer of buttock with fat layer exposed
L98.413
Non-pressure chronic ulcer of buttock with necrosis of muscle
L98.414
Non-pressure chronic ulcer of buttock with necrosis of bone
L98.415
Non-pressure chronic ulcer of buttock with muscle involvement without evidence of necros
L98.416
Non-pressure chronic ulcer of buttock with bone involvement without evidence of necrosis
L98.418
Non-pressure chronic ulcer of buttock with other specified severity
L98.421
Non-pressure chronic ulcer of back limited to breakdown of skin
L98.422
Non-pressure chronic ulcer of back with fat layer exposed
L98.423
Non-pressure chronic ulcer of back with necrosis of muscle
L98.424
Non-pressure chronic ulcer of back with necrosis of bone
L98.425
Non-pressure chronic ulcer of back with muscle involvement without evidence of necrosis
L98.426
Non-pressure chronic ulcer of back with bone involvement without evidence of necrosis
L98.428
Non-pressure chronic ulcer of back with other specified severity
L98.491
Non-pressure chronic ulcer of skin of other sites limited to breakdown of skin
L98.492
Non-pressure chronic ulcer of skin of other sites with fat layer exposed
L98.493
Non-pressure chronic ulcer of skin of other sites with necrosis of muscle
L98.494
Non-pressure chronic ulcer of skin of other sites with necrosis of bone
Frequency Requirements:
Effective for claims with dates of service on and after April 13, 2021, contractors shall cover
PRP services for chronic non-healing diabetic wounds, G0465, for a maximum of 20 weeks
beginning with the first week of treatment.
Effective for claims with dates of services on or after April 13, 2021, the local MACs shall
have discretion to pay PRP services for chronic non-healing diabetic wounds, G0465, that are
performed more than 20 weeks after the date of the first PRP service when the -KX modifier
is reported on the claim.
Effective for claims with dates of service on and after April 13, 2021, contractors shall have
discretion to cover, and determine frequency for, PRP services for chronic non-healing non-
diabetic wounds, G0460.
11.3.3 – Types of Bill (TOB)
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)
11.3.4 – Payment Method
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)
Payment for PRP services is as follows:
• Hospital outpatient departments TOBs 12X and 13X – based on the Outpatient
Prospective Payment System
• Skilled Nursing Facility TOBs 22X and 23X – based on the Medicare Physician Fee
Schedule (MPFS)
• TOB 71X – based on the all-inclusive rate
• TOB 75X – based on the MPFS
• TOB 77X – based on the all-inclusive rate
• TOB 85X – based on reasonable cost
• Critical Access Hospitals TOB 85X and revenue codes 096X, 097X, or 098X – based
on the MPFS
Local MACs shall pay for PRP services for hospitals in Maryland under the jurisdiction of the
Health Services Cost Review Commission on an outpatient basis, TOB 13X, in accordance
with the terms of the Maryland waiver.
11.3.5 - Place of Service (POS) for Professional Claims
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)
Effective for claims with dates of service on or after August 2, 2012, place of service (POS) codes
11, 22, and 49 shall be used for PRP services.
Effective for claims with dates of service on or after April 13, 2021, POS codes 11, 19, 22, and 49
shall be used for PRP services.
11.3.6 – Medicare Summary Notices (MSNs), Remittance Advice Remark
Codes (RARCs), Claim Adjustment Reason Codes (CARCs) and Group
Codes
(Rev. 11214, Issued: 01-20-22, Effective:04-13-21, Implementation: 01-03-22 Shared
Systems Contractors, 02-14-22 MACs)
Contractors shall deny claims for PRP services when provided on other than TOBs 12X, 13X,
22X, 23X, 71X, 75X, 77X, and 85X using:
MSN 21.25 - “This service was denied because Medicare only covers this service in certain
settings.”
Spanish Version - “El servicio fue denegado porque Medicare solamente lo cubre en ciertas
situaciones.”
CARC 58 - “Treatment was deemed by the payer to have been rendered in an inappropriate or
invalid place of service. NOTE: Refer to the 832 Healthcare Policy Identification Segment
(loop 2110 Service payment Information REF), if present.
RARC N428 - “Service/procedure not covered when performed in this place of service.”
Group Code - CO (Contractual Obligation)

Contractors shall reject claims for PRP services for the treatment of chronic non-healing
diabetic wounds, G0465, that are performed more than 20 weeks after the date of the first
PRP service when the --KX modifier is NOT included on the claim using the following
messages:
CARC 119 – Benefit Maximum for this time period or occurrence has been reached.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An
NCD provides a coverage determination as to whether a particular item or service is covered.
A copy of this policy is available www.cms.gov/mcd/search.asp. If you do not have web
access, you may contact the contractor to request a copy of the NCD.
Medicare Summary Notice (MSN) 20.5 – These services cannot be paid because your
benefits are exhausted at this time.
Spanish Version: “Estos servicios no pueden ser pagados porque sus beneficios se han
agotado.”
Group Code – CO (Contractual Obligation)
Contractors shall deny/reject claims for PRP services for the treatment of chronic non-healing
diabetic wounds, G0465, that don’t contain the appropriate diagnosis codes as noted above
and use the following messages:
Claim Adjustment Reason Code (CARC) 50 - These are non-covered services because this is
not deemed a 'medical necessity' by the payer.
Remittance Advice Remark Code (RARC) N386 - This decision was based on a National
Coverage Determination (NCD). An NCD provides a coverage determination as to whether a
particular item or service is covered. A copy of this policy is available at:
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor
to request a copy of the NCD.
Medicare Summary Notice (MSN) 15.19 - “We used a Local Coverage Determination (LCD)
to decide coverage for your claim. To appeal, get a copy of the LCD at
www.cms.gov/medicare-coverage-database (use the MSN Billing Code for the CPT/HCPCS
Code) and send with information from your doctor."
Spanish Version -Usamos una Determinación de Cobertura Local (LCD) para decidir la
cobertura de su reclamo. Para apelar, obtenga una copia del LCD en www.cms.gov/medicare-
coverage-database (use el código de facturación de MSN para el código "CPT/HCPCS") y
envíela con la información de su médico.
MSN 15.20 - “The following polices were used when we made this decision: NCD 270.3.”
Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión:
NCD 270.3.”
NOTE: Due to system requirement, the Fiscal Intermediary Shared System (FISS) has
combined messages 15.19 and 15.20 so that, when used for the same line item, both messages
will appear on the same MSN.
Group Code – Contractual Obligation (CO).
12 - Counseling to Prevent Tobacco Use
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
Background: Effective for services furnished on or after March 22, 2005, a National Coverage
Determination (NCD) provided for coverage of smoking and tobacco-use cessation
counseling services located at Medicare National Coverage Determinations Manual,
Publication 100-03 section 210.4. CMS established a related policy entitled Counseling to
Prevent Tobaccos Use at NCD Manual 210.4.1 effective August 25, 2010. However,
effective September 30, 2016, the conditions of Medicare Part A and Medicare Part B
coverage for smoking and tobacco-use cessation counseling services (210.4) were deleted.
The remaining NCD entitled Counseling to Prevent Tobacco Use (210.4.1), remains in effect,
along with HCPCS codes 99406 and 99407, specifically payable for counseling to prevent
tobacco use effective October 1, 2016.
12.1 - Counseling to Prevent Tobacco Use HCPCS and Diagnosis Coding
(Rev. 4237, Issued: 02-08- 19, Effective: 03-12- 19, Implementation: 03-12-19)
The following HCPCS codes should be reported when billing for counseling to prevent
tobacco use services:
99406 - Smoking and tobacco-use cessation counseling visit; intermediate, greater than 3
minutes up to 10 minutes
99407 - Smoking and tobacco-use cessation counseling visit; intensive, greater than 10
minutes
Note the above codes were effective for dates of service on or after January 1, 2008, and
specifically effective for counseling to prevent tobacco use claims on or after October 1,
2016.
Contractors shall allow payment for a medically necessary E/M service on the same day as
the counseling to prevent tobacco use service when it is clinically appropriate. Physicians
and qualified non-physician practitioners shall use an appropriate HCPCS code, such as
HCPCS 99201– 99215, to report an E/M service with modifier 25 to indicate that the E/M
service is a separately identifiable service from 99406 or 99407.
Contractors shall only pay for 8 counseling to prevent tobacco use sessions in a 12-month
period. The beneficiary may receive another 8 sessions during a second or subsequent year
after 11 full months have passed since the first Medicare covered counseling session was
performed. To start the count for the second or subsequent 12-month period, begin with the
month after the month in which the first Medicare covered counseling session was performed
and count until 11 full months have elapsed.
Claims for counseling to prevent tobacco use services shall be submitted with an appropriate
diagnosis code.
NOTE: This decision does not modify existing coverage for minimal cessation counseling
(defined as 3 minutes or less in duration) which is already considered to be covered as part of
each Evaluation and Management (E/M) visit and is not separately billable.
Claims for counseling to prevent tobacco use services shall be submitted with an applicable
diagnosis code:
ICD-9-CM (prior to October 1, 2015)
V15.82, personal history of tobacco use, or
305.1, non-dependent tobacco use disorder
989.84, toxic effect of tobacco
ICD-10-CM (effective October 1, 2015)
F17.210, nicotine dependence, cigarettes, uncomplicated,
F17.211, nicotine dependence, cigarettes, in remission,
F17.213 Nicotine dependence, cigarettes, with withdrawal
F17.218 Nicotine dependence, cigarettes, with other nicotine-induced disorders
F17.219 Nicotine dependence, cigarettes, with unspecified nicotine-induced disorders
F17.220, nicotine dependence, chewing tobacco, uncomplicated,
F17.221, nicotine dependence, chewing tobacco, in remission,
F17.223 Nicotine dependence, chewing tobacco, with withdrawal
F17.228 Nicotine dependence, chewing tobacco, with other nicotine-induced disorders
F17.229 Nicotine dependence, chewing tobacco, with unspecified nicotine-induced disorders
F17.290, nicotine dependence, other tobacco product, uncomplicated,
F17.291, nicotine dependence, other tobacco product, in remission, or
F17.293 Nicotine dependence, other tobacco product, with withdrawal
F17.298 Nicotine dependence, other tobacco product, with other nicotine-induced disorders
F17.299 Nicotine dependence, other tobacco product, with unspecified nicotine-induced
disorders
Z87.891, personal history of nicotine dependence, unspecified, uncomplicated.
T65.211A, Toxic effect of chewing tobacco, accidental (unintentional), initial encounter
T65.212A, Toxic effect of chewing tobacco, intentional self-harm, initial encounter
T65.213A, Toxic effect of chewing tobacco, assault, initial encounter
T65.214A, Toxic effect of chewing tobacco, undetermined, initial encounter
T65.221A, Toxic effect of tobacco cigarettes, accidental (unintentional), initial encounter
T65.222A, Toxic effect of tobacco cigarettes, intentional self-harm, initial encounter
T65.223A, Toxic effect of tobacco cigarettes, assault, initial encounter
T65.224A, Toxic effect of tobacco cigarettes, undetermined, initial encounter
T65.291A, Toxic effect of other tobacco and nicotine, accidental (unintentional), initial
encounter
T65.292A, Toxic effect of other tobacco and nicotine, intentional self-harm, initial encounter
T65.293A, Toxic effect of other tobacco and nicotine, assault, initial encounter
T65.294A, Toxic effect of other tobacco and nicotine, undetermined, initial encounter
12.2 - Counseling to Prevent Tobacco Use A/B MAC (B) Billing
Requirements
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
A/B MACs (B) shall pay for counseling to prevent tobacco use services billed with codes
99406 and 99407 for dates of service on or after October 1, 2016 A/B MACs (B) shall pay for
counseling services billed with codes G0436 and G0437 for dates of service on and after
August 25, 2010, through September 30, 2016. The type of service (TOS) for each of the
new codes is 1.
A/B MACs (B) pay for these services billed based on the Medicare Physician Fee Schedule
(MPFS). Deductible and coinsurance are waived. Claims from physicians or other providers
where assignment was not taken are subject to the Medicare limiting charge, which means
that charges to the beneficiary may be no more than 115% of the allowed amount.

Physicians or qualified non-physician practitioners shall bill the A/B MAC (B) for counseling
to prevent tobacco use services using the ASC X12 837 professional claim format or the
Form CMS-1500.
12.3 - A/B MAC (A) Billing Requirements
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
The A/B MACs (A) shall pay for counseling to prevent tobacco use services with codes
99406 and 99407 for dates of service on or after October 1, 2016. A/B MACs (A) shall pay
for counseling services billed with codes G0436 and G0437 for dates of service on or after
August 25, 2010, through September 30, 2016. Deductible and coinsurance are waived.
A. Claims for counseling to prevent tobacco use services should be submitted using the
ASC X12 837 institutional claim format or Form CMS-1450.
The applicable bill types are 12X, 13X, 22X, 23X, 34X, 71X, 77X, 83X, and 85X. Effective
April 1, 2006, type of bill 14X is for non-patient laboratory specimens and is no longer
applicable for counseling to prevent tobacco use services.
Applicable revenue codes are as follows:
Provider Type
Revenue Code
Rural Health Centers (RHCs)/Federally Qualified Health Centers
(FQHCs)
052X
Indian Health Services (IHS)
0510
Critical Access Hospitals (CAHs) Method II
096X, 097X,
098X
All Other Providers
0942
NOTE: When these services are provided by a clinical nurse specialist in the RHC/FQHC
setting, they are considered “incident to” and do not constitute a billable visit.
Payment for outpatient services is as follows:
Type of Facility
Method of Payment
Rural Health Centers (RHCs)
All-inclusive rate (AIR) for the encounter
Federally Qualified Health
Centers (FQHCs)
FQHC Prospective Payment System (PPS) for the
encounter
Indian Health Service
(IHS)/Tribally owned or
operated hospitals and hospital-
based facilities
AIR
IHS/Tribally owned or operated
non-hospital-based facilities
Medicare Physician Fee Schedule (MPFS)
IHS/Tribally owned or operated
Critical Access Hospitals
(CAHs)
Facility Specific Visit Rate
Hospitals subject to the
Outpatient Prospective Payment
System (OPPS)
Ambulatory Payment Classification (APC)
Hospitals not subject to OPPS
Payment is made under current methodologies

Skilled Nursing Facilities
(SNFs)
NOTE: Included in Part A PPS
for skilled patients.
MPFS
Home Health Agencies (HHAs)
MPFS
Critical Access Hospitals
(CAHs)
Method I: Technical services are paid at 101% of
reasonable cost. Method II: technical services are paid at
101% of reasonable cost, and Professional services are
paid at 115% of the MPFS Data Base
Maryland Hospitals
Payment is based according to the Health Services Cost
Review Commission (HSCRC). That is 94% of
submitted charges subject to any unmet deductible,
coinsurance, and non-covered charges policies.
NOTE: Inpatient claims submitted with counseling to prevent tobacco use services are
processed under the current payment methodologies. In addition, payment is not allowed for
inpatients whose primary diagnosis is counseling to prevent tobacco use.
12.4 - Remittance Advice (RA) Notices
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
Contractors shall use the appropriate claim RA(s) when denying payment for counseling to
prevent tobacco use services.
The following messages are used where applicable:
• If the counseling services were furnished before August 25, 2010, use an appropriate RA
claim adjustment reason code (CARC), such as, 26, “Expenses incurred prior to
coverage.”
• If the claim for counseling services is being denied because the coverage criteria are
not met, use an appropriate CARC, such as, 272, Coverage/program guidelines were
not met.
• If the claim for counseling services is being denied because the maximum benefit has
been reached, use an appropriate CARC, such as, 119, “Benefit maximum for this
time period or occurrence has been reached.”
12.5 - Medicare Summary Notices (MSNs)
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
(When denying claims for counseling to prevent tobacco use services that were performed
prior to the effective date of coverage, contractors shall use an appropriate MSN, such as,
MSN 21.11, “This service was not covered by Medicare at the time you received it.”
When denying claims for counseling services on the basis that the coverage criteria were not
met, use an appropriate MSN, such as MSN 21.21, “This service was denied because
Medicare only covers this service under certain circumstances.”
When denying claims for counseling services that have dates of service exceeding the
maximum benefit allowed, use an appropriate MSN, such as MSN 17.8, “Payment is denied
because the maximum benefit allowance has been reached.”
12.6 - Post-Payment Review for Smoking and Tobacco-Use Cessation
Counseling Services
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
As with any claim, Medicare may decide to conduct post-payment reviews to determine that
the services provided are consistent with coverage instructions. Providers must keep patient
record information on file for each Medicare patient for whom a counseling claim is made.
These medical records can be used in any post-payment reviews and must include standard
information along with sufficient patient histories to allow determination that the steps
required in the coverage instructions were followed.
12.7 - Common Working File (CWF) Inquiry
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's
Medicare identification number. For purposes of this manual, Medicare beneficiary identifier
references both the Health Insurance Claim Number (HICN) and the Medicare Beneficiary
Identifier (MBI) during the new Medicare card transition period and after for certain business
areas that will continue to use the HICN as part of their processes.
The Common Working File (CWF) maintains the number of counseling sessions rendered to
a beneficiary. By entering the beneficiary’s Medicare beneficiary identifier, providers have
the capability to view the number of sessions a beneficiary has received for this service via
inquiry through CWF.
12.8 - Provider Access to Smoking and Tobacco-Use Cessation Counseling
Services Eligibility Data
(Rev.3848, Issued: 08- 25-17, Effective: 09-26-17, Implementation: 09- 26-17)
Providers may access coverage period remaining counseling sessions and a next eligible date,
when there are no remaining sessions, through the 270/271 eligibility inquiry and response
transaction.
20 – Billing Requirements for Coverage of Kidney Disease Patient
Education Services
(Rev. 1876; Issued: 12-18-09; Effective Date: 01-01-10; Implementation Date: 04-05-
10)
Effective for claims with dates of service on and after January 1, 2010, the Medicare
Improvements for Patients and Providers Act of 2008 (MIPPA) determines that kidney
disease patient education services are covered when provided to patients with stage IV
chronic kidney disease (CKD). See Pub. 100-02, chapter 15, section 310, for complete
coverage guidelines.
Contractors shall pay for kidney disease education (KDE) services that meet the following
conditions:
• No more than 6 sessions of KDE services are provided in a lifetime,
• Is provided in increments of 1 hour. In order to bill for a session, a session must be at
least 31 minutes in duration. A session that lasts at least 31 minutes, but less than 1
hour still constitutes 1 session.
• Is provided either individually or in a group setting of 2 to 20 individuals who need
not all be Medicare beneficiaries.
• Furnished, upon the referral of the physician managing the beneficiary’s kidney
condition, by a qualified person meaning a:
o physician, physician’s assistant, nurse practitioner, or clinical nurse specialist;
o hospital, critical access hospital (CAH), skilled nursing facility (SNF),
comprehensive outpatient rehabilitation facility (CORF), home health agency
(HHA), or hospice, that is located in a rural area, or
o hospital or CAH that is paid as if it were located in a rural area (hospital or CAH
reclassified as rural under section 42 CFR 412.103).
NOTE: A renal dialysis facility (Type of Bill (TOB) 72x) is precluded from providing KDE
services.
20.1 – Additional Billing Requirements Applicable to Claims Submitted to
Fiscal Intermediaries (FIs)
(Rev. 1876; Issued: 12-18-09; Effective Date: 01-01-10; Implementation Date: 04-05-
10)
The FI will reimburse for KDE services when services are rendered in a rural area and
submitted on the following TOBs: 12X, 13X, 22X, 23X, 34X, 75X, 81X, 82X, and 85X.
NOTE: FIs shall use the actual geographic location, core based statistical area (CBSA) to
identify facilities located in rural areas. In addition, KDE services are covered when claims
containing the above mentioned TOBs are received from section 401 hospitals.
Revenue code 0942 should be reported when billing for KDE services in the following: SNFs,
HHAs, CORFs, hospices, and CAHs.
Hospital outpatient departments bill for this service under any valid/appropriate revenue code.
They are not required to report revenue code 0942.
Hospices report this service on a separate claim from any hospice services. Hospice claims
billed for revenue code 0942 that contain any other services will be returned to the provider.
In addition, hospices report value code 61 or G8 when billing for KDE services.
NOTE: KDE services are not covered when services are submitted on TOB 72X.
20.2 - Healthcare Common Procedure Coding System (HCPCS) Procedure
Codes and Applicable Diagnosis Codes
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
Effective for services performed on and after January 1, 2010, the following new HCPCS
codes have been created for KDE services when provided to patients with stage IV CKD.
• G0420: Face-to-face educational services related to the care of chronic kidney
disease; individual, per session, per one hour
• G0421: Face-to-face educational services related to the care of chronic kidney
disease; group, per session, per one hour
When billing for KDE services the applicable ICD diagnosis code shall be used:
• If ICD-9-CM is applicable, ICD-9-CM - 585.4 (chronic kidney disease, Stage IV
(severe)), or
• If ICD-9-CM is applicable, ICD-10-CM – N18.4 (Chronic Kidney Disease, stage 4.
NOTE: Claims with HCPCS codes G0420 or G0421 and ICD-9 code 585.4, if applicable, or,
if ICD -10 is applicable, ICD-10 code N18.4 that are billed for KDE services are not allowed
on a professional and institutional claim on the same service date.
20.3 - Medicare Summary Notices (MSNs) and Claim Adjustment Reason
Codes (CARCs)
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
The following messages are used by Medicare contractors when denying non-covered
services associated with KDE services when provided to patients with stage IV CKD:
When denying claims for KDE services billed without diagnosis code 585.4 contractors shall
use:
• MSN 16.10 - Medicare does not pay for this item or service.
• CARC 167 - This (these) diagnosis(es) is (are) not covered. NOTE: Refer to the 835
Healthcare Policy Identification Segment (loop 2110 Service Payment Information
REF), if present.
When denying claims for KDE services when submitted for more than 6 sessions contractors
shall use:
• MSN 15.22 - The information provided does not support the need for this many
services or items in this period of time so Medicare will not pay for this item or
service.
• CARC 119 - Benefit maximum for this time period or occurrence has been reached.
When denying claims for KDE services when two claims are billed (professional and
institutional) on the same service date, contractors shall use:
• MSN 15.5 – The information provided does not support the need for similar services
by more than one doctor during the same time period.
• CARC 18 – Exact duplicate claim/service (Use only with Group Code OA except
where state workers' compensation regulations requires CO).
A/B MACs (A) shall deny KDE services when rendered in an urban area unless:
• The provider is a hospital on the section 401 list or
• The claim is submitted on TOB 85X.
A/B MACs (A) shall deny payment for KDE services when submitted on TOB 72X.
Use the following messages:
• MSN 21.6 – This item or service is not covered when performed, referred or ordered
by this provider.
• CARC 170 – Payment is denied when performed/billed by this type of provider in this
type of facility. NOTE: Refer to the 835 Healthcare Policy Identification Segment
(loop 2110 Service Payment Information REF), if present.
20.4 - Advance Beneficiary Notice (ABN) Information
(Rev. 1876; Issued: 12-18-09; Effective Date: 01-01-10; Implementation Date: 04-05-
10)
If a signed ABN was provided, contractors shall use Group Code PR (Patient Responsibility)
and the liability falls to the beneficiary.
If an ABN was not provided, contractors shall use Group Code CO (Contractual Obligation)
and the liability falls to the provider.
30 - Hyperbaric Oxygen (HBO) Therapy
(Rev. 187, 05-28-04)
30.1 - Billing Requirements for HBO Therapy for the Treatment of
Diabetic Wounds of the Lower Extremities
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Hyperbaric Oxygen Therapy is a modality in which the entire body is exposed to oxygen
under increased atmospheric pressure. Effective April 1, 2003, a National Coverage
Decision expanded the use of HBO therapy to include coverage for the treatment of
diabetic wounds of the lower extremities. For specific coverage criteria for HBO Therapy,
refer to the National Coverage Determinations Manual, Chapter 1, section 20.29.
NOTE: Topical application of oxygen does not meet the definition of HBO therapy as
stated above. Also, its clinical efficacy has not been established. Therefore, no Medicare
reimbursement may be made for the topical application of oxygen.
•
Billing Requirements for A/B MACs (A)
Claims for HBO therapy should be submitted using the ASC X12 837 institutional claim
format or, in rare cases, on Form CMS-1450.
a. Applicable Bill Types
The applicable hospital bill types are 11X, 13X and 85X.
b. Procedural Coding
• 99183 – Physician attendance and supervision of hyperbaric oxygen
therapy, per session.
• G0277 – Hyperbaric oxygen under pressure, full body chamber, per 30-
minute interval.
NOTE: Code G0277 is not available for use other than in a hospital outpatient department.
In skilled nursing facilities (SNFs), HBO therapy is part of the SNF PPS payment for
beneficiaries in covered Part A stays.
For hospital inpatients and critical access hospitals (CAHs) not electing Method I, HBO
therapy is reported under revenue code 940 without any HCPCS code. For inpatient
services, if ICD-10 is applicable, show ICD-10-PCS code 5A05121.
For CAHs electing Method I, HBO therapy is reported under revenue code 940 along with
HCPCS code 99183.
c. Payment Requirements for A/B MACs (A)
Payment is as follows:
A/B MAC (A) payment is allowed for HBO therapy for diabetic wounds of the lower
extremities when performed as a physician service in a hospital outpatient setting and for
inpatients. Payment is allowed for claims with valid diagnosis codes as shown above with
dates of service on or after April 1, 2003. Those claims with invalid codes should be
denied as not medically necessary.
For hospitals, payment will be based upon the Ambulatory Payment Classification (APC)
or the inpatient Diagnosis Related Group (DRG). Deductible and coinsurance apply.
Payment to Critical Access Hospitals (electing Method I) is made under cost
reimbursement. For Critical Access Hospitals electing Method II, the technical component
is paid under cost reimbursement and the professional component is paid under the
Physician Fee Schedule.
II. A/B MAC (B) Billing Requirements
Claims for this service should be submitted using the ASC X12 837 professional claim
format or Form CMS-1500.
The following HCPCS code applies:
• 99183 – Physician attendance and supervision of hyperbaric oxygen therapy,
per session.
• G0277 – Hyperbaric oxygen under pressure, full body chamber, per 30-
minute interval.
a. Payment Requirements for A/B MACs (B)
Payment and pricing information will occur through updates to the Medicare Physician Fee
Schedule Database (MPFSDB). Pay for this service on the basis of the MPFSDB.
Deductible and coinsurance apply. Claims from physicians or other practitioners where
assignment was not taken, are subject to the Medicare limiting charge.
III. Medicare Summary Notices (MSNs)
Use the following MSN Messages where appropriate:
In situations where the claim is being denied on the basis that the condition does not
meet our coverage requirements, use one of the following MSN Messages:
“Medicare does not pay for this item or service for this condition.” (MSN Message
16.48)
The Spanish version of the MSN message should read:
“Medicare no paga por este articulo o servicio para esta afeccion.”
In situations where, based on the above utilization policy, medical review of the claim
results in a determination that the service is not medically necessary, use the following
MSN message:
“The information provided does not support the need for this service or item.”
(MSN Message 15.4)
The Spanish version of the MSN message should read:
“La informacion proporcionada no confirma la necesidad para este servicio o
articulo.”
IV. Remittance Advice Notices
Use appropriate existing remittance advice remark codes and claim adjustment reason
codes at the line level to express the specific reason if you deny payment for HBO therapy
for the treatment of diabetic wounds of lower extremities.
30.2 Hyperbaric Oxygen (HBO) Therapy (Section C, Topical Application of
Oxygen)
(Rev.3921, Issued: 11-17-17, Effective: 04-03-17, 12-18-17)
CMS considers topical oxygen therapy (TOT) to be a method whereby a local supply of
oxygen is applied to a wound.
I. Billing Requirements for A/B MACs (A)
Claims for HBO therapy should be submitted using the ASC X12 837 institutional claim
format or, in rare cases, on Form CMS-1450.
II. Payment Requirements for A/B MACs (A)
As of April 3, 2017, Medicare coverage of topical oxygen for the treatment of chronic
wounds will be determined by the local contractors.
NOTE: Regardless of whether an A/B MAC (A) has made a determination to cover this
service, there shall be no coverage for any separate or additional physician’s professional
services related to this procedure.
III. Billing Requirements for A/B MACs (B)
As of April 3, 2017, Medicare coverage of topical oxygen for the treatment of chronic
wounds will be determined by the local contractors.
NOTE: Regardless of whether an A/B MAC (B) has made a determination to cover this
service, there shall be no coverage for any separate or additional physician’s professional
services related to this procedure.
40 – Sacral Nerve Stimulation
(Rev. 125, 03-26-04)
A sacral nerve stimulator is a pulse generator that transmits electrical impulses to the sacral
nerves through an implanted wire. These impulses cause the bladder muscles to contract,
which gives the patient ability to void more properly.
40.1 – Coverage Requirements
(Rev. 125, 03-26-04)
Effective January 1, 2002, sacral nerve stimulation is covered for the treatment of urinary
urge incontinence, urgency-frequency syndrome and urinary retention. Sacral nerve
stimulation involves both a temporary test stimulation to determine if an implantable
stimulator would be effective and a permanent implantation in appropriate candidates. Both
the test and the permanent implantation are covered.
The following limitations for coverage apply to all indications:
o Patient must be refractory to conventional therapy (documented behavioral,
pharmacologic and/or surgical corrective therapy) and be an appropriate surgical candidate
such that implantation with anesthesia can occur.
o Patients with stress incontinence, urinary obstruction, and specific neurologic diseases
(e.g., diabetes with peripheral nerve involvement) that are associated with secondary
manifestations of the above three indications are excluded.
o Patient must have had a successful test stimulation in order to support subsequent
implantation. Before a patient is eligible for permanent implantation, he/she must
demonstrate a 50% or greater improvement through test stimulation. Improvement is
measured through voiding diaries.
o Patient must be able to demonstrate adequate ability to record voiding diary data such
that clinical results of the implant procedure can be properly evaluated.
40.2 – Billing Requirements
(Rev. 125, 03-26-04)
40.2.1 – Healthcare Common Procedural Coding System (HCPCS)
(Rev. 11789, Issued:01-19-23, Effective Date: 02-21-23, Implementation Date: 02-21-23)
64561 - Percutaneous implantation of neurostimulator electrodes; sacral
nerve (transforaminal placement)
64581 - Incision for implantation of neurostimulator electrodes; sacral nerve
(transforaminal placement)
64585 - Revision or removal of peripheral neurostimulator electrodes
64590 - Incision and subcutaneous placement of peripheral
neurostimulator pulse generator or receiver, direct or inductive
coupling
64595 - Revision or removal of peripheral neurostimulator pulse generator
or receiver
A4290 - Sacral nerve stimulation test lead, each
C1767 - Generator, neurostimulator (implantable)
C1778 - Lead, neurostimulator (implantable)
C1820 - Generator, neurostimulator (implantable), with rechargeable
battery and charging system - effective 01/01/20 for NCD230.18 with
CR11655
C1883 - Adaptor/extension, pacing lead or neurostimulator lead
(implantable)
C1897 - Lead, neurostimulator test kit (implantable)
E0752 - Implantable neurostimulator electrodes, each
E0756 - Implantable neurostimulator pulse generator
NOTE: The "C" codes listed above are only applicable when billing under the hospital
outpatient prospective payment system (OPPS). They should be reported in place of codes
A4290, E0752 and E0756.
40.2.2 – Payment Requirements for Test Procedures (HCPCS Codes 64585,
64590 and 64595)
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
Payment is as follows:
• Hospital outpatient departments – OPPS
• Critical access hospital (CAH) - Reasonable cost
• Comprehensive outpatient rehabilitation facility - Medicare physician fee schedule
(MPFS)
• Rural health clinics/federally qualified health centers (RHCs/FQHCs) - All inclusive
rate, professional component only. The technical component is outside the scope of
the RHC/FQHC benefit. Therefore, the provider of that technical service bills their
A/B MAC (B) using the ASC X12 837 professional claim format or Form CMS-1500
and payment is made under the MPFS. For provider-based RHCs/FQHCs payment
for the technical component is made as indicated above based on the type of provider
the RHC/FQHC is based with.
Deductible and coinsurance apply.
40.2.3 – Payment Requirements for Device Codes A4290, E0752 and E0756
(Rev. 125, 03-26-04)
Payment is made on a reasonable cost basis when these devices are implanted in a CAH.
40.2.4 – Payment Requirements for Codes C1767, C1778, C1820, C1883
and C1897
(Rev. 11789, Issued:01-19-23, Effective Date: 02-21-23, Implementation Date: 02-21-23)
Only hospital outpatient departments report these codes. Payment is made under OPPS.
40.3 – Bill Types
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
The applicable bill types for test stimulation procedures are 13X, 71X, 73X, 75X and 85X.
The RHCs and FQHCs bill you under bill type 71X and 73X for the professional component.
The technical component is outside the scope of the RHC/FQHC benefit. The provider of that
technical service bills their A/B MAC (B) using the ASC X12 837 professional claim format
or the Form CMS-1500.
The technical component for a provider-based RHC/FQHC is typically furnished by the
provider. The provider of that service bills you under bill type 13X, or 85X as appropriate
using their outpatient provider number (not the RHC/FQHC provider number since these
services are not covered as RHC/FQHC services.) Effective 4/1/06, type of bill 14X is for
non-patient laboratory specimens and is no longer applicable for test stimulation procedures.
The applicable bill types for implantation procedures and devices are 11X, 13X, and 85X.
40.4 – Revenue Codes
(Rev.10881; Issued: 08-06-2021; Effective: 09-07-2021; Implementation: 09-07- 2021)
The applicable revenue code for the test procedures is 920 except for RHCs/FQHCs who
report these procedures under revenue code 521.
Revenue codes for the implantation can be performed in a number of revenue centers within
a hospital such as operating room (360) or clinic (510). Therefore, instruct your hospitals to
report these implantation procedures under the revenue center where they are performed.
The applicable revenue code for the device codes C1767, C1778, C1883, C1897, and C1820
provided in a hospital outpatient department is 272, 274, 275, 276, 278, 279, 280, 289, 290 or
624 as appropriate. The applicable revenue code for device codes A4290, E0752 and
E0756 provided in a CAH is 290.
40.5 – Claims Editing
(Rev. 125, 03-26-04)
Nationwide claims processing edits for pre or post payment review of claim(s) for sacral
nerve stimulation are not being required at this time. Contractors may develop local medical
review policy and edits for such claim(s).
50 – Deep Brain Stimulation for Essential Tremor and Parkinson’s Disease
(Rev. 128, 03-26-04)
Deep brain stimulation (DBS) refers to high-frequency electrical stimulation of anatomic
regions deep within the brain utilizing neurosurgically implanted electrodes. These DBS
electrodes are stereotactically placed within targeted nuclei on one (unilateral) or both
(bilateral) sides of the brain. There are currently three targets for DBS -- the thalamic
ventralis intermedius nucleus (VIM), subthalamic nucleus (STN) and globus pallidus interna
(GPi).
Essential tremor (ET) is a progressive, disabling tremor most often affecting the hands. ET
may also affect the head, voice and legs. The precise pathogenesis of ET is unknown. While
it may start at any age, ET usually peaks within the second and sixth decades. Beta-
adrenergic blockers and anticonvulsant medications are usually the first line treatments for
reducing the severity of tremor. Many patients, however, do not adequately respond or
cannot tolerate these medications. In these medically refractory ET patients, thalamic VIM
DBS may be helpful for symptomatic relief of tremor.
Parkinson’s disease (PD) is an age-related progressive neurodegenerative disorder involving
the loss of dopaminergic cells in the substantia nigra of the midbrain. The disease is
characterized by tremor, rigidity, bradykinesia and progressive postural instability.
Dopaminergic medication is typically used as a first line treatment for reducing the primary
symptoms of PD. However, after prolonged use, medication can become less effective and
can produce significant adverse events such as dyskinesias and other motor function
complications. For patients who become unresponsive to medical treatments and/or have
intolerable side effects from medications, DBS for symptom relief may be considered.
50.1 – Coverage Requirements
(Rev. 128, 03-26-04)
Effective on or after April 1, 2003, Medicare will cover unilateral or bilateral thalamic VIM
DBS for the treatment of ET and/or Parkinsonian tremor and unilateral or bilateral STN or
GPi DBS for the treatment of PD only under the following conditions:
1. Medicare will only consider DBS devices to be reasonable and necessary if they are
Food and Drug Administration (FDA) approved devices for DBS or devices used in
accordance with FDA approved protocols governing Category B Investigational Device
Exemption (IDE) DBS clinical trials.
2. For thalamic VIM DBS to be considered reasonable and necessary, patients must meet
all of the following criteria:
a. Diagnosis of essential tremor (ET) based on postural or kinetic tremors of
hand(s) without other neurologic signs, or diagnosis of idiopathic PD
(presence of at least 2 cardinal PD features (tremor, rigidity or bradykinesia))
which is of a tremor- dominant form.
b. Marked disabling tremor of at least level 3 or 4 on the Fahn-Tolosa-Marin
Clinical Tremor Rating Scale (or equivalent scale) in the extremity intended
for treatment, causing significant limitation in daily activities despite optimal
medical therapy.
c. Willingness and ability to cooperate during conscious operative procedure, as
well as during post-surgical evaluations, adjustments of medications and
stimulator settings.
3. For STN or GPi DBS to be considered reasonable and necessary, patients must meet
all of the following criteria:
a. Diagnosis of PD based on the presence of at least 2 cardinal PD features
(tremor, rigidity or bradykinesia).
b. Advanced idiopathic PD as determined by the use of Hoehn and Yahr stage or
Unified Parkinson’s Disease Rating Scale (UPDRS) part III motor subscale.
c. L-dopa responsive with clearly defined “on” periods.
d. Persistent disabling Parkinson’s symptoms or drug side effects (e.g.,
dyskinesias, motor fluctuations, or disabling “off” periods) despite optimal
medical therapy.
e. Willingness and ability to cooperate during conscious operative procedure, as
well as during post-surgical evaluations, adjustments of medications and
stimulator settings.
The DBS is not reasonable and necessary and is not covered for ET or PD patients with any
of the following:
1. Non-idiopathic Parkinson’s disease or “Parkinson’s Plus” syndromes.
2. Cognitive impairment, dementia or depression which would be worsened by or would
interfere with the patient’s ability to benefit from DBS.
3. Current psychosis, alcohol abuse or other drug abuse.
4. Structural lesions such as basal ganglionic stroke, tumor or vascular malformation as
etiology of the movement disorder.
5. Previous movement disorder surgery within the affected basal ganglion.
6. Significant medical, surgical, neurologic or orthopedic co-morbidities contraindicating
DBS surgery or stimulation.
Patients who undergo DBS implantation should not be exposed to diathermy (deep heat
treatment including shortwave diathermy, microwave diathermy and ultrasound diathermy) or
any type of MRI which may adversely affect the DBS system or adversely affect the brain
around the implanted electrodes.
The DBS should be performed with extreme caution in patients with cardiac pacemakers or
other electronically controlled implants which may adversely affect or be affected by the DBS
system.
For DBS lead implantation to be considered reasonable and necessary, providers and facilities
must meet all of the following criteria:
1. Neurosurgeons must: (a) be properly trained in the procedure; (b) have
experience with the surgical management of movement disorders, including DBS therapy;
and (c) have experience performing stereotactic neurosurgical procedures
2. Operative teams must have training and experience with DBS systems,
including knowledge of anatomical and neurophysiological characteristics for localizing the
targeted nucleus, surgical and/or implantation techniques for the DBS system, and operational
and functional characteristics of the device.
3. Physicians specializing in movement disorders must be involved in both
patient selection and post-procedure care.
4. Hospital medical centers must have: (a) brain imaging equipment (MRI and/or
CT) for pre-operative stereotactic localization and targeting of the surgical site(s); (b)
operating rooms with all necessary equipment for stereotactic surgery; and (c) support
services necessary for care of patients undergoing this procedure and any potential
complications arising intraoperatively or postoperatively.
50.2 – Billing Requirements
(Rev. 128, 03-26-04)
50.2.1 – Part A Intermediary Billing Procedures
(Rev. 128, 03-26-04)
This procedure can be two fold. Implantation of the electrodes is performed in a hospital
inpatient setting. Implantation of the pulse generator can be performed in an outpatient
department.
50.3 - Payment Requirements
(Rev. 128, 03-26-04)
50.3.1 – Part A Payment Methods
(Rev. 128, 03-26-04)
Payment for the inpatient procedure is under Diagnostic Related Group (DRG). The
outpatient procedure is outpatient prospective payment system. For critical access hospitals
(CAH), the inpatient stay is on reasonable cost and the outpatient procedures are also based
on reasonable cost.
50.3.2 – Bill Types
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Deep Brain Stimulation may be submitted on institutional claims using the following Types
of Bill:
11X, 12X, 13X, and 85X
50.3.3 – Revenue Codes
(Rev. 128, 03-26-04)
Revenue codes for implementation can be performed in a number of revenue centers within a
hospital such as operating room (360) or clinic (510). The codes to report the pulse generator
and/or electrodes are 270, 278, 279.
For CAHs that choose method II, use revenue code 98X for the professional component only.
50.4 – Allowable Codes
(Rev. 128, 03-26-04)
50.4.1 – Allowable Covered Diagnosis Codes
(Rev. 12435, Issued:12-28-23, Effective:01-29-24, Implementation:01-29-24)
Deep Brain Stimulation is covered for the following diagnosis codes:
If ICD-10-CM is applicable:
• ICD-10-CM G20.A1 - Parkinson's disease without dyskinesia, without mention of
fluctuations
• ICD-10-CM G20.A2 - Parkinson's disease without dyskinesia, with fluctuations
• ICD-10-CM G20.B1 - Parkinson's disease with dyskinesia, without mention of
fluctuations
• ICD-10 CM G20.B2 - Parkinson's disease with dyskinesia, with fluctuations
• ICD-10-CM G20.C - Parkinsonism, unspecified

• ICD-10-CM G25.0 - Essential tremor
• ICD-10-CM G25.2 - Other specified form of tremor
50.4.2 – Allowable Covered Procedure Codes
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
The following procedure codes may be present:
If ICD-10-PCS is applicable:
ICD-10-PCS
Code
Code Description
00H00MZ
Insertion of Neurostimulator Lead into Brain, Open Approach
00H03MZ
Insertion of Neurostimulator Lead into Brain, Percutaneous
Approach
00H04MZ
Insertion of Neurostimulator Lead into Brain, Endoscopic Approach
00H60MZ
Insertion of Neurostimulator Lead into Cerebral Ventricle, Open
Approach
00H63MZ
Insertion of Neurostimulator Lead into Cerebral Ventricle,
Percutaneous Approach
00H64MZ
Insertion of Neurostimulator Lead into Cerebral Ventricle,
Percutaneous Endoscopic Approach
00P00MZ
Removal of Neurostimulator Lead from Brain, Open Approach
00P03MZ
Removal of Neurostimulator Lead from Brain, Percutaneous
Approach
00P04MZ
Removal of Neurostimulator Lead from Brain, Percutaneous
Endoscopic Approach
00P60MZ
Removal of Neurostimulator Lead from Cerebral Ventricle, Open
Approach
00P63MZ
Removal of Neurostimulator Lead from Cerebral Ventricle,
Percutaneous Approach
00P64MZ
Removal of Neurostimulator Lead from Brain, Open Approach
0H80XZZ
Division of Scalp Skin, External Approach
0HSSXZZ
Reposition Hair, External Approach
Coverage policy may be found in the National Coverage Determinations Manual
in Chapter 1, section 160.24: Deep Brain Stimulation, using the following link:
(http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp).
50.4.3 – Healthcare Common Procedure Coding System (HCPCS)
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
The following HCPCS codes are available for use when billing for covered deep
brain stimulation:
61880 Revision or removal of intracranial neurostimulator electrodes
61885 Incision and subcutaneous placement of cranial neurostimulator pulse
generator or receiver, direct or inductive coupling; with connection to a
single electrode array
61886 Incision and subcutaneous placement of cranial neurostimulator pulse generator
or receiver, direct or inductive coupling; with connection to two or more
electrode arrays
61888 Revision or removal of cranial neurostimulator pulse generator or receiver
95961 Functional cortical and subcortical mapping by stimulation and/or recording of
electrodes on brain surface, or of depth electrodes, to provoke seizures or
identify vital brain structures; initial hour of physician attendance
95962 Functional cortical and subcortical mapping by stimulation and/or recording of
electrodes on brain surface, or of depth electrodes, to provoke seizures or
identify vital brain structures; each additional hour of physician attendance
(List separately in addition to code for primary procedure) (Use 95962 in
conjunction with code 95961)
95970 Electronic analysis of implanted neurostimulator pulse generator system
(e.g., rate, pulse amplitude and duration, configuration of wave form,
battery status, electrode selectability, output modulation, cycling,
impedance and patient compliance measurements); simple or complex
brain, spinal cord, or peripheral (i.e., cranial nerve, peripheral nerve,
autonomic nerve, neuromuscular) neurostimulator pulse
generator/transmitter, without reprogramming
95971 Electronic analysis of implanted neurostimulator pulse generator system
(e.g., rate, pulse amplitude and duration, configuration of wave form,
battery status, electrode selectability, output modulation, cycling,
impedance and patient compliance measurements); simple brain, spinal
cord, or peripheral (i.e., peripheral nerve, autonomic nerve, neuromuscular)
neurostimulator pulse generator/transmitter, with intraoperative or
subsequent programming.
95983 Electronic analysis of implanted neurostimulator pulse
generator/transmitter (eg, contact group(s), interleaving, amplitude, pulse
width, frequency (Hz), on/off cycling, burst, magnet mode, doe lockout,
patient selectable parameters, responsive neurostimulation, detection
algorithms, closed loop parameters, and passive parameters) by physician
or other qualified health care professional; with brain neurostimulator pulse
generator/ transmitter programming, first 15 minutes face-to-face time with
physician or other qualified health care professional.
95984 Electronic analysis of implanted neurostimulator pulse
generator/transmitter (eg, contact group(s), interleaving, amplitude, pulse
width, frequency (Hz), on/off cycling, burst, magnet mode, doe lockout,
patient selectable parameters, responsive neurostimulation, detection
algorithms, closed loop parameters, and passive parameters) by physician
or other qualified health care professional; with brain neurostimulator pulse
generator/transmitter programming, each additional 15 minutes face-to-face
time with physician or other qualified health care professional.
50.5 – Ambulatory Surgical Centers
(Rev. 128, 03-26-04)
The following HCPCS codes are approved for billing in Ambulatory Surgical Centers:
61885 Incision and subcutaneous placement of cranial neurostimulator pulse generator or
receiver, direct or inductive coupling; with connection to a single electrode array -
ASC Payment Group 02
61888 Revision or removal of cranial neurostimulator pulse generator or receiver - ASC
Payment Group 01
NOTE: Pulse generator is payable in an ASC; implantation of electrodes are not.
50.6 – Claims Editing for Intermediaries
(Rev. 128, 03-26-04)
We do not require nationwide standard system claims processing edits for pre and post
payment review of claim(s) at this time. However, carriers and intermediaries may create
local claims processing edits for the requirements listed above.
50.7 – Remittance Advice Notice for Intermediaries
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
Use appropriate existing remittance advice reason and remark codes at the line level to
express the specific reason if you deny payment for DBS. If denying services as furnished
before April 1, 2003, use existing ASC X 12-835 claim adjustment reason code 26 "Expenses
incurred prior to coverage" at the line level.
50.8 - Medicare Summary Notice (MSN) Messages for Intermediaries
(Rev. 128, 03-26-04)
Use the following MSN messages where appropriate:
If a claim for DBS is denied because the service was performed prior to April 1, 2003, use the
MSN message:
"This service was not covered by Medicare at the time you received it." (MSN
Message 21.11)
The Spanish version of the MSN message should read:
"Este servicio no estaba cubierto por Medicare cuando usted lo recibió." (MSN
Message 21.11)
50.9 – Provider Notification
(Rev. 128, 03-26-04)
Contractors should notify providers of this new national coverage in their next regularly
scheduled bulletin, on their Web site within 2 weeks, and in routinely scheduled training
sessions.
60 – Coverage and Billing for Home Prothrombin Time (PT/INR)
Monitoring for Home Anticoagulation Management
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
The prothrombin time (PT) test is an in-vitro test to assess coagulation. PT testing and its
normalized correlate, the International Normalized Ratio (INR), are the standard
measurements for therapeutic effectiveness of warfarin therapy. Warfarin, Coumadin®, and
others, are self-administered, oral anticoagulant, or blood thinner, medications that affect a
person’s Vitamin K-dependent clotting factors.
Use of the INR allows physicians to determine the level of anticoagulation in a patient
independent of the laboratory reagents used. The INR is the ratio of the patient's prothrombin
time compared to the mean prothrombin time for a group of normal individuals.
60.1 – Coverage Requirements
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
For services furnished on or after July 1, 2002, Medicare will cover the use of home INR
monitoring for anticoagulation management for patients with mechanical heart valves on
warfarin. The monitor and the home testing must be prescribed by a physician and the
following patient requirements must be met:
• Must have been anticoagulated for at least 3 months prior to use of the home INR
device;
• Must undergo an educational program on anticoagulation management and the use of
the device prior to its use in the home; and
• Self testing with the device is limited to a frequency of once per week.
For services furnished on or after March 19, 2008, the Centers for Medicare & Medicaid
Services revised its national coverage determination (NCD) on PT/INR Monitoring for Home
Anticoagulation Management as follows:
Medicare will cover the use of home PT/INR monitoring for chronic, oral anticoagulation
management for patients with mechanical heart valves, chronic atrial fibrillation, or venous
thromboembolism (inclusive of deep venous thrombosis and pulmonary embolism) on
warfarin. The monitor and the home testing must be prescribed by a treating physician as
provided at 42 CFR 410.32(a), and all of the following requirements must be met:
1. The patient must have been anticoagulated for at least 3 months prior to use of the home
INR device; and,
2. The patient must undergo a face-to-face educational program on anticoagulation
management and must have demonstrated the correct use of the device prior to its use in the
home; and,
3. The patient continues to correctly use the device in the context of the management of the
anticoagulation therapy following the initiation of home monitoring; and,
4. Self-testing with the device should not occur more frequently than once a week.
NOTE: Porcine valves are not included in this NCD, so Medicare will not make payment on
home INR monitoring for patients with porcine valves unless covered by local Medicare
contractors.

60.2 – Intermediary Payment Requirements
(Rev. 216, 06-25-04)
60.2.1 – Part A Payment Methods
(Rev. 216, 06-25-04)
Payment is as follows:
• Hospital outpatient departments - Outpatient Prospective Payment System (OPPS)
• Critical Access Hospital (CAH) - Reasonable cost or Medicare Physician Fee
Schedule (MPFS)
Deductible and coinsurance apply.
60.3 – Intermediary Billing Procedures
(Rev. 216, 06-25-04)
60.3.1 – Bill Types
(Rev. 216, 06-25-04)
The applicable bill types are 13X and 85X.
60.3.2 – Revenue Codes
(Rev. 216, 06-25-04)
Hospitals may report these services under revenue code 920 or they may report HCPCS codes
G0248 and G0249 under the revenue center where they are performed.
60.4 – Intermediary Allowable Codes
(Rev. 216, 06-25-04)
60.4.1 – Allowable Covered Diagnosis Codes
(Rev.10881; Issued: 08-06-2021; Effective: 09-07-2021; Implementation: 09-07- 2021)
For services furnished on or after the implementation of ICD-10 the applicable ICD-10-CM
diagnosis codes for this benefit are:
ICD-10-CM Code
Code Description
D68.51
Activated protein C resistance
D68.52
Prothrombin gene mutation
D68.59
Other primary thrombophilia
D68.61
Antiphospholipid syndrome
D68.62
Lupus anticoagulant syndrome
I23.6
Thrombosis of atrium, auricular appendage, and ventricle as
current complications following acute myocardial infarction
I26.01
Septic pulmonary embolism with acute cor pulmonale
I26.09
Other pulmonary embolism with acute cor pulmonale
I26.90
Septic pulmonary embolism without acute cor pulmonale
I26.93
Single subsegmental pulmonary embolism without acute cor
pulmonale

I26.94
Multiple subsegmental pulmonary emboli without acute cor
pulmonale
I26.99
Other pulmonary embolism without acute cor pulmonale
I27.24
Chronic thromboembolic pulmonary hypertension
I27.82
Chronic pulmonary embolism
I48.0
Paroxysmal atrial fibrillation
I48.11
Longstanding persistent atrial fibrillation
I48.19
Other persistent atrial fibrillation
I48.21
Permanent atrial fibrillation
I67.6
Nonpyogenic thrombosis of intracranial venous system
I80.11
Phlebitis and thrombophlebitis of right femoral vein
I80.12
Phlebitis and thrombophlebitis of left femoral vein
I80.13
Phlebitis and thrombophlebitis of femoral vein, bilateral
I80.211
Phlebitis and thrombophlebitis of right iliac vein
I80.212
Phlebitis and thrombophlebitis of left iliac vein
I80.213
Phlebitis and thrombophlebitis of iliac vein, bilateral
I80.221
Phlebitis and thrombophlebitis of right popliteal vein
I80.222
Phlebitis and thrombophlebitis of left popliteal vein
I80.223
Phlebitis and thrombophlebitis of popliteal vein, bilateral
I80.231
Phlebitis and thrombophlebitis of right tibial vein
I80.232
Phlebitis and thrombophlebitis of left tibial vein
I80.233
Phlebitis and thrombophlebitis of tibial vein, bilateral
I80.241
Phlebitis and thrombophlebitis of right peroneal vein
I80.242
Phlebitis and thrombophlebitis of left peroneal vein
I80.243
Phlebitis and thrombophlebitis of peroneal vein, bilateral
I80.251
Phlebitis and thrombophlebitis of right calf muscular vein
I80.252
Phlebitis and thrombophlebitis of left calf muscular vein
I80.253
Phlebitis and thrombophlebitis of calf muscular vein, bilateral
I80.291
Phlebitis and thrombophlebitis of other deep vessels of right
lower extremity
I80.292
Phlebitis and thrombophlebitis of other deep vessels of left
lower extremity
I80.293
Phlebitis and thrombophlebitis of other deep vessels of lower
extremity, bilateral
I82.0
Budd-Chiari syndrome
I82.210
Acute embolism and thrombosis of superior vena cava
I82.211
Chronic embolism and thrombosis of superior vena cava
I82.220
Acute embolism and thrombosis of inferior vena cava
I82.221
Chronic embolism and thrombosis of inferior vena cava
I82.290
Acute embolism and thrombosis of other thoracic veins
I82.291
Chronic embolism and thrombosis of other thoracic veins
I82.3
Embolism and thrombosis of renal vein
I82.411
Acute embolism and thrombosis of right femoral vein
I82.412
Acute embolism and thrombosis of left femoral vein
I82.413
Acute embolism and thrombosis of femoral vein, bilateral
I82.421
Acute embolism and thrombosis of right iliac vein
I82.422
Acute embolism and thrombosis of left iliac vein
I82.423
Acute embolism and thrombosis of iliac vein, bilateral
I82.431
Acute embolism and thrombosis of right popliteal vein
I82.432
Acute embolism and thrombosis of left popliteal vein

I82.433
Acute embolism and thrombosis of popliteal vein, bilateral
I82.441
Acute embolism and thrombosis of right tibial vein
I82.442
Acute embolism and thrombosis of left tibial vein
I82.443
Acute embolism and thrombosis of tibial vein, bilateral
I82.451
Acute embolism and thrombosis of right peroneal vein
I82.452
Acute embolism and thrombosis of left peroneal vein
I82.453
Acute embolism and thrombosis of peroneal vein, bilateral
I82.461
Acute embolism and thrombosis of right calf muscular vein
I82.462
Acute embolism and thrombosis of left calf muscular vein
I82.463
Acute embolism and thrombosis of calf muscular vein,
bilateral
I82.491
Acute embolism and thrombosis of other specified deep vein
of right lower extremity
I82.492
Acute embolism and thrombosis of other specified deep vein
of left lower extremity
I82.493
Acute embolism and thrombosis of other specified deep vein
of lower extremity, bilateral
I82.511
Chronic embolism and thrombosis of right femoral vein
I82.512
Chronic embolism and thrombosis of left femoral vein
I82.513
Chronic embolism and thrombosis of femoral vein, bilateral
I82.521
Chronic embolism and thrombosis of right iliac vein
I82.522
Chronic embolism and thrombosis of left iliac vein
I82.523
Chronic embolism and thrombosis of iliac vein, bilateral
I82.531
Chronic embolism and thrombosis of right popliteal vein
I82.532
Chronic embolism and thrombosis of left popliteal vein
I82.533
Chronic embolism and thrombosis of popliteal vein, bilateral
I82.541
Chronic embolism and thrombosis of right tibial vein
I82.542
Chronic embolism and thrombosis of left tibial vein
I82.543
Chronic embolism and thrombosis of tibial vein, bilateral
I82.551
Chronic embolism and thrombosis of right peroneal vein
I82.552
Chronic embolism and thrombosis of left peroneal vein
I82.553
Chronic embolism and thrombosis of peroneal vein, bilateral
I82.561
Chronic embolism and thrombosis of right calf muscular vein
I82.562
Chronic embolism and thrombosis of left calf muscular vein
I82.563
Chronic embolism and thrombosis of calf muscular vein,
bilateral
I82.591
Chronic embolism and thrombosis of other specified deep
vein of right lower extremity
I82.592
Chronic embolism and thrombosis of other specified deep
vein of left lower extremity
I82.593
Chronic embolism and thrombosis of other specified deep
vein of lower extremity, bilateral
I82.621
Acute embolism and thrombosis of deep veins of right upper
extremity
I82.622
Acute embolism and thrombosis of deep veins of left upper
extremity
I82.623
Acute embolism and thrombosis of deep veins of upper
extremity, bilateral
I82.721
Chronic embolism and thrombosis of deep veins of right
upper extremity

I82.722
Chronic embolism and thrombosis of deep veins of left upper
extremity
I82.723
Chronic embolism and thrombosis of deep veins of upper
extremity, bilateral
I82.890
Acute embolism and thrombosis of other specified veins
I82.891
Chronic embolism and thrombosis of other specified veins
I82.A11
Acute embolism and thrombosis of right axillary vein
I82.A12
Acute embolism and thrombosis of left axillary vein
I82.A13
Acute embolism and thrombosis of axillary vein, bilateral
I82.A21
Chronic embolism and thrombosis of right axillary vein
I82.A22
Chronic embolism and thrombosis of left axillary vein
I82.A23
Chronic embolism and thrombosis of axillary vein, bilateral
I82.B11
Acute embolism and thrombosis of right subclavian vein
I82.B12
Acute embolism and thrombosis of left subclavian vein
I82.B13
Acute embolism and thrombosis of subclavian vein, bilateral
I82.B21
Chronic embolism and thrombosis of right subclavian vein
I82.B22
Chronic embolism and thrombosis of left subclavian vein
I82.B23
Chronic embolism and thrombosis of subclavian vein, bilateral
I82.C11
Acute embolism and thrombosis of right internal jugular vein
I82.C12
Acute embolism and thrombosis of left internal jugular vein
I82.C13
Acute embolism and thrombosis of internal jugular vein,
bilateral
I82.C21
Chronic embolism and thrombosis of right internal jugular
vein
I82.C22
Chronic embolism and thrombosis of left internal jugular vein
I82.C23
Chronic embolism and thrombosis of internal jugular vein,
bilateral
O87.3
Cerebral venous thrombosis in the puerperium
Z79.01
Long term (current) use of anticoagulants
Z86.718
Personal history of other venous thrombosis and embolism
Z95.2
Presence of prosthetic heart valve
Coverage policy can be found in Pub. 100-03, Medicare National Coverage Determinations
Manual, Chapter 1, section 190.11 PT/INR.
(http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp
60.4.2 – Healthcare Common Procedure Coding System (HCPCS) for
Intermediaries
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
For services furnished on or after July 1, 2002, and prior to March 19, 2008, the applicable
HCPCS codes for this benefit are:
G0248: Demonstration, at initial use, of home INR monitoring for patient with mechanical
heart valve(s) who meets Medicare coverage criteria, under the direction of a physician;
includes: demonstration use and care of the INR monitor, obtaining at least one blood sample,
provision of instructions for reporting home INR test results and documentation of a patient’s
ability to perform testing.
Short Description: Demonstrate use home INR mon
G0249: Provision of test materials and equipment for home INR monitoring to patient with
mechanical heart valve(s) who meets Medicare coverage criteria. Includes provision of
materials for use in the home and reporting of test results to physician; per 4 tests.
Short Description: Provide test material, equipm
For services furnished on or after March 19, 2008, the applicable HCPCS codes for this
benefit are:
G0248: Demonstration, prior to initial use, of home INR monitoring for patient with either
mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism who meets
Medicare coverage criteria, under the direction of a physician; includes: face-to-face
demonstration of use and care of the INR monitor, obtaining at least one blood sample,
provision of instructions for reporting home INR test results, and documentation of patient
ability to perform testing prior to its use
Short Description: Demonstrate use home INR mon
G0249: Provision of test materials and equipment for home INR monitoring of patient
with either mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism
who meets Medicare coverage criteria; includes provision of materials for use in the home
and reporting of test results to physician; not occurring more frequently than once a week
Short Description: Provide INR test mater/equip
60.5 – Carrier Billing Instructions
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
Effective for claims with dates of service on and after March 19, 2008, the descriptors of
HCPCS Codes G0248, G0249, and G0250 were changed to reflect revised coverage policy.
60.5.1 - HCPCS for Carriers
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
For services furnished on or after July 1, 2002, and prior to March 19, 2008, the applicable
HCPCS codes for this benefit are:
G0248: Demonstration, at initial use, of home INR monitoring for patient with mechanical
heart valve(s) who meets Medicare coverage criteria, under the direction of a physician;
includes: demonstration use and care of the INR monitor, obtaining at least one blood sample,
provision of instructions for reporting home INR test results and documentation of a patient’s
ability to perform testing.
Short Description: Demonstrate use home INR mon
G0249: Provision of test materials and equipment for home INR monitoring to patient with
mechanical heart valve(s) who meets Medicare coverage criteria. Includes provision of
materials for use in the home and reporting of test results to physician; per 4 tests.
Short Description: Provide test material, equipm
G0250: Physician review; interpretation and patient management of home INR testing for a
patient with mechanical heart valve(s) who meets other coverage criteria; per 4 tests (does not
require face-to-face).

Short Description: MD review interpret of test
For services furnished on or after March 19, 2008, the applicable HCPCS codes for this
benefit are:
G0248: Demonstration, prior to initial use, of home INR monitoring for patient with either
mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism who meets
Medicare coverage criteria, under the direction of a physician; includes: face-to-face
demonstration of use and care of the INR monitor, obtaining at least one blood sample,
provision of instructions for reporting home INR test results, and documentation of patient
ability to perform testing prior to its use
Short Description: Demonstrate use home INR mon
G0249: Provision of test materials and equipment for home INR monitoring of patient with
either mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism who
meets Medicare coverage criteria; includes provision of materials for use in the home and
reporting of test results to physician; not occurring more frequently than once a week
Short Description: Provide INR test mater/equip
G0250: Physician review, interpretation, and patient management of home INR testing for a
patient with either mechanical heart valve(s), chronic atrial fibrillation, or venous
thromboembolism who meets Medicare coverage criteria; includes face-to-face verification
by the physician that the patient uses the device in the context of the management of the
anticoagulation therapy following initiation of the home INR monitoring; not occurring more
frequently than once a week
Short Description: MD INR test revie inter mgmt
60.5.2 – Applicable Diagnosis Codes for A/B MACs (B)
(Rev.10881; Issued: 08-06-2021; Effective: 09-07-2021; Implementation: 09-07- 2021)
For services furnished on or after the implementation of ICD-10 the applicable ICD-10-CM
diagnosis codes for this benefit are:
ICD-10-CM Code
Code Description
D68.51
Activated protein C resistance
D68.52
Prothrombin gene mutation
D68.59
Other primary thrombophilia
D68.61
Antiphospholipid syndrome
D68.62
Lupus anticoagulant syndrome
I23.6
Thrombosis of atrium, auricular appendage, and ventricle as
current complications following acute myocardial infarction
I26.01
Septic pulmonary embolism with acute cor pulmonale
I26.09
Other pulmonary embolism with acute cor pulmonale
I26.90
Septic pulmonary embolism without acute cor pulmonale
I26.93
Single subsegmental pulmonary embolism without acute cor
pulmonale
I26.94
Multiple subsegmental pulmonary emboli without acute cor
pulmonale
I26.99
Other pulmonary embolism without acute cor pulmonale

I27.24
Chronic thromboembolic pulmonary hypertension
I27.82
Chronic pulmonary embolism
I48.0
Paroxysmal atrial fibrillation
I48.11
Longstanding persistent atrial fibrillation
I48.19
Other persistent atrial fibrillation
I48.21
Permanent atrial fibrillation
I67.6
Nonpyogenic thrombosis of intracranial venous system
I80.11
Phlebitis and thrombophlebitis of right femoral vein
I80.12
Phlebitis and thrombophlebitis of left femoral vein
I80.13
Phlebitis and thrombophlebitis of femoral vein, bilateral
I80.211
Phlebitis and thrombophlebitis of right iliac vein
I80.212
Phlebitis and thrombophlebitis of left iliac vein
I80.213
Phlebitis and thrombophlebitis of iliac vein, bilateral
I80.221
Phlebitis and thrombophlebitis of right popliteal vein
I80.222
Phlebitis and thrombophlebitis of left popliteal vein
I80.223
Phlebitis and thrombophlebitis of popliteal vein, bilateral
I80.231
Phlebitis and thrombophlebitis of right tibial vein
I80.232
Phlebitis and thrombophlebitis of left tibial vein
I80.233
Phlebitis and thrombophlebitis of tibial vein, bilateral
I80.241
Phlebitis and thrombophlebitis of right peroneal vein
I80.242
Phlebitis and thrombophlebitis of left peroneal vein
I80.243
Phlebitis and thrombophlebitis of peroneal vein, bilateral
I80.251
Phlebitis and thrombophlebitis of right calf muscular vein
I80.252
Phlebitis and thrombophlebitis of left calf muscular vein
I80.253
Phlebitis and thrombophlebitis of calf muscular vein, bilateral
I80.291
Phlebitis and thrombophlebitis of other deep vessels of right
lower extremity
I80.292
Phlebitis and thrombophlebitis of other deep vessels of left
lower extremity
I80.293
Phlebitis and thrombophlebitis of other deep vessels of lower
extremity, bilateral
I82.0
Budd-Chiari syndrome
I82.210
Acute embolism and thrombosis of superior vena cava
I82.211
Chronic embolism and thrombosis of superior vena cava
I82.220
Acute embolism and thrombosis of inferior vena cava
I82.221
Chronic embolism and thrombosis of inferior vena cava
I82.290
Acute embolism and thrombosis of other thoracic veins
I82.291
Chronic embolism and thrombosis of other thoracic veins
I82.3
Embolism and thrombosis of renal vein
I82.411
Acute embolism and thrombosis of right femoral vein
I82.412
Acute embolism and thrombosis of left femoral vein
I82.413
Acute embolism and thrombosis of femoral vein, bilateral
I82.421
Acute embolism and thrombosis of right iliac vein
I82.422
Acute embolism and thrombosis of left iliac vein
I82.423
Acute embolism and thrombosis of iliac vein, bilateral
I82.431
Acute embolism and thrombosis of right popliteal vein
I82.432
Acute embolism and thrombosis of left popliteal vein
I82.433
Acute embolism and thrombosis of popliteal vein, bilateral
I82.441
Acute embolism and thrombosis of right tibial vein
I82.442
Acute embolism and thrombosis of left tibial vein

I82.443
Acute embolism and thrombosis of tibial vein, bilateral
I82.451
Acute embolism and thrombosis of right peroneal vein
I82.452
Acute embolism and thrombosis of left peroneal vein
I82.453
Acute embolism and thrombosis of peroneal vein, bilateral
I82.461
Acute embolism and thrombosis of right calf muscular vein
I82.462
Acute embolism and thrombosis of left calf muscular vein
I82.463
Acute embolism and thrombosis of calf muscular vein,
bilateral
I82.491
Acute embolism and thrombosis of other specified deep vein
of right lower extremity
I82.492
Acute embolism and thrombosis of other specified deep vein
of left lower extremity
I82.493
Acute embolism and thrombosis of other specified deep vein
of lower extremity, bilateral
I82.511
Chronic embolism and thrombosis of right femoral vein
I82.512
Chronic embolism and thrombosis of left femoral vein
I82.513
Chronic embolism and thrombosis of femoral vein, bilateral
I82.521
Chronic embolism and thrombosis of right iliac vein
I82.522
Chronic embolism and thrombosis of left iliac vein
I82.523
Chronic embolism and thrombosis of iliac vein, bilateral
I82.531
Chronic embolism and thrombosis of right popliteal vein
I82.532
Chronic embolism and thrombosis of left popliteal vein
I82.533
Chronic embolism and thrombosis of popliteal vein, bilateral
I82.541
Chronic embolism and thrombosis of right tibial vein
I82.542
Chronic embolism and thrombosis of left tibial vein
I82.543
Chronic embolism and thrombosis of tibial vein, bilateral
I82.551
Chronic embolism and thrombosis of right peroneal vein
I82.552
Chronic embolism and thrombosis of left peroneal vein
I82.553
Chronic embolism and thrombosis of peroneal vein, bilateral
I82.561
Chronic embolism and thrombosis of right calf muscular vein
I82.562
Chronic embolism and thrombosis of left calf muscular vein
I82.563
Chronic embolism and thrombosis of calf muscular vein,
bilateral
I82.591
Chronic embolism and thrombosis of other specified deep
vein of right lower extremity
I82.592
Chronic embolism and thrombosis of other specified deep
vein of left lower extremity
I82.593
Chronic embolism and thrombosis of other specified deep
vein of lower extremity, bilateral
I82.621
Acute embolism and thrombosis of deep veins of right upper
extremity
I82.622
Acute embolism and thrombosis of deep veins of left upper
extremity
I82.623
Acute embolism and thrombosis of deep veins of upper
extremity, bilateral
I82.721
Chronic embolism and thrombosis of deep veins of right
upper extremity
I82.722
Chronic embolism and thrombosis of deep veins of left upper
extremity

I82.723
Chronic embolism and thrombosis of deep veins of upper
extremity, bilateral
I82.890
Acute embolism and thrombosis of other specified veins
I82.891
Chronic embolism and thrombosis of other specified veins
I82.A11
Acute embolism and thrombosis of right axillary vein
I82.A12
Acute embolism and thrombosis of left axillary vein
I82.A13
Acute embolism and thrombosis of axillary vein, bilateral
I82.A21
Chronic embolism and thrombosis of right axillary vein
I82.A22
Chronic embolism and thrombosis of left axillary vein
I82.A23
Chronic embolism and thrombosis of axillary vein, bilateral
I82.B11
Acute embolism and thrombosis of right subclavian vein
I82.B12
Acute embolism and thrombosis of left subclavian vein
I82.B13
Acute embolism and thrombosis of subclavian vein, bilateral
I82.B21
Chronic embolism and thrombosis of right subclavian vein
I82.B22
Chronic embolism and thrombosis of left subclavian vein
I82.B23
Chronic embolism and thrombosis of subclavian vein, bilateral
I82.C11
Acute embolism and thrombosis of right internal jugular vein
I82.C12
Acute embolism and thrombosis of left internal jugular vein
I82.C13
Acute embolism and thrombosis of internal jugular vein,
bilateral
I82.C21
Chronic embolism and thrombosis of right internal jugular
vein
I82.C22
Chronic embolism and thrombosis of left internal jugular vein
I82.C23
Chronic embolism and thrombosis of internal jugular vein,
bilateral
O87.3
Cerebral venous thrombosis in the puerperium
Z79.01
Long term (current) use of anticoagulants
Z86.718
Personal history of other venous thrombosis and embolism
Z95.2
Presence of prosthetic heart valve
Coverage policy can be found in Pub. 100-03, Medicare National Coverage Determinations
Manual, Chapter 1, section 190.11 PT/INR.
(http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp
60.6 – Carrier Claims Requirements
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
Note this test is not covered as durable medical equipment. Therefore, claims submitted to
DMERCs will not be paid. It is covered under the physician fee schedule. Also note that the
cost of the device and supplies is included in the payment for G0249 and therefore not
separately billed to Medicare. G0249 continues to include materials for 4 tests. Additionally,
G0250 continues to mean per 4 tests and should be billed no more frequently than once every
4 weeks.
60.7 – Carrier Payment Requirements
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
Payment and pricing information will be in the Medicare Physician Fee Schedule Database
(MPFSDB). Pay for INR on the basis of the MPFS. Deductible and coinsurance apply.
60.8 – Carrier and Intermediary General Claims Processing Instructions

(Rev. 216, 06-25-04)
60.8.1 – Remittance Advice Notices
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
Use appropriate existing remittance advice reason and remark codes at the line level to
express the specific reason for denying payment for PT/INR:
Remittance Advice Remark Code N386, “This decision was based on a National Coverage
Determination (NCD). An NCD provides a coverage determination as to whether a particular
item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have Web access, you may contact
the contractor to request a copy of the NCD.”
If denying services furnished after July 1, 2002, use ASC X 12-835 claim adjustment reason
code 50, “These are non-covered services because this is not deemed a ‘medical necessity’ by
the payer.”
60.8.2 - Medicare Summary Notice (MSN) Messages
(Rev. 1562, Issued: 07-25-08, Effective: 03-19-08, Implementation: 08-25-08)
If denying services furnished after July 1, 2002, use MSN message:
“The following policies [190.11] were used when we made this decision.” (MSN Message
15.20)
60.12 - Coverage for PET Scans for Dementia and Neurodegenerative
Diseases
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Effective for dates of service on or after September 15, 2004, Medicare will cover FDG PET
scans for a differential diagnosis of fronto-temporal dementia (FTD) and Alzheimer's disease
OR; its use in a CMS-approved practical clinical trial focused on the utility of FDG-PET in
the diagnosis or treatment of dementing neurodegenerative diseases. Refer to Pub. 100-03,
NCD Manual, section 220.6.13, for complete coverage conditions and clinical trial
requirements and section 60.15 of this manual for claims processing information.
A. A/B MAC (A and B) Billing Requirements for PET Scan Claims for FDG-PET for the
Differential Diagnosis of Fronto-temporal Dementia and Alzheimer’s Disease:
CPT Code for PET Scans for Dementia and Neurodegenerative Diseases
Contractors shall advise providers to use the appropriate CPT code from section 60.3.1 for
dementia and neurodegenerative diseases for services performed on or after January 28, 2005.
Diagnosis Codes for PET Scans for Dementia and Neurodegenerative Diseases
The contractor shall ensure one of the following appropriate diagnosis codes is present on
claims for PET Scans for AD:
• ICD-10-CM is applicable, ICD-10 codes are: F03.90, F03.90 plus F05, G30.9,
G31.01, G31.9, R41.2 or R41.3

Medicare contractors shall deny claims when submitted with an appropriate CPT code from
section 60.3.1 and with a diagnosis code other than the range of codes listed above.
Medicare contractors shall instruct providers to issue an Advanced Beneficiary Notice to
beneficiaries advising them of potential financial liability prior to delivering the service if one
of the appropriate diagnosis codes will not be present on the claim.
The contractor shall use the following remittance advice messages and associated codes when
rejecting/denying claims under this policy. This CARC/RARC combination is compliant
with CAQH CORE Business Scenario Three.
Group Code: PR (if claim is received with a GA modifier) otherwise CO
CARC: 11
RARC: N/A
MSN: 16.48
Provider Documentation Required with the PET Scan Claim
Medicare contractors shall inform providers to ensure the conditions mentioned in the NCD
Manual, section 220.6.13, have been met. The information must also be maintained in the
beneficiary's medical record:
- Date of onset of symptoms;
- Diagnosis of clinical syndrome (normal aging, mild cognitive impairment or MCI:
mild, moderate, or severe dementia);
- Mini mental status exam (MMSE) or similar test score;
- Presumptive cause (possible, probably, uncertain AD);
- Any neuropsychological testing performed;
- Results of any structural imaging (MRI, CT) performed;
- Relevant laboratory tests (B12, thyroid hormone); and,
- Number and name of prescribed medications.
B. Billing Requirements for Beta Amyloid Positron Emission Tomography (PET) in
Dementia and Neurodegenerative Disease:
Effective for claims with dates of service on and after September 27, 2013, Medicare will
only allow coverage with evidence development (CED) for Positron Emission Tomography
(PET) beta amyloid (also referred to as amyloid-beta (Aβ)) imaging (HCPCS A9586) or
(HCPCS Q9982) or (HCPCS Q9983) (one PET Aβ scan per patient).
Note: Please note that effective January 1, 2014 the following code A9599 will be updated
in the IOCE and HCPCS update. This code will be contractor priced.
Note: Please note that effective January 1, 2018 the following code A9599 is end-date.
Medicare Summary Notices, Remittance Advice Remark Codes, and Claim
Adjustment Reason Codes
Effective for dates of service on or after September 27, 2013, contractors shall return as
unprocessable/return to provider claims for PET Aβ imaging, through CED during a
clinical trial, not containing the following:
•
Condition code 30, and value code D4 (FI only)
•
Modifier Q0 as appropriate

•
CD-10 dx code Z00.6 (in either the primary/secondary position)
•
A PET HCPCS code (78811 or78814)
•
At least, one Dx code from the table below,
And one of these additional diagnoses is required in addition to Z00.6
F03.90
Unspecified dementia without behavioral disturbance
F03.91
Unspecified dementia with behavioral disturbance
F01.50
Vascular dementia without behavioral disturbance
F01.51
Vascular dementia with behavioral disturbance
F02.80
Dementia in other diseases classified elsewhere without behavioral
disturbance
F02.81
Dementia in other diseases classified elsewhere with behavioral
disturbance
G31.01
Pick's disease
G31.09
Other frontotemporal dementia
G31.85
Corticobasal degeneration
G31.83
Dementia with Lewy bodies
G31.84
Mild cognitive impairment, so stated
R41.1
Anterograde amnesia
R41.2
Retrograde amnesia
R41.3
Other amnesia (amnesia NOS, memory loss NOS)
and
• Aβ HCPCS code A9586 or Q9982 or Q9983)
Contractors shall return as unprocessable claims for PET Aβ imaging using the following
messages:
-Claim Adjustment Reason Code 4 – the procedure code is inconsistent with the modifier
used or a required modifier is missing.
Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF), if present.
Remittance Advice Remark Code N519 - Invalid combination of HCPCS modifiers.
Contractors shall line-item deny claims for PET Aβ , HCPCS code A9586 or Q9982
or Q9983, where a previous PET Aβ, HCPCS code A9586 or Q9982 or Q9983 is
paid in history using the following messages:
• CARC 149: “Lifetime benefit maximum has been reached for this service/benefit
category.”
• RARC N587: “Policy benefits have been exhausted”.
• MSN 20.12: “This service was denied because Medicare only covers this service
once a lifetime.”
• Spanish Version: “Este servicio fue negado porque Medicare sólo cubre este
servicio una vez en la vida.”
• Group Code: PR, if a claim is received with a GA modifier
• Group Code: CO, if a claim is received with a GZ modifier
66 - National Coverage Determination (NCDs) services that are considered
a significant cost for Medicare Advantage Plans
(Rev. 10229, Issued: 07-21-20 Effective: 10-01-20, Implementation: 10-05-20)
CMS is streamlining the editing for MA plans’ claims when it is determined that certain
services are being disallowed on MA plans that are considered a significant cost under section
422.109(a)(2) of title 42 of the Code of Federal Regulations. Original fee-for-service
Medicare will pay for services obtained by beneficiaries enrolled in Medicare Advantage
(MA) plans in this circumstance.
Consistent with §1862 (t)(2) of the Social Security Act, Medicare Administrative Contractors
will pay for identified significant cost services for Medicare beneficiaries enrolled in MA
plans. In addition 42 CFR §422.109, the Medicare payment for the services or benefit is made
directly by the A/B MAC to the provider furnishing the service or benefit in accordance with
original Medicare payment, rules, methods, and requirements.
Beneficiaries are liable for any applicable coinsurance amounts.
Cost for NCD services legislative changes in benefits for which CMS A/B MACs will not
make payment and are the responsibility of the M+C organization are:
I. Services necessary to diagnose a condition covered by the NCD or legislative
changes in benefits;
II. Most services furnished as follow up care to the NCD services or legislative
changes in benefits;
III. Any services that is already a Medicare-covered service and included in the
annual M+C capitation rate or previously, adjusted payments; and
IV. Any services, including costs of the NCD service or legislative change
in benefits, to the extent the M+C organization is already obligated to cover it as
an additional benefit under 42CFR §422.312 or supplemental benefit under 42
CFR §422.102.
66.1 – Institutional Billing for National Coverage Determination (NCDs)
services that are considered a significant cost for Medicare Advantage
(Rev. 10229, Issued: 07-21-20 Effective: 10-01-20, Implementation: 10-05-20)
A. Institutional Inpatient Billing for National Coverage Determination (NCDs) services that
are considered a significant cost for Medicare Advantage.
The Medicare contractors shall allow Condition Code (CC) 78 on any inpatient institutional
claims for Medicare Advantage beneficiaries when it is determined that certain services are
being disallowed on MA plans that are considered a significant cost under section
422.109(a)(2) of title 42 of the Code of Federal Regulations. Any current editing that doesn’t
allow this shall be updated to allow this scenario, unless there has been previous instructions
excluding certain conditions.
Note: Condition Code 78 = Newly covered Medicare service for which an HMO doesn't pay.
B. Institutional Outpatient Billing for National Coverage Determination (NCDs) services that
are considered a significant cost for Medicare Advantage

The Medicare contractors shall allow Condition Code (CC) 78 on any outpatient institutional
claims for Medicare Advantage beneficiaries when it is determined that certain services are
being disallowed on MA plans that are considered a significant cost under section
422.109(a)(2) of title 42 of the Code of Federal Regulations. Any current editing that doesn’t
allow this shall be updated to allow this scenario, unless there has been previous instructions
excluding certain conditions.
Note: Condition Code 78 = Newly covered Medicare service for which an HMO doesn't pay.
66.2 – Services Identified as having Significant Cost for Medicare
Advantage
(Rev. 10229, Issued: 07-21-20 Effective: 10-01-20, Implementation: 10-05-20)
Services Identified as having Significant cost under section 422.109(a)(2) of title 42 of the
Code of Federal Regulations Providers may bill the A/B MAC for these NCD services
provided to a MA beneficiary.
Services Identified as having Significant cost
Service/Benefit
Revenue
Code
HCPCS
ICD-10-
PCS
Procedure
Significant
Cost Start
Significant
Cost End
CAR-T
0891
Q2041,
Q2042
XW033C3
or
XW043C3
08/07/2019
12/31/2020
67 – No Cost Items
(Rev. 1147, Issued: 01-05-07, Effective: 11-06-06, Implementation: 02-05-07)
On occasion, providers may receive an item (such as a device or drug) that is offered by a
manufacturer/supplier free of charge. Such items, for purposes of these instructions, are
considered “no cost items.” Providers are not to seek reimbursement for no cost items as
noted in Section 1862(a)(2) of the Social Security Act.
67.1 – Practitioner Billing for No Cost Items
(Rev. 1657, Issued: 12-31-08, Effective: 01-01-09, Implementation: 01-05-09)
Practitioners typically should not bill for no cost items as there is no non-covered charges
field on the claim and there are also no system edits in place to require providers to do so.
However, practitioners are required to report Category A IDE devices received at no cost on
claims as specified in §68.3 of this chapter (although they will not receive payment).
67.2 – Institutional Billing for No Cost Items
(Rev. 4013, Issued: 03-30-18, Effective: 01-01-09, Implementation: 06-29-18)
Generally speaking, institutional, providers should not have to report the usage of a no cost item.
However, for some claims (e.g., hospital Outpatient Prospective Payment System (OPPS) claims),
providers may be required to bill a no cost item due to claims processing edits that require an item
(even if received at no cost) to be billed along with an associated service (e.g., a specified device
must be reported along with a specified implantation procedure).
For OPPS claims, when a drug is provided at no cost, claims processing edits prevent drug
administration charges from being billed when the claim does not contain a covered/billable drug
charge. Therefore, for drugs provided at no cost in the hospital outpatient department, providers
must report the applicable drug HCPCS code and appropriate units with a token charge of less

than $1.01 for the item in the covered charge field and mirror this less than $1.01 amount reported
in the noncovered charge field. Providers must also bill the corresponding drug administration
charge with the appropriate drug administration CPT or HCPCS code.
For OPPS claims, providers must report a token charge of less than $1.01 for the item in the
covered charge field, along with the applicable HCPCS modifier (i.e., modifier –FB) appended to
the procedure code that reports the service requiring a device. For more information on billing no
cost items under the OPPS, refer to Chapter 4, §20.6.9 and 61.3.1 of this manual.
By billing in this way, the provider is accomplishing four things:
1) Communicating to the contractor that the provider is not seeking payment for the no cost
item;
2) Reflecting, with completeness and accuracy, all services provided to the patient;
3) Preventing the line item or claim from being rejected/denied by system edits that require
an item to be billed in conjunction with an associated procedure (such as implantation or
administration procedures);
4) Assuring that the patient and provider are not held liable for any charges for the no cost
item.
Future updates will be issued in a Recurring Update Notification.
67.2.1 – Billing No Cost Items Due to Recall, Replacement, or Free Sample
(Rev. 3181, Issued: 01-30-15, Effective: 07-01-15, Implementation: 07-06-15)
Currently, institutional providers that use the Healthcare Common Procedural Coding System
(HCPCS) bill device HCPCS codes for no cost or full credit items with token charges in order
for claims to pass OPPS claims processing edits that require certain devices to be billed with
their associated procedures so that payment can be made.
Effective January 1, 2006, modifier –FB is used to indicate that an item used in a procedure
was furnished without cost to the provider, and, therefore, it is not being charged to Medicare
or the beneficiary. More information on billing HCPCS modifier –FB can be located in
Chapter 4, §20.6.9 and 61.3.1 of this manual.
Effective April 1, 2006, two new condition codes were created for institutional use: 49 and 50
(Table 1). These new codes are used to identify and track medical devices that are provided
by a manufacturer at no cost or with full credit to the hospital due to warranty for a
malfunction or recall.
Table 1: New Condition Codes and Descriptions
Condition Code
Description
49
Product Replacement
within Product
Lifecycle
Replacement of a product earlier than the anticipated
lifecycle.
50
Product Replacement
for Known Recall of a
Product
Manufacturer or FDA has identified the product for recall
and therefore replacement.
• Providers must use these condition codes to identify medical devices that are provided by
a manufacturer at no cost or with full credit due to warranty or recall. These condition
codes will be used to track no cost/full credit devices replaced due to recall or warranty.

• Providers must report these condition codes on any inpatient or outpatient institutional
claim that includes a no cost/full credit replacement device when conditions of warranty
or recall are met.
NOTE: OPPS hospitals billing no cost/full credit devices must append modifier –FB to the
procedure code for implanting the no cost/full credit device, along with the appropriate
condition code if applicable (in Table 1 above), in instances when claims processing edits
require that certain devices be billed with their associated procedures. The modifier identifies
the procedure code line for the no cost/full credit device, while the condition code explains if
the device was provided free of cost due to warranty or recall.
Effective January 1, 2014, an additional new condition code was created for institutional use:
53 (Table 2). This new code is used to identify and track medical devices that are provided
by a manufacturer at no cost or with full credit to the hospital due a clinical trial or a free
sample.
Table 2: New Condition Codes and Descriptions
Condition Code
Description
49
Product Replacement
within Product
Lifecycle
Replacement of a product earlier than the anticipated
lifecycle.
50
Product Replacement
for Known Recall of a
Product
Manufacturer or FDA has identified the product for recall
and therefore replacement.
53
Initial placement of a
medical device
provided as part of a
clinical trial or free
sample
Code is for outpatient claims that have received a device
credit upon initial medical device placement in a clinical
trial or a free sample.
• Providers must use these condition codes to identify medical devices that are provided by
a manufacturer at no cost or with full credit due to warranty, recall, or free sample. These
condition codes will be used to track no cost/full credit devices replaced due to recall,
warranty, or free sample.
• Providers must report these condition codes on any inpatient or outpatient institutional
claim that includes a no cost/full credit replacement device when conditions of warranty,
recall, or free sample are met.
NOTE: OPPS hospitals billing no cost/full credit devices are no longer required to append
modifier –FB to the procedure code for implanting the no cost/full credit device, along with
the appropriate condition code if applicable (in Table 2 above), in instances when claims
processing edits require that certain devices be billed with their associated procedures.
68 – Investigational Device Exemption (IDE) Studies
(Rev. 3105, Issued: 11-06-14, Effective: 01-01-15, Implementation: 01-05-15)
See Pub. 100-02, Medicare Benefit Policy Manual, Chapter 14 for complete Medicare
coverage requirements for items and services in Category A and B IDE studies, related to
these billing requirements.
NOTE: For information regarding Medicare coverage related to IDEs in Medicare
Advantage plans, refer to Pub. 100-16, Medicare Managed Care Manual, chapter 4, section
10.7.2.

68.1 – Billing Requirements for Providers Billing for Routine Care Items
and Services in Category A IDE Studies
(Rev. 3105, Issued: 11-06-14, Effective: 01-01-15, Implementation: 01-05-15)
A. Institutional Inpatient and Outpatient Billing in Category A IDE Studies
Routine Care Items and Services
Institutional providers shall submit claims only for routine care items and services in
Category A IDE device studies approved by CMS (or its designated entity) and listed on the
CMS Coverage Website, by billing according to the clinical trial billing instructions found in
§69.6 of this chapter, and as described below under subsection C (“General Billing
Requirements”). The Category A IDE device shall not be reported on institutional claims
since Category A IDE devices are not eligible for payment under Medicare.
B. Practitioner Billing in Category A IDE Studies
Routine Care Items and Services
Practitioners shall submit claims for the routine care items and services in Category A IDE
studies approved by CMS (or its designated entity) and listed on the CMS Coverage Website,
by billing according to the clinical trial billing instructions found in §69.6 of this chapter, and
as described below under subsection C (“General Billing Requirements”). The Category A
IDE device shall not be reported on practitioner claims since Category A IDE devices are not
eligible for payment under Medicare.
C. General Billing Requirements
Effective for claims with dates of service on or after January 1, 2014, it is mandatory to
report a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under coverage with evidence development (CED). This is the
number assigned by the National Library of Medicine (NLM) ClinicalTrials.gov Website
when a new study appears in the NLM Clinical Trials data base. This number is listed
prominently on each specific study’s page and is always preceded by the letters “NCT.”
Contractors verify the validity of a trial/study/registry by consulting CMS’s Coverage
Website at: http://www.cms.gov/Center/Special-Topic/Medicare-Coverage-
Center.html?redirect=/center/coverage.asp. Providers report the 8-digit number on the
following claims locators:
CMS-1500 paper form-place in Field 19 (preceded by ‘CT’); or
837 P—Loop 2300, REF02, REF01=P4 (do not use ‘CT’ on the electronic claim)
In addition to the clinical trial number, claims shall include:
ICD-9 diagnosis code V70.7/ICD-10 diagnosis code Z00.6 (in either the primary/secondary
positions)
HCPCS modifier Q0 or Q1 as appropriate
Claims submitted without a clinical trial number shall be returned as unprocessable reporting
the following messages:
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT.)”

RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption number for
FDA-approved clinical trial services.”
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
Group Code - Contractual Obligation (CO)
Effective for dates of service on or before December 31, 2007, practitioners must place a QV
modifier (Item or service provided as routine care in a Medicare qualifying clinical trial) on
the line for the device along with the IDE number.
Effective for dates of service on or after January 1, 2008, practitioners will no longer bill a
QV modifier to identify the device. Instead, practitioners will bill a Q0 (numeral 0 versus the
letter O) modifier (Investigational clinical service provided in a clinical research study that is
in an approved clinical research study) along with the IDE number.
The following table shows the designated field locations to report the Category A IDE
number on practitioner claims:
Data
CMS-1500
837i and 837p
IDE #
Item 23
Segment 2300,
REF02(REF01=LX)
Contractors will validate the IDE number for the Category A device when modifier Q0 is
submitted on the claim along with the IDE number. Claims containing an invalid IDE
number will be returned to the provider using the following messages:
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption Number for
FDA approved clinical trial services.”
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT).”
68.2 – Billing Requirements for Providers Billing for Category B IDE
Devices and Routine Care Items and Services in Category B IDE Studies
(Rev. 3105, Issued: 11-06-14, Effective: 01-01-15, Implementation: 01-05-15)
Payment for the device may not exceed the Medicare-approved amount for a comparable
device that has been already FDA-approved.
A. Institutional Inpatient Billing for Items and Services in Category B IDE Studies
Routine Care Items and Services
Institutional providers shall submit claims for the routine care items and services in Category
B IDE studies approved by CMS (or its designated entity) and listed on the CMS Coverage
Website, by billing according to the clinical trial billing instructions found in §69.6 of this
chapter, and as described below under subsection D (“General Billing Requirements”).
Category B Device

Institutional providers must bill the Category B IDE number on a 0624 revenue code line with
charges in the covered charges field. Hospital inpatient providers should not bill for the
Category B IDE device if receiving the device free-of-charge.
B. Institutional Outpatient Billing for Items and Services in Category B IDE Studies
Routine Care Items and Services
Institutional providers shall submit claims for the routine care items and services in Category
B IDE studies approved by CMS (or its designated entity) and listed on the CMS Coverage
Website, by billing according to the clinical trial billing instructions found in section 69.6 of
this chapter, and as described below under subsection D (“General Billing Requirements”).
Category B Device
On a 0624 revenue code line, institutional providers must bill the following for Category B
IDE devices for which they incur a cost:
• Category B IDE device HCPCS code, if applicable
• Appropriate HCPCS modifier:
o Q0 or Q1 as appropriate for claims with dates of service on or after January 1,
2014; or
o Q0 (numeral 0 versus the letter O) modifier for claims with dates of service on
or after January 1, 2008; or,
o QA modifier for claims with dates of service prior to January 1, 2008.
• Category B IDE number
• Charges for the device billed as covered charges
NOTE: If the Category B IDE device is provided at no cost, outpatient prospective payment
system (OPPS) providers must report a token charge in the covered charge field along with
the applicable HCPCS modifier (i.e., modifier – FB) appended to the procedure code that
reports the service to furnish the device, in instances when claims processing edits require
that certain devices be billed with their associated procedures. For more information on
billing ‘no cost items’ under the OPPS, refer to chapter 4, §§20.6.9 and 61.3.1 of this manual.
C. Practitioner Billing for Items and Services in Category B IDE Studies
Routine Care Items and Services
Practitioners shall submit claims for routine care items and services in Category B IDE
studies approved by CMS (or its designated entity) and listed on the CMS Coverage Website,
by billing according to the clinical trial billing instructions found in section 69.6 of this
chapter, and as described below under subsection D (“General Billing Requirements”).
Category B Device
Effective for dates of service on or before December 31, 2007, practitioners must bill the
Category B IDE device on a line with a QA modifier (FDA IDE) along with the IDE number.
However, effective for dates of service on or after January 1, 2008, practitioners will no

longer bill a QA modifier to identify a Category B device. Instead, practitioners will bill a Q0
modifier (numeral 0 versus the letter O) (Investigational clinical service provided in a clinical
research study that is in an approved clinical research study) along with the IDE number.
The following table shows the designated field locations to report the Category B IDE
number on institutional and practitioner claims:
Data
CMS-1450
CMS-1500
837i and 837p
IDE #
FL 43
Item 23
Segment 2300,
REF02(REF01=LX)
Contractors will validate the IDE number for the Category B device when modifier Q0 is
submitted on the claim along with the IDE number. Claims containing an invalid IDE
number will be returned to the provider using the following messages:
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption Number for
FDA approved clinical trial services.”
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT.”
D. General Billing Requirements
Effective for claims with dates of service on or after January 1, 2014, it is mandatory to report
a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under CED. This is the number assigned by the NLM
ClinicalTrials.gov Website when a new study appears in the NLM Clinical Trials data base.
This number is listed prominently on each specific study’s page and is always preceded by
the letters “NCT.” Contractors verify the validity of a trial/study/registry by consulting
CMS’s Coverage Website at: http://www.cms.gov/Center/Special-Topic/Medicare-Coverage-
Center.html?redirect=/center/coverage.asp. Providers report the 8-digit number on the
following claims locators:
• CMS-1500 paper form-place in Field 19 (preceded by ‘CT’); or
• 837 P—Loop 2300, REF02, REF01=P4 (do not use ‘CT’ on the electronic claim).
In addition to the clinical trial number, claims shall include:
• ICD-9 diagnosis code V70.7/ICD-10 diagnosis code Z00.6 (in either the
primary/secondary positions)
• HCPCS modifier Q0 or Q1 as appropriate
Claims submitted without a clinical trial number shall be returned as unprocessable reporting
the following messages:
• CARC 16: “Claim/service lacks information which is needed for adjudication. At least
one Remark Code must be provided (may be comprised of either NCPDP Reject
Reason Code, or Remittance Advice Remark Code that is not an ALERT.)”
• RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption
number for FDA-approved clinical trial services.”

• RARC MA130: “Your claim contains incomplete and/or invalid information, and no
appeal rights are afforded because the claim is unprocessable. Please submit a new
claim with the complete/correct information.”
Group Code-Contractual Obligation (CO)
68.4 – Billing Requirements for Providers Billing Routine Costs of Clinical
Trials Involving a Category B IDE
(Rev. 12571; Issued: 04-11-24) Effective: 10-11-23; Implementation: 05-13-24)
As noted above in section 68.2, of this chapter, providers shall first notify their contractor of
the IDE device trial before submitting claims for Category B IDE devices and the routine
costs of clinical trials involving Category B IDE devices. Once the contractor notifies the
provider that all required information for the IDE has been furnished, the provider may bill
Category B IDE claims.
When billing for Category B IDEs, providers shall bill for the device and all related
procedures. The Category B IDE device and the routine costs associated with its use are
eligible for payment under Medicare. (Payment for the device may not exceed the Medicare-
approved amount for a comparable device that has been already FDA-approved.)
Institutional Inpatient Billing
Routine Costs
Institutional providers shall submit claims for the routine costs of a clinical trial involving a
Category B IDE device by billing according to the clinical trial billing instructions found in
§69.6 of this chapter.
Category B Device
Institutional providers must bill the Category B IDE number on a 0624 revenue code line with
charges in the covered charges field. Hospital inpatient providers should not bill for the
Category B IDE device if receiving the device free-of-charge.
Institutional Outpatient Billing
Routine Costs
Institutional providers shall submit claims for the routine costs of a clinical trial involving a
Category B IDE device by billing according to the clinical trial billing instructions found in
section 69.6 of this chapter.
Category B Device
On a 0624 revenue code line, institutional providers must bill the following for Category B
IDE devices for which they incur a cost:
• Category B IDE device HCPCS code, if applicable.
• Appropriate HCPCS modifier:
• Q0 or Q1 as appropriate for claims with dates of service on or after January 1,
2014; or

• Q0 (numeral 0 versus the letter O) modifier for claims with dates of service on or
after January 1, 2008; or
• QA modifier for claims with dates of service prior to January 1, 2008.
• Category B IDE number
• Charges for the device billed as covered charges
NOTE: For claims prior to January 1, 2014, if the Category B IDE device is provided at no
cost, outpatient prospective payment system (OPPS) providers must report a token
charge in the covered charge field along with the applicable HCPCS modifier (i.e.,
modifier –FB) appended to the procedure code that reports the service to furnish
the device, in instances when claims processing edits require that certain devices
be billed with their associated procedures. For more information on billing ‘no
cost items’ under the OPPS, refer to Chapter 4, §§20.6.9 and 61.3.1 of this
manual.
Effective January 1, 2014, if the Category B IDE device is provided at no cost,
outpatient prospective payment system (OPPS) providers must report a token
charge in the covered charge field along with condition code “53” and Value Code
“FD”. For more information on billing ‘no cost items’ under the OPPS, refer to
Chapter 4, §§20.6.9 and 61.3.1 of this manual.
Practitioner Billing
Routine Costs
Practitioners shall submit claims for the routine costs of a clinical trial involving a Category B
IDE device by billing according to the clinical trial billing instructions found in section 69.6
of this chapter.
Category B Device
Effective for claims with dates of service on or after January 1, 2014, it is mandatory to
report a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under CED. Providers report the 8-digit number on the following
claims locators:
• 837 professional claim format (do not use ‘CT’ on the electronic claim) or,
• CMS-1500 paper form-place in Field 19 (preceded by ‘CT’).
In addition to the clinical trial number, claims shall include (in either the primary/secondary
positions):
• If ICD-9-CM is applicable, ICD-9 diagnosis code V70.7
• If ICD-10-CM is applicable, ICD-10 diagnosis code Z00.6
• HCPCS modifier Q0 or Q1 as appropriate
Claims submitted without a clinical trial number shall be returned as unprocessable reporting
the following messages:

CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT.)”
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption number for
FDA-approved clinical trial services.”
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
Group Code-Contractual Obligation (CO)
Effective for dates of service on or before December 31, 2007, practitioners must bill the
Category B IDE device on a line with a QA modifier (FDA IDE) along with the IDE number.
However, effective for dates of service on or after January 1, 2008, practitioners will no
longer bill a QA modifier to identify a Category B device. Instead, practitioners will bill a Q0
modifier (numeral 0 versus the letter O) (Investigational clinical service provided in a clinical
research study that is in an approved clinical research study) along with the IDE number.
The following table shows the designated field locations to report the Category B IDE
number on institutional and practitioner claims:
Data
CMS-1450
CMS-1500
837 institutional claim format and
837 professional claim format
IDE #
Revenue Code
Description field
Item 23
Segment 2300,
REF02(REF01=LX)
Contractors will validate the IDE number for the Category B device when modifier Q0 is
submitted on the claim along with the IDE number. Claims containing an invalid IDE
number will be returned to the provider using the following messages:
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption Number for
FDA approved clinical trial services.”
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT.”
Claims that are submitted without the ‘Q0’ modifier will be returned with the following
messages:
CARC 16 - Claim/service lacks information or has submission/billing error(s). Usage: Do not
use this code for claims attachment(s)/other documentation. At least one Remark Code must
be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance
Advice Remark Code that is not an ALERT.) Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF), if present.
RARC N822 – Missing procedure modifier(s).
69 - Qualifying Clinical Trials
(Rev. 487, Issued: 03-04-05, Effective and Implementation: N/A)
69.1 – General

(Rev. 1147, Issued: 01-05-07, Effective: 11-06-06, Implementation: 02-05-07)
The CMS has issued a National Coverage Determination (NCD) which allows Medicare
coverage for the routine costs of qualifying clinical trial services as well as reasonable and
necessary items and services used to diagnose and treat complications arising from
participation in all clinical trials. The coverage requirements for routine costs of qualifying
clinical trial services are contained in The National Coverage Determinations Manual, Section
310.1.
69.2 - Payment for Qualifying Clinical Trial Services
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
For dates of service on or after September 19, 2000, pay for covered services furnished to
beneficiaries participating in qualifying clinical trials. Payment is based on the payment
methodology applicable for the service that was furnished (e.g., physician fee schedule, lab
fee schedule, durable medical equipment fee schedule, reasonable charge, etc.). With the
exception of managed care enrollees, applicable deductibles and coinsurance rules apply to
clinical trial items and services. The Part A and Part B deductibles are assumed to be met for
covered clinical trial services billed on a fee service basis for managed care enrollees.
NOTE: Effective for claims with dates of service on or after January 1, 2014, it is
mandatory to report a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under CED. This is the number assigned by the National Library of
Medicine (NLM) ClinicalTrials.gov Web site when a new study appears in the NLM Clinical
Trials data base. This number is listed prominently on each specific study’s page and is
always preceded by the letters “NCT.” Contractors verify the validity of a trial/study/registry
by consulting CMS’s clinical trials/registry web site at:
http://www.cms.gov/Medicare/Medicare-General-
Information/MedicareApprovedFacilitie/index.html.
NOTE: Contractors shall ensure value code ‘D4’/amount data from their internal claims
processing is mapped/populated to the 837 institutional claim format for a coordination of
benefits 837 institutional claim.
69.3 - Medical Records Documentation Requirements
(Rev. 487, Issued: 03-04-05, Effective and Implementation: N/A)
The billing provider must include in the beneficiary's medical record the following
information: trial name, sponsor, and sponsor-assigned protocol number. This information
does not need to be submitted with the claim but must be provided if requested for medical
review.
69.4 - Local Medical Review Policy
(Rev. 487, Issued: 03-04-05, Effective and Implementation: N/A)
Do not develop new or revised LMRPs for clinical trial services. Clinical trial services that
meet the requirements of the NCD are considered reasonable and necessary.
69.5 - Billing Requirements – General
(Rev. 2955, Issued: 05-14-14, Effective, 01-01-14, Implementation, 01- 06-14)
Instruct practitioners and institutional providers to enter clinical trial and non-clinical trial
services on separate line items when billing both types of services on the same claim. For
services that require a Certificate of Medical Necessity (CMN), continue to require CMNs.
Items and services provided free-of-charge by research sponsors generally may not be billed

to be paid by Medicare, and providers are not required to submit the charge to Medicare. If it
is necessary for a provider to show the items and services that are provided free-of-charge in
order to receive payment for the covered routine costs (e.g. administration of a non-covered
chemotherapeutic agent), providers are instructed to submit such charges as non-covered at
the time of entry, while also assuring that the beneficiary is not held liable. This instruction
applies to all hospitals including hospitals located in Maryland under the jurisdiction of the
Health Services Cost Review Commission (HSCRC).
For OPPS claims, providers must report a token charge for a ‘no cost’ item in the covered
charge field along with the applicable HCPCS modifier (i.e., modifier –FB) appended to the
procedure code that reports the service provided to furnish the ‘no cost’ item, in instances
when claims processing edits require that certain devices be billed with their associated
procedures. For more information on billing ‘no cost’ items under the OPPS, refer to Chapter
4, §§20.6.9 and 61.3.1 of this manual.
NOTE: Effective for claims with dates of service on or after January 1, 2014, it is
mandatory to report a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under CED.
Future updates will be issued in a Recurring Update Notification.
69.6 - Requirements for Billing Routine Costs of Clinical Trials
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
Routine Costs Submitted by Practitioners/Suppliers
Claims with dates of service on or after January 1, 2008:
• HCPCS modifier ‘Q1’ (numeral 1 instead of the letter i) ; and,
• If ICD-9-CM is applicable, ICD-9 diagnosis code V70.7 (Examination of participant
in clinical trial) reported as the secondary diagnosis (effective September 19, 2000,
diagnosis code V70.7 can be reported as either primary or secondary).
• If ICD-10-CM is applicable, ICD-10 diagnosis code Z00.6
CMS covers costs of healthy volunteers in a qualified clinical trial if it meets the following
conditions:
• The trial is not designed exclusively to test toxicity or disease pathophysiology.
• The trial must have therapeutic intent.
• If the trial has therapeutic interventions, it must enroll patients with diagnosed disease
rather than healthy volunteers.
• If the trial is studying diagnostic interventions, it may enroll healthy patients in order
to have a proper control group.
Effective for claims processed after September 28, 2009, with dates of service on or after
January 1, 2008, claims submitted with modifier Q1 shall be returned as unprocessable if

ICD-9-CM code V70.7 (if ICD-9 is applicable) or ICD-10-CM code Z00.6 (if ICD-10-CM is
applicable) is not submitted on the claim.
Contractors shall return the following messages:
Claims adjustment Reason Code 16: “Claim/service lacks information which is needed for
adjudication. As least one Remark Code must be provided (may be comprised of either the
Remittance Advice Code or NCPDP Reject Reason Code).”
Remittance Advice Remark Code M76: “Missing/incomplete/invalid diagnosis or condition.”
Effective for clinical trial claims received after April 1, 2008, (regardless of the date of
service) providers can begin to report an 8-digit clinical trial number. The reporting of this
number is voluntary through December 31, 2013. Refer to change request (CR) 5790 for
more information regarding the 8-digit number.
Effective for claims with dates of service on or after January 1, 2014 it is mandatory to
report a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under CED. Providers report the 8-digit number on the following
claims locators:
• 837 professional claim format-Loop 2300 REF02 (REF01=P4) (do not use ‘CT’ on
the electronic claim); or
• CMS-1500 paper form-place in Field 19 (preceded by ‘CT’).
In addition to the clinical trial number, claims should include:
• If ICD-9-CM is applicable, ICD-9 diagnosis code V70.7
• If ICD-10-CM is applicable, ICD-10 diagnosis code Z00.6 (in either the
primary/secondary positions)
• HCPCS modifier Q0 or Q1 as appropriate
Practitioner claims submitted without a clinical trial number shall be returned as
unprocessable using the following messages:
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT.)”
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption number for
FDA-approved clinical trial services.”
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
Group Code-Contractual Obligation (CO)
Routine Costs Submitted by Institutional Providers
All Institutional Clinical Trial Claims

Effective for clinical trial claims received after April 1, 2008, (regardless of the date of
service) providers can begin to report an 8-digit clinical trial number. The reporting of this
number is voluntary thru December 31, 2013. Refer to CR 5790 for more information
regarding the 8-digit number. To bill the 8-digit clinical trial number, institutional providers
shall code value code ‘D4’---where the value code amount equals the 8-digit clinical trial
number. Below are the claim locators in which to bill the 8-digit number:
• 837 institutional claim format-Loop 2300 REF02 (REF01=P4)
• Paper CMS-1450 value code ‘D4’
NOTE: Effective for claims with dates of service on or after January 1, 2014, it is
mandatory to report a clinical trial number on claims for items/services provided in clinical
trials/studies/registries, or under CED. Institutional claims submitted without a clinical trial
number shall be return to providers.
NOTE: The Q1 modifier is line item specific and must be used to identify items and services
that constitute medically necessary routine patient care or treatment of complications arising
from a Medicare beneficiary’s participation in a Medicare-covered clinical trial. Items and
services that are provided solely to satisfy data collection and analysis needs and that are not
used in the clinical management of the patient are not covered and may not be billed using the
Q1 modifier. Items and services that are not covered by Medicare by virtue of a statutory
exclusion or lack of a benefit category also may not be billed using the Q1 modifier. When
billed in conjunction with the V70.7/Z00.6 diagnosis code, the Q1 modifier will serve as the
provider’s attestation that the service meets the Medicare coverage criteria (i.e., was furnished
to a beneficiary who is participating in a Medicare qualifying clinical trial and represents
routine patient care, including complications associated with qualifying trial participation).
Inpatient Clinical Trial Claims
Institutional providers billing clinical trial service(s) must report ICD-9 diagnosis code V70.7
if ICD-9 is applicable or, if ICD-10-CM is applicable, ICD-10 diagnosis code Z006 in either
the primary or secondary position and a condition code 30 regardless of whether all services
are related to the clinical trial or not.
NOTE: HCPCS codes are not reported on inpatient claims. Therefore, the HCPCS modifier
requirements (i.e., Q0/Q1) as outlined in the outpatient clinical trial section immediately
below, are not applicable to inpatient clinical trial claims.
Outpatient Clinical Trial Claims
On all outpatient clinical trial claims, providers need to do the following:
• Report condition code 30,
• Report ICD-9 diagnosis code V70.7, if ICD-9-CM is applicable, in the primary or
secondary position;
• Report ICD-10 diagnosis code Z00.6, if ICD-10-CM is applicable, in the primary or
secondary position; and
• Identify all lines that contain an investigational item/service with a HCPCS modifier
of:
o Q0 for dates of service on or after 1/1/08
• Identify all lines that contain a routine service with a HCPCS modifier of:
o Q1 for dates of service on or after 1/1/08.
For clinical trial billing requirements for patients enrolled in a managed care plan, please refer
to Section 69.9 of this chapter.
69.7 - Reserved for Future Use
(Rev. 1418, Issued: 01-18-08, Effective: 01-01-08, Implementation: 04-07-08)
69.8 - Handling Erroneous Denials of Qualifying Clinical Trial Services
(Rev. 487, Issued: 03-04-05, Effective and Implementation: N/A)
If a service Medicare covers was billed with the appropriate clinical trial coding but was
inadvertently denied (e.g., for medical necessity or utilization) and is subsequently brought to
your attention, adjust the denied claim. If the denied services weren’t properly coded as
clinical trial services, instruct the provider to resubmit the service on a new claim with
appropriate clinical trial coding.
69.9 - Billing and Processing Fee for Service Claims for Covered Clinical
Trial Services Furnished to Managed Care Enrollees
(Rev. 1723, Issued: 05-01-09, Effective: 10-01-09, Implementation: 10-05-09)
For dates of service on or after September 19, 2000, and until notified otherwise by CMS,
Medicare contractors will pay for covered clinical trial services furnished to beneficiaries
enrolled in managed care plans. Providers who furnish covered clinical trial services to
managed care beneficiaries must be enrolled with Medicare in order to bill on a fee-for-
service basis. Providers that wish to bill fee for service but have not enrolled with Medicare
must contact their local carrier, intermediary, regional home health intermediary or National
Supplier Clearinghouse, as appropriate, to obtain an enrollment application.
Determine payment for covered clinical trial services furnished to beneficiaries enrolled in
managed care plans in accordance with applicable fee for service rules, except that
beneficiaries are not responsible for the Part A or Part B deductibles (i.e., assume the Part A
or Part B deductible has been met). Managed care enrollees are liable for the coinsurance
amounts applicable to services paid under Medicare fee for service rules.
The clinical trial coding requirements for managed care enrollee claims are the same as those
for regular Medicare fee for service claims. However, for beneficiaries enrolled in a managed
care plan, institutional providers must not bill outpatient clinical trial services and non-
clinical trial services on the same claim. If covered outpatient services unrelated to the
clinical trial are rendered during the same day/stay, the provider must split-bill so that ONLY
the clinical trial services are contained on a single claim and billed as fee-for-service (this
allows the Medicare claims processing system to not apply deductible when the patient is
found to be in a managed care plan). Any outpatient services unrelated to the clinical trial
should be billed to the managed care plan.
69.10 - CWF Editing Of Clinical Trial Claims For Managed Care Enrollees
(Rev. 487, Issued: 03-04-05, Effective and Implementation: N/A)
Submit clinical trial services for managed care enrollees to CWF for payment approval. CWF
will not reject clinical trial claims for managed care enrollees when all services on the claim
transaction record are coded as clinical trial services and the date(s) of service is (are) on or
after September 19, 2000. In addition, CWF will not apply Part B deductible to clinical trial
claims for managed care enrollees (i.e., CWF will process clinical trial services for managed
care enrollees as if the Part B deductible has already been met).
69.11 - Resolution of CWF UR 5232 Rejects
(Rev. 487, Issued: 03-04-05, Effective and Implementation: N/A)
If you send a claim transaction to CWF that includes both clinical and non-clinical trial
services for a managed care enrollee, the entire claim will be rejected with the UR 5232 error
code. When you receive a UR 5232 error code split the claim and resubmit the clinical trial
portion to CWF. Process the non-clinical trial portion of the rejected claims in the same
manner that other non-clinical trial fee for service claims for managed care enrollees are
handled.
70 - Billing Requirements for Islet Cell Transplantation for Beneficiaries in
a National Institutes of Health (NIH) Clinical Trial
(Rev. 986, Issued: 06-16-06, Effective: 05-01-06, Implementation: 07-31-06)
For services performed on or after October 1, 2004, Medicare will cover islet cell
transplantation for patients with Type I diabetes who are participating in an NIH sponsored
clinical trial. See Pub 100-04 (National Coverage Determinations Manual) section 260.3.1
for complete coverage policy.
The islet cell transplant may be done alone or in combination with a kidney transplant. Islet
recipients will also need immunosuppressant therapy to prevent rejection of the transplanted
islet cells. Routine follow-up care will be necessary for each trial patient. See Pub 100-04,
section 310 for further guidance relative to routine care. All other uses for islet cell services
will remain non-covered.
70.1 - Healthcare Common Procedure Coding System (HCPCS) Codes for
Carriers
(Rev. 261, Issued: 07-30-04, Effective: 10-01-04, Implementation: 10-04-04)
G0341: Percutaneous islet cell transplant, includes portal vein catheterization and infusion
Short Descriptor: Percutaneous islet cell trans
Type of Service: 2
G0342: Laparoscopy for islet cell transplant, includes portal vein catheterization and infusion
Short Descriptor: Laparoscopy islet cell trans
Type of Service: 2
G0343: Laparotomy for islet cell transplant, includes portal vein catheterization and infusion
Short Descriptor: Laparotomy islet cell transp
Type of Service: 2
70.2 - Applicable Modifier for Islet Cell Transplant Claims for Carriers
(Rev. 986, Issued: 06-16-06, Effective: 05-01-06, Implementation: 07-31-06)
Carriers shall instruct physicians to bill using the above procedure code(s) with modifier QR
(Item or service provided in a Medicare-specified study) for all claims for islet cell
transplantation and routine follow-up care related to this service.
70.3 - Special Billing and Payment Requirements for Carriers
(Rev. 261, Issued: 07-30-04, Effective: 10-01-04, Implementation: 10-04-04)

Payment and pricing information will be on the October 2004 update of the Medicare
Physician Fee Schedule Database (MPFSDB). Pay for islet cell transplants on the basis of the
MPFS. Deductible and coinsurance apply for fee-for-service beneficiaries.
70.4 - Special Billing and Payment Requirements for A/B MACs (A)
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
If ICD-10 is applicable, ICD-10-PCS codes for the clinical trial are:
ICD-10-PCS
Code
Code Description
3E030U1
Introduction of Nonautologous Pancreatic Islet Cells into
Peripheral Vein, Open Approach
3E033U1
Introduction of Nonautologous Pancreatic Islet Cells into
Peripheral Vein, Percutaneous Approach
3E0J3U1
Introduction of Nonautologous Pancreatic Islet Cells into Biliary
and Pancreatic Tract, Percutaneous Approach
3E0J7U1
Introduction of Nonautologous Pancreatic Islet Cells into Biliary
and Pancreatic Tract, Via Natural or Artificial Opening
3E0J8U1
Introduction of Nonautologous Pancreatic Islet Cells into Biliary
and Pancreatic Tract, Via Natural or Artificial Opening
Endoscopic
E10.9
Type 1 diabetes mellitus without complications
E10.65
Type 1 diabetes mellitus with hyperglycemia
E10.10
Type 1 diabetes mellitus with ketoacidosis without coma
E10.69
Type 1 diabetes mellitus with other specified complication
E10.21
Type 1 diabetes mellitus with diabetic nephropathy
E10.22
Type 1 diabetes mellitus with diabetic chronic kidney disease
E10.29
Type 1 diabetes mellitus with other diabetic kidney complication
E10.311
Type 1 diabetes mellitus with unspecified diabetic retinopathy with macular edema
E10.319
Type 1 diabetes mellitus with unspecified diabetic retinopathy without macular edema
E10.3211
Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema, right
eye
E10.3212
Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema, left eye
E10.3213
Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema,
bilateral
E10.3291
Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema,
right eye
E10.3292
Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema, left
eye
E10.3293
Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema,
bilateral
E10.3311
Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema,
right eye
E10.3312
Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema,
left eye
E10.3313
Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema,
bilateral
E10.3391
Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema,
right eye
E10.3392
Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema,
left eye
E10.3393
Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema,
bilateral
E10.3411
Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema, right
eye
E10.3412
Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema, left
eye
E10.3413
Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema,
bilateral
E10.3491
Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema,
right eye
E10.3492
Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema,
left eye
E10.3493
Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema,
bilateral
E10.3511
Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema, right eye
E10.3512
Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema, left eye
E10.3513
Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema, bilateral
E10.3521
Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment
involving the macula, right eye
E10.3522
Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment
involving the macula, left eye
E10.3523
Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment
involving the macula, bilateral
E10.3531
Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not
involving the macula, right eye
E10.3532
Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not
involving the macula, left eye
E10.3533
Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not
involving the macula, bilateral
E10.3541
Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal
detachment and rhegmatogenous retinal detachment, right eye
E10.3542
Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal
detachment and rhegmatogenous retinal detachment, left eye
E10.3543
Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal
detachment and rhegmatogenous retinal detachment, bilateral
E10.3551
Type 1 diabetes mellitus with stable proliferative diabetic retinopathy, right eye
E10.3552
Type 1 diabetes mellitus with stable proliferative diabetic retinopathy, left eye
E10.3553
Type 1 diabetes mellitus with stable proliferative diabetic retinopathy, bilateral
E10.3591
Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema, right eye
E10.3592
Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema, left eye
E10.3593
Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema, bilateral
E10.37x1
Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment, right eye
E10.37x2
Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment, left eye
E10.37x3
Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment, bilateral
E10.36
Type 1 diabetes mellitus with diabetic cataract
E10.39
Type 1 diabetes mellitus with other diabetic ophthalmic complication
E10.40
Type 1 diabetes mellitus with diabetic neuropathy, unspecified
E10.41
Type 1 diabetes mellitus with diabetic mononeuropathy
E10.42
Type 1 diabetes mellitus with diabetic polyneuropathy
E10.43
Type 1 diabetes mellitus with diabetic autonomic (poly)neuropathy
E10.44
Type 1 diabetes mellitus with diabetic amyotrophy
E10.49
Type 1 diabetes mellitus with other diabetic neurological complication
E10.610
Type 1 diabetes mellitus with diabetic neuropathic arthropathy
E10.51
Type 1 diabetes mellitus with diabetic peripheral angiopathy without gangrene
E10.52
Type 1 diabetes mellitus with diabetic peripheral angiopathy with gangrene
E10.59
Type 1 diabetes mellitus with other circulatory complications
E10.618
Type 1 diabetes mellitus with other diabetic arthropathy
E10.620
Type 1 diabetes mellitus with diabetic dermatitis
E10.621
Type 1 diabetes mellitus with foot ulcer
E10.622
Type 1 diabetes mellitus with other skin ulcer
E10.628
Type 1 diabetes mellitus with other skin complications
E10.630
Type 1 diabetes mellitus with periodontal disease
E10.638
Type 1 diabetes mellitus with other oral complications
If ICD-10 is applicable, ICD-10-CM codes for the clinical trial are:
Secondary ICD-10-CM Diagnosis requirement for Clinical Trial:
Z00.6 Encounter for examination for normal comparison and control in clinical research
program
The applicable TOB is 11X. A secondary diagnosis (diagnoses positions 2 – 9) of ICD-10- CM code
Z00.6 (examination of participant or control in clinical research) must be present along with
condition code 30 (qualifying clinical trial) Z00.6 and condition code 30 alerts the claims
processing system that this is a clinical trial. The procedure is paid under inpatient prospective
payment system for hospitals with patients in the trial. Deductible and coinsurance apply for fee-for-
service beneficiaries.
Inpatient hospitals participating in this trial are entitled to an add-on payment of $18,848.00 for islet
isolation services. This amount is in addition to the final IPPS payment made to the hospital. Should two
infusions occur during the same hospital stay, Medicare will pay for two add-ons for isolation of the islet
cells, but never for more than two add-ons for a hospital stay.
Inpatient hospitals shall report charges for organ acquisition in Revenue Code 0810, 0811, 0812, 0813, or
0819. This includes charges for the pre-transplant items and services related to the acquisition and delivery
of the pancreatic islet cell transplants. As is Medicare’s policy with other organ transplants, Medicare
contractors deduct acquisition charges prior to processing through the IPPS Pricer. Pancreata procured for
islet cell transplant are not included in the prospective payment. They are paid on a reasonable cost basis.
This is a pass-through cost for which interim payments may be made.
Effective for services on or after May 1, 2006, contractors shall accept the QR modifier for islet cell
transplantation follow up care when performed in an outpatient department of a hospital when the transplant
was done in conjunction with an NIH-sponsored clinical trial, and when billed on type of bill 13X or 85X.
All other normal inpatient billing practices apply.
70.5 - Special Billing and Payment Requirements Medicare Advantage (MA)
Beneficiaries
(Rev. 261, Issued: 07-30-04, Effective: 10-01-04, Implementation: 10-04-04)
CMS will make payment directly on a fee-for service basis for the routine costs of pancreatic islet cell
transplants as well as transplantation and appropriate related items and services, for MA beneficiaries
participating in an NIH-sponsored clinical trial. MA organizations will not be liable for payment for routine
costs of this new clinical trial until MA payments can be appropriately adjusted to take into account the cost of
this national coverage decision. Medicare contractors shall make payment on behalf of MA organizations
directly to providers of these islet cell transplants in accordance with Medicare payment rules, except that
beneficiaries are not responsible for the Part A and Part B deductibles. MA enrollees will be liable for any
applicable coinsurance amounts MA organizations have in place for clinical trial benefits.
E10.649
Type 1 diabetes mellitus with hypoglycemia without coma
E10.8
Type 1 diabetes mellitus with unspecified complications
80 - Billing of the Diagnosis and Treatment of Peripheral Neuropathy with Loss of
Protective Sensation in People with Diabetes
(Rev. 498, Issued: 03-11-05, Effective/Implementation: N/A)
Coverage Requirements - Peripheral neuropathy is the most common factor leading to amputation in people
with diabetes. In diabetes, peripheral neuropathy is an anatomically diffuse process primarily affecting
sensory and autonomic fibers; however, distal motor findings may be present in advanced cases. Long nerves
are affected first, with symptoms typically beginning insidiously in the toes and then advancing proximally.
This leads to loss of protective sensation (LOPS), whereby a person is unable to feel minor trauma from
mechanical, thermal, or chemical sources. When foot lesions are present, the reduction in autonomic nerve
functions may also inhibit wound healing.
Peripheral neuropathy with LOPS, secondary to diabetes, is a localized illness of the feet and falls within the
regulation's exception to the general exclusionary rule (see 42 C.F.R. §411.15(l)(l)(i)). Foot exams for people
with diabetic peripheral neuropathy with LOPS are reasonable and necessary to allow for early intervention in
serious complications that typically afflict diabetics with the disease.
Effective for services furnished on or after July 1, 2002, Medicare covers, as a physician service, an
evaluation (examination and treatment) of the feet no more often than every 6 months for individuals with a
documented diagnosis of diabetic sensory neuropathy and LOPS, as long as the beneficiary has not seen a foot
care specialist for some other reason in the interim. LOPS shall be diagnosed through sensory testing with the
5.07 monofilament using established guidelines, such as those developed by the National Institute of Diabetes
and Digestive and Kidney Diseases guidelines. Five sites should be tested on the plantar surface of each foot,
according to the National Institute of Diabetes and Digestive and Kidney Diseases guidelines. The areas must
be tested randomly since the loss of protective sensation may be patchy in distribution, and the patient may get
clues if the test is done rhythmically. Heavily callused areas should be avoided. As suggested by the
American Podiatric Medicine Association, an absence of sensation at two or more sites out of 5 tested on
either foot when tested with the 5.07 Semmes-Weinstein monofilament must be present and documented to
diagnose peripheral neuropathy with loss of protective sensation.
80.1 - General Billing Requirements
(Rev. 2783, Issued: 09-10-13, Effective: 09-30-13, Implementation: 09-30-13)
The following providers of service may bill you for these services:
Hospitals;
Critical Access Hospitals
Rural Health Clinics; and
Free-Standing Federally Qualified Health Clinics (FQHC).
80.2 - Applicable HCPCS Codes
(Rev. 498, Issued: 03-11-05, Effective/Implementation: N/A)
G0245 - Initial physician evaluation and management of a diabetic patient with diabetic sensory neuropathy
resulting in a loss of protective sensation (LOPS) which must include:
1. The diagnosis of LOPS;
2. A patient history;
3. A physical examination that consists of at least the following elements:
(a) visual inspection of the forefoot, hindfoot, and toe web spaces,
(b) evaluation of a protective sensation,
(c) evaluation of foot structure and biomechanics,
(d) evaluation of vascular status and skin integrity,
(e) evaluation and recommendation of footwear, and
4. Patient education.
G0246 - Follow-up physician evaluation and management of a diabetic patient with diabetic sensory
neuropathy resulting in a loss of protective sensation (LOPS) to include at least the following:
1. a patient history;
2. a physical examination that includes:
(a) visual inspection of the forefoot, hindfoot, and toe web spaces,
(b) evaluation of protective sensation,
(c) evaluation of foot structure and biomechanics,
(d) evaluation of vascular status and skin integrity,
(e) evaluation and recommendation of footwear, and
3. patient education.
G0247 - Routine foot care by a physician of a diabetic patient with diabetic sensory neuropathy resulting
in a LOPS to include if present, at least the following:
(1) local care of superficial (i.e., superficial to muscle and fascia) wounds;
(2) debridement of corns and calluses; and
(3) trimming and debridement of nails.
NOTE: Code G0247 must be billed on the same date of service with either G0245 or G0246 in order to be
considered for payment.
The short descriptors for the above HCPCS codes are as follows:
G0245 – INITIAL FOOT EXAM PTLOPS
G0246 – FOLLOWUP EVAL OF FOOT PT LOP

G0247 – ROUTINE FOOTCARE PT W LOPS
80.3 - Diagnosis Codes
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
If ICD-10-CM is applicable--Providers should report one of the following diagnosis codes in
conjunction with this benefit:
ICD-10-CM
ICD-10 DX Description
E08.40
Diabetes mellitus due to underlying condition with diabetic neuropathy, unspecified
E08.42
Diabetes mellitus due to underlying condition with diabetic polyneuropathy
E09.40
Drug or chemical induced diabetes mellitus with neurological complications with diabetic n
E09.42
Drug or chemical induced diabetes mellitus with neurological complications with diabetic p
E10.40
Type 1 diabetes mellitus with diabetic neuropathy, unspecified
E10.41
Type 1 diabetes mellitus with diabetic mononeuropathy
E10.42
Type 1 diabetes mellitus with diabetic polyneuropathy
E10.43
Type 1 diabetes mellitus with diabetic autonomic (poly)neuropathy
E10.44
Type 1 diabetes mellitus with diabetic amyotrophy
E10.49
Type 1 diabetes mellitus with other diabetic neurological complication
E10.610
Type 1 diabetes mellitus with diabetic neuropathic arthropathy
E11.40
Type 2 diabetes mellitus with diabetic neuropathy, unspecified
E11.41
Type 2 diabetes mellitus with diabetic mononeuropathy
E11.42
Type 2 diabetes mellitus with diabetic polyneuropathy
E11.43
Type 2 diabetes mellitus with diabetic autonomic (poly)neuropathy
E11.44
Type 2 diabetes mellitus with diabetic amyotrophy
E11.49
Type 2 diabetes mellitus with other diabetic neurological complication
E11.610
Type 2 diabetes mellitus with diabetic neuropathic arthropathy
E13.40
Other specified diabetes mellitus with diabetic neuropathy, unspecified
E13.41
Other specified diabetes mellitus with diabetic mononeuropathy
E13.42
Other specified diabetes mellitus with diabetic polyneuropathy
E13.43
Other specified diabetes mellitus with diabetic autonomic (poly)neuropathy
E13.44
Other specified diabetes mellitus with diabetic amyotrophy
E13.49
Other specified diabetes mellitus with other diabetic neurological complication
E13.610
Other specified diabetes mellitus with diabetic neuropathic arthropathy
Coverage policy can be found in Pub. 100-03, Medicare National Coverage Determinations Manual, Chapter
1, section 70.2.1 Diabetic neuropathy w/ LOPs.
(http://www.cms.hhs.gov/manuals/103_cov_determ/ncd103index.asp
80.4 – Payment
(Rev. 2783, Issued: 09-10-13, Effective: 09-30-13, Implementation: 09-30-13)
• Hospital outpatient departments – OPPS
• Critical Access Hospital (CAH) - Method I -- Reasonable cost; Method II -- Technical - reasonable
cost, Professional -- 115 percent of the fee schedule
• Rural Health Clinics/Federally Qualified Health Centers (RHCs/FQHCs) - All inclusive rate.
Deductible and coinsurance apply.
While these physician services may be appropriately provided to patients of Comprehensive Outpatient
Rehabilitation Facilities (CORFs), the CORF does not bill. The services are billed by the physician on a
professional claim.
Examples of Payment calculation:
Part B Deductible Met: $900 (MPFS allowed amount) x 20 percent (co-insurance) = $720 (Medicare
reimbursement). Beneficiary is responsible for $180.
Part B Deductible Not met: $900 (MPFS allowed amount) - $100 (Part B deductible) = $800 x 20 percent
(co-insurance) = $640 (Medicare reimbursement). Beneficiary is responsible for $260.
Part B Deductible Met: $800 (actual charged amount) x 20 percent (co-insurance) = $640 (Medicare
Reimbursement), beneficiary is responsible for $160 co-insurance.
Part B Deductible Not Met: $800 (actual charged amount) - $100 (Part B deductible) = $700 x 20 percent (co-
insurance) = $560 (Medicare reimbursement). Beneficiary is responsible for $240, ($100 Part B deductible
and $140 co-insurance).
Services are paid at 80 percent of the lesser of the fee schedule amount or the actual charges.
This service, when furnished in an RHC/FQHC by a physician or non-physician, is considered an RHC/FQHC
service. RHCs/FQHCs bill you under bill type 71X or 73X with revenue code 940 and HCPCS G0245,
G0246, and G0247.
Payment should not be made for this service unless the claim contains a related visit code. Therefore, install
an edit in your system to assure payment is not made for revenue code 940 unless the claim also contains a
visit revenue code (520 or 521).
Applicable Revenue Codes
The applicable revenue code is 940, except for hospitals.
This service can be performed in other revenue centers such as a clinic (510) for hospitals. Therefore, instruct
your hospitals to report these procedures under the revenue center where they are performed.
80.5 - Applicable Revenue Codes
(Rev. 498, Issued: 03-11-05, Effective/Implementation: N/A)
The applicable revenue code is 940, except for hospitals.
This service can be performed in other revenue centers such as a clinic (510) for hospitals. Therefore, instruct
your hospitals to report these procedures under the revenue center where they are performed.
80.6 - Editing Instructions for A/B MACs (A)
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)

Edit 1 - Implement diagnosis to procedure code edits to allow payment only for the LOPS codes,
G0245, G0246, and G0247 when submitted with one of the following ICD-10-CM diagnosis codes
If ICD-10-CM is applicable:
ICD-10-CM
ICD-10 DX Description
E08.40
Diabetes mellitus due to underlying condition with diabetic neuropathy, unspecified
E08.42
Diabetes mellitus due to underlying condition with diabetic polyneuropathy
E09.40
Drug or chemical induced diabetes mellitus with neurological complications with diabetic n
E09.42
Drug or chemical induced diabetes mellitus with neurological complications with diabetic p
E10.40
Type 1 diabetes mellitus with diabetic neuropathy, unspecified
E10.41
Type 1 diabetes mellitus with diabetic mononeuropathy
E10.42
Type 1 diabetes mellitus with diabetic polyneuropathy
E10.43
Type 1 diabetes mellitus with diabetic autonomic (poly)neuropathy
E10.44
Type 1 diabetes mellitus with diabetic amyotrophy
E10.49
Type 1 diabetes mellitus with other diabetic neurological complication
E10.610
Type 1 diabetes mellitus with diabetic neuropathic arthropathy
E11.40
Type 2 diabetes mellitus with diabetic neuropathy, unspecified
E11.41
Type 2 diabetes mellitus with diabetic mononeuropathy
E11.42
Type 2 diabetes mellitus with diabetic polyneuropathy
E11.43
Type 2 diabetes mellitus with diabetic autonomic (poly)neuropathy
E11.44
Type 2 diabetes mellitus with diabetic amyotrophy
E11.49
Type 2 diabetes mellitus with other diabetic neurological complication
E11.610
Type 2 diabetes mellitus with diabetic neuropathic arthropathy
E13.40
Other specified diabetes mellitus with diabetic neuropathy, unspecified
E13.41
Other specified diabetes mellitus with diabetic mononeuropathy
E13.42
Other specified diabetes mellitus with diabetic polyneuropathy
E13.43
Other specified diabetes mellitus with diabetic autonomic (poly)neuropathy
E13.44
Other specified diabetes mellitus with diabetic amyotrophy
E13.49
Other specified diabetes mellitus with other diabetic neurological complication
E13.610
Other specified diabetes mellitus with diabetic neuropathic arthropathy
Deny these services when submitted without one of the appropriate diagnoses. Use the same
messages you currently use for procedure to diagnosis code denials. Edit 2 – Deny G0247 if it is
not submitted on the same claim as G0245 or G0246.
Use MSN 21.21 - This service was denied because Medicare only covers this service under certain
circumstances.
Use RA claim adjustment reason code 107 - The related or qualifying claim/service was not
identified on this claim. NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110
Service Payment Information REF), if present.
80.7 - CWF General Information
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)

The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare
identification number. For purposes of this manual, Medicare beneficiary identifier references both the Health
Insurance Claim Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare
card transition period and after for certain business areas that will continue to use the HICN as part of their
processes.
Though G0245 and G0246 have no technical or professional components, for these codes, CWF will post
institutional claims with type of bill 13X as technical, and professional claims as professional. For bill type
85X with revenue code 940, CWF will post as technical. For 85X bill type with revenue code 98X, (Method
II), CWF will post as technical and professional. This will allow both the facility and professional service
payments to be approved by CWF for payment when the code and date of service match. Therefore, should a
claim be received with the same code and same date of service for the same beneficiary, the second claim
submitted will not be rejected as a duplicate.
Due to the billing and payment methodology of Rural Health Clinics - bill type 71X and Federally Qualified
Health Centers - bill type 73X, CWF will post these claims as usual, which will correctly allow claims from
these entities that are billed on institutional claims to reject as duplicates when the HCPCS code, date of
service, and Medicare beneficiary identifier are an exact match with a claim billed on a professional claim.
Medicare contractors must react to these duplicate claims as they currently do for any other duplicates.
80.8 - CWF Utilization Edits
(Rev. 1742, Issued: 05-22-09, Effective: 06-08-09, Implementation: 06-08-09)
Edit 1 - Should CWF receive a claim from an FI for G0245 or G0246 and a second claim from a contractor for
either G0245 or G0246 (or vice versa) and they are different dates of service and less than 6 months apart, the
second claim will reject. CWF will edit to allow G0245 or G0246 to be paid no more than every 6 months for
a particular beneficiary, regardless of who furnished the service. If G0245 has been paid, regardless of
whether it was posted as a facility or professional claim, it must be 6 months before G0245 can be paid again
or G0246 can be paid. If G0246 has been paid, regardless of whether it was posted as a facility or
professional claim, it must be 6 months before G0246 can be paid again or G0245 can be paid. CWF will not
impose limits on how many times each code can be paid for a beneficiary as long as there has been 6 months
between each service.
The CWF will return a specific reject code for this edit to the contractors and FIs that will be identified in the
CWF documentation. Based on the CWF reject code, the contractors and FIs must deny the claims and return
the following messages:
MSN 18.4 -- This service is being denied because it has not been __ months since your last examination
of this kind (NOTE: Insert 6 as the appropriate number of months.)
RA claim adjustment reason code 96 – Non-covered charges, along with remark code M86 – Service denied
because payment already made for same/similar procedure within set time frame.
Edit 2
The CWF will edit to allow G0247 to pay only if either G0245 or G0246 has been submitted and accepted as
payable on the same date of service. CWF will return a specific reject code for this edit to the contractors and
FIs that will be identified in the CWF documentation. Based on this reject code, contractors and FIs will deny
the claims and return the following messages:

MSN 21.21 - This service was denied because Medicare only covers this service under certain
circumstances.
RA claim adjustment reason code 107 – The related or qualifying claim/service was not identified on this
claim.
Edit 3
Once a beneficiary’s condition has progressed to the point where routine foot care becomes a covered service,
payment will no longer be made for LOPS evaluation and management services. Those services would be
considered to be included in the regular exams and treatments afforded to the beneficiary on a routine basis.
The physician or provider must then just bill the routine foot care codes, per Pub 100-02, Chapter 15, §290.
The CWF will edit to reject LOPS codes G0245, G0246, and/or G0247 when on the beneficiary’s record it
shows that one of the following routine foot care codes were billed and paid within the prior 6 months: 11055,
11056, 11057, 11719, 11720, and/or 11721.
The CWF will return a specific reject code for this edit to the contractors and FIs that will be identified in the
CWF documentation. Based on the CWF reject code, the contractors and FIs must deny the claims and return
the following messages:
MSN 21.21 - This service was denied because Medicare only covers this service under certain
circumstances.
The RA claim adjustment reason code 96 – Non-covered charges, along with remark code M86 – Service
denied because payment already made for same/similar procedure within set time frame.
90 - Stem Cell Transplantation
(Rev.12533; Issued: 03-07-24 Effective: 04-08-24; Implementation:04-08-24)
A. General
Stem cell transplantation is a process in which stem cells are harvested
from either a patient’s (autologous) or donor’s (allogeneic) bone marrow or
peripheral blood for intravenous infusion.
Allogeneic and autologous stem cell transplants are covered under
Medicare for specific diagnoses. See Pub. 100-03, National Coverage
Determinations Manual, section 110.23, for a complete description of
covered and noncovered conditions. For Part A hospital inpatient claims
processing instructions, refer to Pub. 100-04, chapter 3, section 90. The
following sections contain claims processing instructions for all other
claims.
B. Nationally Covered Indications
C. Allogeneic Hematopoietic Stem Cell Transplantation (HSCT)

ICD-10-PCS Procedure Codes
30230G2
Transfusion of Allogeneic Related Bone Marrow into Peripheral Vein,
Open Approach
30230G3
Transfusion of Allogeneic Unrelated Bone Marrow into Peripheral
Vein, Open Approach
30233U2
Transfusion of Allogeneic Related T-cell Depleted Hematopoietic
Stem Cells into Peripheral Vein, Percutaneous Approach
30233U3
Transfusion of Allogeneic Unrelated T-cell Depleted Hematopoietic
Stem Cells into Peripheral Vein, Percutaneous Approach
30230Y2
Transfusion of Allogeneic Related Hematopoietic Stem Cells into
Peripheral Vein, Open Approach
30230Y3
Transfusion of Allogeneic Unrelated Hematopoietic Stem Cells into
Peripheral Vein, Open Approach
30233G2
Transfusion of Allogeneic Related Bone Marrow into Peripheral Vein,
Percutaneous Approach
30233G3
Transfusion of Allogeneic Unrelated Bone Marrow into Peripheral
Vein, Percutaneous Approach
30243U2
Transfusion of Allogeneic Related T-cell Depleted Hematopoietic
Stem Cells into Central Vein, Percutaneous Approach
30243U3
Percutaneous Approach
30233Y2
Transfusion of Allogeneic Related Hematopoietic Stem Cells into
Peripheral Vein, Percutaneous Approach
30233Y3
Transfusion of Allogeneic Unrelated Hematopoietic Stem Cells into
Peripheral Vein, Percutaneous Approach

30240G2
Transfusion of Allogeneic Related Bone Marrow into Central Vein,
Open Approach
30240G3
Transfusion of Allogeneic Unrelated Bone Marrow into Central Vein,
Open Approach
30240Y2
Transfusion of Allogeneic Related Hematopoietic Stem Cells into
Central Vein, Open Approach
30240Y3
Transfusion of Allogeneic Unrelated Hematopoietic Stem Cells into
Central Vein, Open Approach
30243G2
Transfusion of Allogeneic Related Bone Marrow into Central Vein,
Percutaneous Approach
30243G3
Transfusion of Allogeneic Unrelated Bone Marrow into Central Vein,
Percutaneous Approach
30243Y2
Transfusion of Allogeneic Related Hematopoietic Stem Cells into
Central Vein, Percutaneous Approach
30243Y3
Transfusion of Allogeneic Unrelated Hematopoietic Stem Cells into
Central Vein, Percutaneous Approach
HCPCS Code 38240
See below table for ICD-10-DX Codes:
a. Effective for services performed on or after August 1, 1978:
a.
For the treatment of leukemia, leukemia in remission; see table below for ICD-
10-CM codes:
C91.00
Acute lymphoblastic leukemia not having achieved remission
C91.01
Acute lymphoblastic leukemia, in remission
C91.02
Acute lymphoblastic leukemia, in relapse
C91.10
Chronic lymphocytic leukemia of B-cell type not having achieved remission
C91.11
Chronic lymphocytic leukemia of B-cell type in remission
C91.12
Chronic lymphocytic leukemia of B-cell type in relapse
C91.30
Prolymphocytic leukemia of B-cell type not having achieved remission
C91.31
Prolymphocytic leukemia of B-cell type, in remission
C91.32
Prolymphocytic leukemia of B-cell type, in relapse
C91.50
Adult T-cell lymphoma/leukemia (HTLV-1-associated) not having achieved remission
C91.51
Adult T-cell lymphoma/leukemia (HTLV-1-associated), in remission
C91.52
Adult T-cell lymphoma/leukemia (HTLV-1-associated), in relapse
C91.60
Prolymphocytic leukemia of T-cell type not having achieved remission
C91.61
Prolymphocytic leukemia of T-cell type, in remission
C91.62
Prolymphocytic leukemia of T-cell type, in relapse
C91.90
Lymphoid leukemia, unspecified not having achieved remission
C91.91
Lymphoid leukemia, unspecified, in remission
C91.92
Lymphoid leukemia, unspecified, in relapse
C91.A0
Mature B-cell leukemia Burkitt-type not having achieved remission

C91.A1
Mature B-cell leukemia Burkitt-type, in remission
C91.A2
Mature B-cell leukemia Burkitt-type, in relapse
C91.Z0
Other lymphoid leukemia not having achieved remission
C91.Z1
Other lymphoid leukemia, in remission
C91.Z2
Other lymphoid leukemia, in relapse
C92.00
Acute myeloblastic leukemia, not having achieved remission
C92.01
Acute myeloblastic leukemia, in remission
C92.02
Acute myeloblastic leukemia, in relapse
C92.10
Chronic myeloid leukemia, BCR/ABL-positive, not having achieved remission
C92.11
Chronic myeloid leukemia, BCR/ABL-positive, in remission
C92.12
Chronic myeloid leukemia, BCR/ABL-positive, in relapse
C92.20
Atypical chronic myeloid leukemia, BCR/ABL-negative, not having achieved remission
C92.21
Atypical chronic myeloid leukemia, BCR/ABL-negative, in remission
C92.22
Atypical chronic myeloid leukemia, BCR/ABL-negative, in relapse
C92.30
Myeloid sarcoma, not having achieved remission
C92.31
Myeloid sarcoma, in remission
C92.32
Myeloid sarcoma, in relapse
C92.40
Acute promyelocytic leukemia, not having achieved remission
C92.41
Acute promyelocytic leukemia, in remission
C92.42
Acute promyelocytic leukemia, in relapse
C92.50
Acute myelomonocytic leukemia, not having achieved remission
C92.51
Acute myelomonocytic leukemia, in remission
C92.52
Acute myelomonocytic leukemia, in relapse
C92.60
Acute myeloid leukemia with 11q23-abnormality not having achieved remission
C92.61
Acute myeloid leukemia with 11q23-abnormality in remission
C92.62
Acute myeloid leukemia with 11q23-abnormality in relapse
C92.90
Myeloid leukemia, unspecified, not having achieved remission
C92.91
Myeloid leukemia, unspecified in remission
C92.92
Myeloid leukemia, unspecified in relapse
C92.A0
Acute myeloid leukemia with multilineage dysplasia, not having achieved remission
C92.A1
Acute myeloid leukemia with multilineage dysplasia, in remission
C92.A2
Acute myeloid leukemia with multilineage dysplasia, in relapse
C92.Z0
Other myeloid leukemia not having achieved remission
C92.Z1
Other myeloid leukemia, in remission
C92.Z2
Other myeloid leukemia, in relapse
C93.00
Acute monoblastic/monocytic leukemia, not having achieved remission
C93.01
Acute monoblastic/monocytic leukemia, in remission
C93.02
Acute monoblastic/monocytic leukemia, in relapse
C93.10
Chronic myelomonocytic leukemia not having achieved remission
C93.11
Chronic myelomonocytic leukemia, in remission
C93.12
Chronic myelomonocytic leukemia, in relapse
C93.30
Juvenile myelomonocytic leukemia, not having achieved remission
C93.31
Juvenile myelomonocytic leukemia, in remission
C93.32
Juvenile myelomonocytic leukemia, in relapse
C93.90
Monocytic leukemia, unspecified, not having achieved remission

C93.91
Monocytic leukemia, unspecified in remission
C93.92
Monocytic leukemia, unspecified in relapse
C93.Z0
Other monocytic leukemia, not having achieved remission
C93.Z1
Other monocytic leukemia, in remission
C93.Z2
Other monocytic leukemia, in relapse
C94.00
Acute erythroid leukemia, not having achieved remission
C94.01
Acute erythroid leukemia, in remission
C94.02
Acute erythroid leukemia, in relapse
C94.20
Acute megakaryoblastic leukemia not having achieved remission
C94.21
Acute megakaryoblastic leukemia, in remission
C94.22
Acute megakaryoblastic leukemia, in relapse
C94.30
Mast cell leukemia not having achieved remission
C94.31
Mast cell leukemia, in remission
C94.32
Mast cell leukemia, in relapse
C94.80
Other specified leukemias not having achieved remission
C94.81
Other specified leukemias, in remission
C94.82
Other specified leukemias, in relapse
C95.00
Acute leukemia of unspecified cell type not having achieved remission
C95.01
Acute leukemia of unspecified cell type, in remission
C95.02
Acute leukemia of unspecified cell type, in relapse
C95.10
Chronic leukemia of unspecified cell type not having achieved remission
C95.11
Chronic leukemia of unspecified cell type, in remission
C95.12
Chronic leukemia of unspecified cell type, in relapse
C95.90
Leukemia, unspecified not having achieved remission
C95.91
Leukemia, unspecified, in remission
C95.92
Leukemia, unspecified, in relapse
D45
Polycythemia vera
ii. For the treatment of aplastic anemia; see table below for ICD-10- CM
codes)
ICD-10
Description
D60.0
Chronic acquired pure red cell aplasia
D60.1
Transient acquired pure red cell aplasia
D60.8
Other acquired pure red cell aplasias
D60.9
Acquired pure red cell aplasia, unspecified
D61.01
Constitutional (pure) red blood cell aplasia
D61.09
Other constitutional aplastic anemia
D61.1
Drug-induced aplastic anemia
D61.2
Aplastic anemia due to other external agents
D61.3
Idiopathic aplastic anemia
D61.810
Antineoplastic chemotherapy induced pancytopenia
D61.811
Other drug-induced pancytopenia
D61.818
Other pancytopenia
D61.82
Myelophthisis

D61.89
Other specified aplastic anemias and other bone marrow failure syndromes
D61.9
Aplastic anemia, unspecified
b.
Effective for services performed on or after June 3, 1985:
c.
For the treatment of severe combined immunodeficiency disease
(SCID) (ICD-10-CM codes D81.0, D81.1, D81.2, D81.6, D81.7,
D81.89, and D81.9)
d.
For the treatment of Wiskott-Aldrich syndrome ( ICD-10- CM
code D82.0)
c. Effective for services performed on or after August 4, 2010:
For the treatment of Myelodysplastic Syndromes (MDS) (ICD-10- CM
codes D46.A, D46.B, D46.C, D46.Z, D46.0, D46.1, D46.4,
D46.9, D46.20, D46.21, D46.22, and Z00.6) pursuant to Coverage with
Evidence Development (CED) in the context of a Medicare- approved,
prospective clinical study. Refer to Pub. 100-03, NCD Manual, chapter 1,
section 110.23, for further information about this policy. See section F below
for billing instructions.
d. Effective for services performed on or after January 27, 2016:
b. Allogeneic HSCT for multiple myeloma (ICD-10-CM codes C90.00,
C90.01, C90.02, and Z00.6) is covered by Medicare only for beneficiaries
with Durie-Salmon Stage II or III multiple myeloma, or International
Staging
System (ISS) Stage II or Stage III multiple myeloma, and participating in
an approved prospective clinical study. Refer to Pub. 100-03, NCD
Manual, chapter 1, section 110.23, for further information about this
policy. See section F below for billing instructions.
e.
Allogeneic HSCT for myelofibrosis (MF) (ICD-10-CM codes
C94.40, C94.41, C94.42, D47.1, D47.4, D75.81, and Z00.6) is
covered by Medicare only for beneficiaries with Dynamic
International Prognostic Scoring System (DIPSSplus)
intermediate-2 or High primary or secondary MF and
participating in an approved prospective clinical study. Refer to
Pub. 100- 03, NCD Manual, chapter 1, section 110.23, for further
information about this policy. See section F below for billing
instructions.
f.
Allogeneic HSCT for sickle cell disease (SCD) (ICD-10-CM codes D57.00, D57.01, D57.02,
D57.03, D57.09, D57.1, D57.20, D57.211, D57.212, D57.213, D57.218, D57.219, D57.40,
D57.411, D57.412, D57.413, D57.418, D57.419, D57.42, D57.431, D57.432, D57.433, D57.438,
D57.439, D57.44, D57.451, D57.452, D57.453, D57.458, D57.459, D57.80, D57.811,D57.812,
D57.813, D57.818, D57.819, and Z00.6)
is covered by Medicare only for beneficiaries with
severe, symptomatic SCD who participate in an

approved prospective clinical study. Refer to Pub.100-03,
NCD Manual, chapter 1, section 110.23, for further
information about this policy. See section F below for billing
instructions.
II. Autologous Stem Cell Transplantation (AuSCT)
HCPCS Code 38241
ICD-10-PCS Procedure Codes:
30230C0
Transfusion of Autologous Hematopoietic Stem/Progenitor Cells,
Genetically Modified into Peripheral Vein, Open Approach
30230G0
Transfusion of Autologous Bone Marrow into Peripheral Vein,
Open Approach
30230Y0
Transfusion of Autologous Hematopoietic Stem Cells into
Peripheral Vein, Open Approach
30233G0
Transfusion of Autologous Bone Marrow into Peripheral Vein,
Percutaneous Approach
30233C0
Transfusion of Autologous Hematopoietic Stem/Progenitor Cells,
Genetically
Modified into Peripheral Vein, Percutaneous Approach
30233Y0
Transfusion of Autologous Hematopoietic Stem Cells into
Peripheral Vein, Percutaneous Approach
30240C0
Transfusion of Autologous Hematopoietic Stem/Progenitor Cells,
Genetically
Modified into Central Vein, Open Approach
30240G0
Transfusion of Autologous Bone Marrow into Central Vein, Open
Approach
30240Y0
Transfusion of Autologous Hematopoietic Stem Cells into Central
Vein, Open Approach
30243C0
Transfusion of Autologous Hematopoietic Stem/Progenitor Cells,
Genetically
Modified into Central Vein, Percutaneous Approach
30243G0
Transfusion of Autologous Bone Marrow into Central Vein,
Percutaneous Approach
30243Y0
Transfusion of Autologous Hematopoietic Stem Cells into Central
Vein, Percutaneous Approach

Below ICD-10 CM codes Cover autologous SCT (38241) no trial for acute leukemia in
remission, resistant non-Hodgkins lymphomas, recurrent/refractory neuroblastoma,
advanced Hodgkins Disease on or after 4/28/89, and Cover autologous SCT (38241) no
trial for Durie-Salmon stage II/III responsive multiple myeloma and responsive relapse on
or after 10/1/00 over autologous SCT (38241) together with high dose melphalan (HDMI)
no trial for primary amyloid light chain (AL) amyloidosis on or after 3/15/05
C81.01
Nodular lymphocyte predominant Hodgkin lymphoma, lymph
nodes of head, face, and neck
C81.02
Nodular lymphocyte predominant Hodgkin lymphoma,
intrathoracic lymph nodes
C81.03
Nodular lymphocyte predominant Hodgkin lymphoma, intra-
abdominal lymph nodes
C81.04
Nodular lymphocyte predominant Hodgkin lymphoma, lymph
nodes of axilla and upper limb
C81.05
Nodular lymphocyte predominant Hodgkin lymphoma, lymph
nodes of inguinal region and lower limb
C81.06
Nodular lymphocyte predominant Hodgkin lymphoma,
intrapelvic lymph nodes
C81.07
Nodular lymphocyte predominant Hodgkin lymphoma, spleen
C81.08
Nodular lymphocyte predominant Hodgkin lymphoma, lymph
nodes of multiple sites
C81.09
Nodular lymphocyte predominant Hodgkin lymphoma,
extranodal and solid organ sites
C81.11
Nodular sclerosis Hodgkin lymphoma, lymph nodes of head,
face, and neck
C81.12
Nodular sclerosis Hodgkin lymphoma, intrathoracic lymph nodes
C81.13
Nodular sclerosis Hodgkin lymphoma, intra-abdominal lymph
nodes
C81.14
Nodular sclerosis Hodgkin lymphoma, lymph nodes of axilla and
upper limb
C81.15
Nodular sclerosis Hodgkin lymphoma, lymph nodes of inguinal
region and lower limb
C81.16
Nodular sclerosis Hodgkin lymphoma, intrapelvic lymph nodes
C81.17
Nodular sclerosis Hodgkin lymphoma, spleen
C81.18
Nodular sclerosis Hodgkin lymphoma, lymph nodes of multiple
sites
C81.19
Nodular sclerosis Hodgkin lymphoma, extranodal and solid
organ sites
C81.21
Mixed cellularity Hodgkin lymphoma, lymph nodes of head, face,
and neck
C81.22
Mixed cellularity Hodgkin lymphoma, intrathoracic lymph nodes
C81.23
Mixed cellularity Hodgkin lymphoma, intra-abdominal lymph
nodes

C81.24
Mixed cellularity Hodgkin lymphoma, lymph nodes of axilla and
upper limb
C81.25
Mixed cellularity Hodgkin lymphoma, lymph nodes of inguinal
region and lower limb
C81.26
Mixed cellularity Hodgkin lymphoma, intrapelvic lymph nodes
C81.27
Mixed cellularity Hodgkin lymphoma, spleen
C81.28
Mixed cellularity Hodgkin lymphoma, lymph nodes of multiple
sites
C81.29
Mixed cellularity Hodgkin lymphoma, extranodal and solid
organ sites
C81.31
Lymphocyte depleted Hodgkin lymphoma, lymph nodes of head,
face, and neck
C81.32
Lymphocyte depleted Hodgkin lymphoma, intrathoracic lymph
nodes
C81.33
Lymphocyte depleted Hodgkin lymphoma, intra-abdominal
lymph nodes
C81.34
Lymphocyte depleted Hodgkin lymphoma, lymph nodes of axilla
and upper limb
C81.35
Lymphocyte depleted Hodgkin lymphoma, lymph nodes
of inguinal region and lower limb
C81.36
Lymphocyte depleted Hodgkin lymphoma, intrapelvic lymph
nodes
C81.37
Lymphocyte depleted Hodgkin lymphoma, spleen
C81.38
Lymphocyte depleted Hodgkin lymphoma, lymph nodes
of multiple sites
C81.39
Lymphocyte depleted Hodgkin lymphoma, extranodal and solid
organ sites
C81.41
Lymphocyte-rich Hodgkin lymphoma, lymph nodes of head, face,
and neck
C81.42
Lymphocyte-rich Hodgkin lymphoma, intrathoracic lymph nodes
C81.43
Lymphocyte-rich Hodgkin lymphoma, intra-abdominal lymph
nodes
C81.44
Lymphocyte-rich Hodgkin lymphoma, lymph nodes of axilla and
upper limb
C81.45
Lymphocyte-rich Hodgkin lymphoma, lymph nodes of inguinal
region and lower limb
C81.46
Lymphocyte-rich Hodgkin lymphoma, intrapelvic lymph nodes
C81.47
Lymphocyte-rich Hodgkin lymphoma, spleen
C81.48
Lymphocyte-rich Hodgkin lymphoma, lymph nodes of
multiple sites
C81.49
Lymphocyte-rich Hodgkin lymphoma, extranodal and solid organ
sites
C81.71
Other Hodgkin lymphoma, lymph nodes of head, face, and neck
C81.72
Other Hodgkin lymphoma, intrathoracic lymph nodes
C81.73
Other Hodgkin lymphoma, intra-abdominal lymph nodes

C81.74
Other Hodgkin lymphoma, lymph nodes of axilla and upper limb
C81.75
Other Hodgkin lymphoma, lymph nodes of inguinal region and
lower limb
C81.76
Other Hodgkin lymphoma, intrapelvic lymph nodes
C81.77
Other Hodgkin lymphoma, spleen
C81.78
Other Hodgkin lymphoma, lymph nodes of multiple sites
C81.91
Hodgkin lymphoma, unspecified, lymph nodes of head, face, and
neck
C81.92
Hodgkin lymphoma, unspecified, intrathoracic lymph nodes
C81.93
Hodgkin lymphoma, unspecified, intra-abdominal lymph nodes
C81.94
Hodgkin lymphoma, unspecified, lymph nodes of axilla and
upper limb
C81.95
Hodgkin lymphoma, unspecified, lymph nodes of inguinal region
and lower limb
C81.96
Hodgkin lymphoma, unspecified, intrapelvic lymph nodes
C81.97
Hodgkin lymphoma, unspecified, spleen
C81.98
Hodgkin lymphoma, unspecified, lymph nodes of multiple sites
C81.99
Hodgkin lymphoma, unspecified, extranodal and solid organ
sites
C82.01
Follicular lymphoma grade I, lymph nodes of head, face, and
neck
C82.02
Follicular lymphoma grade I, intrathoracic lymph nodes
C82.03
Follicular lymphoma grade I, intra-abdominal lymph nodes
C82.04
Follicular lymphoma grade I, lymph nodes of axilla and upper
limb
C82.05
Follicular lymphoma grade I, lymph nodes of inguinal region
and lower limb
C82.06
Follicular lymphoma grade I, intrapelvic lymph nodes
C82.07
Follicular lymphoma grade I, spleen
C82.08
Follicular lymphoma grade I, lymph nodes of multiple sites
C82.09
Follicular lymphoma grade I, extranodal and solid organ sites
C82.11
Follicular lymphoma grade II, lymph nodes of head, face, and
neck
C82.12
Follicular lymphoma grade II, intrathoracic lymph nodes
C82.13
Follicular lymphoma grade II, intra-abdominal lymph nodes
C82.14
Follicular lymphoma grade II, lymph nodes of axilla and upper
limb
C82.15
Follicular lymphoma grade II, lymph nodes of inguinal region
and lower limb
C82.16
Follicular lymphoma grade II, intrapelvic lymph nodes
C82.17
Follicular lymphoma grade II, spleen
C82.18
Follicular lymphoma grade II, lymph nodes of multiple sites
C82.19
Follicular lymphoma grade II, extranodal and solid organ sites
C82.21
Follicular lymphoma grade III, unspecified, lymph nodes of
head, face, and neck

C82.22
Follicular lymphoma grade III, unspecified, intrathoracic lymph
nodes
C82.23
Follicular lymphoma grade III, unspecified, intra-abdominal
lymph nodes
C82.24
Follicular lymphoma grade III, unspecified, lymph nodes of
axilla and upper limb
C82.25
Follicular lymphoma grade III, unspecified, lymph nodes of
inguinal region and lower limb
C82.26
Follicular lymphoma grade III, unspecified, intrapelvic lymph
nodes
C82.27
Follicular lymphoma grade III, unspecified, spleen
C82.28
Follicular lymphoma grade III, unspecified, lymph nodes of
multiple sites
C82.29
Follicular lymphoma grade III, unspecified, extranodal and solid
organ sites
C82.31
Follicular lymphoma grade IIIa, lymph nodes of head, face, and
neck
C82.32
Follicular lymphoma grade IIIa, intrathoracic lymph nodes
C82.33
Follicular lymphoma grade IIIa, intra-abdominal lymph nodes
C82.34
Follicular lymphoma grade IIIa, lymph nodes of axilla and upper
limb
C82.35
Follicular lymphoma grade IIIa, lymph nodes of inguinal region
and lower limb
C82.36
Follicular lymphoma grade IIIa, intrapelvic lymph nodes
C82.37
Follicular lymphoma grade IIIa, spleen
C82.38
Follicular lymphoma grade IIIa, lymph nodes of multiple sites
C82.39
Follicular lymphoma grade IIIa, extranodal and solid organ sites
C82.41
Follicular lymphoma grade IIIb, lymph nodes of head, face, and
neck
C82.42
Follicular lymphoma grade IIIb, intrathoracic lymph nodes
C82.43
Follicular lymphoma grade IIIb, intra-abdominal lymph nodes
C82.44
Follicular lymphoma grade IIIb, lymph nodes of axilla and upper
limb
C82.45
Follicular lymphoma grade IIIb, lymph nodes of inguinal region
and lower limb
C82.46
Follicular lymphoma grade IIIb, intrapelvic lymph nodes
C82.47
Follicular lymphoma grade IIIb, spleen
C82.48
Follicular lymphoma grade IIIb, lymph nodes of multiple sites
C82.49
Follicular lymphoma grade IIIb, extranodal and solid organ sites
C82.51
Diffuse follicle center lymphoma, lymph nodes of head, face, and
neck
C82.52
Diffuse follicle center lymphoma, intrathoracic lymph nodes
C82.53
Diffuse follicle center lymphoma, intra-abdominal lymph nodes
C82.54
Diffuse follicle center lymphoma, lymph nodes of axilla and
upper limb

C82.55
Diffuse follicle center lymphoma, lymph nodes of inguinal region
and lower limb
C82.56
Diffuse follicle center lymphoma, intrapelvic lymph nodes
C82.57
Diffuse follicle center lymphoma, spleen
C82.58
Diffuse follicle center lymphoma, lymph nodes of multiple sites
C82.59
Diffuse follicle center lymphoma, extranodal and solid organ
sites
C82.61
Cutaneous follicle center lymphoma, lymph nodes of head, face,
and neck
C82.62
Cutaneous follicle center lymphoma, intrathoracic lymph nodes
C82.63
Cutaneous follicle center lymphoma, intra-abdominal lymph
nodes
C82.64
Cutaneous follicle center lymphoma, lymph nodes of axilla and
upper limb
C82.65
Cutaneous follicle center lymphoma, lymph nodes of inguinal
region and lower limb
C82.66
Cutaneous follicle center lymphoma, intrapelvic lymph nodes
C82.67
Cutaneous follicle center lymphoma, spleen
C82.68
Cutaneous follicle center lymphoma, lymph nodes of multiple
sites
C82.69
Cutaneous follicle center lymphoma, extranodal and solid organ
sites
C82.81
Other types of follicular lymphoma, lymph nodes of head, face,
and neck
C82.82
Other types of follicular lymphoma, intrathoracic lymph nodes
C82.83
Other types of follicular lymphoma, intra-abdominal lymph
nodes
C82.84
Other types of follicular lymphoma, lymph nodes of axilla and
upper limb
C82.85
Other types of follicular lymphoma, lymph nodes of inguinal
region and lower limb
C82.86
Other types of follicular lymphoma, intrapelvic lymph nodes
C82.87
Other types of follicular lymphoma, spleen
C82.88
Other types of follicular lymphoma, lymph nodes of multiple sites
C82.89
Other types of follicular lymphoma, extranodal and solid organ
sites
C82.91
Follicular lymphoma, unspecified, lymph nodes of head, face,
and neck
C82.92
Follicular lymphoma, unspecified, intrathoracic lymph nodes
C82.93
Follicular lymphoma, unspecified, intra-abdominal lymph nodes
C82.94
Follicular lymphoma, unspecified, lymph nodes of axilla and
upper limb
C82.95
Follicular lymphoma, unspecified, lymph nodes of inguinal
region and lower limb
C82.96
Follicular lymphoma, unspecified, intrapelvic lymph nodes

C82.97
Follicular lymphoma, unspecified, spleen
C82.98
Follicular lymphoma, unspecified, lymph nodes of multiple sites
C82.99
Follicular lymphoma, unspecified, extranodal and solid organ
sites
C83.01
Small cell B-cell lymphoma, lymph nodes of head, face, and neck
C83.02
Small cell B-cell lymphoma, intrathoracic lymph nodes
C83.03
Small cell B-cell lymphoma, intra-abdominal lymph nodes
C83.04
Small cell B-cell lymphoma, lymph nodes of axilla and upper
limb
C83.05
Small cell B-cell lymphoma, lymph nodes of inguinal region and
lower limb
C83.06
Small cell B-cell lymphoma, intrapelvic lymph nodes
C83.07
Small cell B-cell lymphoma, spleen
C83.08
Small cell B-cell lymphoma, lymph nodes of multiple sites
C83.09
Small cell B-cell lymphoma, extranodal and solid organ sites
C83.11
Mantle cell lymphoma, lymph nodes of head, face, and neck
C83.12
Mantle cell lymphoma, intrathoracic lymph nodes
C83.13
Mantle cell lymphoma, intra-abdominal lymph nodes
C83.14
Mantle cell lymphoma, lymph nodes of axilla and upper limb
C83.15
Mantle cell lymphoma, lymph nodes of inguinal region and lower
limb
C83.16
Mantle cell lymphoma, intrapelvic lymph nodes
C83.17
Mantle cell lymphoma, spleen
C83.18
Mantle cell lymphoma, lymph nodes of multiple sites
C83.19
Mantle cell lymphoma, extranodal and solid organ sites
C83.31
Diffuse large B-cell lymphoma, lymph nodes of head, face, and
neck
C83.32
Diffuse large B-cell lymphoma, intrathoracic lymph nodes
C83.33
Diffuse large B-cell lymphoma, intra-abdominal lymph nodes
C83.34
Diffuse large B-cell lymphoma, lymph nodes of axilla and upper
limb
C83.35
Diffuse large B-cell lymphoma, lymph nodes of inguinal region
and lower limb
C83.36
Diffuse large B-cell lymphoma, intrapelvic lymph nodes
C83.37
Diffuse large B-cell lymphoma, spleen
C83.38
Diffuse large B-cell lymphoma, lymph nodes of multiple sites
C83.39
Diffuse large B-cell lymphoma, extranodal and solid organ sites
C83.51
Lymphoblastic (diffuse) lymphoma, lymph nodes of head, face,
and neck
C83.52
Lymphoblastic (diffuse) lymphoma, intrathoracic lymph nodes
C83.53
Lymphoblastic (diffuse) lymphoma, intra-abdominal lymph nodes
C83.54
Lymphoblastic (diffuse) lymphoma, lymph nodes of axilla and
upper limb
C83.55
Lymphoblastic (diffuse) lymphoma, lymph nodes of inguinal
region and lower limb

C83.56
Lymphoblastic (diffuse) lymphoma, intrapelvic lymph nodes
C83.57
Lymphoblastic (diffuse) lymphoma, spleen
C83.58
Lymphoblastic (diffuse) lymphoma, lymph nodes of multiple sites
C83.59
Lymphoblastic (diffuse) lymphoma, extranodal and solid organ
sites
C83.71
Burkitt lymphoma, lymph nodes of head, face, and neck
C83.72
Burkitt lymphoma, intrathoracic lymph nodes
C83.73
Burkitt lymphoma, intra-abdominal lymph nodes
C83.74
Burkitt lymphoma, lymph nodes of axilla and upper limb
C83.75
Burkitt lymphoma, lymph nodes of inguinal region and lower
limb
C83.76
Burkitt lymphoma, intrapelvic lymph nodes
C83.77
Burkitt lymphoma, spleen
C83.78
Burkitt lymphoma, lymph nodes of multiple sites
C83.79
Burkitt lymphoma, extranodal and solid organ sites
C83.81
Other non-follicular lymphoma, lymph nodes of head, face, and
neck
C83.82
Other non-follicular lymphoma, intrathoracic lymph nodes
C83.83
Other non-follicular lymphoma, intra-abdominal lymph nodes
C83.84
Other non-follicular lymphoma, lymph nodes of axilla and upper
limb
C83.85
Other non-follicular lymphoma, lymph nodes of inguinal region
and lower limb
C83.86
Other non-follicular lymphoma, intrapelvic lymph nodes
C83.87
Other non-follicular lymphoma, spleen
C83.88
Other non-follicular lymphoma, lymph nodes of multiple sites
C83.89
Other non-follicular lymphoma, extranodal and solid organ sites
C83.91
Non-follicular (diffuse) lymphoma, unspecified, lymph nodes of
head, face, and neck
C83.92
Non-follicular (diffuse) lymphoma, unspecified, intrathoracic
lymph nodes
C83.93
Non-follicular (diffuse) lymphoma, unspecified, intra-abdominal
lymph nodes
C83.94
Non-follicular (diffuse) lymphoma, unspecified, lymph nodes of
axilla and upper limb
C83.95
Non-follicular (diffuse) lymphoma, unspecified, lymph nodes of
inguinal region and lower limb
C83.96
Non-follicular (diffuse) lymphoma, unspecified, intrapelvic lymph
nodes
C83.97
Non-follicular (diffuse) lymphoma, unspecified, spleen
C83.98
Non-follicular (diffuse) lymphoma, unspecified, lymph nodes of
multiple sites
C83.99
Non-follicular (diffuse) lymphoma, unspecified, extranodal and
solid organ sites
C84.01
Mycosis fungoides, lymph nodes of head, face, and neck
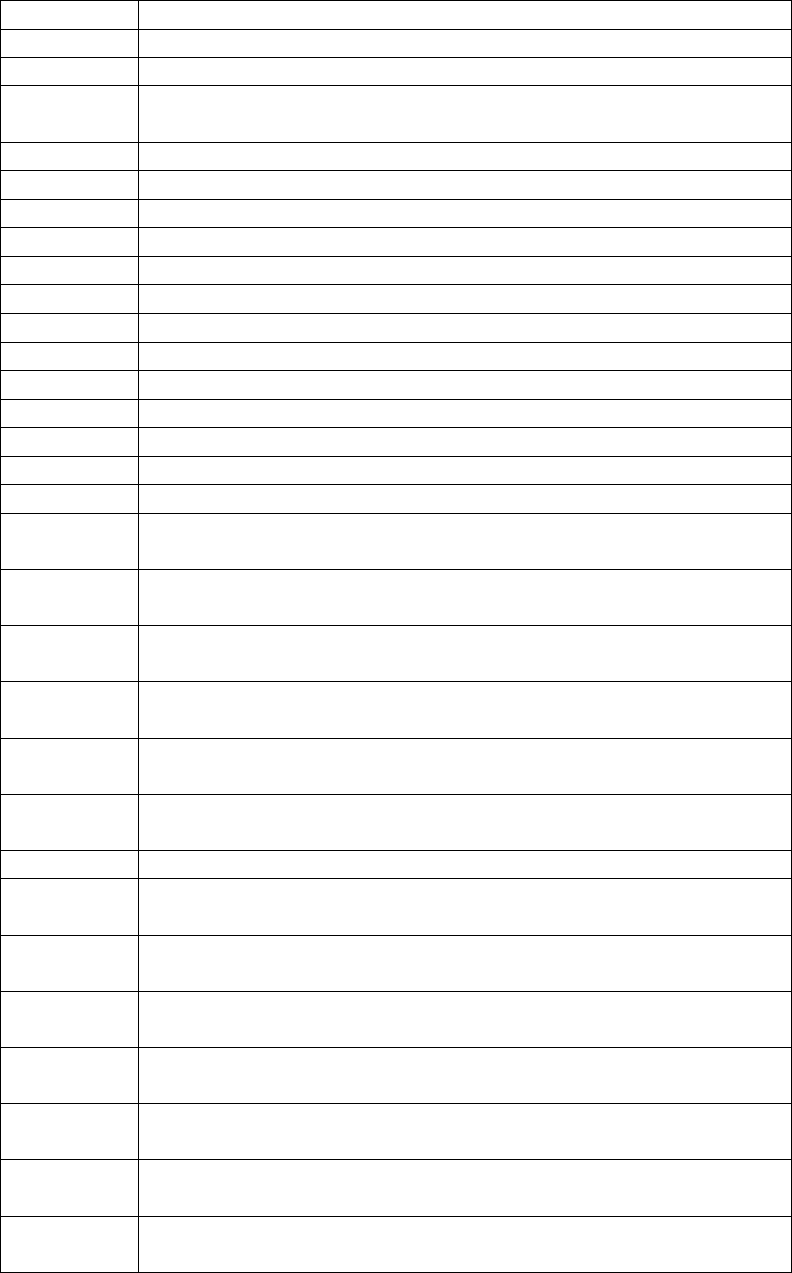
C84.02
Mycosis fungoides, intrathoracic lymph nodes
C84.03
Mycosis fungoides, intra-abdominal lymph nodes
C84.04
Mycosis fungoides, lymph nodes of axilla and upper limb
C84.05
Mycosis fungoides, lymph nodes of inguinal region and lower
limb
C84.06
Mycosis fungoides, intrapelvic lymph nodes
C84.07
Mycosis fungoides, spleen
C84.08
Mycosis fungoides, lymph nodes of multiple sites
C84.09
Mycosis fungoides, extranodal and solid organ sites
C84.11
Sezary disease, lymph nodes of head, face, and neck
C84.12
Sezary disease, intrathoracic lymph nodes
C84.13
Sezary disease, intra-abdominal lymph nodes
C84.14
Sezary disease, lymph nodes of axilla and upper limb
C84.15
Sezary disease, lymph nodes of inguinal region and lower limb
C84.16
Sezary disease, intrapelvic lymph nodes
C84.17
Sezary disease, spleen
C84.18
Sezary disease, lymph nodes of multiple sites
C84.19
Sezary disease, extranodal and solid organ sites
C84.41
Peripheral T-cell lymphoma, not classified, lymph nodes of head,
face, and neck
C84.42
Peripheral T-cell lymphoma, not classified, intrathoracic lymph
nodes
C84.43
Peripheral T-cell lymphoma, not classified, intra-abdominal
lymph nodes
C84.44
Peripheral T-cell lymphoma, not classified, lymph nodes of axilla
and upper limb
C84.45
Peripheral T-cell lymphoma, not classified, lymph nodes of
inguinal region and lower limb
C84.46
Peripheral T-cell lymphoma, not classified, intrapelvic lymph
nodes
C84.47
Peripheral T-cell lymphoma, not classified, spleen
C84.48
Peripheral T-cell lymphoma, not classified, lymph nodes of
multiple sites
C84.49
Peripheral T-cell lymphoma, not classified, extranodal and solid
organ sites
C84.61
Anaplastic large cell lymphoma, ALK-positive, lymph nodes of
head, face, and neck
C84.62
Anaplastic large cell lymphoma, ALK-positive, intrathoracic
lymph nodes
C84.63
Anaplastic large cell lymphoma, ALK-positive, intra-abdominal
lymph nodes
C84.64
Anaplastic large cell lymphoma, ALK-positive, lymph nodes of
axilla and upper limb
C84.65
Anaplastic large cell lymphoma, ALK-positive, lymph nodes of
inguinal region and lower limb

C84.66
Anaplastic large cell lymphoma, ALK-positive, intrapelvic lymph
nodes
C84.67
Anaplastic large cell lymphoma, ALK-positive, spleen
C84.68
Anaplastic large cell lymphoma, ALK-positive, lymph nodes of
multiple sites
C84.69
Anaplastic large cell lymphoma, ALK-positive, extranodal and
solid organ sites
C84.71
Anaplastic large cell lymphoma, ALK-negative, lymph nodes of
head, face, and neck
C84.72
Anaplastic large cell lymphoma, ALK-negative, intrathoracic
lymph nodes
C84.73
Anaplastic large cell lymphoma, ALK-negative, intra-abdominal
lymph nodes
C84.74
Anaplastic large cell lymphoma, ALK-negative, lymph nodes of
axilla and upper limb
C84.75
Anaplastic large cell lymphoma, ALK-negative, lymph nodes of
inguinal region and lower limb
C84.76
Anaplastic large cell lymphoma, ALK-negative, intrapelvic
lymph nodes
C84.77
Anaplastic large cell lymphoma, ALK-negative, spleen
C84.78
Anaplastic large cell lymphoma, ALK-negative, lymph nodes of
multiple sites
C84.79
Anaplastic large cell lymphoma, ALK-negative, extranodal and
solid organ sites
C84.91
Mature T/NK-cell lymphomas, unspecified, lymph nodes of head,
face, and neck
C84.92
Mature T/NK-cell lymphomas, unspecified, intrathoracic lymph
nodes
C84.93
Mature T/NK-cell lymphomas, unspecified, intra-abdominal
lymph nodes
C84.94
Mature T/NK-cell lymphomas, unspecified, lymph nodes of axilla
and upper limb
C84.95
Mature T/NK-cell lymphomas, unspecified, lymph nodes of
inguinal region and lower limb
C84.96
Mature T/NK-cell lymphomas, unspecified, intrapelvic lymph
nodes
C84.97
Mature T/NK-cell lymphomas, unspecified, spleen
C84.98
Mature T/NK-cell lymphomas, unspecified, lymph nodes of
multiple sites
C84.99
Mature T/NK-cell lymphomas, unspecified, extranodal and solid
organ sites
C84.A1
Cutaneous T-cell lymphoma, unspecified lymph nodes of head,
face, and neck
C84.A2
Cutaneous T-cell lymphoma, unspecified, intrathoracic lymph
nodes

C84.A3
Cutaneous T-cell lymphoma, unspecified, intra-abdominal lymph
nodes
C84.A4
Cutaneous T-cell lymphoma, unspecified, lymph nodes of axilla
and upper limb
C84.A5
Cutaneous T-cell lymphoma, unspecified, lymph nodes of
inguinal region and lower limb
C84.A6
Cutaneous T-cell lymphoma, unspecified, intrapelvic lymph
nodes
C84.A7
Cutaneous T-cell lymphoma, unspecified, spleen
C84.A8
Cutaneous T-cell lymphoma, unspecified, lymph nodes of
multiple sites
C84.A9
Cutaneous T-cell lymphoma, unspecified, extranodal and solid
organ sites
C84.Z1
Other mature T/NK-cell lymphomas, lymph nodes of head, face,
and neck
C84.Z2
Other mature T/NK-cell lymphomas, intrathoracic lymph nodes
C84.Z3
Other mature T/NK-cell lymphomas, intra-abdominal lymph
nodes
C84.Z4
Other mature T/NK-cell lymphomas, lymph nodes of axilla and
upper limb
C84.Z5
Other mature T/NK-cell lymphomas, lymph nodes of inguinal
region and lower limb
C84.Z6
Other mature T/NK-cell lymphomas, intrapelvic lymph nodes
C84.Z7
Other mature T/NK-cell lymphomas, spleen
C84.Z8
Other mature T/NK-cell lymphomas, lymph nodes of multiple
sites
C84.Z9
Other mature T/NK-cell lymphomas, extranodal and solid organ
sites
C85.11
Unspecified B-cell lymphoma, lymph nodes of head, face, and
neck
C85.12
Unspecified B-cell lymphoma, intrathoracic lymph nodes
C85.13
Unspecified B-cell lymphoma, intra-abdominal lymph nodes
C85.14
Unspecified B-cell lymphoma, lymph nodes of axilla and upper
limb
C85.15
Unspecified B-cell lymphoma, lymph nodes of inguinal region
and lower limb
C85.16
Unspecified B-cell lymphoma, intrapelvic lymph nodes
C85.17
Unspecified B-cell lymphoma, spleen
C85.18
Unspecified B-cell lymphoma, lymph nodes of multiple sites
C85.19
Unspecified B-cell lymphoma, extranodal and solid organ sites
C85.21
Mediastinal (thymic) large B-cell lymphoma, lymph nodes of
head, face, and neck
C85.22
Mediastinal (thymic) large B-cell lymphoma, intrathoracic lymph
nodes

C85.23
Mediastinal (thymic) large B-cell lymphoma, intra-abdominal
lymph nodes
C85.24
Mediastinal (thymic) large B-cell lymphoma, lymph nodes of
axilla and upper limb
C85.25
Mediastinal (thymic) large B-cell lymphoma, lymph nodes of
inguinal region and lower limb
C85.26
Mediastinal (thymic) large B-cell lymphoma, intrapelvic lymph
nodes
C85.27
Mediastinal (thymic) large B-cell lymphoma, spleen
C85.28
Mediastinal (thymic) large B-cell lymphoma, lymph nodes of
multiple sites
C85.29
Mediastinal (thymic) large B-cell lymphoma, extranodal and
solid organ sites
C85.81
Other specified types of non-Hodgkin lymphoma, lymph nodes of
head, face, and neck
C85.82
Other specified types of non-Hodgkin lymphoma, intrathoracic
lymph nodes
C85.83
Other specified types of non-Hodgkin lymphoma, intra-
abdominal lymph nodes
C85.84
Other specified types of non-Hodgkin lymphoma, lymph nodes of
axilla and upper limb
C85.85
Other specified types of non-Hodgkin lymphoma, lymph nodes of
inguinal region and lower limb
C85.86
Other specified types of non-Hodgkin lymphoma, intrapelvic
lymph nodes
C85.87
Other specified types of non-Hodgkin lymphoma, spleen
C85.88
Other specified types of non-Hodgkin lymphoma, lymph nodes of
multiple sites
C85.89
Other specified types of non-Hodgkin lymphoma, extranodal and
solid organ sites
C85.91
Non-Hodgkin lymphoma, unspecified, lymph nodes of head, face,
and neck
C85.92
Non-Hodgkin lymphoma, unspecified, intrathoracic lymph nodes
C85.93
Non-Hodgkin lymphoma, unspecified, intra-abdominal lymph
nodes
C85.94
Non-Hodgkin lymphoma, unspecified, lymph nodes of axilla and
upper limb
C85.95
Non-Hodgkin lymphoma, unspecified, lymph nodes of inguinal
region and lower limb
C85.96
Non-Hodgkin lymphoma, unspecified, intrapelvic lymph nodes
C85.97
Non-Hodgkin lymphoma, unspecified, spleen
C85.98
Non-Hodgkin lymphoma, unspecified, lymph nodes of multiple
sites
C85.99
Non-Hodgkin lymphoma, unspecified, extranodal and solid
organ sites

C86.0
Extranodal NK/T-cell lymphoma, nasal type
C86.1
Hepatosplenic T-cell lymphoma
C86.2
Enteropathy-type (intestinal) T-cell lymphoma
C86.3
Subcutaneous panniculitis-like T-cell lymphoma
C86.4
Blastic NK-cell lymphoma
C86.5
Angioimmunoblastic T-cell lymphoma
C86.6
Primary cutaneous CD30-positive T-cell proliferations
C88.0
Waldenstrom macroglobulinemia
C88.2
Heavy chain disease
C88.3
Immunoproliferative small intestinal disease
C88.4
Extranodal marginal zone B-cell lymphoma of mucosa-
associated lymphoid tissue [MALT-lymphoma]
C88.8
Other malignant immunoproliferative diseases
C88.9
Malignant immunoproliferative disease, unspecified
C90.00
Multiple myeloma not having achieved remission
C90.01
Multiple myeloma in remission
C90.02
Multiple myeloma in relapse
C90.10
Plasma cell leukemia not having achieved remission
C90.11
Plasma cell leukemia in remission
C90.20
Extramedullary plasmacytoma not having achieved remission
C90.21
Extramedullary plasmacytoma in remission
C90.22
Extramedullary plasmacytoma in relapse
C90.30
Solitary plasmacytoma not having achieved remission
C90.31
Solitary plasmacytoma in remission
C90.32
Solitary plasmacytoma in relapse
C91.01
Acute lymphoblastic leukemia, in remission
C91.11
Chronic lymphocytic leukemia of B-cell type in remission
C91.31
Prolymphocytic leukemia of B-cell type, in remission
C91.51
Adult T-cell lymphoma/leukemia (HTLV-1-associated), in
remission
C91.61
Prolymphocytic leukemia of T-cell type, in remission
C91.91
Lymphoid leukemia, unspecified, in remission
C91.A1
Mature B-cell leukemia Burkitt-type, in remission
C91.Z1
Other lymphoid leukemia, in remission
C92.01
Acute myeloblastic leukemia, in remission
C92.11
Chronic myeloid leukemia, BCR/ABL-positive, in remission
C92.21
Atypical chronic myeloid leukemia, BCR/ABL-negative,
in remission
C92.31
Myeloid sarcoma, in remission
C92.41
Acute promyelocytic leukemia, in remission
C92.51
Acute myelomonocytic leukemia, in remission
C92.61
Acute myeloid leukemia with 11q23-abnormality in remission
C92.91
Myeloid leukemia, unspecified in remission
C92.A1
Acute myeloid leukemia with multilineage dysplasia, in remission
C92.Z1
Other myeloid leukemia, in remission

C93.01
Acute monoblastic/monocytic leukemia, in remission
C93.11
Chronic myelomonocytic leukemia, in remission
C93.31
Juvenile myelomonocytic leukemia, in remission
C93.91
Monocytic leukemia, unspecified in remission
C93.Z1
Other monocytic leukemia, in remission
C94.01
Acute erythroid leukemia, in remission
C94.21
Acute megakaryoblastic leukemia, in remission
C94.31
Mast cell leukemia, in remission
C94.81
Other specified leukemias, in remission
C95.01
Acute leukemia of unspecified cell type, in remission
C95.11
Chronic leukemia of unspecified cell type, in remission
C95.91
Leukemia, unspecified, in remission
C96.0
Multifocal and multisystemic (disseminated) Langerhans-cell
histiocytosis
C96.20
Malignant mast cell neoplasm, unspecified
C96.21
Aggressive systemic mastocytosis
C96.22
Mast cell sarcoma
C96.29
Other malignant mast cell neoplasm
C96.4
Sarcoma of dendritic cells (accessory cells)
C96.5
Multifocal and unisystemic Langerhans-cell histiocytosis
C96.6
Unifocal Langerhans-cell histiocytosis
C96.9
Malignant neoplasm of lymphoid, hematopoietic and related
tissue, unspecified
C96.A
Histiocytic sarcoma
C96.Z
Other specified malignant neoplasms of lymphoid, hematopoietic
and related tissue
D45
Polycythemia vera
D47.Z9
Other specified neoplasms of uncertain behavior of lymphoid,
hematopoietic and related tissue
E85.4
Organ-limited amyloidosis
E85.81
Light chain (AL) amyloidosis
E85.89
Other amyloidosis
E85.9
Amyloidosis, unspecified
a. Effective for services performed on or after April 28, 1989:
Acute leukemia in remission who have a high probability of relapse and who
have no human leucocyte antigens (HLA)- matched (ICD-10-CM diagnosis
codes C91.01, C92.01, C92,41, C92.51, C92.61, C92.A1, C93.01, C94.01,
C94.21, C94.41, C95.01);
Resistant non-Hodgkin's lymphomas or those presenting with poor
prognostic features following an initial response (ICD-
10-CM diagnosis codes C82.01-C85.29, C85.81-C86.6, C96.4, and C96.Z-
C96.9);
Recurrent or refractory neuroblastoma (see ICD-10-CM codes Neoplasm
by site, malignant for the appropriate diagnosis code) following ranges
are reported: C00 - C96, and D00 - D09 Resistant non- Hodgkin’s
lymphomas); or, Advanced Hodgkin's disease who have failed
conventional therapy and have no HLA-matched donor (ICD-10-CM
codes C81.01 - C81.99).
a. Effective for services performed on or after October 1, 2000:
Single AuSCT is only covered for Durie-Salmon Stage II or III multiple
myeloma patients (ICD-10-CM codes C90.00, C90.01, C90.02 and
D47.Z9) that fit the following requirements:
•
Newly diagnosed or responsive multiple myeloma. This includes those patients with
previously untreated disease, those with at least a partial response to prior chemotherapy
(defined as a 50% decrease either in measurable paraprotein [serum and/or urine] or in
bone marrow infiltration, sustained for at least 1 month), and those in responsive
relapse; and
•
Adequate cardiac, renal, pulmonary, and hepatic function.
b. Effective for services performed on or after March 15, 2005:
When recognized clinical risk factors are employed to select patients for
transplantation, high dose melphalan (HDM) together with AuSCT is
reasonable and necessary for Medicare beneficiaries of any age group
with primary amyloid light chain (AL) amyloidosis (ICD-10-CM codes
E85.4, E85.81, E85.89 and E85.9)
who meet the following criteria:
•
Amyloid deposition in 2 or fewer organs; and,
•
Cardiac left ventricular ejection fraction (EF) greater than 45%.
E85.4 Organ-limited amyloidosis
E85.81 Light chain (AL) amyloidosis
E85.89 Other amyloidosis
E85.9 Amyloidosis, unspecified
As the applicable ICD-10 CM codes E85.4, E85.81, E85.9, and
E85.89 for amyloidosis do not differentiate between primary and
non- primary, A/B MACs (B) should perform prepay reviews on all
claims with a diagnosis of ICD- 10-CM code E85.4, E85.81,
E85.9, and E85.89
to determine whether payment is appropriate.
C. Nationally Non-Covered Indications
I. Allogeneic Hematopoietic Stem Cell Transplantation (HSCT)
Effective for claims with dates of service on or after May 24, 1996, through
January 27, 2016, allogeneic HSCT is not covered as treatment for multiple
myeloma (if ICD-10-CM is applicable, ICD- 10-CM codes C90.00, C90.01,
C90.02 and D47.Z9).
II. Autologous Stem Cell Transplantation (AuSCT)
AuSCT is not considered reasonable and necessary within the meaning of
§l862(a)(1)(A) of the Act and is not covered under Medicare for the
following conditions:
• Acute leukemia not in remission prior to October 1, 2000 ( if
ICD-10-CM is applicable, ICD-10-CM codes C91.00, C92.00,
C93.00, C94.00, and C95.00)
• Chronic granulocytic leukemia prior to October 1, 2000 (if
ICD-10-CM is applicable, ICD-10-CM code C92.10);
1.Solid tumors prior to October 1, 2000 (other than
neuroblastoma) (if ICD-10-CM is applicable, ICD-10-
CM codes C00.0 – C80.2 and D00.0 – D09.9);
2.
Multiple myeloma prior to October 1, 2000 (if ICD-10-
CM is applicable, ICD-10-CM codes C90.00, C90.01,
C90.02 and D47.Z9);
3.
Tandem transplantation, on or after October 1, 2000
(if ICD-10-CM is applicable, ICD-10-CM codes
C90.00, C90.01, C90.02, and D47.Z9) ;
4.
Non- primary amyloidosis on or after 10/01/00, for all Medicare
beneficiaries
5.
Primary AL amyloidosis effective October 1, 2000,
through March 14, 2005 for Medicare beneficiaries age
64. (if ICD-10-CM is applicable, ICD-10-CM codes
E85.4, E85.81, E85.9, and E85.89);
As the ICD-10-CM is applicable, as the applicable ICD-10 CM codes E85.4, E85.81,
E85.9, and E85.89 for amyloidosis do not differentiate between primary and non-primary,
A/B MACs (B) should perform prepay reviews on all claims with a diagnosis of ICD-10-
CM code E85.4, E85.81, E85.9, and E85.89 to determine whether payment is appropriate.
2.
Other
All other indications for stem cell transplantation not otherwise noted above
as covered or non-covered remain at local Medicare Administrative
Contractor discretion.
3.
Suggested MSN and RA Messages
The contractor shall use an appropriate MSN and CARC message such as
the following:
MSN - 15.4, The information provided does not support the need for this
service or item;
CARC - 150, Payment adjusted because the payer deems the
information submitted does not support this level of service.
4.
Clinical Trials for Allogeneic Hematopoietic Stem Cell
Transplantation (HSCT) for Myelodysplastic Syndrome
(MDS), Multiple Myeloma, Myelofibrosis (MF), and for
Sickle Cell Disease (SCD)
• Background
Effective for services performed on or after August 4, 2010, contractors shall
pay for claims for allogeneic HSCT for the treatment of Myelodysplastic
Syndromes (MDS) pursuant to Coverage with Evidence Development (CED)
in the context of a Medicare-approved, prospective clinical study.
Effective for services performed on or after January 27, 2016, contractors
shall pay for claims for allogeneic HSCT for the treatment of multiple
myeloma, myelofibrosis (MF), and for sickle cell disease (SCD) pursuant to
CED, in the context of a Medicare-approved, prospective clinical study.
Refer to Pub.100-03, National Coverage Determinations Manual, Chapter
1, section 110.23, for more information about this policy, and Pub. 100-04,
Medicare Claims Processing Manual, Chapter 3, section 90.3, for
information on inpatient billing of this CED.
• Adjudication Requirements
Payable Conditions. For claims with dates of service on and after August
4, 2010, contractors shall pay for claims for allogeneic HSCT for MDS when
the service was provided pursuant to a Medicare-approved clinical study
under CED; these services are paid only in the inpatient setting (Type of Bill
(TOB) 11X), as outpatient Part B (TOB 13X), and in Method II critical
access hospitals (TOB 85X).
Contractors shall require the following coding in order to pay for these claims:
• Existing Medicare-approved clinical trial coding
conventions, as required in Pub. 100-04, Medicare Claims
Processing Manual, Chapter 32, section 69, and inpatient
billing requirements regarding acquisition of stem cells in
Pub. 100- 04, Medicare Claims Processing Manual,
Chapter 3, section 90.3.1.
• If ICD-10-CM is applicable, ICD-10-PCS, procedure
codes 30230G2, 30230G3, 30230Y2, 30230Y3,
30233G2, 30233G3, 30233Y2, 30233Y3, 30240G2,
30240G3, 30240Y2, 30240Y3, 30243G2, 30243G3,
30243Y2, and 30243Y3.
• If Outpatient Hospital or Professional Claims: HCPCS
procedure code 38240
• If ICD-10-CM is applicable, ICD-10-CM codes D46.A,
D46.B, D46.C, D46.Z, D46.0, D46.1, D46.4, D46.9,
D46.20, D46.21, D46.22, and Z00.6.
• Professional claims only: place of service codes 19, 21, or 22.
Payable Conditions. For claims with dates of service on and after January
27, 2016, contractors shall pay for claims for allogeneic HSCT for multiple
myeloma, myelofibrosis (MF), and for sickle cell disease (SCD) when the
service was provided pursuant to a Medicare-approved clinical study under
CED; these services are paid only in the inpatient setting (Type of Bill (TOB)
11X), as outpatient Part B (TOB 13X), and in Method II critical access
hospitals (TOB 85X).
Contractors shall require the following coding in order to pay for these claims:
• Existing Medicare-approved clinical trial coding
conventions, as required in Pub. 100-04, Medicare Claims
Processing Manual, Chapter 32, section 69, and inpatient
billing requirements regarding acquisition of stem cells in
Pub. 100- 04, Medicare Claims Processing Manual,
Chapter 3, section 90.3.1.
• ICD-10-PCS codes 30230G2, 30230G3, 30230Y2,
30230Y3, 30233G2, 30233G3, 30233Y2,
30233Y3,
30240G2, 30240G3, 30240Y2, 30240Y3, 30243G2,
30243G3, 30243Y2, and 30243Y3.
• ICD-10-CM diagnosis codes C90.00, C90.01,
C90.02, C94.40, C94.41, C94.42, D47.1, D47.4,
D75.81, D57.00, D57.01, D57.02, D57.03, D57.09,
D57.1, D57.20, D57.211, D57.212, D57.213,
D57.218, D57.219, D57.40, D57.411, D57.412,
D57.413, D57.418, D57.419, D57.42, D57.431,
D57.432, D57.433, D57.438, D57.439, D57.44,
D57.451, D57.452, D57.453, D57.458, and D57.459,
D57.80, D57.811, D57.812, D57.813, D57.818,
D57.819, and Z00.6.
• If Outpatient Hospital or Professional Claims: HCPCS procedure code
38240
• Professional claims only: place of service codes 19, 21, or 22.
Denials. Contractors shall deny claims failing to meet any of the above criteria. In addition, contractors shall
apply the following requirements:
□
Providers shall issue a hospital issued notice of non- coverage (HINN) or advance beneficiary notice (ABN) to
the beneficiary if the services performed are not provided in accordance with CED.
□
Contractors shall deny claims that do not meet the criteria for coverage with the following messages:
CARC 50 - These are non-covered services because this is not deemed a 'medical necessity' by the payer.
NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF), if present.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An NCD provides a
coverage determination as to whether a particular item or service is covered. A copy of this policy is available a
http:www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to
request a copy of the NCD.
Group Code – Patient Responsibility (PR) if HINN/ABN issued, otherwise Contractual Obligation (CO)
MSN 16.77 – This service/item was not covered because it was not provided as part of a qualifying trial/study.
(Este servicio/artículo no fue cubierto porque no estaba incluido como parte de un ensayo clínico/estudio
calificado.)
MSN 15.20 – The following policies [NCD 110.23] were used when we made this decision. (Las siguientes
políticas [NCD 110.23] fueron utilizadas cuando se tomó esta decisión.)
90.1 - General
(Rev. 486, Issued: 03-04-05, Effective Date/Implementation Date: N/A)
Allogeneic Stem Cell Transplantation.
Allogeneic stem cell transplantation is a procedure in which a portion of a healthy donor’s stem cells is
obtained and prepared for intravenous infusion to restore normal hematopoietic function in recipients having
an inherited or acquired hematopoietic deficiency or defect.
Expenses incurred by a donor are a covered benefit to the recipient/beneficiary but, except for physician
services, are not paid separately. Services to the donor include physician services, hospital care in connection
with screening the stem cell, and ordinary follow-up care.
Autologous Stem Cell Transplantation
Autologous stem cell transplantations is a technique for restoring stem cells using the patient’s own previously
stored cells. Autologous stem cell transplants are covered for certain specified diagnoses for services rendered
on or after April 28, 1989.
90.2 - HCPCS and Diagnosis Coding – ICD-9-CM Applicable
(Rev.11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-21)
Allogeneic Stem Cell Transplantation
• Effective for services performed on or after August 1, 1978:
For the treatment of leukemia or leukemia in remission, providers shall use appropriate ICD-10 diagnosis codes
noted in section 90 and HCPCS code 38240.
For the treatment of aplastic anemia, providers shall use appropriate ICD-10 diagnosis codes noted in section
90 and HCPCS code 38240.
• Effective for services performed on or after June 3, 1985:
For the treatment of severe combined immunodeficiency disease, providers shall use appropriate ICD-10
diagnosis codes noted in section 90 and HCPCS code 38240.
For the treatment of Wiskott-Aldrich syndrome, providers shall use appropriate ICD-10-CM code D82.0 and
HCPCS code 38240.
Autologous Stem Cell Transplantation.--Is covered under the following circumstances effective for services
performed on or after April 28, 1989:
For the treatment of patients with acute leukemia in remission who have a high probability of relapse and who
have no human leucocyte antigens (HLA) matched, providers shall use appropriate ICD-10 diagnosis codes
noted in section 90 for lymphoid; myeloid; monocytic; acute erythremia; erythroleukemia; unspecified cell
type and HCPCS code 38241.
For the treatment of resistant non-Hodgkin’s lymphomas for those patients presenting with poor prognostic
features following an initial response, providers shall use appropriate ICD-10 diagnosis codes noted in section
90 and HCPCS code 38241.
For the treatment of recurrent or refractory neuroblastoma, providers shall use ICD- 10-CM codes
Neoplasm by site, malignant, the appropriate HCPCS code and HCPCS code 38241.
For the treatment of advanced Hodgkin’s disease for patients who have failed conventional therapy and
have no HLA-matched donor, providers shall use appropriate ICD-10 diagnosis codes and HCPCS code
38241

Autologous Stem Cell Transplantation.--Is covered under the following circumstances effective for services
furnished on or after October 1, 2000:
For the treatment of multiple myeloma (only for beneficiaries who are less than age 78, have Durie-
Salmon stage II or III newly diagnosed or responsive multiple myeloma, and have adequate cardiac,
renal, pulmonary and hepatic functioning), providers shall use appropriate ICD-10-CM code and
HCPCS code 38241.
For the treatment of recurrent or refractory neuroblastoma, providers shall use appropriate code (see ICD-10-
CM neoplasm by site, malignant) and HCPCS code 38241.
Effective for services performed on or after March 15, 2005, when recognized clinical risk factors are
employed to select patients for transplantation, high-dose melphalan (HDM) together with autologous
stem cell transplantation (HDM/AuSCT) is reasonable and necessary for Medicare beneficiaries of any
age group for the treatment of primary amyloid light chain (AL) amyloidosis, ICD-10- CM codes E85.4,
E85.81, E85.9, and E85.89 who meet the following criteria:
Amyloid deposition in 2 or fewer organs; and,
Cardiac left ventricular ejection fraction (EF) greater than 45%.
90.2.1 - HCPCS and Diagnosis Coding for Stem Cell Transplantation - ICD-10-CM
Applicable
(Rev. 11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-17-21)
ICD-10 is applicable to services on and after the implementation of ICD-.
For services provided use the appropriate code from the ICD-10 CM codes the table below..
See §90.2 for a list of covered conditions
ICD-10
Description
C91.00
Acute lymphoblastic leukemia not having achieved remission
C91.01
Acute lymphoblastic leukemia, in remission
C91.02
Acute lymphoblastic leukemia, in relapse
C91.10
Chronic lymphocytic leukemia of B-cell type not having achieved remission
C91.11
Chronic lymphocytic leukemia of B-cell type in remission
C91.12
Chronic lymphocytic leukemia of B-cell type in relapse

C91.30
Prolymphocytic leukemia of B-cell type not having achieved remission
C91.31
Prolymphocytic leukemia of B-cell type, in remission
C91.32
Prolymphocytic leukemia of B-cell type, in relapse
C91.50
Adult T-cell lymphoma/leukemia (HTLV-1-associated) not having achieved remission
C91.51
Adult T-cell lymphoma/leukemia (HTLV-1-associated), in remission
C91.52
Adult T-cell lymphoma/leukemia (HTLV-1-associated), in relapse
C91.60
Prolymphocytic leukemia of T-cell type not having achieved remission
C91.61
Prolymphocytic leukemia of T-cell type, in remission
C91.62
Prolymphocytic leukemia of T-cell type, in relapse
C91.90
Lymphoid leukemia, unspecified not having achieved remission
C91.91
Lymphoid leukemia, unspecified, in remission
C91.92
Lymphoid leukemia, unspecified, in relapse
C91.A0
Mature B-cell leukemia Burkitt-type not having achieved remission
C91.A1
Mature B-cell leukemia Burkitt-type, in remission
C91.A2
Mature B-cell leukemia Burkitt-type, in relapse
C91.Z0
Other lymphoid leukemia not having achieved remission
C91.Z1
Other lymphoid leukemia, in remission
C91.Z2
Other lymphoid leukemia, in relapse
C92.00
Acute myeloblastic leukemia, not having achieved remission
C92.01
Acute myeloblastic leukemia, in remission
C92.02
Acute myeloblastic leukemia, in relapse
C92.10
Chronic myeloid leukemia, BCR/ABL-positive, not having achieved remission
C92.11
Chronic myeloid leukemia, BCR/ABL-positive, in remission
C92.12
Chronic myeloid leukemia, BCR/ABL-positive, in relapse
C92.20
Atypical chronic myeloid leukemia, BCR/ABL-negative, not having achieved
remission
C92.21
Atypical chronic myeloid leukemia, BCR/ABL-negative, in remission
C92.22
Atypical chronic myeloid leukemia, BCR/ABL-negative, in relapse
C92.30
Myeloid sarcoma, not having achieved remission
C92.31
Myeloid sarcoma, in remission
C92.32
Myeloid sarcoma, in relapse
C92.40
Acute promyelocytic leukemia, not having achieved remission
C92.41
Acute promyelocytic leukemia, in remission
C92.42
Acute promyelocytic leukemia, in relapse
C92.50
Acute myelomonocytic leukemia, not having achieved remission
C92.51
Acute myelomonocytic leukemia, in remission
C92.52
Acute myelomonocytic leukemia, in relapse
C92.60
Acute myeloid leukemia with 11q23-abnormality not having achieved remission
C92.61
Acute myeloid leukemia with 11q23-abnormality in remission
C92.62
Acute myeloid leukemia with 11q23-abnormality in relapse
C92.90
Myeloid leukemia, unspecified, not having achieved remission
C92.91
Myeloid leukemia, unspecified in remission
C92.92
Myeloid leukemia, unspecified in relapse
C92.A0
Acute myeloid leukemia with multilineage dysplasia, not having achieved remission
C92.A1
Acute myeloid leukemia with multilineage dysplasia, in remission
C92 A2
At l id lk i ith ltili d li i l

C92.Z0
Other myeloid leukemia not having achieved remission
C92.Z1
Other myeloid leukemia, in remission
C92.Z2
Other myeloid leukemia, in relapse
C93.00
Acute monoblastic/monocytic leukemia, not having achieved remission
C93.01
Acute monoblastic/monocytic leukemia, in remission
C93.02
Acute monoblastic/monocytic leukemia, in relapse
C93.10
Chronic myelomonocytic leukemia not having achieved remission
C93.11
Chronic myelomonocytic leukemia, in remission
C93.12
Chronic myelomonocytic leukemia, in relapse
C93.30
Juvenile myelomonocytic leukemia, not having achieved remission
C93.31
Juvenile myelomonocytic leukemia, in remission
C93.32
Juvenile myelomonocytic leukemia, in relapse
C93.90
Monocytic leukemia, unspecified, not having achieved remission
C93.91
Monocytic leukemia, unspecified in remission
C93.92
Monocytic leukemia, unspecified in relapse
C93.Z0
Other monocytic leukemia, not having achieved remission
C93.Z1
Other monocytic leukemia, in remission
C93.Z2
Other monocytic leukemia, in relapse
C94.00
Acute erythroid leukemia, not having achieved remission
C94.01
Acute erythroid leukemia, in remission
C94.02
Acute erythroid leukemia, in relapse
C94.20
Acute megakaryoblastic leukemia not having achieved remission
C94.21
Acute megakaryoblastic leukemia, in remission
C94.22
Acute megakaryoblastic leukemia, in relapse
C94.30
Mast cell leukemia not having achieved remission
C94.31
Mast cell leukemia, in remission
C94.32
Mast cell leukemia, in relapse
C94.80
Other specified leukemias not having achieved remission
C94.81
Other specified leukemias, in remission
C94.82
Other specified leukemias, in relapse
C95.00
Acute leukemia of unspecified cell type not having achieved remission
C95.01
Acute leukemia of unspecified cell type, in remission
C95.02
Acute leukemia of unspecified cell type, in relapse
C95.10
Chronic leukemia of unspecified cell type not having achieved remission
C95.11
Chronic leukemia of unspecified cell type, in remission
C95.12
Chronic leukemia of unspecified cell type, in relapse
C95.90
Leukemia, unspecified not having achieved remission
C95.91
Leukemia, unspecified, in remission
C95.92
Leukemia, unspecified, in relapse
D45
Polycythemia vera
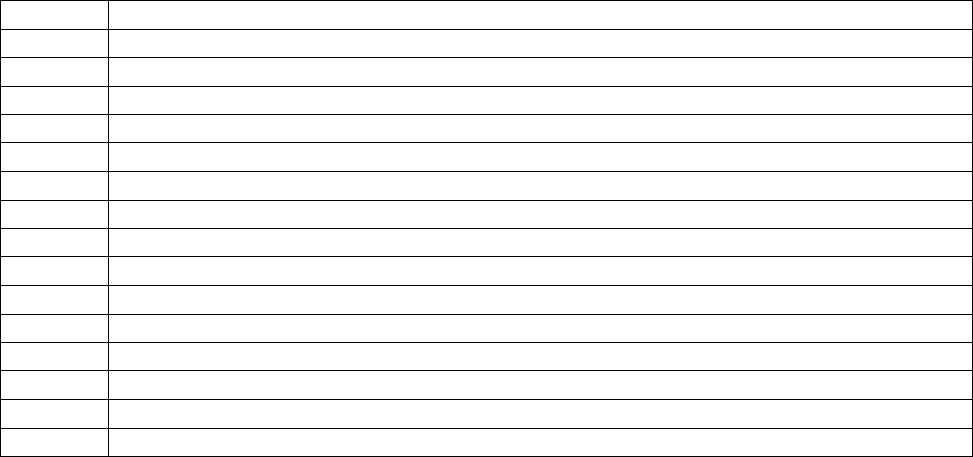
III. For the treatment of aplastic anemia; see table below for
ICD-10- CM codes)
If ICD-10-CM is applicable, the following ranges of ICD-10-
CM codes are also covered for AuSCT:
• Resistant non-Hodgkin’s lymphomas, ICD-10-CM
diagnosis codes C82.01-C85.29, C85.81- C86.6, C96.4, and
C96.Z-C96.9.
• Tandem transplantation (multiple rounds of autologous
stem cell transplantation) for patients with multiple
myeloma, ICD-10-CM codes C90.00, C90.01, C90.02
and D47.Z9
NOTE: The following conditions are not covered:
• Acute leukemia not in remission
• Chronic granulocytic leukemia
• Solid tumors (other than neuroblastoma)
• Multiple myeloma
• For Medicare beneficiaries age 64 or older, all forms of
amyloidosis, primary and non-primary
• Non-primary amyloidosis
Also coverage for conditions other than those specifically designated as
covered in §90.2 or specifically designated as non-covered in this
section or in §90.3will be at the discretion of the individual contractor.
ICD-10
Description
D60.0
Chronic acquired pure red cell aplasia
D60.1
Transient acquired pure red cell aplasia
D60.8
Other acquired pure red cell aplasias
D60.9
Acquired pure red cell aplasia, unspecified
D61.01
Constitutional (pure) red blood cell aplasia
D61.09
Other constitutional aplastic anemia
D61.1
Drug-induced aplastic anemia
D61.2
Aplastic anemia due to other external agents
D61.3
Idiopathic aplastic anemia
D61.810
Antineoplastic chemotherapy induced pancytopenia
D61.811
Other drug-induced pancytopenia
D61.818
Other pancytopenia
D61.82
Myelophthisis
D61.89
Other specified aplastic anemias and other bone marrow failure syndromes
D61.9
Aplastic anemia, unspecified
90.3 - Non-Covered Conditions
(Rev.11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-17-21)
Autologous stem cell transplantation is not covered for the following conditions:
a) Acute leukemia not in remission prior to October 1, 2000 (if ICD-10-CM
is applicable, ICD-10-CM codes C91.00, C92.00, C93.00, C94.00, and C95.00)
b) Chronic granulocytic leukemia prior to October 1, 2000 (if ICD-10-CM is
applicable, ICD-10-CM code C92.10);
c) Solid tumors prior to October 1, 2000 (other than neuroblastoma) (if ICD-
10-CM is applicable, ICD-10-CM codes C00.0 – C80.2 and D00.0 – D09.9);
d) Multiple myeloma prior to October 1, 2000 (if ICD-10-CM is applicable,
ICD-10-CM codes C90.00, C90.01, C90.02 and D47.Z9);
e) Tandem transplantation, on or after October 1, 2000 (if ICD-10-CM is
applicable, ICD-10-CM codes C90.00, C90.01, C90.02, and D47.Z9) ;
f) Non- primary amyloidosis on or after 10/01/00, for all Medicare
beneficiaries
g) Primary AL amyloidosis effective October 1, 2000, through March 14,
2005 for Medicare beneficiaries age 64. (if ICD-10-CM is applicable, ICD-10-
CM codes E85.4, E85.81, E85.9, and E85.89);
NOTE: Coverage for conditions other than those specifically designated as covered in
90.2 or 90.2.1 or specifically designated as non-covered in this section will be at the discretion of the
individual A/B MAC (B).
90.4 - Edits
(Rev.11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-17-21)
NOTE: Coverage for conditions other than those specifically designated as covered in
80.2 or specifically designated as non-covered in this section will be at the discretion of the
individual A/B MAC (B).
Appropriate diagnosis to procedure code edits should be implemented for the non-covered conditions and
services in 90.2 90.2.1, and 90.3 as applicable
As the ICD-10-CM codes E85.4, E85.81, E85.89, and E85.9
amyloidosis does not differentiate between primary and non-primary, A/B MACs (B) should perform prepay
reviews on all claims with a diagnosis of ICD-10-CM codes E85.4, E85.81, E85.89, and E85.9 and a HCPCS
procedure code of 38241 to determine whether payment is appropriate.
90.5 - Suggested MSN and RA Messages
(Rev.11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-17-21)
The contractor shall use an appropriate MSN and CARC message such as the following:
MSN - 15.4, The information provided does not support the need for this service or item;
CARC - 150, Payment adjusted because the payer deems the information submitted does not support this level
of service.
90.6 - Clinical Trials for Allogeneic Hematopoietic Stem Cell Transplantation (HSCT)
for Myelodysplastic Syndrome (MDS)
(Rev. 11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-21)
Myelodysplastic Syndrome (MDS) refers to a group of diverse
blood disorders in which the bone marrow does not produce
enough healthy, functioning blood cells. These disorders are
varied with regard to clinical characteristics, cytologic and
pathologic features, and cytogenetics.
On August 4, 2010, the Centers for Medicare & Medicaid
Services (CMS) issued a national coverage determination
(NCD) stating that
CMS believes that the evidence does not demonstrate that the
use of allogeneic hematopoietic stem cell transplantation (HSCT)
improves health outcomes in Medicare beneficiaries with MDS.
Therefore, allogeneic HSCT for MDS is not reasonable and
necessary under
§1862(a)(1)(A) of the Social Security Act (the Act).
However, allogeneic HSCT for MDS is reasonable and
necessary under
§1862(a)(1)(E) of the Act and therefore covered by Medicare
ONLY if provided pursuant to a Medicare-approved clinical
study under Coverage with Evidence Development (CED). Refer
to Pub.100-03, National Coverage Determinations Manual,
Chapter 1, section 110.8.1, for more information about this
policy, and Pub. 100-04, Medicare Claims Processing Manual,
Chapter 3, section 90.3.1, for information on CED.
B Adjudication Requirements
Payable Conditions. For claims with dates of service on and
after August 4, 2010, contractors shall pay for claims for HSCT
for MDS when the service was provided pursuant to a
Medicare-approved clinical study under CED; these services
are paid only in the inpatient setting (Type of Bill (TOB) 11X),
as outpatient Part B (TOB 13X), and in Method II critical
access hospitals (TOB 85X). Contractors shall require the
following coding in order to pay for these claims:
• Existing Medicare-approved clinical trial coding conventions,
as required in Pub. 100-04, Medicare Claims Processing
Manual, Chapter 32, section 69, and inpatient billing
requirements regarding acquisition of stem cells in Pub. 100-
04, Medicare Claims Processing Manual, Chapter 3, section
90.3.3.
• If ICD-10-CM is applicable, ICD-10-PCS, procedure codes
30230C0, 30230G0, 30230Y0, 30233G0, 30233C0,
30233Y0, 30240C0, 30240G0, 30240Y0, 30243C0,
30243G0, and30243Y0
• If Outpatient Hospital or Professional Claims: HCPCS procedure code 38240
• If ICD-10-CM is applicable, ICD-10-CM diagnosis codes, D46.A, D46.B,
D46.C, D46.Z, D46.0, D46.1, D46.20, D46.21, D46.22, D46.4, D46.9, and
Z00.6
• Professional claims only: place of service codes 21 or 22.
Denials. Contractors shall deny claims failing to meet any of
the above criteria. In addition, contractors shall apply the
following requirements:
• Providers shall issue a hospital issued notice of non-coverage
(HINN) or advance beneficiary notice (ABN) to the
beneficiary if the services performed are not provided in
accordance with CED.
• Contractors shall deny claims that do not meet the criteria
for coverage with the following messages:
CARC 50 - These are non-covered services because this is not deemed a 'medical necessity' by the payer.
NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information
REF), if present.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An NCD provides a
coverage determination as to whether a particular item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to
request a copy of the NCD.
Group Code – Patient Responsibility (PR) if HINN/ABN issued, otherwise Contractual Obligation (CO)
MSN 16.77 – This service/item was not covered because it was not provided as part of a qualifying trial/study.
(Este servicio/artículo no fue cubierto porque no estaba incluido como parte de un ensayo clínico/estudio
calificado.)
100 – Billing Requirements for Expanded Coverage of Cochlear Implantation
(Rev. 11875; Issued:02-23-23; Effective: 09-26-22; Implementation: 03-24-23)
Effective for dates of services on and after September 26, 2022, the Centers for Medicare & Medicaid
Services (CMS) has expanded the coverage for cochlear implantation to cover bilateral pre- or post- linguistic,
sensorineural, moderate-to-profound hearing loss in individuals with hearing test scores equal to or less than
60% correct in the best aided listening condition on recorded tests of open-set sentence recognition and who
demonstrate limited benefit from amplification. (See Publication 100-03, Chapter 1, Section 50.3, for
complete coverage criteria).
In addition, CMS is covering cochlear implants for beneficiaries not meeting the coverage criteria listed
under Publication 100-03, Chapter 1, Section 50.3 when performed in context with:
• A Food and Drug Administration (FDA)-approved category B investigational device exemption (IDE)
clinical trial as defined at 42 CFR 405.201; or
• As a routine cost in a clinical trial under the CMS clinical trial policy (see Pub. 100-03, section 310.1).
100.1 – A/B MACs (Part A) Billing Procedures
(Rev. 11875; Issued:02-23-23; Effective: 09-26-22; Implementation: 03-24-23)
There are no special payment methods. Existing payment methods shall apply.
100.1.1 – Applicable Bill Types
(Rev. 601, Issued: 07-01-05; Effective: 04-04-05; Implementation: 07-25-05)
11X, 12X (see note below), 13X, 83X, 85X
NOTE: Surgical procedures are not acceptable on 12x bill types.
100.1.2 – Special Billing Requirements for A/B MACs (A) for Inpatient Billing
(Rev. 11875; Issued:02-23-23; Effective: 09-26-22; Implementation: 03-24-23)
• The second or subsequent diagnosis code must be ICD-10-CM Z00.6 (Encounter for exam for normal
comparison and control in clinical research program). These diagnoses alert the claims processing
system that this is a clinical trial.
• For patients in an FDA-approved category B IDE clinical trial the -Q0 modifier must be reported with
the cochlear implantation device and all other related costs or; (see note below)
• For patients in an approved clinical trial under the clinical trial policy the -Q1 modifier must be billed
for routine costs and not for the device itself
NOTE: The -Q0/-Q1 modifiers do not need to be applied to these services (92601-92604, 92507 & 92521-
92524).
100.2 – Intermediary Payment Requirements
(Rev. 601, Issued: 07-01-05; Effective: 04-04-05; Implementation: 07-25-05)
There are no special payment methods. Existing payment methods shall apply.
100.3 – A/B MACs (Part B) Billing Procedures
(Rev. 11875; Issued:02-23-23; Effective: 09-26-22; Implementation: 03-24-23)
Effective for dates of service performed on and after September 26, 2022, the following applies:
A/B MACs (Part B) shall accept claims for cochlear implantation devices and services for beneficiaries
meeting the coverage criteria listed under Publication 100-03, Chapter 1, section 50.3.
A/B MACs (Part B) shall accept claims for cochlear implantation devices and all related costs for
beneficiaries not meeting the coverage criteria listed under Publication 100-03, Chapter 1, Section 50.3
provided in an FDA-approved category B IDE clinical trial or a trial under the CMS Clinical Trial policy, that
is billed with the -Q0 modifier. The definition of the -Q0 modifier is, “Item or service provided in a Medicare
specified study.”
A/B MACs (Part B) shall accept claims for routine costs pertaining to beneficiaries not meeting the coverage
criteria listed under Publication 100-03, Chapter 1, Section 50.3 who are in a clinical trial under the clinical
trial policy that is billed with the -Q1 modifier. The definition of the -Q1 modifier is, “Routine clinical
service provided in a clinical research study that is in an approved clinical research study”
A/B MACs (Part B) shall accept claims for evaluation and therapeutic services related to cochlear
implantation.
NOTE: The -Q0/-Q1 modifier does not need to be applied to these services (92601-92604, 92507 & 92521-
92524).
These services should be billed on an approved electronic claim form or a paper CMS Form 1500.
100.4 – Healthcare Common Procedural Coding System (HCPCS)
(Rev. 11875; Issued:02-23-23; Effective: 09-26-22; Implementation: 03-24-23)
The following HCPCS codes are some of those available for use when billing for cochlear implantation
services and devices provided by audiologists or physicians, and for the service of 92507, by speech language
pathologists.
69930 – Cochlear device implantation, with or without mastoidectomy
L8614 – Cochlear Device includes all internal and external components
L8619 – Cochlear implant external speech processor and controller, integrated system, replacement
L7510 – Repair of prosthetic device, repair or replace minor parts
92507 – Treatment of speech, language, voice, communication, and/or auditory processing disorder (includes
aural rehabilitation); individual
92521 – Evaluation of speech fluency (e.g. stuttering, cluttering)
92522 – Evaluation of speech sound production (e.g. articulation, phonological process, apraxia, dysarthria)
92523 – Evaluation of speech sound production (e.g. articulation, phonological process, apraxia, dysarthria)
with evaluation of language comprehension and expression (e.g. receptive and expressive language).
92524 – Behavioral and qualitive analysis of voice and resonance
92601 – Diagnostic analysis of cochlear implant, patient under 7 years of age; with programming
(Codes 92601 and 92603 describe post-operative analysis and fitting of previously placed external devices,
connection to the cochlear implant, and programming of the stimulator. Codes 92602 and 92604 describe
subsequent sessions for measurements and adjustment of the external transmitter and re-programming of the
internal stimulator.)
92602 – Diagnostic analysis of cochlear implant, patient under 7 years of age; subsequent programming. (Do
not report 92602 in addition to 92601.)
92603 – Diagnostic analysis of cochlear implant, age 7 years or older; with programming
92604 – Diagnostic analysis of cochlear implant, age 7 years or older; subsequent reprogramming

A complete list of audiology codes can be found in Pub 100-4, chapter12, section 30.3.
100.5 - Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes
(RARCs), Group Codes, and Medicare Summary Notice (MSN) Messages
(Rev. 11875; Issued:02-23-23; Effective: 09-26-22; Implementation: 03-24-23)
Contractors shall use the appropriate claim adjustment reason codes (CARCs), remittance advice remark
codes (RARCs), group codes, or Medicare summary notice (MSN) messages when denying payment for
cochlear implantation devices and services for beneficiaries with moderate-to-profound hearing loss in
patients with hearing test scores ≤ 40% through 9/25/22; ≤ 60% effective 9/26/22.
Use the following messages when denying services on claims:
• submitted on a TOB other than 11X, 12X (except surgical procedures), 13X or 85X (For Part A only);
or
• submitted without the Q0/Q1; or
• submitted without diagnostic code Z000.6 or
• submitted without one of the CPT/HCPCs listed (92521-92524, 92507, 92601- 92604, L7510, L8614,
L8619, 69930)
CARC 50 - “These are non-covered services because this is not deemed a ‘medical necessity’
by the payer”
RARC N386 - “This decision was based on a National Coverage Determination (NCD). An
NCD provides a coverage determination as to whether a particular item or service is covered. A
copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not have web
access, you may contact the contractor to request a copy of the NCD.”
MSN 15.20 = “The following policies were used when we made this decision:
NCD 50. 3”
Spanish translation: “Las siguientes políticas fueron utilizadas cuando se tomó esta
decisión: NCD 50.3”)
Contractors processing institutional claims shall use the following MSN message in addition to
MSN 15.20:
MSN 15.19 - Local Coverage Determinations (LCDs) help Medicare decide what is covered.
An LCD was used for your claim. You can compare your case to the LCD, and send
information from your doctor if you think it could change our decision. Call 1-800-
MEDICARE (1-800-633-4227) for a copy of the LCD.
Spanish Version - Las Determinaciones Locales de Cobertura (LCDs en inglés) le
ayudan a decidir a Medicare lo que está cubierto. Un LCD se usó para su reclamación.
Usted puede comparar su caso con la determinación y enviar información de su médico
si piensa que puede cambiar nuestra decisión. Para obtener una copia del LCD, llame al
1-800-MEDICARE (1-800-633-4227).

NOTE: Due to system requirement, FISS has combined messages 15.19 and 15.20 so that,
when used for the same line item, both messages will appear on the same MSN.
Group Code: CO (Contractual Obligation) assigning financial liability to the provider
A/B MACs (Part A) shall deny for any covered dx audiology/therapy services related to cochlear implantation
with the following messages:
Use the following messages when denying services on claims:
• Submitted on a TOB other than 11X, 12X (except surgical procedures), 13X or 85X (Part A only), or
• submitted without diagnostic code Z00.6
• submitted without one of the CPT/HCPCs listed (92521-92524, 92507, 92601- 92604, L7510, L8614,
L8619, 69930)
CARC 50 - “These are non-covered services because this is not deemed a ‘medical necessity’
by the payer”
RARC N386 - “This decision was based on a National Coverage Determination (NCD). An
NCD provides a coverage determination as to whether a particular item or service is covered. A
copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not have web
access, you may contact the contractor to request a copy of the NCD.”
MSN 15.20 = “The following policies were used when we made this decision:
NCD 50. 3”
Spanish translation: “Las siguientes políticas fueron utilizadas cuando se tomó esta
decisión: NCD 50.3”)
Contractors processing institutional claims shall use the following MSN message in addition to
MSN 15.20:
MSN 15.19 - Local Coverage Determinations (LCDs) help Medicare decide what is covered.
An LCD was used for your claim. You can compare your case to the LCD, and send
information from your doctor if you think it could change our decision. Call 1-800-
MEDICARE (1-800-633-4227) for a copy of the LCD.
Spanish Version - Las Determinaciones Locales de Cobertura (LCDs en inglés) le
ayudan a decidir a Medicare lo que está cubierto. Un LCD se usó para su reclamación.
Usted puede comparar su caso con la determinación y enviar información de su médico
si piensa que puede cambiar nuestra decisión. Para obtener una copia del LCD, llame al
1-800-MEDICARE (1-800-633-4227).
NOTE: Due to system requirement, FISS has combined messages 15.19 and 15.20 so that,
when used for the same line item, both messages will appear on the same MSN.
Group Code: CO (Contractual Obligation) assigning financial liability to the provider

A/B/MACs (Part B) shall deny claims for evaluation and therapeutic services related to cochlear implantation.
NOTE: Modifiers -Q0/-Q1 do not need to be applied to these services (92601– 92604, 92521-92524 or any
applicable audiology codes).
Use the following messages when denying services on claims:
• Submitted without one of the CPT/HCPCs listed (92521-92524, 92507, 92601- 92604).
CARC 50 - “These are non-covered services because this is not deemed a ‘medical necessity’
by the payer”
RARC N386 - “This decision was based on a National Coverage Determination (NCD). An
NCD provides a coverage determination as to whether a particular item or service is covered. A
copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not have web
access, you may contact the contractor to request a copy of the NCD.”
MSN 15.20 - “The following policies were used when we made this decision: NCD 50. 3”
Spanish translation: “Las siguientes políticas fueron utilizadas cuando se tomó esta
decisión: NCD 50.3”)
Group Code - CO (Contractual Obligation) assigning financial liability to the provider
110 – Coverage and Billing for Ultrasound Stimulation for Nonunion Fracture Healing
(Rev. 597, Issued: 06-24-05, Effective: 04-27-05, Implementation: 08-01-05)
An ultrasonic osteogenic stimulator is a non-invasive device that emits low intensity, pulsed ultrasound. This
device is applied to the surface of the skin at the fracture site and ultrasound waves are emitted via a
conductive coupling gel to stimulate fracture healing. The ultrasonic osteogenic stimulators are not to be used
concurrently with other non-invasive osteogenic devices.
110.1 – Coverage Requirements
(Rev. 597, Issued: 06-24-05, Effective: 04-27-05, Implementation: 08-01-05)
Effective for dates of service on and after April 27, 2005, ultrasonic osteogenic stimulators are covered as
medically reasonable and necessary for the treatment of nonunion bone fractures prior to surgical intervention.
In demonstrating nonunion fractures, CMS expects:
• A minimum of 2 sets of radiographs, obtained prior to starting treatment with the osteogenic
stimulator, separated by a minimum of 90 days. Each radiograph set must include multiple views of
the fracture site accompanied with a written interpretation by a physician stating that there has been no
clinically significant evidence of fracture healing between the 2 sets of radiographs.
For further coverage information, please refer to the National Coverage Determinations Manual, Pub. 100-03,
chapter 1, section 150.2.
110.2 – Intermediary Billing Requirements
(Rev. 597, Issued: 06-24-05, Effective: 04-27-05, Implementation: 08-01-05)
The RHHIs will pay for ultrasonic osteogenic stimulators only when services are submitted on type of bills
(TOBs) listed under Pub. 100-04, Medicare Claims Processing Manual, chapter 32, section 100.3.
Fiscal intermediaries (FIs) must educate hospitals that there are no covered services for Ultrasonic
Osteogenic Stimulation for which hospitals can be paid by the FI.
NOTE: Hospitals can not bill for Ultrasonic Osteogenic Stimulators.
110.3 – Bill Types
(Rev. 597, Issued: 06-24-05, Effective: 04-27-05, Implementation: 08-01-05)
Only the following TOBs can bill for Ultrasonic Osteogenic Stimulators: 32X, 33X, 34X, which is payable
under the DMEPOS Fee Schedule.
NOTE: Ultrasonic Osteogenic Stimulators must be in the patient’s home health plan of care if billed on
TOBs 32X or 33X.
110.4 – Carrier and Intermediary Billing Instructions
(Rev. 597, Issued: 06-24-05, Effective: 04-27-05, Implementation: 08-01-05)
Effective for dates of service on or after April 27, 2005, contractors shall allow payment for ultrasonic
osteogenic stimulators with the following current procedural terminology (CPT) code:
• 20979 - Low intensity ultrasound stimulation to aid bone healing, noninvasive (nonoperative)
110.5 – DMERC Billing Instructions
(Rev. 816, Issued: 01-20-06, Effective: 04-27-05, Implementation: 04-03-06)
Effective for dates of service on or after April 27, 2005, DMERCs shall allow payment for ultrasonic
osteogenic stimulators with the following HCPCS codes:
E0760 for low intensity ultrasound (include modifier “KF”), or;
E1399 for other ultrasound stimulation (include modifier “KF”)
120 - Presbyopia-Correcting (P-C IOLS) and Astigmatism-Correcting Intraocular
Lenses (A-C IOLs) (General Policy Information)
(Rev. 1228; Issued: 04-27-07; Effective: 01-22-07; Implementation: 05-29-07)
Per CMS Ruling 05-01, issued May 3, 2005, Medicare will allow beneficiaries to pay additional charges
associated with insertion of a P-C IOL following cataract surgery.
• Presbyopia is a type of age-associated refractive error that results in progressive loss of the focusing
power of the lens of the eye, causing difficulty seeing objects at near distance, or close-up. Presbyopia
occurs as the natural lens of the eye becomes thicker and less flexible with age.
• A presbyopia-correcting IOL is indicated for primary implantation in the capsular bag of the eye for
the visual correction of aphakia (absence of the lens of the eye) following cataract extraction that is
intended to provide near, intermediate and distance vision without the need for eyeglasses or contact
lenses.

Per CMS-1536-Ruling, effective for services on and after January 22, 2007, Medicare will allow beneficiaries
to pay additional charges (which are non-covered by Medicare as these additional charges are not part of a
Medicare benefit category) for insertion of an A-C IOL.
• Regular astigmatism is a visual condition where part of an image is blurred due to uneven corneal
curvature. A normal cornea has the same curvature at all axes, whereas the curvature of an
astigmatic cornea differs in two primary axes, resulting in vision that is distorted at all distances.
• The A-C IOL is intended to provide what is otherwise achieved by two separate items; an
implantable conventional IOL (one that is not astigmatism-correcting) that is covered by Medicare,
and the surgical correction, eyeglasses or contact lenses that are not covered by Medicare.
A list of A-C IOLs and P-C IOLs can be accessed online at
http://www.cms.hhs.gov/HospitalOutpatientPPS/01_overview.asp
120.1 - Payment for Services and Supplies
(Rev. 1430; Issued: 02-01-08; Effective: 01-01-08; Implementation: 03-03-08)
For an IOL inserted following removal of a cataract in a hospital, on either an outpatient or inpatient basis,
that is paid under the hospital Outpatient Prospective Payment System (OPPS) or the Inpatient Prospective
Payment System (IPPS), respectively; or in a Medicare-approved ambulatory surgical center (ASC) that is
paid under the ASC fee schedule:
• Medicare does not make separate payment to the hospital or ASC for an IOL inserted subsequent to
extraction of a cataract. Payment for the IOL is packaged into the payment for the surgical cataract
extraction/lens replacement procedure.
• Any person or ASC, who presents or causes to be presented a bill or request for payment for an IOL
inserted during or subsequent to cataract surgery for which payment is made under the ASC fee
schedule, is subject to a civil money penalty.
• For a P-C IOL or A-C IOL inserted subsequent to removal of a cataract in a hospital, on either an
outpatient or inpatient basis, that is paid under the OPPS or the IPPS, respectively; or in a Medicare-
approved ASC that is paid under the ASC fee schedule:
• The facility shall bill for the removal of a cataract with insertion of a conventional IOL, regardless of
whether a conventional, P-C IOL, or A-C IOL is inserted. When a beneficiary receives a P-C or A-C
IOL following removal of a cataract, hospitals and ASCs shall report the same CPT code that is used
to report removal of a cataract with insertion of a conventional IOL. Physicians, hospitals and ASCs
may also report an additional HCPCS code, V2788, to indicate any additional charges that accrue
when a P-C IOL or A-C IOL is inserted in lieu of a conventional IOL until January 1, 2008. Effective
for A-C IOL insertion services on or after January 1, 2008, physicians, hospitals and ASCs should use
V2787 to report any additional charges that accrue. On or after January 1, 2008, physicians, hospitals,
and ASCs should continue to report HCPCS code V2788 to indicate any additional charges that accrue
for insertion of a P-C IOL. See Section 120.2 for coding guidelines.
• There is no Medicare benefit category that allows payment of facility charges for services and supplies
required to insert and adjust a P-C or A-C IOL following removal of a cataract that exceed the facility
charges for services and supplies required for the insertion and adjustment of a conventional IOL.
• There is no Medicare benefit category that allows payment of facility charges for subsequent
treatments, services and supplies required to examine and monitor the beneficiary who receives a P-C
or A-C IOL following removal of a cataract that exceeds the facility charges for subsequent treatments,
services and supplies required to examine and monitor a beneficiary after cataract surgery followed by
insertion of a conventional IOL.
A - For a P-C IOL or A-C IOL inserted in a physician's office
- A physician shall bill for a conventional IOL, regardless of a whether a conventional, P-C IOL, or A-
C IOL is inserted (see section 120.2, General Billing Requirements)
- There is no Medicare benefit category that allows payment of physician charges for services and
supplies required to insert and adjust a P-C or A-C IOL following removal of a cataract that exceed the
physician charges for services and supplies for the insertion and adjustment of a conventional IOL.
- There is no Medicare benefit category that allows payment of physician charges for subsequent
treatments, service and supplies required to examine and monitor a beneficiary following removal of a cataract
with insertion of a P-C or A-C IOL that exceed physician charges for services and supplies to examine and
monitor a beneficiary following removal of a cataract with insertion of a conventional IOL.
B - For a P-C IOL or A-C IOL inserted in a hospital
- A physician may not bill Medicare for a P-C or A-C IOL inserted during a cataract procedure
performed in a hospital setting because the payment for the lens is included in the payment made to the
facility for the surgical procedure.
- There is no Medicare benefit category that allows payment of physician charges for services and
supplies required to insert and adjust a P-C or A-C IOL following removal of a cataract that exceed the
physician charges for services and supplies required for the insertion of a conventional IOL.
C - For a P-C IOL or A-C IOL inserted in an Ambulatory Surgical Center
- Refer to Chapter 14, Section 40.3 for complete guidance on payment for P-C IOL or A-C IOL in
Ambulatory Surgical Centers.
120.2 - Coding and General Billing Requirements
(Rev. 1430; Issued: 02-01-08; Effective: 01-01-08; Implementation: 03-03-08)
Physicians and hospitals must report one of the following Current Procedural Terminology (CPT) codes on
the claim:
66982 - Extracapsular cataract removal with insertion of intraocular lens prosthesis (one stage
procedure), manual or mechanical technique (e.g., irrigation and aspiration or phacoemulsification), complex
requiring devices or techniques not generally used in routine cataract surgery (e.g., iris expansion device,
suture support for intraocular lens, or primary posterior capsulorrhexis) or performed on patients in the
amblyogenic development stage.
• 66983 - Intracapsular cataract with insertion of intraocular lens prosthesis (one stage procedure)
• 66984 - Extracapsular cataract removal with insertion of intraocular lens prosthesis (one stage
procedure), manual or mechanical technique (e.g., irrigation and aspiration or phacoemulsification)
• 66985 - Insertion of intraocular lens prosthesis (secondary implant), not associated with concurrent
cataract extraction
• 66986 - Exchange of intraocular lens
In addition, physicians inserting a P-C IOL or A-C IOL in an office setting may bill code V2632 (posterior
chamber intraocular lens) for the IOL. Medicare will make payment for the lens based on reasonable cost for a
conventional IOL. Place of Service (POS) = 11.
Effective for dates of service on and after January 1, 2006, physician, hospitals and ASCs may also bill the
non-covered charges related to the P-C function of the IOL using HCPCS code V2788. Effective for dates of
service on and after January 22, 2007 through January 1, 2008, non-covered charges related to A-C function
of the IOL can be billed using HCPCS code V2788. The type of service indicator for the non-covered billed
charges is Q. (The type of service is applied by the Medicare carrier and not the provider). Effective for A-C
IOL insertion services on or after January 1, 2008, physicians, hospitals and ASCs should use V2787 rather
than V2788 to report any additional charges that accrue.
When denying the non-payable charges submitted with V2787 or V2788, contractors shall use an appropriate
Medical Summary Notice (MSN) such as 16.10 (Medicare does not pay for this item or service) and an
appropriate claim adjustment reason code such as 96 (non-covered charges) for claims submitted with the
non-payable charges.
Hospitals and physicians may use the proper CPT code(s) to bill Medicare for evaluation and management
services usually associated with services following cataract extraction surgery, if appropriate.
A - Applicable Bill Types
The hospital applicable bill types are 12X, 13X, 83X and 85X.
B - Other Special Requirements for Hospitals
Hospitals shall continue to pay CAHs method 2 claims under current payment methodologies for conditional
IOLs.
120.3 - Provider Notification Requirements
(Rev. 1228; Issued: 04-27-07; Effective: 01-22-07; Implementation: 05-29-07)
When a beneficiary requests insertion of a P-C or A-C IOL instead of a conventional IOL following removal
of a cataract:
• Prior to the procedure to remove a cataractous lens and insert a P-C or A-C lens, the facility and the
physician must inform the beneficiary that Medicare will not make payment for services that are
specific to the insertion, adjustment or other subsequent treatments related to the P-C or A-C
functionality of the IOL.
• The P-C or A-C functionality of a P-C or A-C IOL does not fall into a Medicare benefit category, and,
therefore, is not covered. Therefore, the facility and physician are not required to provide an
Advanced Beneficiary Notice to beneficiaries who request a P-C or A-C IOL.

• Although not required, CMS strongly encourages facilities and physicians to issue a Notice of
Exclusion from Medicare Benefits to beneficiaries in order to clearly identify the non-payable aspects
of a P-C or A-C IOL insertion. This notice may be found in English at
http:\\cms.hhs.gov/medicare/bni/20007_English.pdf
• Spanish language at: http://cms.hhs.gov/medicare/bni/20007_Spanish.pdf.
120.4 - Beneficiary Liability
(Rev. 1228; Issued: 04-27-07; Effective: 01-22-07; Implementation: 05-29-07)
When a beneficiary requests insertion of a P-C or A-C IOL instead of a conventional IOL following removal
of a cataract and that procedure is performed, the beneficiary is responsible for payment of facility and
physician charges for services and supplies attributable to the P-C or A-C functionality of the P-C or A-C
IOL:
• In determining the beneficiary's liability, the facility and physician may take into account any
additional work and resources required for insertion, fitting, vision acuity testing, and monitoring of
the P-C or A-C IOL that exceed the work and resources attributable to insertion of a conventional IOL.
The physician and the facility may not charge for cataract extraction with insertion of a P-C or A-C
IOL unless the beneficiary requests this service.
o The physician and the facility may not require the beneficiary to request a P-C or A-C IOL as a
condition of performing a cataract extraction with IOL insertion.
130 - External Counterpulsation (ECP) Therapy
(Rev. 898, Issued: 03-31-06; Effective/Implementation Dates: 03-31-06)
Commonly referred to as enhanced external counterpulsation, is a non-invasive outpatient treatment for
coronary artery disease refractory medical and/or surgical therapy. Effective for dates of service July 1, 1999,
and after, Medicare will cover ECP when its use is in patients with stable angina (Class III or Class IV,
Canadian Cardiovascular Society Classification or equivalent classification) who, in the opinion of a
cardiologist or cardiothoracic surgeon, are not readily amenable to surgical intervention, such as PTCA or
cardiac bypass, because:
• Their condition is inoperable, or at high risk of operative complications or post-operative failure;
• Their coronary anatomy is not readily amenable to such procedures; or
• They have co-morbid states that create excessive risk.
(Refer to Publication 100-03, section 20.20 for further coverage criteria.)
130.1 - Billing and Payment Requirements
(Rev. 12109; Issued:06-29-23; Effective: 10-02-23; Implementation: 10-02-23)
Effective for dates of service on or after January 1, 2000, use HCPCS code G0166 (External counterpulsation,
per session) to report ECP services. The codes for external cardiac assist (92971), ECG rhythm strip and
report (93040 or 93041), pulse oximetry (94760 or 94761) and plethysmography (93922 or 93923) or other
monitoring tests for examining the effects of this treatment are not clinically necessary with this service and
should not be paid on the same day, unless they occur in a clinical setting not connected with the delivery of
the ECP. Daily evaluation and management service, e.g., 99201- 99205, 99211-99215, 99217-99220, 99241-
99245, and G0463 cannot be billed with the ECP treatments. Any evaluation and management service must be
justified with adequate documentation of the medical necessity of the visit. Deductible and coinsurance apply.
Note: Please note that effective December 31, 2020 evaluation and management service code 99201 is end-
dated. Effective December 31, 2022 codes 99217,99218,99219,99220 and 99241 are end dated. For Part A,
remove CPT codes 99202-99215, 99242-99245 and replace with G0463 (the OPPS equivalent of E/M codes)
effective retroactive to 10/1/2015.
130.2 - Special Intermediary Billing and Payment Requirements
(Rev. 898, Issued: 03-31-06; Effective/Implementation Dates: 03-31-06)
Payment is made to hospitals for the facility costs it incurs under Part B on a reasonable cost basis. Payment is
also made to PPS-exempt hospitals for the facility costs it incurs on a reasonable cost basis. Deductible and
coinsurance apply.
Applicable bill types are 12X, 13X, 83X or 85X.
140 - Cardiac Rehabilitation (CR) Programs, Intensive Cardiac Rehabilitation (ICR)
Programs, and Pulmonary Rehabilitation (PR) Programs On or After January 1, 2024
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
Cardiac rehabilitation (CR) means a physician or nonphysician practitioner supervised program that furnishes
physician prescribed exercise; cardiac risk factor modification, including education, counseling, and behavioral
intervention; psychosocial assessment; and outcomes assessment. Intensive cardiac rehabilitation (ICR)
program means a physician or nonphysician practitioner supervised program that furnishes CR and has shown,
in peer-reviewed published research, that it improves patients’ cardiovascular disease through specific outcome
measurements described in 42 CFR 410.49(c). Nonphysician practitioner means a physician assistant, nurse
practitioner, or clinical nurse specialist as those terms are defined in section 1861(aa)(5)(A) of the Social
Security Act (the Act).
Effective January 1, 2024, Medicare Part B pays for CR/ICR if specific criteria are met by the Medicare
beneficiary, the CR/ICR program itself, the setting in which it is administered, and the physician administering
the program.
Pulmonary rehabilitation (PR) means a physician or nonphysician practitioner supervised program for chronic
obstructive pulmonary disease (COPD) and certain other chronic respiratory diseases designed to optimize
physical and social performance and autonomy. Nonphysician practitioner means a physician assistant, nurse
practitioner, or clinical nurse specialist as those terms are defined in section 1861(aa)(5)(A) of the Act.
Effective January 1, 2024, Medicare Part B pays for PR if specific criteria are met by the Medicare beneficiary,
the PR program itself, the setting in which it is administered, and the physician administering the program, as
outlined below.
140.1 – CR Program Services Furnished On or Before December 31, 2009
(Rev. 11426; Issued: 05-20-22; Effective: 01-01-22; Implementation: 07-05-22)
Medicare covers CR exercise programs for patients who meet the following criteria:
• Have a documented diagnosis of acute myocardial infarction (MI) within the preceding 12
months; or
• Have had coronary bypass surgery; or,
• Have stable angina pectoris; or,
• Have had heart valve repair/replacement; or,
• Have had percutaneous transluminal coronary angioplasty (PTCA) or coronary
stenting; or,
• Have had a heart or heart-lung transplant.

Effective for dates of services on or after March 22, 2006, services provided in connection with a CR exercise
program may be considered reasonable and necessary for up to 36 sessions. Patients generally receive 2 to 3
sessions per week for 12 to 18 weeks. The contractor has discretion to cover CR beyond 18 weeks. Coverage
must not exceed a total of 72 sessions for 36 weeks.
CR programs shall be performed incident to physician’s services in outpatient hospitals, or outpatient settings
such as clinics or offices. Follow the policies for services incident to the services of a physician as they apply in
each setting. For example, see Pub. 100-02, Chapter 6, §2.4.1, and Pub. 100-02, Chapter 15, §60.1. (Refer to
Publication 100-03, §20.10 for further coverage guidelines.)
140.1.1 - Coding Requirements for Cardiac Rehabilitation Services Furnished On or
Before Dec. 31, 2009
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
The following are the applicable Healthcare Common Procedure Coding System (HCPCS) codes:
93797 - Physician or other qualified health care professional services for outpatient cardiac rehabilitation;
without continuous
ECG monitoring (per session); and
93798 - Physician or other qualified health care professional services for outpatient cardiac rehabilitation; with
continuous ECG
monitoring (per session).
Note: The above HCPCS descriptors are effective January 1, 2013.
Effective for dates of service on or after January 1, 2008, and before January 1, 2010, providers and
practitioners may report more than one unit of CPT code 93797 or 97398 for a date of service if more than one
CR session lasting at least 1 hour each is provided on the same day. In order to report more than one session for
a given date of service, each session must last a minimum of 60 minutes. For example, if the CR provided on a
given day total 1 hour and 50 minutes, then only one session should be billed to report the CR provided on that
day.
140.2 – Cardiac Rehabilitation Program Services Effective for Dates of Service On or
After January 1, 2024
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
As specified at 42 CFR 410.49, Medicare Part B covers CR for beneficiaries who have experienced one or more
of the following:
• An acute MI within the preceding 12 months;
• A coronary artery bypass surgery;
• Current stable angina pectoris;
• Heart valve repair or replacement;
• PTCA or coronary stenting;
• A heart or heart-lung transplant;
• Stable, chronic heart failure defined as patients with left ventricular ejection fraction
of 35% or less and New York Heart Association (NYHA) class II to IV symptoms despite being on optimal
heart failure therapy for at least 6 weeks, on or after February 18, 2014; or,
• Other cardiac conditions as specified through a national coverage determination (NCD).
CR must include all of the following components:
• Physician prescribed exercise each day CR items and
services are furnished.
• Cardiac risk factor modification, including education, counseling, and behavioral
intervention, tailored to the individual’s needs.
• Psychosocial assessment.
• Outcomes assessment.
• An individualized treatment plan detailing how components are utilized for each
patient. The individualized treatment plan must be established, reviewed, and signed
by a physician every 30 days.
Medicare Part B pays for CR in a physician’s office or a hospital outpatient setting. All settings must have a
physician or nonphysician practitioner immediately available and accessible for medical consultations and
emergencies at all times when items and services are being furnished under the program. This provision is
satisfied if the physician or nonphysician practitioner meets the requirements for direct supervision for
physician office services, at 42 CFR 410.26, and for hospital outpatient services at 42 CFR 410.27.
Note: Nonphysician practitioners are eligible to supervise CR effective January 1, 2024.
As specified at 42 CFR 410.49(f)(1), the number of CR sessions are limited to a maximum of 2 1-hour sessions
per day for up to 36 sessions over up to 36 weeks with the option for an additional 36 sessions over an extended
period of time if approved by the
Medicare Administrative Contractor (MAC).
140.2.1 – Coding Requirements for CR Services Furnished On or After January 1, 2010
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
The following are the applicable Current Procedural Technology (CPT) codes for CR services:
93797 Physician or other qualified health care professional services for outpatient cardiac rehabilitation;
without continuous ECG monitoring (Per Session)
93798 Physician or other qualified care health professional services for outpatient cardiac rehabilitation; with
continuous ECG monitoring (Per Session)
Note: The above HCPCS descriptors are effective January 1, 2013.
Effective for dates of service on or after January 1, 2010, hospitals and practitioners may report a maximum of
2 1-hour sessions per day. In order to report one session of CR in a day, the duration of treatment must be at
least 31 minutes. Two sessions of CR may only be reported in the same day if the duration of treatment is at
least 91 minutes. In other words, the first session would account for 60 minutes and the second session would
account for at least 31 minutes if two sessions are reported. If several shorter periods of CR are furnished on a
given day, the minutes of service during those periods must be added together for reporting in 1-hour session
increments.
Example: If the patient receives 20 minutes of CR in the day, no CR session may be reported because less than
31 minutes of services were
furnished.
Example: If a patient receives 20 minutes of CR in the morning and 35 minutes of CR in the afternoon of a
single day, the hospital or practitioner would report 1 session of CR under 1 unit of the appropriate CPT code
for the total duration of 55 minutes of CR on that day.
Example: If the patient receives 70 minutes of CR in the morning and 25 minutes of CR in the afternoon of a
single day, the hospital or practitioner would report two sessions of CR under the appropriate CPT code(s)
because the total duration of CR on that day of 95 minutes exceeds 90 minutes.
Example: If the patient receives 70 minutes of CR in the morning and 85 minutes of CR in the afternoon of a
single day, the hospital or practitioner would report two sessions of CR under the appropriate CPT code(s) for
the total duration of CR of 155 minutes. A maximum of two sessions per day may be reported, regardless of the
total duration of CR.
sessions after 36 (to include completed ICR sessions prior to switch). In these cases, and consistent with the
information above, the -KX modifier must be included on the claim should the beneficiary participate in more
than 36 CR sessions following the switch.
See Pub. 100-06, Medicare Financial Management Manual, chapter 6, section 420, and Pub.
100-02, Medicare Benefit Policy Manual, chapter 15, section 232, and Pub. 100-08, Medicare
Program Integrity Manual, chapter 10, section 10.2.2.5 for detailed information regarding CR and ICR policy
and claims processing.
140.2.2 – Claims Processing Requirements for Cardiac Rehabilitation (CR) and Intensive
Cardiac Rehabilitation (ICR) Services Furnished On or After January 1, 2010
(Rev. 11426; Issued: 05-20-22; Effective: 01-01-22; Implementation: 07-05-22)
NOTE: A beneficiary may switch from an ICR program to a CR program. The beneficiary is limited to a one-
time switch, multiple switches are not allowable. Once the beneficiary switches from ICR to CR he or she will
be limited to the number of sessions remaining in the program. For example, a beneficiary who switches from
ICR to CR after 12 sessions will have 24 sessions of CR remaining, (i.e., 12 sessions of ICR + 24 sessions of
CR = total of 36 sessions). Should a beneficiary experience more than one indication simultaneously, he or she
may participate in a single series of CR or ICR sessions (i.e., a patient who had a MI within 12 months and
currently experiences stable angina is entitled to one series of CR sessions, up to 36 1-hour sessions with
contractor discretion for an additional 36 sessions; or one series of ICR sessions, up to 72 1-hour sessions over a
period up to 18 weeks). Beneficiaries may not switch from CR to ICR. Upon completion of a CR or ICR
program, beneficiaries must experience another indication in order to be eligible for coverage of more CR or
ICR.
Contractors shall accept the inclusion of the -KX modifier on the claim line(s) as an attestation by the provider
of the service that documentation is on file verifying that further treatment beyond 36 sessions of CR up to a
total of 72 sessions meets the requirements of the medical policy or, for ICR, that any further sessions beyond
72 sessions within a 126-day period counting from the date of the first session, or for any sessions provided
after 126 days from the date of the first session, meet the requirements of the medical policy. Beneficiaries who
switch from ICR to CR may also be eligible for up to 72 combined sessions with contractor discretion for CR
sessions after 36 (to include completed ICR sessions prior to switch). In these cases, and consistent with the
information above, the -KX modifier must be included on the claim should the beneficiary participate in more
than 36 CR sessions following the switch.
See Pub. 100-06, Medicare Financial Management Manual, chapter 6, section 420, and Pub.
100-02, Medicare Benefit Policy Manual, chapter 15, section 232, and Pub. 100-08, Medicare
Program Integrity Manual, chapter 10, section 10.2.2.5 for detailed information regarding CR and ICR policy
and claims processing.
140.2.2.1 – Correct Place of Service (POS) Code for CR and ICR Services on Professional
Claims
(Rev. 3058, Issued: 08-29-14, Effective: 02-18-14, Implementation: 08-18-14)
Effective for claims with dates of service on and after January 1, 2010, place of service (POS) code 11 shall be
used for CR and ICR services provided in a physician’s office and POS 22 shall be used for services provided in
a hospital outpatient setting. All other POS codes shall be denied. Contractors shall adjust their prepayment
procedure edits as appropriate.
The following messages shall be used when contractors deny CR and ICR claims for POS:
Claim Adjustment Reason Code (CARC) 171 – Payment is denied when performed/billed by this type of
provider in this type of facility.
NOTE: Refer to the 832 Healthcare Policy Identification Segment (loop 2110 Service payment Information
REF), if present.
Remittance Advice Remark Code (RARC) N428 - Service/procedure not covered when performed in this place
of service.
Medicare Summary Notice (MSN) 21.25 - This service was denied because Medicare only covers this service in
certain settings.
Group Code PR (Patient Responsibility) - Where a claim is received with the GA modifier indicating that a
signed ABN is on file.
Group Code CO (Contractor Responsibility) – Where a claim is received with the GZ modifier indicating that
no signed ABN is on file.
140.2.2.2 – Requirements for CR and ICR Services on Institutional Claims
(Rev. 3084, Issued: 10-03-14, Effective: 05-06-14, Implementation: 11-04-14)
Effective for claims with dates of service on and after January 1, 2010, contractors shall pay for CR and ICR
services when submitted on Types of Bill (TOBs) 13X and 85X only. All other TOBs shall be denied.
The following messages shall be used when contractors deny CR and ICR claims for TOBs other than 13X and
85X:
Claim Adjustment Reason Code (CARC) 171 – Payment is denied when performed/billed by this type of
provider in this type of facility. NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110
Service Payment Information REF), if present.
Remittance Advice Remark Code (RARC) N428 - Service/procedure not covered when performed in this place
of service.
Medicare Summary Notice (MSN) 21.25 - This service was denied because Medicare only covers this service in
certain settings.
Group Code PR (Patient Responsibility) – Where a claim is received with the GA modifier indicating that a
signed ABN is on file.
Group Code CO (Contractor Responsibility) – Where a claim is received with the GZ modifier indicating that
no signed ABN is on file.
140.2.2.3 – Frequency Edits for CR and ICR Claims
(Rev. 11426; Issued: 05-20-22; Effective: 01-01-22; Implementation: 07-05-22)
Effective for claims with dates of service on or after January 1, 2010, contractors shall deny all CR claims (both
professional and institutional claims) that exceed 2 units per date of service for CR and 6 units per date of
service for ICR.
The following messages shall be used when contractors deny CR and ICR claims for exceeding units per date of
service:
CARC 119 - Benefit maximum for this time period or occurrence has been reached.
RARC N362 - The number of days or units of service exceeds our acceptable maximum.
MSN 20.5 - These services cannot be paid because your benefits are exhausted at this time.
Spanish Version - Estos servicios no pueden ser pagados porque sus beneficios se han agotado.
Group Code PR – Where a claim is received with the GA modifier indicating that a signed ABN is on file.
Group Code CO – Where a claim is received with the GZ modifier indicating that no signed ABN is on file.
Contractors shall not research and adjust CR claims (HCPCS 93797 and 93798) paid for more than 2 units on
the same date of service processed prior to the implementation of edits. However, contractors may adjust claims
brought to their attention.
Contractors shall not research and adjust ICR claims (HCPCS G0422 and G0423) paid for more than 6 units on
the same date of service processed prior to the implementation of edits. However, contractors may adjust claims
brought to their attention.
140.2.2.4 – Edits for CR Services Exceeding 36 Sessions
(Rev. 11426; Issued: 05-20-22; Effective: 01-01-22; Implementation: 07-05-22)
Effective for claims with dates of service on or after January 1, 2010, contractors shall deny all claims with
HCPCS 93797 and 93798 (both professional and institutional claims) that exceed 36 CR sessions when a -KX
modifier is not included on the claim line.
The following messages shall be used when contractors deny CR claims that exceed 36 sessions, when a -KX
modifier is not included on the claim line:
-CARC-) 119 – Benefit maximum for this period or occurrence has been reached.
RARC N435 - Exceeds number/frequency approved/allowed within time period without support documentation.
MSN 23.17- Medicare won’t cover these services because they are not considered medically necessary.
Spanish Version - Medicare no cubrirá estos servicios porque no son considerados necesarios por razones
médicas.
Group Code PR – Where a claim is received with the GA modifier indicating that a signed ABN is on file.
Group Code CO – Where a claim is received with the GZ modifier indicating that no signed ABN is on file.
Contractors shall not research and adjust CR claims paid for more than 36 sessions processed prior to the
implementation of Common Working File (CWF) edits. However, contractors may adjust claims brought to
their attention.
140.2.2.5 – Edits for ICR Services Exceeding 126 Days and 72 Sessions
(Rev. 1974, Issued: 05-21-10, Effective: 01-10-10, Implementation: 10-04-10)
Effective for claims with dates of service on and after January 1, 2010, CWF shall reject ICR claims (G0422
and G0423) that exceed 72 sessions or where any billed sessions were provided after126 days from the date of
the first session and a KX modifier is not included on the claim line.
The following messages shall be used when contractors deny ICR claims that exceed 72 sessions or where any
billed sessions were received after the 126 days from the date of the first session:
Claim Adjustment Reason Code (CARC) 119 - Benefit maximum for this time period or occurrence has been
reached.
RARC N435 - Exceeds number/frequency approved/allowed within time period without support documentation.
MSN 20.5 - These services cannot be paid because your benefits are exhausted at this time.
Spanish Version - Estos servicios no pueden ser pagados porque sus beneficios se han agotado.
Group Code PR (Patient Responsibility) – Where a claim is received with the GA modifier indicating that a
signed ABN is on file.
Group Code CO (Contractor Responsibility) – Where a claim is received with the GZ modifier indicating that
no signed ABN is on file.
Contractors shall not research and adjust ICR claims paid for more than 72 sessions or where any billed sessions
were received after 126 days from the date of the first session that were processed prior to the implementation
of CWF edits. However, contractors may adjust claims brought to their attention.
140.2.2.6 – Supplier Specialty Code 31 Requirements for ICR Claims
(Rev. 1974, Issued: 05-21-10, Effective: 01-10-10, Implementation: 10-04-10)
Effective for claims with dates of service on and after January 1, 2010, contractors shall pay for ICR services
when submitted by providers enrolled as the new supplier specialty code 31 for ICR. ICR services submitted by
providers enrolled as other than the new supplier specialty code 31 for ICR are to be denied using the following
messages:
CARC 8: “The procedure code is inconsistent with the provider type/specialty (taxonomy). NOTE: Refer to
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.”
RARC N95: “This provider type may not bill this service.”

MSN 21.18 – “This item or service is not covered when performed or ordered by this provider.”
Spanish Version: Este servicio no está cubierto cuando es ordenado o rendido por este proveedor.
Group Code PR (Patient Responsibility) – Where a claim is received with the GA modifier indicating that a
signed ABN is on file.
Group Code CO (Contractor Responsibility) – Where a claim is received with the GZ modifier indicating that
no signed ABN is on file.
140.3 – ICR Program Services Effective for Dates of Service On or After January 1, 2024
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
As specified at 42 CFR 410.49, Medicare Part B covers ICR for beneficiaries who have experienced one or
more of the following:
• An acute MI within the preceding 12 months;
• A coronary artery bypass surgery;
• Current stable angina pectoris;
• Heart valve repair or replacement;
• PTCA or coronary stenting;
• A heart or heart-lung transplant;
• Stable, chronic heart failure defined as patients with left ventricular ejection fraction of 35% or less and
NYHA class II to IV symptoms despite being on optimal heart failure therapy for at least 6 weeks, on or after
February 9, 2018; or,
• Other cardiac conditions as specified through an NCD. The NCD process may also be used to specify non-
coverage of a cardiac condition for ICR if coverage is not supported by clinical evidence.
ICR must include all of the following components:
• Physician prescribed exercise each day CR items and services are furnished.
• Cardiac risk factor modification, including education, counseling, and behavioral
intervention, tailored to the individual’s needs.
• Psychosocial assessment.
• Outcomes assessment.
• An individualized treatment plan detailing how components are utilized for each
patient. The individualized treatment plan must be established, reviewed, and signed
by a physician every 30 days.
A list of approved ICR programs, identified through the NCD process, will be listed in the Federal Register and
is available on the CMS website at https://www.cms.gov/Medicare/Medicare-General-
Information/MedicareApprovedFacilitie/ICR. In order to be approved, a program must demonstrate through
peer-reviewed, published research that it has accomplished one or more of the following for its patients:
• Positively affected the progression of coronary heart disease.
• Reduced the need for coronary bypass surgery.
• Reduced the need for percutaneous coronary interventions.
An ICR program must also demonstrate through peer-reviewed published research that it accomplished a
statistically significant reduction in 5 or more of the following measures for patients from their levels before CR
services to after CR services:
• Low density lipoprotein.
• Triglycerides.
• Body mass index.
• Systolic blood pressure.
• Diastolic blood pressure.
• The need for cholesterol, blood pressure, and diabetes medications.
Medicare Part B pays for ICR in a physician’s office or a hospital outpatient setting. All settings must have a
physician or nonphysician practitioner immediately available and accessible for medical consultations and
emergencies at all times when items and services are being furnished under the program. This provision is
satisfied if the physician or nonphysician practitioner meets the requirements for direct supervision for
physician office services, at 42 CFR 410.26, and for hospital outpatient services at 42 CFR 410.27.
Note: Nonphysician practitioners are eligible to supervise ICR effective January 1, 2024.
As specified at 42 CFR 410.49(f)(2), ICR sessions are limited to 72 1-hour sessions (as defined in section
1848(b)(5) of the Act), up to 6 sessions per day, over a period of up to 18 weeks.
140.3.1 – Coding Requirements for ICR Services Furnished On or After January 1, 2010
(Rev. 11426; Issued: 05-20-22; Effective: 01-01-22; Implementation: 07-05-22)
The following are the applicable HCPCS codes for ICR:
G0422 (Intensive cardiac rehabilitation; with or without continuous ECG monitoring,
with exercise, per hour, per session)
G0423 (Intensive cardiac rehabilitation; with or without continuous ECG monitoring,
without exercise, per hour, per session)
Effective for dates of service on or after January 1, 2010, hospitals and practitioners may report a maximum of
6 1-hour sessions per day. In order to report one session of ICR in a day, the duration of treatment must be at
least 31 minutes. Additional sessions of ICR beyond the first session may only be reported in the same day if
the duration of treatment is 31 minutes or greater beyond the hour increment. In other words, in order to report 6
sessions of ICR on a given date of service, the first five sessions would account for 60 minutes each and the
sixth session would account for at least 31 minutes. If several shorter periods of ICR are furnished on a given
day, the minutes of service during those periods must be added together for reporting in 1-hour session
increments.
Example: If the patient receives 20 minutes of ICR in the day, no ICR session may be reported because less
than 31 minutes of services were furnished.
Example: If a patient receives 20 minutes of ICR in the morning and 35 minutes of ICR in the afternoon of a
single day, the hospital or practitioner would report 1 session of ICR under 1 unit of the appropriate HCPCS
code for the total duration of 55 minutes of ICR on that day.
Example: If the patient receives 70 minutes of ICR in the morning and 25 minutes of ICR in the afternoon of a
single day, the hospital or practitioner would report two sessions of ICR under the appropriate HCPCS code(s)
because the total duration of ICR on that day of 95 minutes exceeds 90 minutes.
Example: If the patient receives 70 minutes of ICR in the morning and 85 minutes of ICR in the afternoon of a
single day, the hospital or practitioner would report three sessions of ICR under the appropriate HCPCS code(s)
because the total duration of ICR on that day is 155 minutes, which exceeds 150 minutes and is less than 211
minutes.
140.4 – PR Program Services Effective for Dates of Service On or After January 1, 2024
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
As specified in 42 CFR 410.47, Medicare Part B covers PR for beneficiaries:
• With moderate to very severe COPD (defined as GOLD classification II, III and IV), when referred by
the physician treating the chronic respiratory disease;
• Who have had confirmed or suspected COVID-19 and experience persistent symptoms that include
respiratory dysfunction for at least four weeks (effective January 1, 2022);
• Additional medical indications for coverage for PR may be established through an NCD.
PR must include all of the following components:
• Physician prescribed exercise during each pulmonary rehabilitation session.
• Education or training that is closely and clearly related to the individual’s care and treatment which is tailored
to the individual’s needs and assists in achievement of goals toward independence in activities of daily living,
adaptation to limitations and improved quality of life. Education must include information on respiratory
problem management and, if appropriate, brief smoking cessation counseling.
• Psychosocial assessment.
• Outcomes assessment.
• An individualized treatment plan detailing how components are utilized for each patient. The individualized
treatment plan must be established, reviewed, and signed by a physician every 30 days.
Medicare Part B pays for PR in a physician’s office or a hospital outpatient setting. All settings must have the
following: (i) A physician or nonphysician practitioner immediately available and accessible for medical
consultations and emergencies at all times when items and services are being furnished under the program. This
provision is satisfied if the physician or nonphysician practitioner meets the requirements for direct supervision
for physician office services, at 42 CFR 410.26, and for hospital outpatient services at 42 CFR 410.27, and, (ii)
The necessary cardio-pulmonary, emergency, diagnostic, and therapeutic life-saving equipment accepted by the
medical community as medically necessary (for example, oxygen, cardiopulmonary resuscitation equipment,
and defibrillator) to treat chronic respiratory disease.
Note: Nonphysician practitioners are eligible to supervise PR effective January 1, 2024.
As specified at 42 CFR 410.47(e), the number of PR sessions are limited to a maximum of 2 1-hour sessions per
day for up to 36 sessions over up to 36 weeks with the option for an additional 36 sessions over an extended
period of time if approved by the MACs.
140.4.1 – Coding Requirements for PR Services Furnished On or After January 1, 2010
(Rev. 11426; Issued: 05-20-22; Effective: 01-01-22; Implementation: 07-05-22)
The following are the applicable HCPCS codes for PR:
Effective January 1, 2010 through December 31, 2021
G0424 (Pulmonary rehabilitation, including exercise (includes monitoring), per hour, per
session)
Effective January 1, 2022
94625 (Physician or other qualified health care professional services for outpatient pulmonary rehabilitation;
without continuous oximetry monitoring (per session))
94626 (Physician or other qualified health care professional services for outpatient pulmonary rehabilitation;
with continuous oximetry monitoring (per session)
Effective for dates of service on or after January 1, 2010, hospitals and practitioners may report a maximum of
2 1-hour sessions per day. In order to report one session of PR in a day, the duration of treatment must be at
least 31 minutes. Two sessions of PR may only be reported in the same day if the duration of treatment is at
least 91 minutes. In other words, the first session would account for 60 minutes and the second session would
account for at least 31 minutes, if two sessions are reported. If several shorter periods of PR are furnished on a
given day, the minutes of service during those periods must be added together for reporting in 1-hour session
increments.
Example: If the patient receives 20 minutes of PR in the day, no PR session may be reported because less than
31 minutes of services were furnished.
Example: If a patient receives 20 minutes of PR in the morning and 35 minutes of PR in the afternoon of a
single day, the hospital or practitioner would report 1 session of PR under 1 unit of HCPCS code/CPT code for
the total duration of 55 minutes of PR on that day.
Example: If the patient receives 70 minutes of pulmonary rehabilitation services in the morning and 25 minutes
of pulmonary rehabilitation services in the afternoon of a single day, the hospital or practitioner would report
two sessions of pulmonary rehabilitation services under the HCPCS G-code/CPT codes because the total
duration of pulmonary rehabilitation services on that day of 95 minutes exceeds 90 minutes.
Example: If the patient receives 70 minutes of pulmonary rehabilitation services in the morning and 85 minutes
of pulmonary rehabilitation services in the afternoon of a single day, the hospital or practitioner would report
two sessions of pulmonary rehabilitation services under the HCPCS G-code/CPT codes for the total duration of
pulmonary rehabilitation services of 155 minutes. A maximum of two sessions per day may be reported,
regardless of the total duration of pulmonary rehabilitation services.
140.4.2 – Claims Processing Requirements for Pulmonary Rehabilitation (PR) Services
Furnished On or After January 1, 2010
(Rev. 1966, Issued: 05-07-10, Effective: 01-01-10, Implementation: 10-04-10)
140.4.2.1 – Correct Place of Service (POS) Code for PR Services on Professional Claims
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Effective for claims with dates of service on and after January 1, 2010, place of service (POS) code 11
shall be used for pulmonary rehabilitation (PR) services provided in a physician’s office and POS 22 shall
be used for services provided in a hospital outpatient setting. All other POS codes shall be denied.
Medicare contractors shall adjust their prepayment procedure edits as appropriate.
The following messages shall be used when Medicare contractors deny PR claims for POS:
CARC 96: “Non-covered charge(s).”
RARC N428: “Service/procedure not covered when performed in this place of service.”
Medicare Summary Notice (MSN) 21.25: “This service was denied because Medicare only covers this
service in certain settings.”
Spanish Version: El servicio fue denegado porque Medicare solamente lo cubre en ciertas
situaciones."
NOTE: This is a new MSN message.
Contractors shall use Group Code PR (Patient `Responsibility) assigning financial liability to the beneficiary,
if a claim is received with a GA modifier indicating a signed ABN is on file.
Contractors shall use Group Code CO (Contractual Obligation) assigning financial liability to the provider, if
a claim is received with a GZ modifier indicating no signed ABN is on file.
140.4.2.2 – Requirements for PR Services on Institutional Claims
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Effective for claims with dates of service on and after January 1, 2010, Medicare contractors shall pay for
PR services when submitted on a type of bill (TOB) 13X and 85X only, along with revenue code 0948.
All other TOBs shall be denied.
The following messages shall be used when Medicare contractors deny PR claims for TOB:
CARC 96: “Non-covered charge(s).”
RARC N428: “Service/procedure not covered when performed in this place of service.”
Medicare Summary Notice (MSN) 21.25: “This service was denied because Medicare only covers this
service in certain settings.”
Spanish Version: El servicio fue denegado porque Medicare solamente lo cubre en ciertas
situaciones."
NOTE: This is a new MSN message.
Contractors shall use Group Code PR (Patient `Responsibility) assigning financial liability to the beneficiary,
if a claim is received with a GA modifier indicating a signed ABN is on file.
Contractors shall use Group Code CO (Contractual Obligation) assigning financial liability to the provider, if
a claim is received with a GZ modifier indicating no signed ABN is on file.
140.4.2.3 – Daily Frequency Edits for PR Claims
(Rev. 1966, Issued: 05-07-10, Effective: 01-01-10, Implementation: 10-04-10)
Effective for claims with dates of service on or after January 1, 2010, Medicare contractors shall deny all PR
claims (both professional and institutional claims) that exceed two units on the same date of service.
The following messages shall be used when Medicare contractors deny PR claims for exceeding the daily
frequency limit:
CARC 119: “Benefit maximum for this time period or occurrence has been reached.”
RARC N362: “The number of days or units of service exceeds our acceptable maximum.”
MSN 20.5: “These services cannot be paid because your benefits are exhausted at this time.”
Spanish Version: “Estos servicios no pueden ser pagados porque sus beneficios se han agotado.”
Contractors shall use Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a
claim is received with a GA modifier indicating a signed ABN is on file.
Contractors shall use Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a
claim is received with a GZ modifier indicating no signed ABN is on file.
140.4.2.4 – Edits for PR Services Exceeding 36 Sessions
(Rev. 1966, Issued: 05-07-10, Effective: 01-01-10, Implementation: 10-04-10)
When a beneficiary has reached 37 PR sessions, CWF shall reject the claims to the contractors if the KX
modifier is not included on the claim line. Effective for claims with dates of service on or after January 1, 2010,
Medicare contractors shall deny all claims (both professional and institutional claims) that exceed 36 PR
sessions without a KX modifier included on the claim line.
The following messages shall be used when Medicare contractors deny PR claims that exceed 36 sessions,
without the KX modifier on the claim line:
CARC 151: “Payment adjusted because the payer deems the information submitted does not support this
many/frequency of services.”
MSN 23.17: “Medicare won’t cover these services because they are not considered medically necessary.”
Spanish Version: “Medicare no cubrirá estos servicios porque no son considerados necesarios por razones
médicas.”
Contractors shall use Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a
claim is received with a GA modifier indicating a signed ABN is on file.
Contractors shall use Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a
claim is received with a GZ modifier indicating no signed ABN is on file.
140.4.2.5 – Edits for PR Services Exceeding 72 Sessions
(Rev. 12497; Issued: 02-08-24; Effective: 01-01-24; Implementation: 03-12-24)
Effective for claims with dates of service on and after January 1, 2010, through December 31, 2021, CWF shall
reject PR claims that exceed 72 sessions. Medicare contractors shall deny PR claims that exceed 72 sessions
regardless of whether the -KX modifier is submitted on the claim line.
The following messages shall be used when Medicare contractors deny PR claims that exceed 72 sessions:
CARC 119: “Benefit maximum for this time period or occurrence has been reached.”

RARC N362: “The number of days or units of service exceeds our acceptable maximum.”
MSN 20.5: “These services cannot be paid because your benefits are exhausted at this time.”
Spanish Version: “Estos servicios no pueden ser pagados porque sus beneficios se han agotado.”
Contractors shall use Group Code PR assigning financial liability to the beneficiary, if a claim is received with a
GA modifier indicating a signed ABN is on file.
Contractors shall use Group Code CO assigning financial liability to the provider, if a claim is received with a
GZ modifier indicating no signed ABN is on file.
Effective for claims with dates of service on and after January 1, 2022, Medicare Contractors shall deny PR
claims that exceed 72 sessions only when the -KX modifier is not submitted on the claim line.
150 - Billing Requirements for Bariatric Surgery for Treatment of Morbid Obesity
(Rev. 931, Issued: 04-28-06, Effective: 02-21-06, Implementation: 05-30-06 Carrier/10-02-06 FI)
150.1 - General
(Rev. 2841, Issued: 12-23-13, Effective: 09-24-13, Implementation: 12-17-13)
Bariatric Surgery for Treatment of Co-Morbid Conditions Related to Morbid Obesity
Effective for services on or after February 21, 2006, Medicare has determined that the following bariatric
surgery procedures are reasonable and necessary under certain conditions for the treatment of morbid obesity.
The patient must have a body-mass index (BMI) ≥35, have at least one co-morbidity related to obesity, and
have been previously unsuccessful with medical treatment for obesity. This medical information must be
documented in the patient's medical record. In addition, the procedure must be performed at an approved
facility. A list of approved facilities may be found at http://www.cms.gov/Medicare/Medicare-General-
Information/MedicareApprovedFacilitie/Bariatric-Surgery.html
Effective for services performed on and after February 12, 2009, Medicare has determined that Type 2 diabetes
mellitus is a co-morbidity for purposes of processing bariatric surgery claims.
Effective for dates of service on and after September 24, 2013, the Centers for Medicare & Medicaid Services
(CMS) has removed the certified facility requirements for Bariatric Surgery for Treatment of Co-Morbid
Conditions Related to Morbid Obesity.
Please note the additional national coverage determinations related to bariatric surgery will be consolidated and
subsumed into Publication 100-03, Chapter 1, section 100.1. These include sections 40.5, 100.8, 100.11 and
100.14.
Open Roux-en-Y gastric bypass (RYGBP)
Laparoscopic Roux-en-Y gastric bypass (RYGBP)
Laparoscopic adjustable gastric banding (LAGB)
Open biliopancreatic diversion with duodenal switch (BPD/DS) or gastric reduction duodenal switch
(BPD/GRDS)
Laparoscopic biliopancreatic diversion with duodenal switch (BPD/DS) or gastric reduction duodenal switch
(BPD/GRDS)
Laparoscopic sleeve gastrectomy (LSG) (Effective June 27, 2012, covered at Medicare Administrative
Contractor (MAC) discretion.
150.2 - HCPCS Procedure Codes for Bariatric Surgery
(Rev. 2641, Issued: 01-29-13, Effective: 06-27-12, Implementation: 02-28-13)
A. Covered HCPCS Procedure Codes
For services on or after February 21, 2006, the following HCPCS procedure codes are covered for bariatric
surgery:
43770 - Laparoscopy, surgical, gastric restrictive procedure; placement of adjustable gastric band (gastric band
and subcutaneous port components).
43644 - Laparoscopy, surgical, gastric restrictive procedure; with gastric bypass and Roux-en-Y
gastroenterostomy (roux limb 150 cm or less).
43645 - Laparoscopy with gastric bypass and small intestine reconstruction to limit absorption. (Do not report
43645 in conjunction with 49320, 43847.)
43845 - Gastric restrictive procedure with partial gastrectomy, pylorus-preserving duodenoileostomy and
ileoieostomy (50 to 100 cm common channel) to limit absorption (biliopancreatic diversion with duodenal
switch).
43846 - Gastric restrictive procedure, with gastric bypass for morbid obesity; with short limb (150 cm or less
Roux-en-Y gastroenterostomy. (For greater than 150 cm, use 43847.) (For laparoscopic procedure, use 43644.)
43847 - With small intestine reconstruction to limit absorption.
43775- Laparoscopy, surgical, gastric restrictive procedure; longitudinal gastrectomy (i.e., sleeve gastrectomy)
(Effective June 27, 2012, covered at contractor’s discretion.)
B. Non-Covered HCPCS Procedure Codes
For services on or after February 21, 2006, the following HCPCS procedure codes are non-covered for bariatric
surgery:
43842 - Gastric restrictive procedure, without gastric bypass, for morbid obesity; vertical banded gastroplasty
NOC code 43999 used to bill for:
Laparoscopic vertical banded gastroplasty
Open sleeve gastrectomy
Laparoscopic sleeve gastrectomy (for contractor non-covered instances)
Open adjustable gastric banding

150.3 - ICD Procedure Codes for Bariatric Surgery for Treatment of Co-Morbid
Conditions Related to Morbid Obesity (A/MACs only)
(Rev. 12683 Issued: 06-13-24; Effective: 01-01-20; Implementation: 07-15-24)
Covered ICD Procedure Codes
For services on or after October 1, 2015, the following independent ICD-10 procedure codes are
covered for bariatric surgery:
0D16479
Bypass Stomach to Duodenum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1647A
Bypass Stomach to Jejunum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1647B
Bypass Stomach to Ileum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1647L
Bypass Stomach to Transverse Colon with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D164J9
Bypass Stomach to Duodenum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D164JA
Bypass Stomach to Jejunum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D164JB
Bypass Stomach to Ileum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D164JL
Bypass Stomach to Transverse Colon with Synthetic Substitute,
Percutaneous Endoscopic Approach
0D164K9
Bypass Stomach to Duodenum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D164KA
Bypass Stomach to Jejunum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D164KB
Bypass Stomach to Ileum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D164KL
Bypass Stomach to Transverse Colon with Non-autologous Tissue
Substitute, Percutaneous Endoscopic Approach
0D164Z9
Bypass Stomach to Duodenum, Percutaneous Endoscopic Approach
0D164ZA
Bypass Stomach to Jejunum, Percutaneous Endoscopic Approach
0D164ZB
Bypass Stomach to Ileum, Percutaneous Endoscopic Approach
0D164ZL
Bypass Stomach to Transverse Colon, Percutaneous Endoscopic
Approach
0D16079
Bypass Stomach to Duodenum with Autologous Tissue Substitute, Open
Approach
0D1607A
Bypass Stomach to Jejunum with Autologous Tissue Substitute, Open
Approach
0D1607B
Bypass Stomach to Ileum with Autologous Tissue Substitute, Open
Approach
0D1607L
Bypass Stomach to Transverse Colon with Autologous Tissue Substitute,
Open Approach
0D160J9
Bypass Stomach to Duodenum with Synthetic Substitute, Open Approach
0D160JA
Bypass Stomach to Jejunum with Synthetic Substitute, Open Approach
0D160JB
Bypass Stomach to Ileum with Synthetic Substitute, Open Approach
0D160JL
Bypass Stomach to Transverse Colon with Synthetic Substitute, Open
Approach
0D160K9
Bypass Stomach to Duodenum with Non-autologous Tissue Substitute,
Open Approach
0D160KA
Bypass Stomach to Jejunum with Non-autologous Tissue Substitute,
Open Approach
0D160KB
Bypass Stomach to Ileum with Non-autologous Tissue Substitute, Open
Approach
0D160KL
Bypass Stomach to Transverse Colon with Non-autologous Tissue
Substitute, Open Approach
0D160Z9
Bypass Stomach to Duodenum, Open Approach
0D160ZA
Bypass Stomach to Jejunum, Open Approach
0D160ZB
Bypass Stomach to Ileum, Open Approach
0D160ZL
Bypass Stomach to Transverse Colon, Open Approach
0D16879
Bypass Stomach to Duodenum with Autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1687A
Bypass Stomach to Jejunum with Autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1687B
Bypass Stomach to Ileum with Autologous Tissue Substitute, Via Natural
or Artificial Opening Endoscopic
0D1687L
Bypass Stomach to Transverse Colon with Autologous Tissue Substitute,
Via Natural or Artificial Opening Endoscopic
0D168J9
Bypass Stomach to Duodenum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D168JA
Bypass Stomach to Jejunum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D168JB
Bypass Stomach to Ileum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D168JL
Bypass Stomach to Transverse Colon with Synthetic Substitute, Via
Natural or Artificial Opening Endoscopic
0D168K9
Bypass Stomach to Duodenum with Non-autologous Tissue Substitute,
Via Natural or Artificial Opening Endoscopic
0D168KA
Bypass Stomach to Jejunum with Non-autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D168KB
Bypass Stomach to Ileum with Non-autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D168KL
Bypass Stomach to Transverse Colon with Non-autologous Tissue
Substitute, Via Natural or Artificial Opening Endoscopic
0D168Z9
Bypass Stomach to Duodenum, Via Natural or Artificial Opening
Endoscopic
0D168ZA
Bypass Stomach to Jejunum, Via Natural or Artificial Opening
Endoscopic
0D168ZB
Bypass Stomach to Ileum, Via Natural or Artificial Opening Endoscopic
0D168ZL
0DV64CZ
Bypass Stomach to Transverse Colon, Via Natural or Artificial Opening
Endoscopic
Restriction of Stomach with Extraluminal Device, Percutaneous
Endoscopic Approach
To describe either laparoscopic or open BPD with DS or GRDS, one code from each of the following three
groups must be on the claim:
Group 1:
0DB60Z3 Excision of Stomach, Open Approach, Vertical
0DB60ZZ Excision of Stomach, Open Approach
0DB63Z3 Excision of Stomach, Percutaneous Approach, Vertical
0DB63ZZ Excision of Stomach, Percutaneous Approach
0DB67Z3 Excision of Stomach, Via Natural or Artificial Opening, Vertical
0DB67ZZ Excision of Stomach, Via Natural or Artificial Opening
0DB68Z3 Excision of Stomach, Via Natural or Artificial Opening Endoscopic, Vertical
Group 2:
(Note: One code from A-C below is required for a correct equivalent)
0DB80ZZ Excision of Small Intestine, Open Approach – A
0DB84ZZ Excision of Small Intestine, Perc Endo Approach – A (Effective 01-01-20)
0DB90ZZ Excision of Duodenum, Open Approach – A
0DB93ZZ Excision of Duodenum, Percutaneous Approach – A (Effective 01-01-20)
0DBB0ZZ Excision of Ileum, Open Approach – A
0DBB3ZZ Excision of Ileum, Percutaneous Approach – A (Effective 01-01-20)
0D160ZB Bypass Stomach to Ileum, Open Approach – B
0D164ZB Bypass Stomach to Ileum, Percutaneous Endoscopic Approach – B (Effective
01-01-20)
0F190Z3 Bypass Common Bile Duct to Duodenum, Open Approach – C
0F194Z3 Bypass Common Bile Duct to Duodenum, Perc Endo Approach – C (Effective
01-01-20)
Group 3:
0D19079
Bypass Duodenum to Duodenum with Autologous Tissue Substitute,
Open Approach
0D1907A
Bypass Duodenum to Jejunum with Autologous Tissue Substitute, Open
Approach
0D1907B
Bypass Duodenum to Ileum with Autologous Tissue Substitute, Open
Approach
0D190J9
Bypass Duodenum to Duodenum with Synthetic Substitute, Open
Approach
0D190JA
Bypass Duodenum to Jejunum with Synthetic Substitute, Open Approach
0D190JB
Bypass Duodenum to Ileum with Synthetic Substitute, Open Approach
0D190K9
Bypass Duodenum to Duodenum with Non-autologous Tissue Substitute,
Open Approach
0D190KA
Bypass Duodenum to Jejunum with Non-autologous Tissue Substitute,
Open Approach
0D190KB
Bypass Duodenum to Ileum with Non-autologous Tissue Substitute, Open
Approach
0D190Z9
Bypass Duodenum to Duodenum, Open Approach
0D190ZA
Bypass Duodenum to Jejunum, Open Approach
0D190ZB
Bypass Duodenum to Ileum, Open Approach
0D19479
Bypass Duodenum to Duodenum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1947A
Bypass Duodenum to Jejunum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1947B
Bypass Duodenum to Ileum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D194J9
Bypass Duodenum to Duodenum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D194JA
Bypass Duodenum to Jejunum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D194JB
Bypass Duodenum to Ileum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D194K9
Bypass Duodenum to Duodenum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D194KA
Bypass Duodenum to Jejunum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D194KB
Bypass Duodenum to Ileum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D194Z9
Bypass Duodenum to Duodenum, Percutaneous Endoscopic Approach
0D194ZA
Bypass Duodenum to Jejunum, Percutaneous Endoscopic Approach
0D194ZB
Bypass Duodenum to Ileum, Percutaneous Endoscopic Approach
0D19879
Bypass Duodenum to Duodenum with Autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1987A
Bypass Duodenum to Jejunum with Autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1987B
Bypass Duodenum to Ileum with Autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D198J9
Bypass Duodenum to Duodenum with Synthetic Substitute, Via Natural
or Artificial Opening Endoscopic
0D198JA
Bypass Duodenum to Jejunum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D198JB
Bypass Duodenum to Ileum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D198K9
Bypass Duodenum to Duodenum with Non-autologous Tissue Substitute,
Via Natural or Artificial Opening Endoscopic
0D198KA
Bypass Duodenum to Jejunum with Non-autologous Tissue Substitute,
Via Natural or Artificial Opening Endoscopic
0D198KB
Bypass Duodenum to Ileum with Non-autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D198Z9
Bypass Duodenum to Duodenum, Via Natural or Artificial Opening
Endoscopic
0D198ZA
Bypass Duodenum to Jejunum, Via Natural or Artificial Opening
Endoscopic
0D198ZB
Bypass Duodenum to Ileum, Via Natural or Artificial Opening
Endoscopic
0D1A07A
Bypass Jejunum to Jejunum with Autologous Tissue Substitute, Open
Approach
0D1A07B
Bypass Jejunum to Ileum with Autologous Tissue Substitute, Open
Approach
0D1A0JA
Bypass Jejunum to Jejunum with Synthetic Substitute, Open Approach
0D1A0JB
Bypass Jejunum to Ileum with Synthetic Substitute, Open Approach
0D1A0KA
Bypass Jejunum to Jejunum with Non-autologous Tissue Substitute, Open
Approach
0D1A0KB
Bypass Jejunum to Ileum with Non-autologous Tissue Substitute, Open
Approach
0D1A0ZA
Bypass Jejunum to Jejunum, Open Approach
0D1A0ZB
Bypass Jejunum to Ileum, Open Approach
0D1A47A
Bypass Jejunum to Jejunum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1A47B
Bypass Jejunum to Ileum with Autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1A4JA
Bypass Jejunum to Jejunum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D1A4JB
Bypass Jejunum to Ileum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D1A4KA
Bypass Jejunum to Jejunum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1A4KB
Bypass Jejunum to Ileum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1A4ZA
Bypass Jejunum to Jejunum, Percutaneous Endoscopic Approach
0D1A4ZB
Bypass Jejunum to Ileum, Percutaneous Endoscopic Approach
0D1A87A
Bypass Jejunum to Jejunum with Autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1A87B
Bypass Jejunum to Ileum with Autologous Tissue Substitute, Via Natural
or Artificial Opening Endoscopic
0D1A8JA
Bypass Jejunum to Jejunum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D1A8JB
Bypass Jejunum to Ileum with Synthetic Substitute, Via Natural or
Artificial Opening Endoscopic
0D1A8KA
Bypass Jejunum to Jejunum with Non-autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1A8KB
Bypass Jejunum to Ileum with Non-autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1A8ZA
Bypass Jejunum to Jejunum, Via Natural or Artificial Opening
Endoscopic
0D1A8ZB
Bypass Jejunum to Ileum, Via Natural or Artificial Opening Endoscopic
0D1A8ZH
Bypass Jejunum to Cecum, Via Natural or Artificial Opening Endoscopic
0D1B07B
Bypass Ileum to Ileum with Autologous Tissue Substitute, Open
Approach
0D1B0JB
Bypass Ileum to Ileum with Synthetic Substitute, Open Approach
0D1B0KB
Bypass Ileum to Ileum with Non-autologous Tissue Substitute, Open
Approach
0D1B0ZB
Bypass Ileum to Ileum, Open Approach
0D1B47B
Bypass Ileum to Ileum with Autologous Tissue Substitute, Percutaneous
Endoscopic Approach
0D1B4JB
Bypass Ileum to Ileum with Synthetic Substitute, Percutaneous
Endoscopic Approach
0D1B4KB
Bypass Ileum to Ileum with Non-autologous Tissue Substitute,
Percutaneous Endoscopic Approach
0D1B4ZB
Bypass Ileum to Ileum, Percutaneous Endoscopic Approach
0D1B87B
Bypass Ileum to Ileum with Autologous Tissue Substitute, Via Natural or
Artificial Opening Endoscopic
0D1B8JB
Bypass Ileum to Ileum with Synthetic Substitute, Via Natural or Artificial
Opening Endoscopic

0D1B8KB
Bypass Ileum to Ileum with Non-autologous Tissue Substitute, Via
Natural or Artificial Opening Endoscopic
0D1B8ZB
Bypass Ileum to Ileum, Via Natural or Artificial Opening Endoscopic
0D1B8ZH
Bypass Ileum to Cecum, Via Natural or Artificial Opening Endoscopic
NOTE: There is no distinction between open and laparoscopic BPD with DS or GRDS for the inpatient
setting. For either approach, one code from each of the above three groups must appear on the claim to be
covered.
Effective October 1, 2015, the following ICD-10 procedure code is covered for bariatric surgery at
contractor discretion:
0DB64Z3 Excision of stomach, percutaneous endoscopic approach, vertical.
150.4 - ICD Diagnosis Codes for Bariatric Surgery
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
For services on or after October 1, 2015, the following ICD-10 diagnosis code is covered for bariatric
surgery if certain other conditions are met:
E66.01 - Morbid (severe) obesity due to excess calories
Effective for services performed on and after February 12, 2009, type 2 diabetes mellitus (T2DM) is
considered a comorbid condition related to morbid obesity for covered bariatric surgery procedures in
Medicare beneficiaries with a BMI ≥35. When T2DM is the comorbid condition related to morbid obesity,
the claim must include a covered ICD procedure code, ICD diagnosis code E66.01 as a primary diagnosis,
a covered ICD diagnosis code indicating T2DM as a secondary diagnosis, and an ICD diagnosis code
indicating a BMI ≥ 35 as a secondary diagnosis.
150.5 - ICD Diagnosis Codes for BMI ≥35
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
The following ICD-10 diagnosis codes identify BMI ≥35:
Z68.35 - Body Mass Index 35.0-35.9, adult
Z68.36 - Body Mass Index 36.0-36.9, adult
Z68.37 - Body Mass Index 37.0-37.9, adult
Z68.38 - Body Mass Index 38.0-38.9, adult
Z68.39 - Body Mass Index 39.0-39.9, adult
Z68.41 - Body Mass Index 40.0-44.9, adult
Z68.42 - Body Mass Index 45.0-49.9, adult
Z68.43 - Body Mass Index 50.0-59.9, adult
Z68.44 - Body Mass Index 60.0-69.9, adult
Z68.45 - Body Mass Index 70.0 and over, adult
150.5.1 – ICD Codes for Type II Diabetes Mellitus Complication
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)

E11.9
Type 2 diabetes mellitus without complications
E13.9
Other specified diabetes mellitus without complications
E11.65
Type 2 diabetes mellitus with hyperglycemia
E13.10
Other specified diabetes mellitus with ketoacidosis without coma
E11.69
Type 2 diabetes mellitus with other specified complication
Note: E11.69 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this policy.
E11.00
Type 2 diabetes mellitus with hyperosmolarity without nonketotic
hyperglycemic-hyperosmolar coma (NKHHC)
E11.01
Type 2 diabetes mellitus with hyperosmolarity with coma
E13.00
Other specified diabetes mellitus with hyperosmolarity without nonketotic
hyperglycemic-hyperosmolar coma (NKHHC)
E13.01
Other specified diabetes mellitus with hyperosmolarity with coma
Note: E11.00 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this policy.
E11.641
Type 2 diabetes mellitus with hypoglycemia with coma
E13.11
Other specified diabetes mellitus with ketoacidosis with coma
E13.641
Other specified diabetes mellitus with hypoglycemia with coma
Note: E11.01 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy.
E11.21
Type 2 diabetes mellitus with diabetic nephropathy
E11.22
Type 2 diabetes mellitus with diabetic chronic kidney disease
E11.29
Type 2 diabetes mellitus with other diabetic kidney complication
E13.21
Other specified diabetes mellitus with diabetic nephropathy
E13.22
Other specified diabetes mellitus with diabetic chronic kidney disease
E13.29
Other specified diabetes mellitus with other diabetic kidney complication
Note: E11.21 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy.
E11.3211
Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with
macular edema, right eye
E11.3212
Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with
macular edema, left eye
E11.3213
Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with
macular edema, bilateral
E11.3591
Type 2 diabetes mellitus with proliferative diabetic retinopathy without
macular edema, right eye
E11.3592
Type 2 diabetes mellitus with proliferative diabetic retinopathy without
macular edema, left eye
E11.3593
Type 2 diabetes mellitus with proliferative diabetic retinopathy without
macular edema, bilateral
E11.37X1
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, right eye
E11.37X2
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, left eye
E11.37X3
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, bilateral
E11.3291
Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy
without macular edema, right eye

E11.3292
Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy
without macular edema, left eye
E11.3293
Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy
without macular edema, bilateral
E11.3311
Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
with macular edema, right eye
E11.3312
Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
with macular edema, left eye
E11.3313
Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
with macular edema, bilateral
E11.3391
Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
without macular edema, right eye
E11.3392
Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
without macular edema, left eye
E11.3393
Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
without macular edema, bilateral
E11.3411
Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
with macular edema, right eye
E11.3412
Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
with macular edema, left eye
E11.3413
Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
with macular edema, bilateral
E11.3491
Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
without macular edema, right eye
E11.3492
Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
without macular edema, left eye
E11.3493
Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
without macular edema, bilateral
E11.3511
Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular
edema, right eye
E11.3512
Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular
edema, left eye
E11.3513
Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular
edema, bilateral
E11.3521
Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction
retinal detachment involving the macula, right eye
E11.3522
Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction
retinal detachment involving the macula, left eye
E11.3523
Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction
retinal detachment involving the macula, bilateral
E11.3531
Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction
retinal detachment not involving the macula, right eye
E11.3532
Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction
retinal detachment not involving the macula, left eye
E11.3533
Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction
retinal detachment not involving the macula, bilateral
E11.3591
Type 2 diabetes mellitus with proliferative diabetic retinopathy without
macular edema, right eye
E11.3592
Type 2 diabetes mellitus with proliferative diabetic retinopathy without
macular edema, left eye

E11.3593
Type 2 diabetes mellitus with proliferative diabetic retinopathy without
macular edema, bilateral
E11.37X1
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, right eye
E11.37X2
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, left eye
E11.37X3
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, bilateral
E13.311
Other specified diabetes mellitus with unspecified diabetic retinopathy with
macular edema
E13.319
Other specified diabetes mellitus with unspecified diabetic retinopathy
without macular edema
E13.3211
Other specified diabetes mellitus with mild nonproliferative diabetic
retinopathy with macular edema, right eye
E13.3212
Other specified diabetes mellitus with mild nonproliferative diabetic
retinopathy with macular edema, left eye
E13.3213
Other specified diabetes mellitus with mild nonproliferative diabetic
retinopathy with macular edema, bilateral
E13.3291
Other specified diabetes mellitus with mild nonproliferative diabetic
retinopathy without macular edema, right eye
E13.3292
Other specified diabetes mellitus with mild nonproliferative diabetic
retinopathy without macular edema, left eye
E13.3293
Other specified diabetes mellitus with mild nonproliferative diabetic
retinopathy without macular edema, bilateral
E13.3311
Other specified diabetes mellitus with moderate nonproliferative diabetic
retinopathy with macular edema, right eye
E13.3312
Other specified diabetes mellitus with moderate nonproliferative diabetic
retinopathy with macular edema, left eye
E13.3313
Other specified diabetes mellitus with moderate nonproliferative diabetic
retinopathy with macular edema, bilateral
E13.3391
Other specified diabetes mellitus with moderate nonproliferative diabetic
retinopathy without macular edema, right eye
E13.3392
Other specified diabetes mellitus with moderate nonproliferative diabetic
retinopathy without macular edema, left eye
E13.3393
Other specified diabetes mellitus with moderate nonproliferative diabetic
retinopathy without macular edema, bilateral
E13.3411
Other specified diabetes mellitus with severe nonproliferative diabetic
retinopathy with macular edema, right eye
E13.3412
Other specified diabetes mellitus with severe nonproliferative diabetic
retinopathy with macular edema, left eye
E13.3413
Other specified diabetes mellitus with severe nonproliferative diabetic
retinopathy with macular edema, bilateral
E13.3491
Other specified diabetes mellitus with severe nonproliferative diabetic
retinopathy without macular edema, right eye
E13.3492
Other specified diabetes mellitus with severe nonproliferative diabetic
retinopathy without macular edema, left eye
E13.3493
Other specified diabetes mellitus with severe nonproliferative diabetic
retinopathy without macular edema, bilateral
E13.3511
Other specified diabetes mellitus with proliferative diabetic retinopathy with
macular edema, right eye

E13.3512
Other specified diabetes mellitus with proliferative diabetic retinopathy with
macular edema, left eye
E13.3513
Other specified diabetes mellitus with proliferative diabetic retinopathy with
macular edema, bilateral
E13.3521
Other specified diabetes mellitus with proliferative diabetic retinopathy with
traction retinal detachment involving the macula, right eye
E13.3522
Other specified diabetes mellitus with proliferative diabetic retinopathy with
traction retinal detachment involving the macula, left eye
E13.3523
Other specified diabetes mellitus with proliferative diabetic retinopathy with
traction retinal detachment involving the macula, bilateral
E13.3531
Other specified diabetes mellitus with proliferative diabetic retinopathy with
traction retinal detachment not involving the macula, right eye
E13.3532
Other specified diabetes mellitus with proliferative diabetic retinopathy with
traction retinal detachment not involving the macula, left eye
E13.3533
Other specified diabetes mellitus with proliferative diabetic retinopathy with
traction retinal detachment not involving the macula, bilateral
E13.3541
Other specified diabetes mellitus with proliferative diabetic retinopathy with
combined traction retinal detachment and rhegmatogenous retinal
detachment, right eye
E13.3542
Other specified diabetes mellitus with proliferative diabetic retinopathy with
combined traction retinal detachment and rhegmatogenous retinal
detachment, left eye
E13.3543
Other specified diabetes mellitus with proliferative diabetic retinopathy with
combined traction retinal detachment and rhegmatogenous retinal
detachment, bilateral
E13.3551
Other specified diabetes mellitus with stable proliferative diabetic
retinopathy, right eye
E13.3552
Other specified diabetes mellitus with stable proliferative diabetic
retinopathy, left eye
E13.3553
Other specified diabetes mellitus with stable proliferative diabetic
retinopathy, bilateral
E13.3591
Other specified diabetes mellitus with proliferative diabetic retinopathy
without macular edema, right eye
E13.3592
Other specified diabetes mellitus with proliferative diabetic retinopathy
without macular edema, left eye
E13.3593
Other specified diabetes mellitus with proliferative diabetic retinopathy
without macular edema, bilateral
E13.36
Other specified diabetes mellitus with diabetic cataract
E13.39
Other specified diabetes mellitus with other diabetic ophthalmic complication
E11.311
Type 2 diabetes mellitus with unspecified diabetic retinopathy with macular
edema OR
E11.319
Type 2 diabetes mellitus with unspecified diabetic retinopathy without
macular edema OR
E11.36
Type 2 diabetes mellitus with diabetic cataract OR
E11.39
Type 2 diabetes mellitus with other diabetic ophthalmic complication AND
Note: E11.39 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy
E13.37X1
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, right eye

E13.37X2
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, left eye
E13.37X3
Type 2 diabetes mellitus with diabetic macular edema, resolved following
treatment, bilateral
E11.40
Type 2 diabetes mellitus with diabetic neuropathy, unspecified
E11.41
Type 2 diabetes mellitus with diabetic mononeuropathy
E11.42
Type 2 diabetes mellitus with diabetic polyneuropathy
E11.43
Type 2 diabetes mellitus with diabetic autonomic (poly)neuropathy
E11.44
Type 2 diabetes mellitus with diabetic amyotrophy
E11.49
Type 2 diabetes mellitus with other diabetic neurological complication
E11.610
Type 2 diabetes mellitus with diabetic neuropathic arthropathy
E13.40
Other specified diabetes mellitus with diabetic neuropathy, unspecified
E13.41
Other specified diabetes mellitus with diabetic mononeuropathy
E13.42
Other specified diabetes mellitus with diabetic polyneuropathy
E13.43
Other specified diabetes mellitus with diabetic autonomic (poly)neuropathy
E13.44
Other specified diabetes mellitus with diabetic amyotrophy
E13.49
Other specified diabetes mellitus with other diabetic neurological
complication
E13.610
Other specified diabetes mellitus with diabetic neuropathic arthropathy
Note: E11.40 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy.
E11.51
Type 2 diabetes mellitus with diabetic peripheral angiopathy without
gangrene
E11.52
Type 2 diabetes mellitus with diabetic peripheral angiopathy with gangrene
E11.59
Type 2 diabetes mellitus with other circulatory complications
E13.51
Other specified diabetes mellitus with diabetic peripheral angiopathy without
gangrene
E13.52
Other specified diabetes mellitus with diabetic peripheral angiopathy with
gangrene
E13.59
Other specified diabetes mellitus with other circulatory complications
Note: E11.51 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy.
E11.618
Type 2 diabetes mellitus with other diabetic arthropathy
E11.620
Type 2 diabetes mellitus with diabetic dermatitis
E11.621
Type 2 diabetes mellitus with foot ulcer
E11.622
Type 2 diabetes mellitus with other skin ulcer
E11.628
Type 2 diabetes mellitus with other skin complications
E11.630
Type 2 diabetes mellitus with periodontal disease
E11.638
Type 2 diabetes mellitus with other oral complications
E11.649
Type 2 diabetes mellitus with hypoglycemia without coma
E13.618
Other specified diabetes mellitus with other diabetic arthropathy
E13.620
Other specified diabetes mellitus with diabetic dermatitis
E13.621
Other specified diabetes mellitus with foot ulcer
E13.622
Other specified diabetes mellitus with other skin ulcer
E13.628
Other specified diabetes mellitus with other skin complications
E13.630
Other specified diabetes mellitus with periodontal disease
E13.638
Other specified diabetes mellitus with other oral complications

E13.649
Other specified diabetes mellitus with hypoglycemia without coma
E13.65
Other specified diabetes mellitus with hyperglycemia
E13.69
Other specified diabetes mellitus with other specified complication
Note: E11.69 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy.
E13.8
Other specified diabetes mellitus with unspecified complications
E11.8
Type 2 diabetes mellitus with unspecified complications
Note: E11.8 with E11.65 are a cluster BUT since each code on its own
justifies the service, the combination is not required together for this
policy.
150.6 - Claims Guidance for Payment
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Covered Bariatric Surgery Procedures for Treatment of Co-Morbid Conditions Related to
Morbid Obesity
Contractors shall process covered bariatric surgery claims as follows:
C.
Identify bariatric surgery claims.
Contractors identify inpatient bariatric surgery claims by the presence of ICD-10 diagnosis code E66.01as
the primary diagnosis (for morbid obesity) and one of the covered ICD-10 procedure codes listed in
§150.3.
Contractors identify practitioner bariatric surgery claims by the presence of ICD-10 diagnosis code E66.01
as the primary diagnosis (for morbid obesity) and one of the covered HCPCS procedure codes listed in
§150.2.
D.
Perform facility certification validation for all bariatric surgery claims on a pre-pay basis up to and
including date of service September 23, 2013.
A list of approved facilities are found at the link noted in section 150.1, section A, above.
E.
Review bariatric surgery claims data and determine whether a pre- or post-pay sample of bariatric
surgery claims need further review to assure that the beneficiary has a BMI ≥35 (Z68.35-Z68.45) (see ICD-
10 equivalents above in section 150.5), and at least one co-morbidity related to obesity.
The A/B MAC medical director may define the appropriate method for addressing the obesity-related
co-morbid requirement.
Effective for dates of service on and after September 24, 2013, CMS has removed the certified facility
requirements for Bariatric Surgery for Treatment of Co-Morbid Conditions Related to Morbid Obesity.
NOTE: If ICD-10 diagnosis code E66.01 is present, but a covered procedure code (listed in §150.2 or §150.3)
is/are not present, the claim is not for bariatric surgery and should be processed under normal procedures.
NOTE: If ICD-10 diagnosis code E66.01 is present, but a covered procedure code (listed in §150.2 or
§150.3) is/are not present, the claim is not for bariatric surgery and should be processed under normal
procedures.
150.7 - Medicare Summary Notices (MSNs) and Claim Adjustment Reason Codes
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
When rejecting/denying claims because bariatric surgery procedures were performed in an unapproved
facility use:
• MSN 16.2 - "This service cannot be paid when provided in this location/facility."
• Claim Adjustment Reason Code 58 - "Payment adjusted because treatment was deemed by the
payer to have been rendered in an inappropriate or invalid place of service."
• Remittance Advice Remark Code N386 - “This decision was based on a National Coverage
Determination (NCD). An NCD provides a coverage determination as to whether a particular item or
service is covered. A copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not
have web access, you may contact the contractor to request a copy of the NCD.”
When rejecting/denying claims for non-covered bariatric surgery procedures use:
• MSN16.10 - Medicare does not pay for this item or service.
• Claim Adjustment Reason Code 50 - "These are non-covered services because this is not deemed a
“medical necessity” by the payer."
• Remittance Advice Remark Code N386 - “This decision was based on a National
Coverage Determination (NCD). An NCD provides a coverage determination as to whether a
particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to
request a copy of the NCD.”
•
When rejecting/denying claims for covered bariatric surgery procedures because the patient did not meet the
conditions for coverage use:
• MSN 15.4 - “The information provided does not support the need for this service or item.”
• Claim Adjustment Reason Code 167 - "This (these) diagnosis(es) is (are) not covered”
• Remittance Advice Remark Code N386 - “This decision was based on a National
Coverage Determination (NCD). An NCD provides a coverage determination as to whether a
particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to
request a copy of the NCD.”
• Group Code CO – Contractual Obligation
In addition to the codes listed above, afford appeal rights to all denied parties.
150.8 - A/MAC Billing Requirements
(Rev. 2841, Issued: 12-23-13, Effective: 09-24-13, Implementation: 12-17-13)
The A/MAC billing requirements will pay for bariatric surgery only when the services are submitted on the
following type of bill (TOB): 11X. Type of facility and setting determines the basis of payment:
• For services performed in Indian Health Services inpatient hospitals, TOB 11X under the inpatient
prospective payment system (IPPS) is based on the diagnosis-related group (DRG).
• For services performed in inpatient hospitals, TOB 11X under IPPS is based on the DRG.
• For services performed in IHS critical access hospitals (CAHs), TOB 11X, payment is based on 101%
facility specific per diem rate.
• For services performed in CAH inpatient hospitals, TOB 11X, payment is based on 101% of reasonable
cost.
150.9 - Advance Beneficiary Notice and HINN Information
(Rev. 1233, Issued: 04-27-07, Effective: 02-21-06, Implementation: 05-29-07)
Physicians must be advised that the physician is liable for charges if the surgery is performed in an
unapproved facility, unless the beneficiary was informed that he or she would be financially responsible prior
to performance for the procedure. The provider must have the beneficiary sign an advance beneficiary notice
(ABN) if the bariatric surgery is performed in an unapproved facility. Note that the ABN is the appropriate
notice for Part B services.
The HINN model language should be adapted to this situation in the sections addressing: description of the
care at issue if the surgery is performed on an inpatient basis, in an unapproved facility, to avoid being liable,
the provider must issue a HINN. Other content requirements of HINN still apply. Use the HINN letter most
appropriate to the overall situation.
160 – PTA for Implanting the Carotid Stent
(Rev. 1042, Issued: 08-25-06; Effective: 03-17-05; Implementation: 10-02-06)
160.1 – Category B Investigational Device Exemption (IDE) Study Coverage
(Rev. 12571; Issued: 04-11-24) Effective: 10-11-23; Implementation: 05-13-24)
Effective July 1, 2001, Medicare covers percutaneous transluminal angioplasty (PTA) of the carotid artery
concurrent with stent placement when furnished in accordance with the Food and Drug Administration (FDA)
protocols governing Category B Investigational Device Exemption (IDE) studies.
The billing for this procedure is based upon how the service is delivered. There are several CPT codes that
may be billed depending upon how the procedure is performed. Contractor medical directors should consider
what provider education information is needed to assist providers on the billing for this service.
Contractors must review their local coverage determinations to ensure that payment is provided for claims for
PTA in an FDA-approved clinical study.
As a requirement for Category B IDE coverage, providers must bill a six-digit IDE Number that begins with a
“G” (i.e., G123456). To identify the line as an IDE line, institutional providers must bill this IDE Number on a
0624 Revenue Code line while practitioners must bill this IDE Number along with a Q0 modifier.
160.2 – Post-Approval Study Coverage
(Rev. 12571; Issued: 04-11-24) Effective: 10-11-23; Implementation: 05-13-24)
Effective October 12, 2004, under section B3 of NCD 20.7, Medicare covers PTA of the carotid artery
concurrent with the placement of an FDA-approved carotid stent and an FDA-approved or –cleared
embolic protection device (effective December 9, 2009) for an FDA-approved indication when furnished
in accordance with FDA-approved protocols governing post-approval studies. Also included in the
currently covered population of patients participating in FDA-approved post-approval studies are patients
participating in post-approval extension studies and patients participating in studies following FDA 510k
approval of these devices.
Billing post-approval studies is similar to normal Category B IDE billing procedures, except that under post-
approval coverage, providers must bill the Pre-Market Approval (PMA) number assigned to the stent system
by the FDA. PMA numbers are like typical IDE Numbers in that they have six-digits, but they begin with a
“P” (i.e., P123456) instead of a “G.”
160.2.1 – Carotid Artery Stenting (CAS) for Post-Approval Studies
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
A. Background
As the post-approval studies began to end, CMS received requests to extend coverage for the post-
approval studies. CMS has reviewed the extension requests and has determined that patients participating
in post-approval extension studies are also included in the currently covered population of patients
participating in FDA-approved post-approval studies.
B. Policy
To grant approval for post-approval studies, the FDA reviews each study protocol. Once approval is
granted, the FDA issues a formal approval letter to the study sponsor.
Extensions of post-approval studies are not subject to approval by the FDA because they surpass the post-
approval study requirements identified in the conditions of approval for post-approval studies. Since the
FDA cannot approve these extension studies, individual Post-Market Approval (PMA) numbers cannot be
issued to separately identify each study. Currently, in order to receive reimbursement for procedures
performed as part of a carotid artery stenting post-approval study, providers must include the FDA-issued
PMA number on each claim to indicate participation in a specific study.
CMS has determined that all extension studies must be reviewed by the FDA. The FDA will issue an
acknowledgement letter stating that the extension study is scientifically valid and will generate clinically
relevant post-market data. Upon receipt of this letter and review of the extension study protocol, CMS will
issue a letter to the study sponsor indicating that the study under review will be covered by Medicare. Since
an individual PMA number cannot be assigned by the FDA to each extension study, these studies will use
the PMA number assigned to the original FDA-approved post-approval study (i.e., CAPTURE 2 shall use
the PMA number assigned to CAPTURE 1).
C. Billing

In order to receive Medicare coverage for patients participating in post-approval extension studies,
providers shall submit both the FDA acknowledgement letter and the CMS letter providing coverage for
the extension study to their contractor. Additionally, providers shall submit any other materials contractors
would require for FDA-approved post- approval studies.
In response, contractors will issue a letter assigning an effective date for each facility’s participation in the
extension study. Providers may bill for procedures performed in the extension study for dates of service on
and after the assigned effective date. Providers billing A/B MACs (A) must bill using the most current
ICD-10-CM is applicable, Indications for PTA of the Carotid Artery Concurrent with Stenting (must bill
one of these primary codes to meet coverage under 20.7B2, 20.7B3, 20.7B4)
I63.031
Cerebral infarction due to thrombosis of right carotid artery
I63.032
Cerebral infarction due to thrombosis of left carotid artery
I63.033
Cerebral infarction due to thrombosis of bilateral carotid arteries
I63.131
Cerebral infarction due to embolism of right carotid artery
I63.132
Cerebral infarction due to embolism of left carotid artery
I63.133
Cerebral infarction due to embolism of bilateral carotid arteries
I63.231
Cerebral infarction due to unspecified occlusion or stenosis of
right carotid arteries
I63.232
Cerebral infarction due to unspecified occlusion or stenosis of
left carotid arteries
I63.233
Cerebral infarction due to unspecified occlusion or stenosis of
bilateral carotid arteries
I65.21
Occlusion and stenosis of right carotid artery
I65.22
Occlusion and stenosis of left carotid artery
I65.23
Occlusion and stenosis of bilateral carotid arteries
ICD-10-PCS codes may be used.
037G34Z
Dilation of Intracranial Artery with Drug-eluting Intraluminal Device, Percutaneous Approach
037G35Z
Dilation of Intracranial Artery with Two Drug-eluting Intraluminal Devices, Percutaneous Appro
037G36Z
Dilation of Intracranial Artery with Three Drug-eluting Intraluminal Devices, Percutaneous Appr
037G37Z
Dilation of Intracranial Artery with Four or More Drug-eluting Intraluminal Devices, Percutaneo
Approach
037G3DZ
Dilation of Intracranial Artery with Intraluminal Device, Percutaneous Approach
037G3EZ
Dilation of Intracranial Artery with Two Intraluminal Devices, Percutaneous Approach
037G3FZ
Dilation of Intracranial Artery with Three Intraluminal Devices, Percutaneous Approach
037G3GZ
Dilation of Intracranial Artery with Four or More Intraluminal Devices, Percutaneous Approach
037G44Z
Dilation of Intracranial Artery with Drug-eluting Intraluminal Device, Percutaneous Endoscopic
Approach
037G45Z
Dilation of Intracranial Artery with Two Drug-eluting Intraluminal Devices, Percutaneous Endos
Approach
037G46Z
Dilation of Intracranial Artery with Three Drug-eluting Intraluminal Devices, Percutaneous
Endoscopic Approach
037G47Z
Dilation of Intracranial Artery with Four or More Drug-eluting Intraluminal Devices, Percutaneo
Endoscopic Approach
037G4DZ
Dilation of Intracranial Artery with Intraluminal Device, Percutaneous Endoscopic Approach
037G4EZ
Dilation of Intracranial Artery with Two Intraluminal Devices, Percutaneous Endoscopic Approa
037G4FZ
Dilation of Intracranial Artery with Three Intraluminal Devices, Percutaneous Endoscopic Appro

037G4GZ
Dilation of Intracranial Artery with Four or More Intraluminal Devices, Percutaneous Endoscopic
Approach
037H34Z
Dilation of Right Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037H35Z
Dilation of Right Common Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutan
Approach
037H36Z
Dilation of Right Common Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037H37Z
Dilation of Right Common Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Approach
037H3DZ
Dilation of Right Common Carotid Artery with Intraluminal Device, Percutaneous Approach
037H3EZ
Dilation of Right Common Carotid Artery with Two Intraluminal Devices, Percutaneous Approa
037H3FZ
Dilation of Right Common Carotid Artery with Three Intraluminal Devices, Percutaneous Appro
037H3GZ
Dilation of Right Common Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Approach
037H44Z
Dilation of Right Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037H45Z
Dilation of Right Common Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutan
Endoscopic Approach
037H46Z
Dilation of Right Common Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037H47Z
Dilation of Right Common Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037H4DZ
Dilation of Right Common Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037H4EZ
Dilation of Right Common Carotid Artery with Two Intraluminal Devices, Percutaneous Endosc
Approach
037H4FZ
Dilation of Right Common Carotid Artery with Three Intraluminal Devices, Percutaneous Endos
Approach
037H4GZ
Dilation of Right Common Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Endoscopic Approach
037J34Z
Dilation of Left Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037J35Z
Dilation of Left Common Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutane
Approach
037J36Z
Dilation of Left Common Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutan
Approach
037J37Z
Dilation of Left Common Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Approach
037J3DZ
Dilation of Left Common Carotid Artery with Intraluminal Device, Percutaneous Approach
037J3EZ
Dilation of Left Common Carotid Artery with Two Intraluminal Devices, Percutaneous Approach
037J3FZ
Dilation of Left Common Carotid Artery with Three Intraluminal Devices, Percutaneous Approa
037J3GZ
Dilation of Left Common Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Approach
037J44Z
Dilation of Left Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037J45Z
Dilation of Left Common Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutane
Endoscopic Approach
037J46Z
Dilation of Left Common Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutan
Endoscopic Approach

037J47Z
Dilation of Left Common Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037J4DZ
Dilation of Left Common Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037J4EZ
Dilation of Left Common Carotid Artery with Two Intraluminal Devices, Percutaneous Endoscop
Approach
037J4FZ
Dilation of Left Common Carotid Artery with Three Intraluminal Devices, Percutaneous Endosco
Approach
037J4GZ
Dilation of Left Common Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Endoscopic Approach
037K34Z
Dilation of Right Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037K35Z
Dilation of Right Internal Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutane
Approach
037K36Z
Dilation of Right Internal Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutan
Approach
037K37Z
Dilation of Right Internal Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Approach
037K3DZ
Dilation of Right Internal Carotid Artery with Intraluminal Device, Percutaneous Approach
037K3EZ
Dilation of Right Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Approach
037K3FZ
Dilation of Right Internal Carotid Artery with Three Intraluminal Devices, Percutaneous Approac
037K3GZ
Dilation of Right Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Approach
037K44Z
Dilation of Right Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037K45Z
Dilation of Right Internal Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutane
Endoscopic Approach
037K46Z
Dilation of Right Internal Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutan
Endoscopic Approach
037K47Z
Dilation of Right Internal Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037K4DZ
Dilation of Right Internal Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037K4EZ
Dilation of Right Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Endoscop
Approach
037K4FZ
Dilation of Right Internal Carotid Artery with Three Intraluminal Devices, Percutaneous Endosco
Approach
037K4GZ
Dilation of Right Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Endoscopic Approach
037L34Z
Dilation of Left Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037L35Z
Dilation of Left Internal Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutaneo
Approach
037L36Z
Dilation of Left Internal Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutane
Approach
037L37Z
Dilation of Left Internal Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Approach
037L3DZ
Dilation of Left Internal Carotid Artery with Intraluminal Device, Percutaneous Approach
037L3EZ
Dilation of Left Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Approach
037L3FZ
Dilation of Left Internal Carotid Artery with Three Intraluminal Devices, Percutaneous Approach

037L3GZ
Dilation of Left Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Approach
037L44Z
Dilation of Left Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037L45Z
Dilation of Left Internal Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutaneo
Endoscopic Approach
037L46Z
Dilation of Left Internal Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutane
Endoscopic Approach
037L47Z
Dilation of Left Internal Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037L4DZ
Dilation of Left Internal Carotid Artery with Intraluminal Device, Percutaneous Endoscopic App
037L4EZ
Dilation of Left Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Endoscopi
Approach
037L4FZ
Dilation of Left Internal Carotid Artery with Three Intraluminal Devices, Percutaneous Endoscop
Approach
037L4GZ
Dilation of Left Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Endoscopic Approach
037M34Z
Dilation of Right External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037M35Z
Dilation of Right External Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutan
Approach
037M36Z
Dilation of Right External Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037M37Z
Dilation of Right External Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Approach
037M3DZ
Dilation of Right External Carotid Artery with Intraluminal Device, Percutaneous Approach
037M3EZ
Dilation of Right External Carotid Artery with Two Intraluminal Devices, Percutaneous Approac
037M3FZ
Dilation of Right External Carotid Artery with Three Intraluminal Devices, Percutaneous Approa
037M3GZ
Dilation of Right External Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Approach
037M44Z
Dilation of Right External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037M45Z
Dilation of Right External Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutan
Endoscopic Approach
037M46Z
Dilation of Right External Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037M47Z
Dilation of Right External Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037M4DZ
Dilation of Right External Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037M4EZ
Dilation of Right External Carotid Artery with Two Intraluminal Devices, Percutaneous Endosco
Approach
037M4FZ
Dilation of Right External Carotid Artery with Three Intraluminal Devices, Percutaneous Endosc
Approach
037M4GZ
Dilation of Right External Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Endoscopic Approach
037N34Z
Dilation of Left External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037N35Z
Dilation of Left External Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutaneo
Approach

037N36Z
Dilation of Left External Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutane
Approach
037N37Z
Dilation of Left External Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Approach
037N3DZ
Dilation of Left External Carotid Artery with Intraluminal Device, Percutaneous Approach
037N3EZ
Dilation of Left External Carotid Artery with Two Intraluminal Devices, Percutaneous Approach
037N3FZ
Dilation of Left External Carotid Artery with Three Intraluminal Devices, Percutaneous Approac
037N3GZ
Dilation of Left External Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Approach
037N44Z
Dilation of Left External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037N45Z
Dilation of Left External Carotid Artery with Two Drug-eluting Intraluminal Devices, Percutaneo
Endoscopic Approach
037N46Z
Dilation of Left External Carotid Artery with Three Drug-eluting Intraluminal Devices, Percutan
Endoscopic Approach
037N47Z
Dilation of Left External Carotid Artery with Four or More Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037N4DZ
Dilation of Left External Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037N4EZ
Dilation of Left External Carotid Artery with Two Intraluminal Devices, Percutaneous Endoscop
Approach
037N4FZ
Dilation of Left External Carotid Artery with Three Intraluminal Devices, Percutaneous Endosco
Approach
037N4GZ
Dilation of Left External Carotid Artery with Four or More Intraluminal Devices, Percutaneous
Endoscopic Approach
160.3 – Carotid Artery Stenting (CAS) With Embolic Protection Coverage
(Rev. 12571; Issued: 04-11-24) Effective: 10-11-23; Implementation: 05-13-24)
On October 11, 2023, CMS issued a reconsideration of NCD 20.7. The updated NCD covers PTA of the
carotid artery concurrent with stenting with the placement of an FDA-approved carotid stent with an FDA-
approved or cleared embolic protection device, for Medicare beneficiaries with symptomatic carotid artery
stenosis ≥50% and asymptomatic carotid artery stenosis ≥70%. The NCD also sets forth requirements
regarding neurological assessments, imaging, shared decision-making, and retains institutional and physician
standards but removes the requirement that facilities that perform CAS procedures must be approved by CMS.
Additionally, CMS revised section D of NCD 20.7 to allow MACs to make reasonable and necessary
determinations under section 1862(a)(1)(A) for any other beneficiary seeking coverage for PTA of the carotid
artery concurrent with stenting.
A. Billing
Effective for claims with dates of services on or after October 11, 2023, contractors shall cover PTA of the
carotid artery concurrent with stenting with the placement of an FDA-approved carotid stent with an FDA-
approved or cleared embolic protection device, for Medicare beneficiaries under the following conditions:
A. Patients with symptomatic carotid artery stenosis ≥50%; and,
B. Patients with asymptomatic carotid artery stenosis ≥70%.
Also effective for claims with dates of service on or after October 11, 2023, beneficiaries no longer have to be
enrolled in a clinical trial for this service. Contractors may also pay for claims for PTA of the carotid artery

concurrent with stenting not otherwise addressed in The National Coverage Determinations Manual, Chapter
1, part 1, section 20.7 at local discretion.
Effective March 17, 2005, through October 10, 2023, Medicare covered PTA of the carotid artery concurrent
with the placement of an FDA-approved carotid stent with embolic protection under specific patient
indications found in Pub. 100-03, Medicare National Coverage Determinations Manual, part 1, section 20.7.
Coverage was limited to procedures performed using FDA-approved CAS systems and FDA-approved or –
cleared (effective December 9, 2009) embolic protection devices (EPDs). If deployment of the EPD was not
technically possible, and not performed, then the procedure was not covered.
In addition to the specific patient indications, CMS determined that CAS with embolic protection was
reasonable and necessary only if performed in facilities that had been determined to be competent in
performing the evaluation, procedure, and follow-up necessary to ensure optimal patient outcomes. CMS
created a list of minimum standards modeled in part on professional society statements on competency. All
facilities were required to at least meet CMS’s standards in order to receive coverage for CAS for high-risk
patients. Facilities were required to recertify every 2 years in order to maintain coverage of CAS procedures.
161 - Intracranial Percutaneous Transluminal Angioplasty (PTA) With Stenting
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
A. Background
In the past, PTA to treat obstructive lesions of the cerebral arteries was non-covered by Medicare because
the safety and efficacy of the procedure had not been established. This national coverage determination
(NCD) meant that the procedure was also non-covered for beneficiaries participating in Food and Drug
Administration (FDA)-approved investigational device exemption (IDE) clinical trials.
B. Policy
On February 9, 2006, a request for reconsideration of this NCD initiated a national coverage analysis. CMS
reviewed the evidence and determined that intracranial PTA with stenting is reasonable and necessary
under §1862(a)(1)(A) of the Social Security Act for the treatment of cerebral vessels (as specified in The
National Coverage Determinations Manual, Chapter 1, part 1, section 20.7) only when furnished in
accordance with FDA- approved protocols governing Category B IDE clinical trials. All other indications
for intracranial PTA with stenting remain non-covered.
•
Billing
Providers of covered intracranial PTA with stenting shall use Category B IDE billing requirements, as listed
above in section 68.4. In addition to these requirements, providers must bill the appropriate procedure and
diagnosis codes for the date of service to receive payment.
See the below ICD-10-CM diagnosis codes list applies, depending on the date of
service. Indications for PTA and Stenting of Intracranial Arteries (must bill I67.2 and one of these primary
codes to meet coverage under 20.7B5)
If ICD-10-CM is applicable:
I67.2 Cerebral atherosclerosis

I66.01 Occlusion and stenosis of right middle cerebral artery
I66.02 Occlusion and stenosis of left middle cerebral artery
I66.03 Occlusion and stenosis of bilateral middle cerebral arteries
I66.11 Occlusion and stenosis of right anterior cerebral artery
I66.12 Occlusion and stenosis of left anterior cerebral artery
I66.13 Occlusion and stenosis of bilateral anterior cerebral arteries
I66.21 Occlusion and stenosis of right posterior cerebral artery
I66.22 Occlusion and stenosis of left posterior cerebral artery
I66.23 Occlusion and stenosis of bilateral posterior cerebral arteries
I66.8 Occlusion and stenosis of other cerebral arteries
I63.59 Cerebral infarction due to unspecified occlusion or stenosis of other cerebral artery
If ICD-10-PCS is applicable, ICD-10-PCS procedure codes.
That is, under Part A, providers must bill intracranial PTA using if ICD-10-PCS procedure codes is
applicable.
037G34Z
Dilation of Intracranial Artery with Drug-eluting Intraluminal Device, Percutaneous Approach
037G35Z
Dilation of Intracranial Artery with Two Drug-eluting Intraluminal Devices, Percutaneous
Approach
037G36Z
Dilation of Intracranial Artery with Three Drug-eluting Intraluminal Devices, Percutaneous
Approach
037G37Z
Dilation of Intracranial Artery with Four or More Drug-eluting Intraluminal Devices, Percutan
Approach
037G3DZ
Dilation of Intracranial Artery with Intraluminal Device, Percutaneous Approach
037G3EZ
Dilation of Intracranial Artery with Two Intraluminal Devices, Percutaneous Approach
037G3FZ
Dilation of Intracranial Artery with Three Intraluminal Devices, Percutaneous Approach
037G3GZ
Dilation of Intracranial Artery with Four or More Intraluminal Devices, Percutaneous Approa
037G44Z
Dilation of Intracranial Artery with Drug-eluting Intraluminal Device, Percutaneous Endoscop
Approach
037G45Z
Dilation of Intracranial Artery with Two Drug-eluting Intraluminal Devices, Percutaneous
Endoscopic Approach
037G46Z
Dilation of Intracranial Artery with Three Drug-eluting Intraluminal Devices, Percutaneous
Endoscopic Approach
037G47Z
Dilation of Intracranial Artery with Four or More Drug-eluting Intraluminal Devices, Percutan
Endoscopic Approach
037G4DZ
Dilation of Intracranial Artery with Intraluminal Device, Percutaneous Endoscopic Approach
037G4EZ
Dilation of Intracranial Artery with Two Intraluminal Devices, Percutaneous Endoscopic
Approach
037G4FZ
Dilation of Intracranial Artery with Three Intraluminal Devices, Percutaneous Endoscopic
Approach
037G4GZ
Dilation of Intracranial Artery with Four or More Intraluminal Devices, Percutaneous Endosc
Approach
037H34Z
Dilation of Right Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneo
Approach
037H35Z
Dilation of Right Common Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Approach
037H36Z
Dilation of Right Common Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach

037H37Z
Dilation of Right Common Carotid Artery with Four or More Drug-eluting Intraluminal Devi
Percutaneous Approach
037H3DZ
Dilation of Right Common Carotid Artery with Intraluminal Device, Percutaneous Approach
037H3EZ
Dilation of Right Common Carotid Artery with Two Intraluminal Devices, Percutaneous
Approach
037H3FZ
Dilation of Right Common Carotid Artery with Three Intraluminal Devices, Percutaneous
Approach
037H3GZ
Dilation of Right Common Carotid Artery with Four or More Intraluminal Devices, Percutane
Approach
037H44Z
Dilation of Right Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneo
Endoscopic Approach
037H45Z
Dilation of Right Common Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037H46Z
Dilation of Right Common Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037H47Z
Dilation of Right Common Carotid Artery with Four or More Drug-eluting Intraluminal Devi
Percutaneous Endoscopic Approach
037H4DZ
Dilation of Right Common Carotid Artery with Intraluminal Device, Percutaneous Endoscopi
Approach
037H4EZ
Dilation of Right Common Carotid Artery with Two Intraluminal Devices, Percutaneous
Endoscopic Approach
037H4FZ
Dilation of Right Common Carotid Artery with Three Intraluminal Devices, Percutaneous
Endoscopic Approach
037H4GZ
Dilation of Right Common Carotid Artery with Four or More Intraluminal Devices, Percutane
Endoscopic Approach
037J34Z
Dilation of Left Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneou
Approach
037J35Z
Dilation of Left Common Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Approach
037J36Z
Dilation of Left Common Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037J37Z
Dilation of Left Common Carotid Artery with Four or More Drug-eluting Intraluminal Device
Percutaneous Approach
037J3DZ
Dilation of Left Common Carotid Artery with Intraluminal Device, Percutaneous Approach
037J3EZ
Dilation of Left Common Carotid Artery with Two Intraluminal Devices, Percutaneous Appro
037J3FZ
Dilation of Left Common Carotid Artery with Three Intraluminal Devices, Percutaneous App
037J3GZ
Dilation of Left Common Carotid Artery with Four or More Intraluminal Devices, Percutaneo
Approach
037J44Z
Dilation of Left Common Carotid Artery with Drug-eluting Intraluminal Device, Percutaneou
Endoscopic Approach
037J45Z
Dilation of Left Common Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037J46Z
Dilation of Left Common Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037J47Z
Dilation of Left Common Carotid Artery with Four or More Drug-eluting Intraluminal Device
Percutaneous Endoscopic Approach
037J4DZ
Dilation of Left Common Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037J4EZ
Dilation of Left Common Carotid Artery with Two Intraluminal Devices, Percutaneous
Endoscopic Approach

037J4FZ
Dilation of Left Common Carotid Artery with Three Intraluminal Devices, Percutaneous
Endoscopic Approach
037J4GZ
Dilation of Left Common Carotid Artery with Four or More Intraluminal Devices, Percutaneo
Endoscopic Approach
037K34Z
Dilation of Right Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneou
Approach
037K35Z
Dilation of Right Internal Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Approach
037K36Z
Dilation of Right Internal Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037K37Z
Dilation of Right Internal Carotid Artery with Four or More Drug-eluting Intraluminal Device
Percutaneous Approach
037K3DZ
Dilation of Right Internal Carotid Artery with Intraluminal Device, Percutaneous Approach
037K3EZ
Dilation of Right Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Appro
037K3FZ
Dilation of Right Internal Carotid Artery with Three Intraluminal Devices, Percutaneous Appr
037K3GZ
Dilation of Right Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneo
Approach
037K44Z
Dilation of Right Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneou
Endoscopic Approach
037K45Z
Dilation of Right Internal Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037K46Z
Dilation of Right Internal Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037K47Z
Dilation of Right Internal Carotid Artery with Four or More Drug-eluting Intraluminal Device
Percutaneous Endoscopic Approach
037K4DZ
Dilation of Right Internal Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037K4EZ
Dilation of Right Internal Carotid Artery with Two Intraluminal Devices, Percutaneous
Endoscopic Approach
037K4FZ
Dilation of Right Internal Carotid Artery with Three Intraluminal Devices, Percutaneous
Endoscopic Approach
037K4GZ
Dilation of Right Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneo
Endoscopic Approach
037L34Z
Dilation of Left Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037L35Z
Dilation of Left Internal Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Approach
037L36Z
Dilation of Left Internal Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037L37Z
Dilation of Left Internal Carotid Artery with Four or More Drug-eluting Intraluminal Devices
Percutaneous Approach
037L3DZ
Dilation of Left Internal Carotid Artery with Intraluminal Device, Percutaneous Approach
037L3EZ
Dilation of Left Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Approa
037L3FZ
Dilation of Left Internal Carotid Artery with Three Intraluminal Devices, Percutaneous Appro
037L3GZ
Dilation of Left Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneou
Approach
037L44Z
Dilation of Left Internal Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037L45Z
Dilation of Left Internal Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach

037L46Z
Dilation of Left Internal Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037L47Z
Dilation of Left Internal Carotid Artery with Four or More Drug-eluting Intraluminal Devices
Percutaneous Endoscopic Approach
037L4DZ
Dilation of Left Internal Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037L4EZ
Dilation of Left Internal Carotid Artery with Two Intraluminal Devices, Percutaneous Endosc
Approach
037L4FZ
Dilation of Left Internal Carotid Artery with Three Intraluminal Devices, Percutaneous
Endoscopic Approach
037L4GZ
Dilation of Left Internal Carotid Artery with Four or More Intraluminal Devices, Percutaneou
Endoscopic Approach
037M34Z
Dilation of Right External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneou
Approach
037M35Z
Dilation of Right External Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Approach
037M36Z
Dilation of Right External Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037M37Z
Dilation of Right External Carotid Artery with Four or More Drug-eluting Intraluminal Devic
Percutaneous Approach
037M3DZ
Dilation of Right External Carotid Artery with Intraluminal Device, Percutaneous Approach
037M3EZ
Dilation of Right External Carotid Artery with Two Intraluminal Devices, Percutaneous Appr
037M3FZ
Dilation of Right External Carotid Artery with Three Intraluminal Devices, Percutaneous
Approach
037M3GZ
Dilation of Right External Carotid Artery with Four or More Intraluminal Devices, Percutaneo
Approach
037M44Z
Dilation of Right External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneou
Endoscopic Approach
037M45Z
Dilation of Right External Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037M46Z
Dilation of Right External Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037M47Z
Dilation of Right External Carotid Artery with Four or More Drug-eluting Intraluminal Devic
Percutaneous Endoscopic Approach
037M4DZ
Dilation of Right External Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037M4EZ
Dilation of Right External Carotid Artery with Two Intraluminal Devices, Percutaneous
Endoscopic Approach
037M4FZ
Dilation of Right External Carotid Artery with Three Intraluminal Devices, Percutaneous
Endoscopic Approach
037M4GZ
Dilation of Right External Carotid Artery with Four or More Intraluminal Devices, Percutaneo
Endoscopic Approach
037N34Z
Dilation of Left External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Approach
037N35Z
Dilation of Left External Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Approach
037N36Z
Dilation of Left External Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Approach
037N37Z
Dilation of Left External Carotid Artery with Four or More Drug-eluting Intraluminal Device
Percutaneous Approach

037N3DZ
Dilation of Left External Carotid Artery with Intraluminal Device, Percutaneous Approach
037N3EZ
Dilation of Left External Carotid Artery with Two Intraluminal Devices, Percutaneous Appro
037N3FZ
Dilation of Left External Carotid Artery with Three Intraluminal Devices, Percutaneous Appr
037N3GZ
Dilation of Left External Carotid Artery with Four or More Intraluminal Devices, Percutaneou
Approach
037N44Z
Dilation of Left External Carotid Artery with Drug-eluting Intraluminal Device, Percutaneous
Endoscopic Approach
037N45Z
Dilation of Left External Carotid Artery with Two Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037N46Z
Dilation of Left External Carotid Artery with Three Drug-eluting Intraluminal Devices,
Percutaneous Endoscopic Approach
037N47Z
Dilation of Left External Carotid Artery with Four or More Drug-eluting Intraluminal Device
Percutaneous Endoscopic Approach
037N4DZ
Dilation of Left External Carotid Artery with Intraluminal Device, Percutaneous Endoscopic
Approach
037N4EZ
Dilation of Left External Carotid Artery with Two Intraluminal Devices, Percutaneous Endos
Approach
037N4FZ
Dilation of Left External Carotid Artery with Three Intraluminal Devices, Percutaneous
Endoscopic Approach
037N4GZ
Dilation of Left External Carotid Artery with Four or More Intraluminal Devices, Percutaneou
Endoscopic Approach
Under Part B, providers must bill HCPCS procedure code 37799. If above ICD-10-CM is applicable.
NOTE: ICD- codes are subject to modification. Providers must always ensure they are
using the latest and most appropriate codes.
170 - Billing Requirements for Lumbar Artificial Disc Replacement
(Rev. 992, Issued: 06-23-06, Effective: 05-16-06, Implementation: Carriers 07-17-06/FIs 10-01-06)
170.1 - General
(Rev. 1340, Issued: 09-21-07, Effective: 08-14-07, Implementation: 10-01-07)
Effective for services performed from May 16, 2006 through August 13, 2007, the Centers for Medicare &
Medicaid Services (CMS) made the decision that lumbar artificial disc replacement (LADR) with the
Charite
TM
lumbar artificial disc is non-covered for Medicare beneficiaries over 60 years of age. See Pub. 100-
03, Medicare National Coverage Determinations Manual, section 150.10, for more information about the non-
covered determination.
Effective for services performed on or after August 14, 2007, CMS made the decision that LADR with any
lumbar artificial disc is non-covered for Medicare beneficiaries over 60 years of age, (i.e., on or after a
beneficiary’s 61
st
birthday).
For Medicare beneficiaries 60 years of age and younger, there is no national coverage determination for
LADR, leaving such determinations to continue to be made by the local contractors.
170.2 - Carrier Billing Requirements
(Rev. 11902; Issued:03-16-23; Effective: 04-17-23; Implementation: 04-17-23)
Effective for services performed on or after May 16, 2006 through December 31, 2006, carriers shall deny
claims, for Medicare beneficiaries over 60 years of age, submitted with the following Category III Codes:
• 0091T Single interspace, lumbar; and
• 0092T Each additional interspace (List separately in addition to code for primary procedure.)
Effective for services performed on or after January 1, 2007 through August 13, 2007, for Medicare
beneficiaries over 60 years of age, LADR with the Charite
TM
lumbar artificial disc, carriers shall deny claims
submitted with the following codes:
• 22857 Total disc arthroplasty (artificial disc), anterior approach, including discectomy to prepare
interspace (other than for decompression), lumbar, single interspace
• 0163T Total disc arthroplasty (artificial disc), anterior approach, including discectomy to prepare
interspace (other than for decompression), lumbar, each additional interspace. NOTE:
Effective December 31, 2022, code 0163T is end dated.
Carriers shall continue to follow their normal claims processing criteria for IDEs for LADR performed with an
implant eligible under the IDE criteria.
For dates of service May 16, 2006 through August 13, 2007, Medicare coverage under the investigational
device exemption (IDE) for LADR with a disc other than the Charite
TM
lumbar disc in eligible clinical trials is
not impacted.
Effective for services performed on or after August 14, 2007, carriers shall deny claims for LADR surgery, for
Medicare beneficiaries over 60 years of age, (i.e., on or after a beneficiary’s 61
st
birthday) submitted with the
following codes:
• 22857 Total disc arthroplasty (artificial disc), anterior approach, including discectomy to prepare
interspace (other than for decompression), lumbar, single interspace
• 0163T Total disc arthroplasty (artificial disc), anterior approach, including
discectomy to prepare interspace (other than for decompression), lumbar, each
additional interspace NOTE: Effective December 31, 2022, code 0163T is end
dated.
• 22860 Total disc arthroplasty (artificial disc), anterior approach, including discectomy to prepare
interspace (other than for decompression); second interspace, lumbar. Effective 01/01/23
170.3 - A/B MAC (A) Billing Requirements
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC X12,
Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
The A/B MAC (A) will pay for LADR when approved under the IDE/clinical trial criteria only when
submitted with ICD-9-CM procedure code 84.65 if ICD-9 is applicable, with condition code 30 and if ICD-9-
CM is applicable, ICD-9-CM diagnosis code V70.7 when submitted on type of bill (TOB) 11X from May 16,
2006 through August 13, 2007.
Special Billing instructions:
For services performed on TOB 11X in critical access hospitals (CAH), the payment will be 101% of
reasonable cost.
For services performed on TOB 11X Indian Health Services (IHS) inpatient hospitals will pay under the
inpatient prospective payment system (IPPS) based on the DRG.
For services performed on TOB 11X, IHS CAHs will pay under 101% facility specific per diem rate.
NOTE: The ICD-9-CM procedure code 84.65 is not payable for beneficiaries over 60 years of age, with the
Charite
TM
lumbar artificial disc, which is the only one that is FDA approved for any diagnosis. If a different
manufacture’s disc is used in an approved clinical trials or is an approved IDE, then condition code 30 and
ICD-9-CM diagnosis code V70.7 must be on the claim for it to be payable.
Effective for discharges on or after August 14, 2007, CMS has found that LADR is not reasonable and
necessary for the Medicare population over 60 years of age. Therefore, LADR is non-covered for Medicare
beneficiaries over 60 years of age as identified in section 150.10, of Pub.100-03, the NCD Manual. A/B
MACS (A) shall deny claims with ICD-9-CM procedure code 84.65 for Medicare beneficiaries over 60 years
of age.
For Medicare beneficiaries 60 years of age and younger, there is no NCD, leaving such determinations to
continue to be made by the local contractors.
170.4 – Reasons for Denial and Medicare Summary Notice (MSN), Claim Adjustment
Reason Code Messages, and Remittance Advice Remark Code
(Rev. 1340, Issued: 09-21-07, Effective: 08-14-07, Implementation: 10-01-07)
Contractors shall use the following messages when denying claims for Medicare beneficiaries over 60 years of
age (i.e. on or after a beneficiary’s 61
st
birthday).
21.24 “This service is not covered for patients over age 60.”
“Este servicio no está cubierto en pacientes mayores de 60 años.”
Use an appropriate Claim Adjustment Reason Code:
96 "Non-covered charge(s)."
Use an appropriate Remittance Advice Remark Code:
N386 “This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have Web access, you may contact the contractor to
request a copy of the NCD.”
170.5 - Advance Beneficiary Notice (ABN) and Hospital Issued Notice of Noncoverage
(HINN) Information
(Rev. 1340, Issued: 09-21-07, Effective: 08-14-07, Implementation: 10-01-07)

Providers must be advised that the provider is liable for charges if the lumbar artificial disc replacement is
used in the surgery, unless the beneficiary was informed that he/she would be financially responsible prior to
performance of the procedure. To avoid this liability the provider should have the beneficiary sign an ABN.
The HINN model language should be adapted to this situation in the sections addressing description of the
care at issue if the surgery is performed on an inpatient basis. Unless the beneficiary was informed prior to the
admission that he/ she would be financially liable for the admission, the provider is liable. To avoid this
liability the provider must issue a HINN. Other content requirements of a HINN still apply. Use the HINN
letter most appropriate to the overall situation.
180 – Cryosurgery of the Prostate Gland
(Rev. 1111, Issued: 11-09-06, Effective: 04-01-07, Implementation: 04-02-07)
Cryosurgery of the prostate gland, also known as cryosurgical ablation of the prostate (CAP), destroys
prostate tissue by applying extremely cold temperatures in order to reduce the size of the prostate gland.
180.1 - Coverage Requirements
(Rev. 1111, Issued: 11-09-06, Effective: 04-01-07, Implementation: 04-02-07)
Medicare covers cryosurgery of the prostate gland effective for claims with dates of service on or after July 1,
1999. The coverage is for:
1. Primary treatment of patients with clinically localized prostate cancer, Stages T1 – T3 (diagnosis code is
185 – malignant neoplasm of prostate).
2. Salvage therapy (effective for claims with dates of service on or after July 1, 2001 for patients:
a. Having recurrent, localized prostate cancer;
b. Failing a trial of radiation therapy as their primary treatment; and
c. Meeting one of these conditions: State T2B or below; Gleason score less than 9 or; PSA less
than 8 ng/ml.
180.2 - Billing Requirements
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC X12,
Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
Claims for cryosurgery for the prostate gland are to be submitted on the ASC X12 837, or, in exceptional
circumstances, on a hard copy Form CMS – 1450. This procedure can be rendered in an inpatient or
outpatient hospital setting (types of bill (TOBs) 11x 13x, 83x, and 85x).
The A/B MAC (A) will look for the following when processing claims with cryosurgery services:
• If ICD-9-CM is applicable, ICD-9 CM diagnosis code 185 or
• If ICD-10-CM is applicable, ICD-10 CM diagnosis code C61 must be on all cryosurgical claims;
• For outpatient claims HCPCS 55873 and revenue codes 0360, 0361, or 0369 Cryosurgery ablation of
localized prostate cancer, stages T1- T3 (includes ultrasonic guidance for interstitial cryosurgery probe
placement, postoperative irrigations and aspiration of sloughing tissue included) must be on all
outpatient claims; and
• For inpatient claims correct procedure codes are:
o If ICD-9-CM is applicable, ICD-9-CM procedure code 60.62 (perineal prostatectomy- the
definition includes cryoablation of prostate, cryostatectomy of prostate, and radical
cryosurgical ablation of prostate)
o If ICD-10 is applicable,ICD-10-PCS procedure code 0V500ZZ (Destruction of Prostate, Open
Approach), or 0V503ZZ (Destruction of Prostate, Percutaneous Approach), or 0V504ZZ
(Destruction of Prostate, Percutaneous Endoscopic Approach).
180.3 – Payment Requirements
(Rev. 1111, Issued: 11-09-06, Effective: 04-01-07, Implementation: 04-02-07)
This service may be paid as a primary treatment for patients with clinically localized prostate cancer, Stages
T1 – T3. The ultrasonic guidance associated with this procedure will not be paid for separately, but is bundled
into the payment for the surgical procedure. When one provider has furnished the cryosurgical ablation and
another the ultrasonic guidance, the provider of the ultrasonic guidance must seek compensation from the
provider of the cryosurgical ablation.
Effective July 1, 2001, cryosurgery performed as salvage therapy, will be paid only according to the coverage
requirements described above.
Type of facility and setting determines the basis of payment:
• For services performed on an inpatient or outpatient basis in a CAH, TOBs 11x and 85x: the FI will
pay 101 percent of reasonable cost minus any applicable deductible and coinsurance.
• For services performed on an inpatient basis in short term acute care hospitals, (including those in
Guam, America Samoa, Virgin Islands, Saipan, and Indian Health Services Hospitals) TOB 11x: the
FI will pay the DRG payment minus any applicable deductible and coinsurance.
• For services performed on an outpatient basis in hospitals subject to the Outpatient PPS, TOB 13x: the
FI will pay the assigned APC minus any applicable deductible and coinsurance.
• For outpatient services in hospitals that are exempt from OPPS (such as in American Samoa, Virgin
Islands, Guam, and Saipan) TOBs 13x: the FI will pay reasonable cost, minus any applicable
deductible and coinsurance.
• For outpatient services in Indian Health Service hospitals TOBs 13x and 83x: the FI will pay the ASC
payment amount for TOB 83x. minus any applicable deductible and coinsurance.
• For inpatient or outpatient services in hospitals in Maryland, make payment according to the State Cost
Containment system.
For services performed on an inpatient basis: the hospitals exempt from inpatient acute care PPS shall be paid
on reasonable cost basis, minus any applicable deductible and coinsurance.
180.4 - Claim Adjustment Reason Codes, Remittance Advice Remark Codes, Group
Codes, and Medicare Summary Notice Messages
(Rev 2544, Issued: 09-13-2012, Effective: 10-01-2012, Implementation: 10-01-2012)
Contractors shall use the appropriate claim adjustment reason codes (CARCs), remittance advice remark
codes (RARCs), group codes, or Medicare summary notice (MSN) messages when denying payment for
alcohol misuse screening and alcohol misuse behavioral counseling sessions:
• For RHC and FQHC claims that contain screening for alcohol misuse HCPCS code G0442 and alcohol
misuse counseling HCPCS code G0443 with another encounter/visit with the same line item date of
service, use group code CO and reason code:
o Claim Adjustment Reason Code (CARC) 97 – The benefit for this service is included in the
payment/allowance for another service/procedure that has already been adjudicated. Note: Refer to
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF) if
present
• Denying claims containing HCPCS code G0442 and HCPCS code G0443 submitted on a TOB other than
13X, 71X, 77X, and 85X:
o Claim Adjustment Reason Code (CARC) 5 - The procedure code/bill type is inconsistent with the
place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF) if present
o Remittance Advice Remark Code (RARC) M77 – Missing/incomplete/invalid place of service
o Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a claim is
received with a GA modifier indicating a signed ABN is on file.
o Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
NOTE: For modifier GZ, use CARC 50 and MSN 8.81 per instructions in CR 7228/TR 2148.
• Denying claims that contains more than one alcohol misuse behavioral counseling session G0443 on the
same date of service:
o Medicare Summary Notice (MSN) 15.6 – The information provided does not support the need for this
many services or items within this period of time.
o Claim Adjustment Reason Code (CARC) 151 – Payment adjusted because the payer deems the
information submitted does not support this many/frequency of services.
o Remittance Advice Remark Code (RARC) M86 – Service denied because payment already made for
same/similar procedure within set time frame.
o Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a claim is
received with a GA modifier indicating a signed ABN is on file.
o Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
NOTE: For modifier GZ, use CARC 50 and MSN 8.81 per instructions in CR 7228/TR 2148.
• Denying claims that are not submitted from the appropriate provider specialties:
o Medicare Summary Notice (MSN) 21.18 – This item or service is not covered when performed or
ordered by this provider.
o Claim Adjustment Reason Code (CARC) 185 - The rendering provider is not eligible to perform the
service billed. NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF), if present.
o Remittance Advice Remark Code (RARC) N95 - This provider type/provider specialty may not bill
this service.
o Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a claim is
received with a GA modifier indicating a signed ABN is on file.
o Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
NOTE: For modifier GZ, use CARC 50 and MSN 8.81 per instructions in CR 7228/TR 2148.
• Denying claims without the appropriate POS code:
o Medicare Summary Notice (MSN) 21.25 – This service was denied because Medicare only covers this
service in certain settings.
o Claim Adjustment Reason Code (CARC) 58 – Treatment was deemed by the payer to have been
rendered in an inappropriate or invalid place of service. Note: Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF) if present.
o Remittance Advice Remark Code (RARC) N428 – Not covered when performed in this place of
service.
o Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a claim is
received with a GA modifier indicating a signed ABN is on file.
o Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
NOTE: For modifier GZ, use CARC 50 and MSN 8.81 per instructions in CR 7228/TR 2148.
• Denying claims for alcohol misuse screening HCPCS code G0442 more than once in a 12-month period,
and denying alcohol misuse counseling sessions HCPCS code G0443 more than four times in the same 12-
month period:
o Medicare Summary Notice (MSN) 20.5 – These services cannot be paid because your benefits are
exhausted at this time.
o Claim Adjustment Reason Code (CARC) 119 – Benefit maximum for this time period or occurrence
has been reached.
o Remittance Advice Remark Code (RARC) N362 – The number of Days or Units of service exceeds
our acceptable maximum.
o Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a claim is
received with a GA modifier indicating a signed ABN is on file.
o Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
NOTE: For modifier GZ, use CARC 50 and MSN 8.81 per instructions in CR 7228/TR 2148.
• Denying claims for alcohol misuse counseling session HCPCS code G0443 when there is no claim in
history for the screening service HCPCS code G0442 in the prior 12 months:
° Medicare Summary Notice (MSN) 16.26 – Medicare does not pay for services or items related
to a procedure that has not been approved or billed.
° Claim Adjustment Reason Code (CARC) B15 – This service/procedure requires that a
qualifying service/procedure be received and covered. The qualifying other service/procedure
has not been received/adjudicated. Note: Refer to the 835 Healthcare Policy Identification
Segment (loop 2110 Service Payment Information REF), if present.
° Remittance Advice Remark Code (RARC) M16 – Alert: Please see our web site, mailings, or
bulletins for more details concerning this policy/procedure/decision.
° Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary, if a
claim is received with a modifier indicating a signed ABN is on file.
° Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received without a modifier indicating no signed ABN is on file.
180.5 – Additional CWF and Contractor Requirements
(Rev 2544, Issued: 09-13-2012, Effective: 10-01-2012, Implementation: 10-01-2012)
• When applying frequency, CWF shall count 11 full months following the month of the last alcohol
misuse screening visit, G0442, before allowing subsequent payment of another G0442 screening.
• CWF shall reject incoming claims when G0443 PROF is billed if four G0443 services have been billed
and posted to the BEHV auxiliary file within the 12 month period.
• CWF shall continue to reject incoming claims with consistency error code ‘32#3’ when HCPCS code
G0442 PROF and HCPCS code G0443 PROF are billed on same day for TOB 71X, 77X, 85X with
096X, 097X and 098X.
• Contractors and CWF shall use the last date of G0442 PROF for counting the 12-month period for
G0443 PROF services.
° Contractors and CWF shall apply all the same TOBs (13x,71x, 77x and 85x with Rev. Code 96, 97
and 98) POS (11, 22, 49 and 71), no deductible/co-insurance and institutional/professional
processing for G0443 that was implemented for G0442 in CR 7633.
• If a claim with G0442 is cancelled, CWF shall do a look back for claims with G0443 and create an
IUR (Information Unsolicited Response) along with a Trailer ‘24’ back to the contractor to reject the
G0443 claim(s) paid within the 12 month period of the G0442 claims.
• CWF shall display the number of counseling sessions remaining for G0443 PROF on all CWF
provider query screens (HUQA, HIQA, HIQH, ELGA, ELGB, ELGH).
• CWF shall display the remaining PROF services counting DOWN from four (4) for the HCPCS code
‘G0443’ on the MBD/NGD extract file.
° CWF shall calculate a next eligible date for G0442 PROF and G0443 PROF for a given
beneficiary.
° The calculation shall include all applicable factors including beneficiary Part B entitlement
status, beneficiary claims history and utilization rules.
° When there is no next eligible date, the CWF provider query screens shall display an 8-position
alpha code in the date field to indicate why there is not a next eligible date.
° Any change to beneficiary master data or claims data that would result in a change to any next
eligible date shall result in an update to the beneficiary’s next eligible date.
NOTE: If G0442 is not paid, the beneficiary is not eligible for G0443.
ο CWF shall create a utility to remove previously posted G0442 TECH for the AUX file.
ο CWF shall remove G0442/G0443 TECH from editing, MBD, NGD, Provider Inquiry screens
and all other applicable areas (i.e., HICR) previously done under CR 7633.
Frequency Requirements
When applying frequency, CWF shall count 11 full months following the month of the last alcohol misuse
screening visit, G0442, before allowing subsequent payment of another G0442 screening. Additionally, CWF
shall create an edit to allow alcohol misuse brief behavioral counseling, HCPCS G0443, no more than 4 times
in a 12-month period. CWF shall also count four alcohol misuse counseling sessions HCPCS G0443 in the
same 12-month period used for G0442 counting from the date the G0442 screening session was billed.
When applying frequency limitations to G0442 screening on the same date of service as G0443 counseling,
CWF shall allow both a claim for the professional service and a claim for a facility fee. CWF shall identify
the following institutional claims as facility fee claims for screening services: TOB 13X, TOB 85X when the
revenue code is not 096X, 097X, or 098X. CWF shall identify all other claims as professional service claims
for screening services (professional claims, and institutional claims with TOB 71X, 77X, and 85X when the
revenue code is 096X, 097X, or 098X). NOTE: This does not apply to RHCs and FQHCs.
190 – Billing Requirements for Extracorporeal Photopheresis
(Rev. 3050, Issued: 08-22-14, Effective: 09-23-14, ICD-10: Upon Implementation of ICD-10,
Implementation: 09-23-14, ICD-10: Upon Implementation of ICD-10)
Effective for dates of services on and after December 19, 2006, Medicare has expanded coverage for
extracorporeal photopheresis for patients with acute cardiac allograft rejection whose disease is refractory to
standard immunosuppresive drug treatment and patients with chronic graft versus host disease whose disease
is refractory to standard immunosuppresive drug treatment. (See the National Coverage Determinations
(NCD) Manual, Pub. 100-03, Chapter 1, part 2, section 110.4, for complete coverage guidelines.)
Effective for claims with dates of service on or after April 30, 2012, the Centers for Medicare & Medicaid
Services has expanded coverage for extracorporeal photopheresis for the treatment of bronchiolitis obliterans
syndrome (BOS) following lung allograft transplantation only when extracorporeal photopheresis is provided
under a clinical research study that meets specific requirements to assess the effect of extracorporeal
photopheresis for the treatment of BOS following lung allograft transplantation. Further coverage criteria is
outlined in Pub. 100-03, Chapter 1, part 2, section 110.4 of the NCD Manual.
190.1 – Applicable Intermediary Bill Types
(Rev. 1206; Issued: 03-16-07; Effective: December 19, 2006; Implementation: 04-02-07)
11X, 13X, or 85X
190.2 – Healthcare Common Procedural Coding System (HCPCS), Applicable Diagnosis
Codes and Procedure Code
(Rev.10881; Issued: 08-06-2021; Effective: 09-07-2021; Implementation: 09-07- 2021)
The following HCPCS procedure code is used for billing extracorporeal photopheresis:
•
36522 - Photopheresis, extracorporeal
Effective for claims with dates of service on or after Oct 1, 2015, the following are the applicable ICD-10-
CM procedure codes for the new expanded coverage:
• 6A650ZZ Phototherapy, Circulatory, Single
• 6A651ZZ Phototherapy, Circulatory, Multiple
NOTE: Contractors shall edit for an appropriate oncological and autoimmune disorder diagnosis for
payment of extracorporeal photopheresis according to the NCD.
Effective for claims with dates of service on or after Oct 1, 2015, in addition to HCPCS 36522, the following
ICD-10-CM codes are applicable for extracorporeal photopheresis for the treatment of BOS following lung
allograft transplantation only when extracorporeal photopheresis is provided under a clinical research study as
outlined in above sections 190 and 190.2 Healthcare Common Procedural Coding System (HCPCS) codes,
and applicable diagnosis codes as below::

A reference listing of ICD-10-CM coding and descriptions is listed below:
CUTANEOUS T-CELL LYMPHOMA
C84.01
Mycosis fungoides, lymph nodes of head, face, and neck
C84.02
Mycosis fungoides, intrathoracic lymph nodes
C84.03
Mycosis fungoides, intra-abdominal lymph nodes
C84.04
Mycosis fungoides, lymph nodes of axilla and upper limb
C84.05
Mycosis fungoides, lymph nodes of inguinal region and lower limb
C84.06
Mycosis fungoides, intrapelvic lymph nodes
C84.07
Mycosis fungoides, spleen
C84.08
Mycosis fungoides, lymph nodes of multiple sites
C84.09
Mycosis fungoides, extranodal and solid organ sites
C84.11
Sézary disease, lymph nodes of head, face, and neck
C84.12
Sézary disease, intrathoracic lymph nodes
C84.13
Sézary disease, intra-abdominal lymph nodes
C84.14
Sézary disease, lymph nodes of axilla and upper limb
C84.15
Sézary disease, lymph nodes of inguinal region and lower limb
C84.16
Sézary disease, intrapelvic lymph nodes
C84.17
Sézary disease, spleen
C84.18
Sézary disease, lymph nodes of multiple sites
C84.19
Sezary disease, extranodal/solid organ sites
C84.A0
Cutaneous T-cell lymphoma, unspecified, unspecified site
C84.A1
Cutaneous T-cell lymphoma, unspecified lymph nodes of head, face, and neck
C84.A2
Cutaneous T-cell lymphoma, unspecified, intrathoracic lymph nodes
C84.A3
Cutaneous T-cell lymphoma, unspecified, intra-abdominal lymph nodes
C84.A4
Cutaneous T-cell lymphoma, unspecified, lymph nodes of axilla and upper limb
C84.A5
Cutaneous T-cell lymphoma, unspecified, lymph nodes of inguinal region and lower limb
C84.A6
Cutaneous T-cell lymphoma, unspecified, intrapelvic lymph nodes
C84.A7
Cutaneous T-cell lymphoma, unspecified, spleen
C84.A8
Cutaneous T-cell lymphoma, unspecified, lymph nodes of multiple sites
C84.A9
Cutaneous T-cell lymphoma, unspecified, extranodal and solid organ sites
ACUTE CARDIAC ALLOGRAFT REJECTION/GRAFT-VERSUS-HOST-DISEASE
D89.811
Chronic graft-versus-host disease
D89.812
Acute on chronic graft-versus-host disease
D89.813
Graft-versus-host disease, unspecified
T86.01
Bone marrow transplant rejection
T86.02
Bone marrow transplant failure
T86.03
Bone marrow transplant infection
T86.21
Heart transplant rejection
T86.22
Heart transplant failure
T86.23
Heart transplant infection
T86.290
Cardiac allograft vasculopathy
T86.31
Heart-lung transplant rejection
T86.32
Heart-lung transplant failure
T86.33
Heart-lung transplant infection
T86.5
Complications of stem cell transplant
Z94.3
Heart and lungs transplant status

Z94.81
Bone marrow transplant status
BOS (CED/TRIAL ONLY)
J42
Unspecified chronic bronchitis
J44.0
Chronic obstructive pulmonary disease with (acute) lower respiratory infection
J44.1
Chronic obstructive pulmonary disease with (acute) exacerbation
J44.9
Chronic obstructive pulmonary disease, unspecified
T86.810
Lung transplant rejection
T86.811
Lung transplant failure
T86.812
Lung transplant infection
T86.818
Other complications of lung transplant
T86.819
Unspecified complication of lung transplant
Z94.2
Lung transplant status
Z00.6
Encounter for examination for normal comparison and control in clinical research program
190.3 – Medicare Summary Notices (MSNs), Remittance Advice Remark Codes (RAs)
and Claim Adjustment Reason Code
(Rev.10881; Issued: 08-06-2021; Effective: 09-07-2021; Implementation: 09-07- 2021)
Contractors shall continue to use the appropriate existing messages that they have in place when denying
claims submitted that do not meet the Medicare coverage criteria for extracorporeal photopheresis.
Medicare coverage for extracorporeal photopheresis is restricted to the inpatient or outpatient hospital
settings specifically for BOS, and not for the other covered diagnosis (including chronic graft versus host
disease) which remain covered in the hospital inpatient, hospital outpatient, and non-facility (physician-
directed clinic or office settings) settings.
Contractors shall deny claims for extracorporeal photopheresis for BOS when the service is not rendered to
an inpatient or outpatient of a hospital, including critical access hospitals using the following codes:
• Claim Adjustment Reason Code (CARC) 96 – Non-covered charge(s). At least one Remark Code
must be provided (may be comprised of either the NCPDP Reject Reason [sic] Code, or Remittance
Advice Remark Code that is not an ALERT.) NOTE: Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF), if present.
• CARC 171 – Payment is denied when performed/billed by this type of provider in this type of
facility. NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF), if present.
• Medicare Summary Notice 16.2 - This service cannot be paid when provided in this
location/facility." Spanish translation: "Este servicio no se puede pagar cuando es suministrado en
esta sitio/facilidad. (Include either MSN 36.1 or 36.2 dependent on liability.)
• Remittance Advice Remark Code (RARC) N428 – Not covered when performed in
this place of service. (A/MACs only)
B.
Group Code CO (Contractual Obligations) or PR (Patient Responsibility) dependent
on liability.
Contractors shall return to provider/ return as unprocessable claims for BOS containing HCPCS procedure
code 36522 along with one of the allowable ICD-10 codes if the claim is missing diagnosis code Z00.6 (as
primary/secondary diagnosis, institutional only), condition code 30 (institutional claims only), clinical trial
modifier Q0/Q1, and value code D4 with an 8-digit clinical trial identifier number (A/MACs only). Use the
following messages:
When diagnosis code Z00.6 is missing, use:
• CARC 16 “Claim/service lacks information or has submission/billing error(s).” and
• RARC M76, “Missing/incomplete/invalid diagnosis or condition.”
When Condition Code 30 is missing, use CARC 16 and
• RARC M44 “Missing/incomplete/invalid condition code.”
When Clinical Trial modifier Q0/Q1 is missing, use CARC 16 and
• RARC N822, “Missing procedure modifier(s).”
When Clinical Trial Number is missing, use CARC 16 and
• RARC MA50, “Missing/incomplete/invalid Investigational Device Exemption number or Clinical
Trial number.”
When Value Code D4 is missing, use CARC 16 and
• RARC M49, “Missing/incomplete/invalid value code(s) or amount(s).”
190.4 – Advance Beneficiary Notice and Hospital Issued Notice of Noncoverage
Information
(Rev. 1206; Issued: 03-16-07; Effective: December 19, 2006; Implementation: 04-02-07)
If this service is not reasonable and necessary under 1862(a)(1)(A) of the Act (falls outside the scope of the
revised NCD found in Pub. 100-03, chapter 1, section 110.4), contractors shall advise physicians and/or
hospital outpatient departments, including critical access hospitals (CAHs), that they will be held liable for
charges unless the physician and/or hospital has the beneficiary sign an Advance Beneficiary Notice in
advance of providing the service.
If this service is provided to a hospital inpatient, including CAHs, for a reason unrelated to the admission
(outside of the bundled payment) contractors shall advise hospitals billing for inpatient services that they will
be held liable for charges unless the hospital has the beneficiary sign a Hospital Issued Notice of Noncoverage
letter 11 in advance of providing the service.
200 - Billing Requirements for Vagus Nerve Stimulation (VNS)
(Rev. 1271, Issued: 06-22-07; Effective: 05-04-07; Implementation: 07-23-07)
200.1 - General
(Rev. 1271, Issued: 06-22-07; Effective: 05-04-07; Implementation: 07-23-07)
VNS is a pulse generator, similar to a pacemaker, that is surgically implanted under the skin of the left chest
and an electrical lead (wire) is connected from the generator to the left vagus nerve. Electrical signals are sent
from the battery-powered generator to the vagus nerve via the lead. These signals are in turn sent to the brain.
FDA approved VNS for treatment of refractory epilepsy in 1999. Further coverage guidelines can be found in
the National Coverage Determination Manual (Publication 100-03), Chapter 1, Section 160.18. Since the
HCPCS codes for VNS can also be used for other indications, contractors must determine if the service being
billed are for VNS and make a determination to pay or deny. CMS guidance on payment is listed below.
200.2 - ICD-10 Diagnosis Codes for Vagus Nerve Stimulation (Covered since DOS on and
after July 1, 1999)
(Rev. 12435, Issued:12-28-23, Effective:01-29-24, Implementation:01-29-24)
One of the following diagnosis codes must be reported as appropriate, when
billing for Vagus Nerve Stimulation:
If ICD-10-CM is applicable:
• G40.011 Localization-related (focal) (partial) idiopathic epilepsy and
epileptic syndromes with seizures of localized onset, intractable, with
status epileptic
• G40.019 Localization-related (focal) (partial) idiopathic epilepsy and
epileptic syndromes with seizures of localized onset, intractable, without
status epilepticus
• G40.111 Localization-related (focal) (partial) symptomatic epilepsy and
epileptic syndromes with simple partial seizures, intractable, with status
epilepticus
• G40.119 Localization-related (focal) (partial) symptomatic epilepsy and
epileptic syndromes with simple partial seizures, intractable, without status
epilepticus
• G40.211 Localization-related (focal) (partial) symptomatic epilepsy and
epileptic syndromes with complex partial seizures, intractable, with status
epilepticus
• G40.219 Localization-related (focal) (partial) symptomatic epilepsy and
epileptic syndromes with complex partial seizures, intractable, without
status epilepticus
• G40.833 Dravet syndrome, intractable, with status epilepticus
• G40.834 Dravet syndrome, intractable, without status epilepticus
• G40.C11 Lafora progressive myoclonus epilepsy, intractable, with status epilepticus
• G40.C19 Lafora progressive myoclonus epilepsy, intractable, without status epilepticus
200.3 - Carrier/MAC Billing Requirements
(Rev. 1271, Issued: 06-22-07; Effective: 05-04-07; Implementation: 07-23-07)
Effective for services performed on or after July 1, 1999, contractors are accepting claims
submitted for vagus nerve stimulation for epilepsy and recurrent seizures.
Effective for services performed on or after July 1, 1999, CMS determined that vagus nerve
stimulation is not reasonable and necessary for all other types of seizures which are refractory
and for whom surgery is not recommended or for whom surgery has failed.
Effective for services performed on or after May 4, 2007, contractors will deny claims
submitted for vagus nerve stimulation for resistant depression. Contractors need to update
their local coverage determination policy to include this new NCD determination. There is no
coverage for vagus nerve stimulation for patient with resistant depression.
200.4 - Fiscal Intermediary Billing Requirements
(Rev. 1271, Issued: 06-22-07; Effective: 05-04-07; Implementation: 07-23-07)
Effective for services performed on or after July 1, 1999, contractors are accepting claims
submitted for vagus nerve stimulation for epilepsy and recurrent seizures.
Effective for services performed on or after July 1, 1999, CMS determined that vagus nerve
stimulation is not reasonable and necessary for all other types of seizures which are refractory
and for whom surgery is not recommended or for whom surgery has failed.
Effective for services performed on or after May 4, 2007, contractors will reject claims
submitted for vagus nerve stimulation for resistant depression.
200.5 - Medicare Summary Notice (MSN), Remittance Advice Remark
Code (RARC) and Claim Adjustment Reason Code (CARC) Messages
(Rev.11035, Issued:10-13-21, Effective: 11-17-21; Implementation: 11-17-21)
The following messages are used by Medicare contractors when denying non- covered VNS
services:
MSN: 16.10 “Medicare does not pay for this item or service."
CARC: 50 “These are non-covered services because this is not deemed a “medical
necessity” by the payer."
The following RARC messages can be used depending on liability:
M27 Alert: The patient has been relieved of liability of payment of these items and services
under the limitation of liability provision of the law. You, the provider, are ultimately liable for
the patient's waived charges, including any charges for coinsurance, since the items or services
were not reasonable and necessary or constituted custodial care, and you knew or could
reasonably have been expected to know, that they were not covered. You may appeal this
determination. You may ask for an appeal regarding both the coverage determination and the
issue of whether you exercised due care. The appeal request must be filed within 120 days of the
date you receive this notice. You must make the request through this office.
Or
M38 Alert: The patient is liable for the charges for this service as you informed the patient in
writing before the service was furnished that we would not pay for it, and the patient agreed to
pay.
Contractors will also include group code CO (contractual obligation) or PR (patient
responsibility) depending on liability.
200.6 - Advance Beneficiary Notice and HINN Information
(Rev. 1271, Issued: 06-22-07; Effective: 05-04-07; Implementation: 07-23-07)
Physicians are liable for non-covered VNS procedures unless they issue an appropriate
advance beneficiary notice (ABN). The following language should be included in the ABN:
Items or Service Section:
“Vagas Nerve Stimulation”.
Because Section:
“As specified in section 160.18 of Pub.100-03, Medicare National Coverage Determination
Manual, Medicare will not pay for this procedure as it is not a reasonable and necessary
treatment for (select either “your type of seizure disorder” or “resistant depression.”)
Note that the ABN is the appropriate notice for Part B services and is valid whether the
language above is inserted or not.
210 - Billing Requirements for Continuous Positive Airway Pressure
(CPAP) for Obstructive Sleep Apnea (OSA)
(Rev.)
220 - Billing Requirements for Thermal Intradiscal Procedures (TIPs)
(Rev. 1646, Issued: 12-09-08, Effective: 09-29-08, Implementation: 01-05-09)
220.1 - General
(Rev. 1646, Issued: 12-09-08, Effective: 09-29-08, Implementation: 01-05-09)
Effective for services on or after September 29, 2008, the Center for Medicare & Medicaid
Services (CMS) made the decision that Thermal Intradiscal Procedures (TIPS) are not
reasonable and necessary for the treatment of low back pain. Therefore, TIPs are non-
covered. Refer to Pub.100-03, Medicare National Coverage Determination (NCD) Manual
Chapter 1, Part 2, Section 150.11, for further information on the NCD.
220.2 - Contractors, A/B Medicare Administrative Contractors (MACs)
(Rev. 1646, Issued: 12-09-08, Effective: 09-29-08, Implementation: 01-05-09)
The following Healthcare Common Procedure Coding System (HCPCS) codes will be
nationally non-covered by Medicare effective for dates of service on and after September 29,
2008:
22526: Percutaneous intradiscal electrothermal annuloplasty, unilateral or bilateral including
fluoroscopic guidance; single level
22527: Percutaneous intradiscal electrothermal annuloplasty, unilateral or bilateral including
fluoroscopic guidance; one or more additional levels

0062T: Percutaneous intradiscal annuloplasty, any method except electrothermal, unilateral
or bilateral including fluoroscopic guidance; single level
0063T: Percutaneous intradiscal annuloplasty, any method except electrothermal, unilateral
or bilateral including fluoroscopic guidance; one or more additional levels
NOTE: The change to add the non-covered indicator for the above HCPCS codes will be
part of the January 2009 Medicare Physician Fee Schedule Update. The change to the status
indicator to non-cover the above HCPCS will be part of the January Integrated Outpatient
Code Editor (IOCE) update.
Claims submitted with the non-covered HCPCS codes on or after September 29, 2008, will be
denied by Medicare contractors.
220.3 - Medicare Summary Notice (MSN), Claim Adjustment Reason Code
(CARC), and Remittance Advice Remark Code (RARC)
(Rev. 1646, Issued: 12-09-08, Effective: 09-29-08, Implementation: 01-05-09)
The following messages are used by Medicare contractors when denying non-covered TIP
services:
• MSN: 21.11 “This service was not covered by Medicare at the time you received it.”
• CARC: 96 “Non-covered charge(s)”
N386 “This decision was based on a National Coverage Determination (NCD). An NCD
provides a coverage determination as to whether a particular item or service is covered. A
copy of this policy is available at http://www.cms.hhs.gov/med/search.asp. If you do not have
web access, you may contact the contractor to request a copy of the NCD.”
220.4 - Advance Beneficiary Notice (ABN)
(Rev. 1646, Issued: 12-09-08, Effective: 09-29-08, Implementation: 01-05-09)
Providers are liable for charges if TIPS is used in surgery, unless the beneficiary was
informed that he/she would be financially responsible prior to performance of the procedure.
To avoid this liability the provider should have the beneficiary sign an ABN.
230 – Billing Wrong Surgical or Other Invasive Procedures Performed on a
Patient, Surgical or Other Invasive Procedures Performed on the Wrong
Body Part, and Surgical or Other Invasive Procedures Performed on the
Wrong Patient
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
The Centers for Medicare & Medicaid Services (CMS) internally generated a request for a
national coverage analysis (NCA) to establish national coverage determinations (NCDs)
addressing Medicare coverage of Wrong Surgical or Other Invasive Procedures Performed on
a Patient, Surgical or Other Invasive Procedures Performed on the Wrong Body Part, and
Surgical or Other Invasive Procedures Performed on the Wrong Patient. Information
regarding these NCDs can be found in Publication (Pub.) 100-03, Chapter 1, sections 140.6,
140.7, and 140.8, respectively.
Inpatient Claims

Hospitals are required to bill two claims when a surgical error is reported and a covered
service is also being reported:
• One claim with covered service(s)/procedure(s) unrelated to the erroneous surgery(s)
on a Type of Bill (TOB) 11X (with the exception of 110), and
• The other claim with the non-covered service(s)/procedure(s) related to the erroneous
surgery(s) on a TOB 110 (no-pay claim)
NOTE: Both the covered and non-covered claim shall have a matching Statement Covers
Period.
For discharges prior to October 1, 2009, the non-covered TOB 110 must indicate on the 837
institutional claim format, or in the Remarks field of the Form CMS1450 one of the
applicable erroneous surgery(s) two-digit codes (entered exactly as specified below):
• For a wrong surgery on patient, enter the following: MX
• For a surgery on a wrong body part, enter the following: MY
• For a surgery on wrong patient, enter the following: MZ
For discharges on or after October 1, 2009, the non-covered TOB 110 must have one of the
following diagnosis codes reported in diagnosis position 2-9, instead of billing the
aforementioned two-digit codes in Remarks:
If ICD-9-CM Is Applicable
• E876.5 - Performance of wrong operation (procedure) on correct patient (existing
code)
• E876.6 - Performance of operation (procedure) on patient not scheduled for surgery
• E876.7- Performance of correct operation (procedure) on wrong side/body part
NOTE: The above codes shall not be reported in the External Cause of Injury (E-code)
field.
If ICD-10-CM Is Applicable
• Y65.51 Performance of wrong procedure (operation) on correct patient
• Y65.52 Performance of procedure (operation) on patient not scheduled for surgery
• Y65.53 Performance of correct procedure (operation) on wrong side of body parts
Outpatient, Ambulatory Surgical Centers, and Practitioner Claims
Providers are required to append one of the following applicable HCPCS modifiers to all lines
related to the erroneous surgery(s):
• PA: Surgery Wrong Body Part
• PB: Surgery Wrong Patient
• PC: Wrong Surgery on Patient
All claims
Claim/Lines submitted with a surgical error will be denied/line-item denied using the
following:
Medicare Summary Notice
23.17 – Medicare won’t cover these services because they are not considered medically
necessary.”
23.17 – Medicare no cubrirá estos servicios porque no son considerados necesarios por
razones médicas.

Claim Adjustment Reason Code
CARC 50 – These are non-covered services because this is not deemed a ‘medical necessity”
by the payer.
Group Code
CO – Contractual Obligation
Beneficiary Liability
Generally, beneficiary liability notices such an Advance Beneficiary Notice of Non-coverage
(ABN) or a Hospital Issued Notice of Non-coverage (HINN) is appropriate when a provider is
furnishing an item or service that the provider reasonably believes Medicare will not cover on
the basis of §1862(a)(1). An ABN must include all of the elements described in Pub. 100-04,
Claims Processing Manual (CPM), Ch. 30, §50.6.3, in order to be considered valid. For
example, the ABN must specifically describe the item or service expected to be denied (e.g. a
left leg amputation) and must include a cost estimate for the non-covered item or service.
Similarly, HINNs must specifically describe the item or service expected to be denied (e.g. a
left leg amputation) and must include all of the elements described in the instructions found in
the CPM Ch. 3,0 §200. Thus, a provider cannot shift financial liability for the non-covered
services to the beneficiary, unless the ABN or the HINN satisfies all of the applicable
requirements in the CPM Ch. 30, §50.6.3 and §200, respectively. Given these requirements,
CMS cannot envision a scenario in which HINNs or ABNs could be validly delivered in these
NCD cases. However, an ABN or a HINN could be validly delivered prior to furnishing
services related to the follow-up care for the non-covered surgical error that would not be
considered a related service to the non-covered surgical error.
240 – Special Instructions for Services with a Gender/Procedure Conflict
(Rev. 1877, Issued: 12-18-09, Effective: 04-01-10, Implementation: 04-05-10)
Claims for some services for beneficiaries with transgender, ambiguous genitalia, and
hermaphrodite issues, may inadvertently be denied due to sex related edits unless these
services are billed properly.
The National Uniform Billing Committee (NUBC) has approved condition code 45
(Ambiguous Gender Category) as a result of the increasing number of claims received that are
denied due to sex/diagnosis and sex/procedure edits. This claim level condition code should
be used by institutional providers to identify these unique claims and alerts the fiscal
intermediary that the gender/procedure or gender/diagnosis conflict is not an error allowing
the sex related edits to be by-passed.
The KX modifier (Requirements specified in the medical policy have been met) is now a
multipurpose informational modifier and will also be used identify services for transgender,
ambiguous genitalia, and hermaphrodite beneficiaries in addition to its other existing uses.
Physicians and non-physician practitioners should use modifier KX with procedure codes that
are gender specific in the particular cases of transgender, ambiguous genitalia, and
hermaphrodite beneficiaries. Therefore, if a gender/procedure or gender/diagnosis conflict
edit occurs, the KX modifier alerts the MAC that it is not an error and will allow the claim to
continue with normal processing.
240.1 - Billing Instructions for Institutional Providers
(Rev. 1877, Issued: 12-18-09, Effective: 04-01-10, Implementation: 04-05-10)
Institutional providers are to report condition code 45 on any inpatient or outpatient claim
related to transgender, ambiguous genitalia, or hermaphrodite issues.
240.2 – Billing Instructions for Physicians and Non-Physician Practitioners
(Rev. 1877, Issued: 12-18-09, Effective: 04-01-10, Implementation: 04-05-10)
The KX modifier is to be billed on the detail line only with the procedure code(s) that is
gender specific for transgender, ambiguous genitalia, and hermaphrodite beneficiaries.
(NOTE: The KX modifier is a multipurpose informational modifier, and may also be used in
conjunction with other medical policies.)
250 – Pharmacogenomic Testing for Warfarin Response
(Rev. 1889, Issued: 01-08-10; Effective Date: 08-03-09; Implementation Date: 04-05-
10)
250.1 – Coverage Requirements
(Rev. 1889, Issued: 01-08-10; Effective Date: 08-03-09; Implementation Date: 04-05-
10)
Effective August 3, 2009, pharmacogenomic testing to predict warfarin responsiveness is
covered only when provided to Medicare beneficiaries who are candidates for anticoagulation
therapy with warfarin; i.e., have not been previously tested for CYP2C9 or VKORC1 alleles;
and have received fewer than five days of warfarin in the anticoagulation regimen for which
the testing is ordered; and only then in the context of a prospective, randomized, controlled
clinical study when that study meets certain criteria as outlined in Pub 100-03, section 90.1,
of the NCD Manual.
NOTE: A new temporary HCPCS Level II code effective August 3, 2009, G9143, warfarin
responsiveness testing by genetic technique using any method, any number of specimen(s),
was developed to enable implementation of CED for this purpose.
250.2 – Billing Requirements
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Institutional clinical trial claims for pharmacogenomic testing for warfarin response are
identified through the presence of all of the following elements:
• Value Code D4 and 8-digit clinical trial number (when present on the claim) - Refer to
Transmittal 310, Change Request 5790, dated January 18, 2008;
• ICD-10 diagnosis code Z00.6 (secondary) - Refer to Transmittal 310, Change Request
5790, dated January 18, 2008; and Z79.01 (primary);
• Condition Code 30 - Refer to Transmittal 310, Change Request 5790, dated January 18,
2008;
• HCPCS modifier Q0: outpatient claims only - Refer to Transmittal 1418, Change
Request 5805, dated January 18, 2008; and,
• HCPCS code G9143 (mandatory with the April 2010 Integrated Outpatient Code Editor
(IOCE) and the January 2011 Clinical Laboratory Fee Schedule (CLFS) updates. Prior
to these times, any trials should bill FIs for this test as they currently do absent these
instructions, and the FIs should process and pay those claims accordingly.)
Practitioner clinical trial claims for pharmacogenomic testing for warfarin response are
identified through the presence of all of the following elements:

• ICD-10-diagnosis code Z00.6 (secondary), and ICD-10 diagnosis code Z79.01
(primary) MCS edit 031L70.7;
• 8-digit clinical trial number(when present on the claim);
• HCPCS modifier Q0; and, MCS edit 031L
• HCPCS code G9143 (to be carrier priced for claims with dates of service on and
after August 3, 2009, that are processed prior to the January 2011 CLFS
update.)
NOTE: This NCD does not determine coverage to identify CYP2C9 or VKORC1 alleles for
other purposes beside warfarin responsiveness, nor does it determine national coverage to
identify other alleles to predict warfarin responsiveness. These decisions are made at the local
MAC level.
250.3 – Payment Requirements
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Beginning April 5, 2010, for claims with dates of service on and after August 3, 2009, the
Medicare Shared System will track the number of times a beneficiary receives
pharmacogenomic testing for warfarin response. When a claim is received for
pharmacogenomic testing for warfarin response, and the shared system has determined
that the beneficiary has already received the test in his/her lifetime, it will generate a
Medicare line-item denial and the Medicare contractor will provide the following
messages to enforce the one-time limitation for the test:
Claim Adjustment Reason Code (CARC) 50 – These are non-covered services because this
is not deemed a ‘medical necessity’ by the payer. This change to be effective April 1, 2010:
These are non-covered services because this is not deemed a ‘medical necessity’ by the
payer.
NOTE: Refer to the 835 Healthcare Policy Identification Segment, if present.
Remittance Advice Remark Code (RARC) N362 – The number of Days or Units of Service
exceeds our acceptable maximum.
Group Code CO – Contractual Obligation
Medicare Summary Notice (MSN) 16.76 – This service/item was not covered because you
have exceeded the lifetime limit for getting this service/item. (Este servicio/artículo no fue
cubierto porque usted ya se ha pasado del límite permitido de por vida, para recibirlo.).
The Medicare shared system and the A/B MACs (B) will also ensure that pharmacogenomic
testing for warfarin response is billed in accordance with clinical trial reporting
requirements. In other words, the shared system and the A/B MACs (B) will return to
provider/return as unprocessable lines for pharmacogenomic testing for warfarin response
when said line is not billed with HCPCS modifier Q0 and ICD-10- CM diagnosis code if
applicable, ICD-10-CM Z00.6 is not present as a secondary diagnosis. When the system or
the A/B MAC (B) initiates the line- item return to provider or returns the claim as
unprocessable, the Medicare contractor will respond with the following messages:
For a missing Q0 modifier:
CARC 4 - The procedure code is inconsistent with the modifier used or a required modifier
is missing.

For a missing Z00.6 diagnosis code when a HCPCS Q0 modifier is reported with HCPCS
G9143:
CARC 16 - Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either the NCPDP Reject Reason
Code, or Remittance Advice Remark Code that is not an ALERT.)
Remark Code M64 - Missing/incomplete/invalid other diagnosis.
For either a missing Q0 modifier and/or a missing ICD-10-CM Z00.6 diagnosis code:
Group Code CO- Contractual Obligation
MSN 16.77 – This service/item was not covered because it was not provided as part of a
qualifying trial/study. (Este servicio/artículo no fue cubierto porque no estaba incluido
como parte de un ensayo clínico/estudio calificado.)
260 - Dermal Injections for Treatment of Facial Lipodystrophy Syndrome
(LDS)
(Rev. 2105, Issued: 11-24-10, Effective: 03-23-10, Implementation: 07-06-10)
260.1 – Policy
(Rev. 2105, Issued: 11-24-10, Effective: 03-23-10, Implementation: 07-06-10)
The Centers for Medicare & Medicaid Services (CMS) received a request for national
coverage of treatments for facial lipodystrophy syndrome (LDS) for human
immunodeficiency virus (HIV)-infected Medicare beneficiaries. Facial LDS is often
characterized by a loss of fat that results in a facial abnormality such as severely sunken
cheeks. This fat loss can arise as a complication of HIV and/or highly active antiretroviral
therapy. Due to their appearance and stigma of the condition, patients with facial LDS may
become depressed, socially isolated, and in some cases may stop their HIV treatments in an
attempt to halt or reverse this complication.
Effective for claims with dates of service on and after March 23, 2010, dermal injections for
facial LDS are only reasonable and necessary using dermal fillers approved by the Food and
Drug Administration for this purpose, and then only in HIV-infected beneficiaries who
manifest depression secondary to the physical stigmata of HIV treatment.
See Pub. 100-03, National Coverage Decision manual, section 250.5, for detailed policy
information concerning treatment of LDS.
260.1.1– Hospital Billing Instructions
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
A - Hospital Outpatient Claims
For hospital outpatient claims, hospitals must bill covered dermal injections for
treatment of facial LDS by having all of the required elements on the claim:
1. A line with HCPCS codes Q2026 or Q2027 with a Line Item Date of service
(LIDOS) on or after March 23, 2010,
NOTE: Q2027 is replaced with Q2028 effective 1/1/14 as per the 2014 HCPCS
update.
2. A line with HCPCS code G0429 with a LIDOS on or after March 23, 2010,

3. If ICD-10-CM is applicable, ICD-10-CM diagnosis codes B20 Human
Immunodeficiency Virus (HIV) disease and E88.1 Lipodystrophy, not elsewhere
classified
The applicable NCD is 250.5 Facial Lipodystrophy.
B - Outpatient Prospective Payment System (OPPS) Hospitals or Ambulatory
Surgical Centers (ASCs):
For line item dates of service on or after March 23, 2010, and until HCPCS codes Q2026
and Q2027 are billable, facial LDS claims shall contain a temporary HCPCS code C9800,
instead of HCPCS G0429 and HCPCS Q2026/Q2027, as shown above.
NOTE: Q2027 is replaced with Q2028 effective 1/1/14 as per the 2014, HCPCS
update.
C - Hospital Inpatient Claims
Hospitals must bill covered dermal injections for treatment of facial LDS by having all of
the required elements on the claim:
C.
Discharge date on or after March 23, 2010,
D.
If ICD-10-PCS is applicable,
• ICD-10-PCS procedure code 3E00XGC Introduction of Other Therapeutic
Substance into Skin and Mucous Membrances, External Approach, or
E.
If ICD-10-CM is applicable on or after 10/01/2015,
disease and E88.1 Lipodystrophy not elsewhere classified.
A diagnosis code for a comorbidity of depression may also be required for coverage on an
outpatient and/or inpatient basis as determined by the individual Medicare contractor’s
policy.
260.2 –Billing Instructions
(Rev. 2105, Issued: 11-24-10, Effective: 03-23-10, Implementation: 07-06-10)
260.2.1 – Hospital Billing Instructions
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
A - Hospital Outpatient Claims
For hospital outpatient claims, hospitals must bill covered dermal injections for treatment of
facial LDS by having all of the required elements on the claim:
• A line with HCPCS codes Q2026 or Q2027 with a Line Item Date of service (LIDOS)
on or after March 23, 2010,

• A line with HCPCS code G0429 with a LIDOS on or after March 23, 2010,
• If ICD-9-CM is applicable, ICD-9-CM diagnosis codes 042 (HIV) and 272.6
(Lipodystrophy) or,
• If ICD-10-CM is applicable, ICD-10-CM diagnosis codes B20 Human
Immunodeficiency Virus (HIV) disease and E88.1 Lipodystrophy, not elsewhere
classified
The applicable NCD is 250.5 Facial Lipodystrophy.
B - Outpatient Prospective Payment System (OPPS) Hospitals or Ambulatory Surgical
Centers (ASCs):
For line item dates of service on or after March 23, 2010, and until HCPCS codes Q2026 and
Q2027 are billable, facial LDS claims shall contain a temporary HCPCS code C9800, instead
of HCPCS G0429 and HCPCS Q2026/Q2027, as shown above.
C - Hospital Inpatient Claims
Hospitals must bill covered dermal injections for treatment of facial LDS by having all of the
required elements on the claim:
• Discharge date on or after March 23, 2010,
• If ICD-9-CM is applicable,
o ICD-9-CM procedure code 86.99 (other operations on skin and subcutaneous
tissue, i.e., injection of filler material), or
o ICD-9-CM diagnosis codes 042 (HIV) and 272.6 (Lipodystrophy)
• If ICD-10-PCS is applicable,
o ICD-10-PCS procedure code 3E00XGC Introduction of Other Therapeutic
Substance into Skin and Mucous Membrances, External Approach, or
o ICD-10-CM diagnosis codes B20 Human Immundodeficiency Virus [HIV]
disease and E88.1 Lipodystrophy not elsewhere classified.
A diagnosis code for a comorbidity of depression may also be required for coverage on an
outpatient and/or inpatient basis as determined by the individual Medicare contractor’s policy.
260.2.2 – Practitioner Billing Instructions
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Practitioners must bill covered claims for dermal injections for treatment of facial LDS by
having all of the required elements on the claim:
Performed in a non-facility setting:
• A line with HCPCS codes Q2026 or Q2027 with a LIDOS on or after March 23,
2010,
NOTE: Q2027 is replaced with Q2028 effective 1/1/14 per the 2014 HCPCS update.
• A line with HCPCS code G0429 with a LIDOS on or after March 23, 2010,
51 If ICD-10-CM applies, diagnosis codes B20 Human Immunodeficiency Virus
(HIV) disease and E88.1 (Lipodystrophy not elsewhere classified). Both
diagnoses are required on the claim.
NOTE: A diagnosis code for a comorbidity of depression may also be required for
coverage based on the individual Medicare contractor’s policy.
52 A line with HCPCS code G0429 with a LIDOS on or after March 23, 2010,
Virus (HIV) disease and E88.1 (Lipodystrophy not elsewhere classified). Both
diagnoses are required on the claim.
NOTE: A diagnosis code for a comorbidity of depression may also be required for
coverage based on the individual Medicare contractor’s policy.
260.3 – Claims Processing System Editing
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Billing for Services Prior to Medicare Coverage
Hospitals and practitioners billing for dermal injections for treatment of facial LDS prior to
the coverage date of March 23, 2010, will receive the following messages upon their
Medicare denial:
• Claim Adjustment Reason Code (CARC) 26: Expenses incurred prior to coverage.
NOTE: Outpatient hospitals and beneficiaries that received services in a hospital
outpatient setting may receive different message as established by their particular
Medicare contractor processing the claim.)
Medicare beneficiaries whose provider bills Medicare for dermal injections for treatment of
facial LDS prior to the coverage date of March 23, 2010, will receive the following
Medicare Summary Notice (MSN) message upon the Medicare denial:
•
- This service was not covered by Medicare at the time you received it. (Spanish
Version: Este servicio no estaba cubierto por Medicare cuando usted lo recibió.)
Billing for Services Not Meeting Comorbidity Coverage Requirements
Hospitals and practitioners billing for dermal injections for treatment of facial LDS on
patients that do not have a comorbidity of HIV and lipodystrophy (or even depression if
deemed required by the Medicare contractor) will receive the following messages upon
their Medicare denial:
• CARC 50: These are non-covered services because this is not deemed a 'medical
necessity' by the payer. Note: Refer to the 835 Healthcare Policy Identification
Segment (loop 2110 Service Payment Information REF), if present.
• RARC N386: This decision was based on a National Coverage Determination
(NCD). An NCD provides a coverage determination as to whether a particular item
or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may
contact the contractor to request a copy of the NCD.
• RARC M64: Missing/incomplete/invalid other diagnosis.
• Group Code: CO
Medicare beneficiaries who do not meet Medicare comorbidity requirements of HIV and
lipodystrophy (or even depression if deemed required by the Medicare contractor) and
whose provider bills Medicare for dermal injections for treatment of facial LDS will
receive the following MSN message upon the Medicare denial:
15.4 - The information provided does not support the need for this service or item. (Spanish
Version: La información proporcionada no confirma la necesidad para este servicio oículo.)
270 – Claims Processing for Implantable Automatic Defibrillators
(Rev. 2005, Issued: 7-23-10, Effective: 8-31-10, Implementation: 8-31-10)
Coverage Requirements- The implantable automatic defibrillator is an electronic device
designed to detect and treat life threatening tachyarrhythmias. The device consists of a pulse
generator and electrodes for sensing and defibrillating.
See §20.4 -Medicare National Coverage Determinations (NCD) Manual for the complete list
of covered indications.
270.1 – Coding Requirements for Implantable Automatic Defibrillators
(Rev. 2998, Issued: 07-25-14, Effective: Upon implementation of ICD-10; 01-01-12 - ASC
X12, Implementation: 08-25-2014 - ASC X12; Upon Implementation of ICD-10)
The following are the applicable HCPCS procedure codes for implantable automatic
defibrillators:
33240- (Insertion of single or dual chamber pacing cardioverter-defibrillator pulse
generator)
33241(Subcutaneous removal of single or dual chamber pacing cardioverter-
defibrillator pulse generator)
33243 (Removal of single or dual chamber pacing cardioverter-defibrillator
electrode(s); by thoracotomy)
33244 (Removal of single or dual chamber pacing cardioverter-defibrillator electrodes
by transvenous extraction)
33249- (Insertion or repositioning of electrode leads(s) for single or dual chamber
pacing cardioverter-defibrillator and insertion of pulse generator)
For inpatient hospitals claims, if ICD-9 CM is applicable use procedure code 37.94. If ICD-
10-PCS is applicable the following applies.
More than one ICD-10-PCS code (a cluster) is required. There are two possible clusters:
FIRST CLUSTER: Use 1 code from the first list and one code from the second list.
Cluster 1 first list:
0JH608Z Insertion of Defibrillator Generator into Chest Subcutaneous Tissue and Fascia, Open
Approach
0JH638Z Insertion of Defibrillator Generator into Chest Subcutaneous Tissue and Fascia,
Percutaneous Approach
0JH808Z Insertion of Defibrillator Generator into Abdomen Subcutaneous Tissue and Fascia, Open
Approach
0JH838Z Insertion of Defibrillator Generator into Abdomen Subcutaneous Tissue and Fascia,
Percutaneous Approach
Cluster 1 second list:
02H60KZ Insertion of Defibrillator Lead into Right Atrium, Open Approach
02H63KZ Insertion of Defibrillator Lead into Right Atrium, Percutaneous Approach
02H64KZ Insertion of Defibrillator Lead into Right Atrium, Percutaneous Endoscopic
Approach
02H70KZ Insertion of Defibrillator Lead into Left Atrium, Open Approach
02H73KZ Insertion of Defibrillator Lead into Left Atrium, Percutaneous Approach
02H74KZ Insertion of Defibrillator Lead into Left Atrium, Percutaneous Endoscopic
Approach
02HK0KZ Insertion of Defibrillator Lead into Right Ventricle, Open Approach
02HK3KZ Insertion of Defibrillator Lead into Right Ventricle, Percutaneous Approach
02HK4KZ Insertion of Defibrillator Lead into Right Ventricle, Percutaneous Endoscopic
Approach
02HL0KZ Insertion of Defibrillator Lead into Left Ventricle, Open Approach
02HL3KZ Insertion of Defibrillator Lead into Left Ventricle, Percutaneous Approach
02HL4KZ Insertion of Defibrillator Lead into Left Ventricle, Percutaneous Endoscopic
Approach
SECOND CLUSTER:
Use 1 code from 1st list & 1 code from the 4th list; also add one code from each of the
2nd & 3rd lists if doing a replacement instead of initial insertion.
Cluster 2 first list:
0JH608Z Insertion of Defibrillator Generator into Chest Subcutaneous Tissue and Fascia,
Open Approach
0JH638Z Insertion of Defibrillator Generator into Chest Subcutaneous Tissue and Fascia,
Percutaneous Approach
0JH808Z Insertion of Defibrillator Generator into Abdomen Subcutaneous Tissue and Fascia,
Open Approach
0JH838Z Insertion of Defibrillator Generator into Abdomen Subcutaneous Tissue and Fascia,
Percutaneous Approach
Cluster 2 second list:
0JPT0PZ Removal of Cardiac Rhythm Related Device from Trunk Subcutaneous Tissue and
Fascia, Open Approach
0JPT3PZ Removal of Cardiac Rhythm Related Device from Trunk Subcutaneous Tissue and
Fascia, Percutaneous Approach
Cluster 2 third list:
02PA0MZ Removal of Cardiac Lead from Heart, Open Approach
02PA3MZ Removal of Cardiac Lead from Heart, Percutaneous Approach
02PA4MZ Removal of Cardiac Lead from Heart, Percutaneous Endoscopic Approach
02PAXMZ Removal of Cardiac Lead from Heart, External Approach
Cluster 2 fourth list:
02H60KZ Insertion of Defibrillator Lead into Right Atrium, Open Approach
02H63KZ Insertion of Defibrillator Lead into Right Atrium, Percutaneous Approach
02H64KZ Insertion of Defibrillator Lead into Right Atrium, Percutaneous Endoscopic
Approach
02H70KZ Insertion of Defibrillator Lead into Left Atrium, Open Approach
02H73KZ Insertion of Defibrillator Lead into Left Atrium, Percutaneous Approach
02H74KZ Insertion of Defibrillator Lead into Left Atrium, Percutaneous Endoscopic
Approach
02HK0KZ Insertion of Defibrillator Lead into Right Ventricle, Open Approach
02HK3KZ Insertion of Defibrillator Lead into Right Ventricle, Percutaneous Approach
02HK4KZ Insertion of Defibrillator Lead into Right Ventricle, Percutaneous Endoscopic
Approach
02HL0KZ Insertion of Defibrillator Lead into Left Ventricle, Open Approach
02HL3KZ Insertion of Defibrillator Lead into Left Ventricle, Percutaneous Approach
02HL4KZ Insertion of Defibrillator Lead into Left Ventricle, Percutaneous Endoscopic
Approach
270.2 – Billing Requirements for Patients Enrolled in a Data Collection
System
(Rev.11759, Issued:12-21-2022, Effective:01-23-2023, Implementation:01-23-2023)
Effective for dates of service on or after April 1, 2005, Medicare required that patients
receiving a defibrillator for the primary prevention of sudden cardiac arrest be enrolled in a
qualifying data collection system. Providers shall use modifier Q0 to identify patients whose
data is being submitted to a data collection system.
The following diagnosis codes identify non-primary prevention (secondary prevention)
patient or replacement implantations (e.g. due to recalled devices):
If ICD-9-CM is applicable, select from the following diagnosis codes:
427.1 Ventricular tachycardia
427.41 Ventricular fibrillation
427.42 Ventricular flutter
427.5 Cardiac arrest
427.9 Cardiac dysrhythmia, unspecified
V12.53 Personal history of sudden cardiac arrest
996.04 Mechanical complication of cardiac device, implant, and graft, due to automatic
implantable cardiac defibrillator
V53.32 Fitting and adjustment of other device, automatic implantable cardiac defibrillator
If ICD-10-CM is applicable, select from the following list:
I47.0 Re-entry Ventricular Arrhythmia
I47.2 Ventricular Tachycardiaselect - end date September 30, 2022
I47.20 Ventricular Tachycardia, unspecified - effective October 1, 2022
I47.21 Torsades De Pointes - effective October 1, 2022
I47.29 Other Ventricular Tachycardia - effective October 1, 2022
I49.3 Ventricular Premature depolarization
I49.01 Ventricular Fibrillation
I49.02 Ventricular Flutter
I46.2 Cardiac arrest due to underlying cardiac condition
I46.8 Cardiac arrest due to other underlying condition
I46.9 Cardiac arrest, cause unspecified
I49.9 Cardiac arrhythmia, unspecified
T82.110A Breakdown (mechanical) of cardiac electrode, initial encounter
T82.111A Breakdown (mechanical) of cardiac pulse generator (battery), initial encounter
T82.118A Breakdown (mechanical) of other cardiac electronic device, initial encounter
T82.119A Breakdown (mechanical) of unspecified cardiac electronic device, initial encounter
T82.120A Displacement of cardiac electrode, initial encounter
T82.121A Displacement of cardiac pulse generator (battery), initial encounter
T82.128A Displacement of other cardiac electronic device, initial encounter
T82.129A Displacement of unspecified cardiac electronic device, initial encounter
T82.190A Other mechanical complication of cardiac electrode, initial encounter
T82.191A Other mechanical complication of cardiac pulse generator (battery), initial
encounter
T82.198A Other mechanical complication of other cardiac electronic device, initial encounter
T82.199A Other mechanical complication of unspecified cardiac device, initial encounter
Z86.74 Personal history of sudden cardiac arrest
Z45.02 Encounter for adjustment and management of automatic implantable cardiac
defibrillator
When any of the above codes appear on a claim, the Q0 modifier is not required. The Q0
modifier may be appended to claims for secondary prevention indications when data is being
entered into a qualifying data collection system.
280 - Autologous Cellular Immunotherapy Treatment of Prostate Cancer
(Rev. 2380, Issued: 01-06-12, Effective: 06-30-11, Implementation: 08-08-11)
280.1 - Policy
(Rev. 2380, Issued: 01-06-12, Effective: 06-30-11, Implementation: 08-08-11)
Effective for services furnished on or after June 30, 2011, a National Coverage Determination
(NCD) provides coverage of sipuleucel-T (PROVENGE®) for patients with asymptomatic or
minimally symptomatic metastatic, castrate-resistant (hormone refractory) prostate cancer.
Conditions of Medicare Part A and Medicare Part B coverage for sipuleucel-T are located in
the Medicare NCD Manual, Publication 100-03, section 110.22.
280.2 - Healthcare Common Procedure Coding System (HCPCS) Codes
and Diagnosis Coding
(Rev. 2380, Issued: 01-06-12, Effective: 06-30-11, Implementation: 08-08-11)
HCPCS Codes
Effective for claims with dates of service on June 30, 2011, Medicare providers shall report
one of the following HCPCS codes for PROVENGE®:
• C9273 - Sipuleucel-T, minimum of 50 million autologous CD54+ cells activated with
PAP-GM-CSF, including leukapheresis and all other preparatory procedures, per infusion,
or
• J3490 – Unclassified Drugs, or
• J3590 – Unclassified Biologics.

NOTE: Contractors shall continue to process claims for HCPCS code C9273, J3490, and
J3590, with dates of service June 30, 2011, as they do currently.
Effective for claims with dates of service on and after July 1, 2011, Medicare providers shall
report the following HCPCS code:
• Q2043 – Sipuleucel-T, minimum of 50 million autologous CD54+ cells activated with
PAP-GM-CSF, including leukapheresis and all other preparatory procedures, per infusion;
short descriptor, Sipuleucel-T auto CD54+.
ICD-9 Diagnosis Coding
For claims with dates of service on and after July 1, 2011, for PROVENGE®, the on-label
indication of asymptomatic or minimally symptomatic metastatic, castrate-resistant (hormone
refractory) prostate cancer, must be billed using ICD-9 code 185 (malignant neoplasm of
prostate) and at least one of the following ICD-9 codes:
ICD-9
code
Description
196.1
Secondary and unspecified malignant
neoplasm of intrathoracic lymph nodes
196.2
Secondary and unspecified malignant
neoplasm of intra-abdominal lymph nodes
196.5
Secondary and unspecified malignant
neoplasm of lymph nodes of inguinal
region and lower limb
196.6
Secondary and unspecified malignant
neoplasm of intrapelvic lymph nodes
196.8
Secondary and unspecified malignant
neoplasm of lymph nodes of multiple sites
196.9
Secondary and unspecified malignant
neoplasm of lymph node site unspecified -
The spread of cancer to and establishment
in the lymph nodes.
197.0
Secondary malignant neoplasm of lung –
Cancer that has spread from the original
(primary) tumor to the lung. The spread of
cancer to the lung. This may be from a
primary lung cancer, or from a cancer at a
distant site.
197.7
Malignant neoplasm of liver secondary -
Cancer that has spread from the original
(primary) tumor to the liver. A malignant
neoplasm that has spread to the liver from
another (primary) anatomic site. Such
malignant neoplasms may be carcinomas
(e.g., breast, colon), lymphomas,
melanomas, or sarcomas.
198.0
Secondary malignant neoplasm of kidney -
The spread of the cancer to the kidney.
This may be from a primary kidney cancer

involving the opposite kidney, or from a
cancer at a distant site.
198.1
Secondary malignant neoplasm of other
urinary organs
198.5
Secondary malignant neoplasm of bone
and bone marrow – Cancer that has spread
from the original (primary) tumor to the
bone. The spread of a malignant neoplasm
from a primary site to the skeletal system.
The majority of metastatic neoplasms to
the bone are carcinomas.
198.7
Secondary malignant neoplasm of adrenal
gland
198.82
Secondary malignant neoplasm of genital
organs
Coding for Off-Label PROVENGE® Services
The use of PROVENGE® off-label for the treatment of prostate cancer is left to the discretion
of the Medicare Administrative Contractors. Claims with dates of service on and after July 1,
2011, for PROVENGE® paid off-label for the treatment of prostate cancer must be billed
using either ICD-9 code 233.4 (carcinoma in situ of prostate), or ICD-9 code 185 (malignant
neoplasm of prostate) in addition to HCPCS Q2043. Effective with the implementation date
for ICD-10 codes, off-label PROVENGE® services must be billed with either ICD-10 code
D075(carcinoma in situ of prostate), or C61 (malignant neoplasm of prostate) in addition to
HCPCS Q2043.
ICD-10 Diagnosis Coding
Contractors shall note the appropriate ICD-10 code(s) that are listed below for future
implementation. Contractors shall track the ICD-10 codes and ensure that the updated edit is
turned on as part of the ICD-10 implementation effective October 1, 2013.
ICD-10 Description
C61 Malignant neoplasm of prostate (for on-
label or off-label indications)
D075 Carcinoma in situ of prostate (for off-label
indications only)
C77.1
Secondary and unspecified malignant
neoplasm of intrathoracic lymph nodes
C77.2
Secondary and unspecified malignant
neoplasm of intra-abdominal lymph nodes
C77.4
Secondary and unspecified malignant
neoplasm of inguinal and lower limb
lymph nodes
C77.5
Secondary and unspecified malignant
neoplasm of intrapelvic lymph nodes
C77.8
Secondary and unspecified malignant
neoplasm of lymph nodes of multiple
regions

C77.9
Secondary and unspecified malignant
neoplasm of lymph node, unspecified
C78.00
Secondary malignant neoplasm of
unspecified lung
C78.01
Secondary malignant neoplasm of right
lung
C78.02 Secondary malignant neoplasm of left lung
C78.7 Secondary malignant neoplasm of liver
C79.00
Secondary malignant neoplasm of
unspecified kidney and renal pelvis
C79.01
Secondary malignant neoplasm of right
kidney and renal pelvis
C79.02
Secondary malignant neoplasm of left
kidney and renal pelvis
C79.10
Secondary malignant neoplasm of
unspecified urinary organs
C79.11 Secondary malignant neoplasm of bladder
C79.19
Secondary malignant neoplasm of other
urinary organs
C79.51 Secondary malignant neoplasm of bone
C79.52
Secondary malignant neoplasm of bone
marrow
C79.70
Secondary malignant neoplasm of
unspecified adrenal gland
C79.71
Secondary malignant neoplasm of right
adrenal gland
C79.72
Secondary malignant neoplasm of left
adrenal gland
C79.82
Secondary malignant neoplasm of genital
organs
280.3 - Types of Bill (TOB) and Revenue Codes
(Rev. 2380, Issued: 01-06-12, Effective: 06-30-11, Implementation: 08-08-11)
The applicable TOBs for PROVENGE® are: 12X, 13X, 22X, 23X, 71X, 77X, and 85X.
On institutional claims, TOBs 12X, 13X, 22X, 23X, and 85X, use revenue code 0636 - drugs
requiring detailed coding.
280.4 - Payment Method
(Rev. 2380, Issued: 01-06-12, Effective: 06-30-11, Implementation: 08-08-11)
Payment for PROVENGE® is as follows:
• TOBs 12X, 13X, 22X and 23X - based on the Average Sales Price (ASP) + 6%,
• TOB 85X – based on reasonable cost,
• TOBs 71X and 77X – based on all-inclusive rate.
For Medicare Part B practitioner claims, payment for PROVENGE® is based on ASP + 6%.
Contractors shall not pay separately for routine costs associated with PROVENGE®, HCPCS
Q2043, except for the cost of administration. (Q2043 is all-inclusive and represents all routine
costs except for its cost of administration).
280.5 - Medicare Summary Notices (MSNs), Remittance Advice Remark
Codes (RARCs), Claim Adjustment Reason Codes (CARCs), and Group
Codes
(Rev. 2394, Issued: 01-25-12, Effective: 06-30-11 for-(claims with dates of service on or
after 07-01- 11 processed on or after July 02-12, Implementation: 07-02-12)
Contractors shall use the following messages when denying claims for the on-label indication
for PROVENGE®, HCPCS Q2043, submitted without ICD-9-CM diagnosis code 185 and at
least one diagnosis code from the ICD-9 table in Section 280.2 above:
MSN 14.9 - Medicare cannot pay for this service for the diagnosis shown on the claim.
Spanish Version - Medicare no puede pagar por este servicio debido al diagnóstico indicado
en la reclamación.
RARC 167 - This (these) diagnosis (es) are not covered. Note: Refer to the 835 Healthcare
Policy Identification segment (loop 2110 Service Payment Information REF), if present.
Group Code – CO (Contractual Obligation)
Contractors shall use the following messages when denying claims for the off-label indication
for PROVENGE®, HCPCS Q2043, submitted without ICD-9-CM diagnosis code 233.4:
MSN 14.9 - Medicare cannot pay for this service for the diagnosis shown on the claim.
Spanish Version - Medicare no puede pagar por este servicio debido al diagnóstico indicado
en la reclamación.
RARC 167 - This (these) diagnosis (es) are not covered. Note: Refer to the 835 Healthcare
Policy Identification segment (loop 2110 Service Payment Information REF), if present.
Group Code – CO (Contractual Obligation)
For claims with dates of service on or after July 1, 2012, processed on or after July 2, 2012,
when denying claims for PROVENGE®, HCPCS Q2043® that exceed three (3) services in a
patient’s lifetime, contractors shall use the following messages:
MSN 20.5 - These services cannot be paid because your benefits are exhausted at this time.
Spanish Version - Estos servicios no pueden ser pagados porque sus beneficios se han
agotado.
RARC N362 - The number of Days or Units of Service exceeds our acceptable maximum.
CARC 149 - Lifetime benefit maximum has been reached for this service/benefit category.
Group Code – CO (Contractual Obligation)
290 – Transcatheter Aortic Valve Replacement (TAVR)
(Rev. 10179, Issued: 06-10-20, Effective: 06-21-19, Implementation: 06-12-20)
Transcatheter aortic valve replacement (TAVR - also known as TAVI or transcatheter aortic
valve implantation) is used in the treatment of aortic stenosis. A bioprosthetic valve is
inserted percutaneously using a catheter and implanted in the orifice of the aortic valve.
The most recent reconsideration of the TAVR policy is effective for claims with dates of
service on and after June 21, 2019. It makes changes to the criteria for the heart team and the
hospital, and to the trial outcomes and the registry questions/criteria. Please see Publication
100-03, National Coverage Determination Manual Part 1, section 20.32, for complete national
policy criteria.
HISTORICAL NOTE: CR 7897, Transmittal (TR) 2552, issued September 24, 2012,
implemented the initial NCD for TAVR, effective May 1, 2012. CR 8168, TR 2628, issued
January 7, 2013, implemented replacement coding to TAVR effective January 1, 2013. CR
8255, TR 2737, issued July 11, 2013, implemented clinical trial number reporting effective
July 1, 2013. CR 8537, TR 2827, issued November 29, 2013, implemented replacement CPT
coding effective January 1, 2013.
290.1 – Coding Requirements for TAVR Furnished on or After May 1,
2012, through December 31, 2012
(Rev. 10179, Issued: 06-10-20, Effective: 06-21-19, Implementation: 06-12-20)
The following are the applicable Current Procedural Terminology (CPT) codes for TAVR:
0256T: Implantation of catheter-delivered prosthetic aortic heart valve; endovascular
approach
0257T: Implantation of catheter-delivered prosthetic aortic heart valve; open thoracic
approach (eg, transapical, transventricular)
0258T: Transthoracic cardiac exposure (i.e. sternotomy, thoracotomy, subxiphoid) for
catheter-delivered aortic valve replacement; without cardiopulmonary bypass
0259T: Transthoracic cardiac exposure (i.e. sternotomy, thoracotomy, subxiphoid) for
catheter-delivered aortic valve replacement; with cardiopulmonary bypass
The following are the International Classification of Diseases (ICD)-9 procedure codes
applicable for TAVR:
35.05: Endovascular replacement of aortic valve
35.06: Transapical replacement of aortic valve
The following are the ICD-10 procedure codes applicable for TAVR:
35.05: 02RF37Z, 02RF38Z. 02RF3JZ, 02RF3KZ
35.06: 02RF37H, 02RF38H, 02RF3JH, 02RF3KH
290.1.1 - Coding Requirements for TAVR Services Furnished on or After
January 1, 2013
(Rev. 10179, Issued: 06-10-20, Effective: 06-21-19, Implementation: 06-12-20)
Beginning January 1, 2013, the following are the applicable CPT codes for TAVR:

33361 Transcatheter aortic valve replacement (TAVR/TAVI) with prosthetic valve;
percutaneous femoral artery approach
33362 Transcatheter aortic valve replacement (TAVR/TAVI) with prosthetic valve; open
femoral approach
33363 Transcatheter aortic valve replacement (TAVR/TAVI) with prosthetic valve; open
axillary artery approach
33364 Transcatheter aortic valve replacement (TAVR/TAVI) with prosthetic valve; open iliac
artery approach
33365 Transcatheter aortic valve replacement (TAVR/TAVI) with prosthetic valve;
transaortic approach (e.g., median sternotomy, mediastinotomy)
0381T Transcatheter aortic valve replacement (TAVR/TAVI) with prosthetic valve;
transapical approach (e.g., left thoracotomy)
Beginning January 1, 2014, temporary CPT code 0318T above is retired. TAVR claims with
dates of service on and after January 1, 2014, shall instead use permanent CPT code 33366.
290.2 - Claims Processing Requirements for TAVR Services on Professional
Claims
(Rev. 10179, Issued: 06-10-20, Effective: 06-21-19, Implementation: 06-12-20)
Place of Service (POS) Professional Claims
Effective for claims with dates of service on and after May 1, 2012, place of service (POS)
code 21 shall be used for TAVR services. All other POS codes shall be denied.
The following messages shall be used when Medicare contractors deny TAVR claims for
POS:
Claim Adjustment Reason Code (CARC) 58: “Treatment was deemed by the payer to have
been rendered in an inappropriate or invalid place of service. NOTE: Refer to the 835
Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if
present.”
Remittance advice remark code (RARC) N428: “Not covered when performed in this place of
service.” Beginning January 2, 2020, contractors shall no longer report RARC N428 for
claims denied for invalid POS.
Medicare Summary Notice (MSN) 21.25: “This service was denied because Medicare only
covers this service in certain settings.”
Spanish Version: “El servicio fue denegado porque Medicare solamente lo cubre en ciertas
situaciones."
Professional Claims Modifier -62
For TAVR claims with dates of service on or after July 1, 2013, contractors shall pay claim
lines with 33361, 33362, 33363, 33364, 33365 & 0318T only when billed with modifier -62.
Claim lines billed without modifier -62 shall be returned as unprocessable.
Beginning January 1, 2014, temporary CPT code 0318T above is retired. TAVR claims with

dates of service on and after January 1, 2014 shall instead use permanent CPT code 33366.
The following messages shall be used when Medicare contractors return TAVR claims billed
without modifier -62 as unprocessable:
CARC 4: “The procedure code is inconsistent with the modifier used or a required modifier is
missing. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF), if present.”
RARC N29: “Missing documentation/orders/notes/summary/report/chart.” Beginning January
2, 2020, contractors shall no longer report RARC N29 on remittance for claims billed without
modifier -62 and returned as unprocessable.
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
Professional Claims Modifier -Q0
For claims with dates of service on or after January 1 , 2013, contractors shall pay TAVR
claim lines for 33361, 33362, 33363, 33364, 33365 & 0318T when billed with modifier-Q0.
Claim lines billed without modifier -Q0 shall be returned as unprocessable.
Beginning January 1, 2014, temporary CPT code 0318T above is retired. TAVR claims with
dates of service on and after January 1, 2014, shall instead use permanent CPT code 33366.
The following messages shall be used when Medicare contractors return TAVR claims billed
without modifier -Q0 as unprocessable:
CARC 4: “The procedure code is inconsistent with the modifier used or a required modifier is
missing. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service
Payment Information REF), if present.”
RARC N29: “Missing documentation/orders/notes/summary/report/chart.” Beginning January
2, 2020, contractors shall no longer report RARC N29 on remittance for claims billed without
modifier –Q0 and returned as unprocessable.
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
Diagnosis Coding
For claims with dates of service on or after July 1, 2013, contractors shall pay TAVR claim
lines for 33361, 33362, 33363, 33364, 33365 & 0318T when billed with diagnosis code
V70.7 (ICD-10 Z00.6). Claim lines billed without diagnosis code V70.7 (ICD-10 Z00.6)
shall be returned as unprocessable.
Beginning January 1, 2014, temporary CPT code 0318T above is retired. TAVR claims with
dates of service on and after January 1, 2014 shall instead use permanent CPT code 33366.
The following messages shall be used when Medicare contractors return TAVR claims billed
without diagnosis code V70.7 (ICD-10 Z00.6) as unprocessable:
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either the NCPDP Reject Reason

Code, or Remittance Advice Remark Code that is not an ALERT).”
RARC M76: “Missing/incomplete/invalid diagnosis or condition”
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
Group Code – Contractual Obligation (CO): Beginning January 2, 2020, contractors shall no
longer report Group Code CO on remittances for claims billed without ICD-10 dx Z00.6 and
returned as unprocessable.
MSN 16.77: This service/item was not covered because it was not provided as part of a
qualifying trial/study. Spanish version: Este servicio/articulo no fue cubierto porque no estaba
incluido como parte de un ensavo clinic/studio calificado. Beginning January 2, 2020,
contractors shall no longer report MSN 16.77 on remittances for claims billed without ICD-10
diagnosis Z00.6 and returned as unprocessable.
Professional Claims 8-digit ClinicalTrials.gov Identifier Number
For claims with dates of service on or after July 1, 2013, contractors shall pay TAVR claim
lines for 33361, 33362, 33363, 33364, 33365 & 0318T when billed with the numeric, 8-digit
clinicaltrials.gov identifier number preceded by the two alpha characters “CT” when placed in
Field 19 of paper Form CMS-1500, or when entered without the “CT” prefix in the electronic
837P in Loop 2300REF02(REF01=P4). Claim lines billed without an 8-digit clinicaltrials.gov
identifier number shall be returned as unprocessable.
Beginning January 1, 2014, temporary CPT code 0318T above is retired. TAVR claims with
dates of service on and after January 1, 2014 shall instead use permanent CPT code 33366.
The following messages shall be used when Medicare contractors return TAVR claims billed
without an 8-digit clinicaltrials.gov identifier number as unprocessable:
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one
Remark Code must be provided (may be comprised of either NCPDP Reject Reason Code, or
Remittance Advice Remark Code that is not an ALERT).”
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption number for
FDA-approved clinical trial services.”
RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal
rights are afforded because the claim is unprocessable. Please submit a new claim with the
complete/correct information.”
NOTE: Clinicaltrials.gov identifier numbers for TAVR are listed on our website:
(http://www.cms.gov/Medicare/Coverage/Coverage-with-Evidence-
Development/Transcatheter-Aortic-Valve-Replacement-TAVR-.html)
290.3 - Claims Processing Requirements for TAVR Services on Inpatient
Hospital Claims
(Rev. 10179, Issued: 06-10-20, Effective: 06-21-19, Implementation: 06-12-20)
Inpatient hospitals shall bill for TAVR on an 11X TOB effective for discharges on or after
May 1, 2012. Refer to Section 69 of this chapter for further guidance on billing under CED.
Inpatient hospital discharges for TAVR shall be covered when billed with:
• ICD-9 V70.7 through September 30, 2015, ICD-10 Z00.6 for dates of service on or after
October 1, 2015. and Condition Code 30.
• An 8-digit clinicaltrials.gov identifier number listed on the CMS website (effective July 1,
2013)
Inpatient hospital discharges for TAVR shall be rejected when billed without:
• ICD-9 V70.7 through September 30, 2015, ICD-10 Z00.6 for dates of service on or after
October 1, 2015, and Condition Code 30.
• An 8-digit clinicaltrials.gov identifier number listed on the CMS website (effective July 1,
2013)
Claims billed by hospitals not participating in the trial/registry shall be rejected with the
following messages:
CARC 50: These are non-covered services because this is not deemed a “medical necessity”
by the payer.
RARC N386: This decision was based on a National Coverage Determination (NCD). An
NCD provides a coverage determination as to whether a particular item or service is covered.
A copy of this policy is available at http://www.cms.hhs.gov/mcd/search.asp. If you do not
have web access, you may contact the contractor to request a copy of the NCD.
Group Code:Contractual Obligation (CO)
MSN 16.77: This service/item was not covered because it was not provided as part of a
qualifying trial/study. Spanish version: Este servicio/artículo no fue cubierto porque no estaba
incluido como parte de un ensayo clínico/estudio calificado.
290.4 - Claims Processing Requirements for TAVR Services for Medicare
Advantage (MA) Plan Participants
(Rev. 3898, Issued: 10-27-17; Effective: 04-01- 15, Implementation: 04-02-18)
MA plans are responsible for payment of TAVR services for MA plan participants. Medicare
coverage for TAVR is not included under section 310.1 of the NCD Manual (Routine Costs in
Clinical Trials).
300 – Billing Requirements for Ocular Photodynamic Therapy (OPT) with
Verteporfin
(Rev. 2728, Issued: 06-14-13-Effective: 04-03-13, Implementation: 07-16-13)
Ocular Photodynamic Therapy (OPT) is used in the treatment of ophthalmologic diseases;
specifically, for age-related macular degeneration (AMD), a common eye disease among the
elderly. OPT involves the infusion of an intravenous photosensitizing drug called Verteporfin,
followed by exposure to a laser. For complete Medical coverage guidelines, see National
Coverage Determinations (NCD) Manual (Pub 100-03) § 80.2 through 80.3.1.
300.1 - Coding Requirements for OPT with Verteporfin
(Rev. 2728, Issued: 06-14-13, Effective: 04-03-13, Implementation: 07-16-13)
The following are applicable Current Procedural Terminology (CPT) codes for OPT with
Verteporfin:

67221- Destruction of localized lesion of choroid (e.g. choroidal neovascularization);
photodynamic therapy (includes intravenous infusion)
67225- Destruction of localized lesion of choroid (e.g. choroidal neovascularization);
photodynamic therapy, second eye, at single session (List separately in addition to code for
primary eye treatment)
The following are applicable Healthcare Common Procedure Coding System (HCPCS) code
for OPT with Verteporfin:
J3396- Injection, Verteporfin, 0.1 mg
300.2 - Claims Processing Requirements for OPT with Verteporfin Services
on Professional Claims and Outpatient Facility Claims
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
OPT with Verteporfin is a covered service when billed with the below ICD-10-CM
codes
Nationally Covered ICD-10-CM codes
H35.321
0
Exudative age-related macular degeneration, right eye, stage unspecified
H35.321
1
Exudative age-related macular degeneration, right eye, with active choroidal
neovascularization
H35.321
2
Exudative age-related macular degeneration, right eye, with inactive choroidal
neovascularization
H35.321
3
Exudative age-related macular degeneration, right eye, with inactive scar
H35.322
0
Exudative age-related macular degeneration, left eye, stage unspecified
H35.322
1
Exudative age-related macular degeneration, left eye, with active choroidal
neovascularization
H35.322
2
Exudative age-related macular degeneration, left eye, with inactive choroidal
neovascularization
H35.322
3
Exudative age-related macular degeneration, left eye, with inactive scar
H35.323
0
Exudative age-related macular degeneration, bilateral, stage unspecified
H35.323
1
Exudative age-related macular degeneration, bilateral, with active choroidal
neovascularization
H35.323
2
Exudative age-related macular degeneration, bilateral, with inactive choroidal
neovascularization
H35.323
3
Exudative age-related macular degeneration, bilateral, with inactive scar
ICD-10- Codes for OPT with Verteporfin for other ocular indications are
eligible for local coverage determinations through individual contractor
discretion.

B39.4
Histocapsulati, unspecified
(Translates to combination of both B39.4 & H32)
B39.5
Histoplasmosis duboisii
(Requires H32 coverage)
B39.9
Histoplasmosis, unspecified
(Requires H32 coverage)
H32
Chorioretinal disorders in diseases classified elsewhere
(Requires B39.4 coverage)
H44.2A1
Degenerative myopia with choroidal neovascularization,
right eye
H44.2A2
Degenerative myopia with choroidal neovascularization,
left eye
H44.2A3
Degenerative myopia with choroidal neovascularization,
bilateral eye
H44.2B1
Degenerative myopia with macular hole, right eye
H44.2B2
Degenerative myopia with macular hole, left eye
H44.2B3
Degenerative myopia with macular hole, bilateral eye
H44.2C1
Degenerative myopia with retinal detachment, right eye
H44.2C2
Degenerative myopia with retinal detachment, left eye
H44.2C3
Degenerative myopia with retinal detachment, bilateral
eye
H44.2D1
Degenerative myopia with foveoschisis, right eye
H44.2D2
Degenerative myopia with foveoschisis, left eye
H44.2D3
Degenerative myopia with foveoschisis, bilateral eye
H44.2E1
Degenerative myopia with other maculopathy, right eye
H44.2E2
Degenerative myopia with other maculopathy, left eye
H44.2E3
Degenerative myopia with other maculopathy, bilateral
eye
H44.21
Degenerative Myopia, right eye
H44.22
Degenerative Myopia, left eye
H44.23
Degenerative Myopia, bilateral
H35.711
Central serous chorioretinopathy, right eye
H35.712
Central serous chorioretinopathy, left eye
H35.713
Central serous chorioretinopathy, bilateral
Coverage is denied when billed with the below Nationally Non-Covered ICD-10-CM
codes
Nationally Non-Covered ICD-10-CM codes:
H35.30
Unspecified macular degeneration
H35.311
0
Nonexudative age-related macular degeneration, right eye, stage unspecified
H35.311
1
Nonexudative age-related macular degeneration, right eye, early dry stage
H35.311
2
Nonexudative age-related macular degeneration, right eye, intermediate dry
stage
H35.311
3
Nonexudative age-related macular degeneration, right eye, advanced atrophic
without subfoveal involvement
H35.311
4
Nonexudative age-related macular degeneration, right eye, advanced atrophic
with subfoveal involvement
H35.312
0
Nonexudative age-related macular degeneration, left eye, stage unspecified

H35.312
1
Nonexudative age-related macular degeneration, left eye, early dry stage
H35.312
2
Nonexudative age-related macular degeneration, left eye, intermediate dry
stage
H35.312
3
Nonexudative age-related macular degeneration, left eye, advanced atrophic
without subfoveal involvement
H35.312
4
Nonexudative age-related macular degeneration, left eye, advanced atrophic
with subfoveal involvement
H35.313
0
Nonexudative age-related macular degeneration, bilateral, stage unspecified
H35.313
1
Nonexudative age-related macular degeneration, bilateral, early dry stage
H35.313
2
Nonexudative age-related macular degeneration, bilateral, intermediate dry
stage
H35.313
3
Nonexudative age-related macular degeneration, bilateral, advanced atrophic
without subfoveal involvement
H35.313
4
Nonexudative age-related macular degeneration, bilateral, advanced atrophic
with subfoveal involvement
Payment for OPT service (CPT code 67221/67225) must be billed on the same claim as the
drug (J3396) for the same date of service.
Claims for OPT with Verteporfin for dates of service prior to April 3, 2013 are covered
at the initial visit as determined by a fluorescein angiogram (FA) CPT code 92235 .
Subsequent follow-up visits also require a FA prior to treatment.
For claims with dates of service on or after April 3, 2013, contractors shall accept and
process claims for subsequent follow-up visits with either a FA, CPT code 92235, or
optical coherence tomography (OCT), CPT codes 92133 or 92134, prior to treatment.
Regardless of the date of service of the claim, the FA or OCT is not required to be
submitted on the claim for OPT and can be maintained in the patient’s file for audit
purposes.
300.3 - Claims Processing Requirements for OPT with Verteporfin Services
on Inpatient Facility Claims
(Rev. 11021; Issued: 10-01-21; Effective: 10-29-21; Implementation: 10-29-21)
Inpatient facilities shall report ICD-10-CM codes H35.3210-H35.3233 (Exudative Age-
related Macular Degeneration) and ICD-10-PCS codes 085E3ZZ (Destruction of Right
Retina, Percutaneous Approach) and 085F3ZZ (Destruction of Left Retina, Percutaneous
Approach)
300.4 - Medicare Summary Notice (MSN) and Remittance Advice (RA)
Messages
(Rev. 2728, Issued: 06-14-13, Effective: 04-03-13, Implementation: 07-16-13)
The following message shall be used to notify beneficiaries and providers of denial situations
that may occur:
MSN 14.9: “Medicare cannot pay for this service for the diagnosis shown on the claim.”
(English version) or “Medicare no puede pagar por este servicio debido al diagnostic indicado
en la reclamacion.” (Spanish Version)
Claims Adjustment Reason Code B22: “This payment is adjusted based on the diagnosis.”
310 - Transesophageal Doppler Used for Cardiac Monitoring
(Rev. 2743, Issued: 07-25-13, Effective: 07-01-01-13, Implementation, 08-26-13)
Effective May 17, 2007, Transesophageal Doppler used for cardiac monitoring is covered for
ventilated patients in the ICU and operative patients with a need for intra-operative fluid
optimization was deemed reasonable and necessary. See National Coverage Determinations
Manual (Pub. 100-03) §220.5, for complete coverage guidelines.
A new Healthcare Common Procedure Coding System (HCPCS) code, G9157,
Transesophageal Doppler used for cardiac monitoring, will be made effective for use for dates
of service on or after January 1, 2013.
310.1 - Coding Requirements for Transesophageal Doppler Cardiac
Monitoring
Furnished Before January 1, 2013
(Rev. 2743, Issued: 07-25-13, Effective: 07-01-01-13, Implementation, 08-26-13)
Prior to January 1, 2013, the applicable HCPCS code for Transesophageal Doppler cardiac
monitoring is:
HCPCS 76999 (billed with modifier -26) when performed in a hospital setting for ventilated
patients in the ICU or for operative patients with a need for intra-operative fluid optimization.
If globally billed using code 76999, it shall be returned as unprocessable to the provider using
a claim adjustment reason code (CARC) such as:
CARC 58: “Treatment was deemed by the payer to have been rendered in an
inappropriate or invalid place of service. Note: Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF), if present.”
HCPCS 76999 (billed with modifier -TC) shall be denied when performed in a hospital
setting for ventilated patients in the ICU or for operative patients with a need for intra-
operative fluid optimization with a message such as:
CARC 58: “Treatment was deemed by the payer to have been rendered in an
inappropriate or invalid place of service. Note: Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF), if present.”
RARC M77: “Missing/incomplete/invalid place of service.”
MSN 17.9: “Medicare (Part A/Part B) pays for this service. The provider must bill the
correct Medicare contractor.” (English version) or “Este servicio es pagado por
Medicare (Parte A/Parte B). El proveedor debe enviar la facture al contratista de
Medicare correcto.”(Spanish version).
HCPCS 76999 (billed globally or with -26 or -TC) when performed in an ASC setting for
operative patients with a need for intra-operative fluid optimization, ultrasound diagnostic
procedures are covered when performed by an entity other than the ASC.
310.2 - Coding Requirements for Transesophageal Doppler Cardiac
Monitoring
Furnished On or After January 1, 2013
(Rev. 2743, Issued: 07-25-13, Effective: 07-01-01-13, Implementation, 08-26-13)
After January 1, 2013, the applicable HCPCS code for Transesophageal Doppler cardiac
monitoring is:
HCPCS G9157: Transesophageal Doppler used for cardiac monitoring
Contractors shall allow HCPCS G9157 to be billed when services are provided in POS 21 for
ventilated patients in the ICU or for operative patients with a need for intra-operative fluid
optimization.
Contractors shall deny HCPCS 76999 when billed for Esophageal Doppler for ventilated
patients in the ICU or for operative patients with a need for intra-operative fluid optimization
using the following messages:
CARC 189: “’Not otherwise classified’ or ‘unlisted’ procedure code (CPT/HCPCS)
was billed when there is a specific procedure code for this procedure/service.”
RARC M20: “Missing/incomplete/invalid HCPCS.”
MSN 16.13: “The code(s) your provider used is/are not valid for the date of service
billed.” (English version) or “El/los código(s) que usó su proveedor no es/son válido(s) en la
fecha de servicio facturada.” (Spanish version).
Group Code: Contractual Obligation (CO)
310.3 - Correct Place of Service (POS) Code for Transesophageal Doppler
Cardiac Monitoring
Services on Professional Claims
(Rev. 2743, Issued: 07-25-13, Effective: 07-01-01-13, Implementation, 08-26-13)
Contractors shall pay for Transesophageal Doppler cardiac monitoring, G9157, only when
services are provided at POS 21.
Contractors shall deny HCPCS G9157 when billed globally in any POS other than 21 for
ventilated patients in the ICU or for operative patients with a need for intra-operative fluid
optimization using the following messages:
CARC 58: “Treatment was deemed by the payer to have been rendered in an inappropriate or
invalid place of service. Note: Refer to the 835 Healthcare Policy Identification Segment
(loop 2110 Service Payment Information REF), if present.
MSN 16.2: This service cannot be paid when provided in this location/facility.
Group Code: CO
320 - Artificial Hearts and Related Devices
(Rev.10837; Issued: 06-11-21; Effective: 12-01-20; Implementation: 07-27-21)
Effective for claims with dates of service on or after December 1, 2020, as a result of a
reconsideration of National Coverage Determination (NCD) 20.9 of the Medicare NCD
Manual, coverage determinations for artificial hearts and related devices shall be made by the
Medicare Administrative Contractors.
320.1 – Coding Requirements for Artificial Hearts Furnished Before May 1,
2008
(Rev. 3054, Issued: 08-29-14, Effective: 10-30- 13, Implementation: 09-30-14)

Effective for discharges before May 1, 2008, Medicare does not cover the use of artificial
hearts, either as a permanent replacement for a human heart or as a temporary life-support
system until a human heart becomes available for transplant (often referred to a "bridge to
transplant").
320.2 – Coding Requirements for Artificial Hearts Furnished On or After
May 1, 2008
(Rev. 3054, Issued: 08-29-14, Effective: 10-30- 13, Implementation: 09-30-14)
Effective for discharges on or after May 1, 2008, the use of artificial hearts will be covered by
Medicare under Coverage with Evidence Development (CED) when beneficiaries are enrolled
in a clinical study that meets all of the criteria listed in IOM Pub. 100-03, Medicare NCD
Manual, section 20.9.
Claims Coding
For claims with dates of service on or after May 1, 2008, artificial hearts in the context of an
approved clinical study for a Category A IDE, refer to section 69 in this manual for more
detail on CED billing. Appropriate ICD-10 diagnosis and procedure codes are included
below:
ICD-10
Diagnosis
Code
Definition
Discharges
Effective
I09.81
Rheumatic heart failure
On or After
ICD-10
Implementation
I11.0
Hypertensive heart disease with heart failure
I13.0
Hypertensive heart and chronic kidney disease with heart
failure and stage 1 through stage 4 chronic kidney disease, or
unspecified chronic kidney disease
I13.2
Hypertensive heart and chronic kidney disease with heart
failure and with stage 5 chronic kidney disease, or end stage
renal disease
I20.0
Unstable angina
I21.01
ST elevation (STEMI) myocardial infarction involving left
main coronary artery
I21.02
ST elevation (STEMI) myocardial infarction involving left
anterior descending coronary artery
I21.09
ST elevation (STEMI) myocardial infarction involving other
coronary artery of anterior wall
I21.11
ST elevation (STEMI) myocardial infarction involving right
coronary artery
I21.19
ST elevation (STEMI) myocardial infarction involving other
coronary artery of inferior wall
I21.21
ST elevation (STEMI) myocardial infarction involving left
circumflex coronary artery
I21.29
ST elevation (STEMI) myocardial infarction involving other
sites
I21.3
ST elevation (STEMI) myocardial infarction of unspecified
site
I21.4
Non-ST elevation (NSTEMI) myocardial infarction
I22.0
Subsequent ST elevation (STEMI) myocardial infarction of
anterior wall
I22.1
Subsequent ST elevation (STEMI) myocardial infarction of
inferior wall
I22.2
Subsequent non-ST elevation (NSTEMI) myocardial
infarction

I22.8
Subsequent ST elevation (STEMI) myocardial infarction of
other sites
I22.9
Subsequent ST elevation (STEMI) myocardial infarction of
unspecified site
I24.0
Acute coronary thrombosis not resulting in myocardial
infarction
I24.1
Dressler's syndrome
I24.8
Other forms of acute ischemic heart disease
I24.9
Acute ischemic heart disease, unspecified
I25.10
Atherosclerotic heart disease of native coronary artery
without angina pectoris
I25.110
Atherosclerotic heart disease of native coronary artery with
unstable angina pectoris
I25.111
Atherosclerotic heart disease of native coronary artery with
angina pectoris with documented spasm
I25.118
Atherosclerotic heart disease of native coronary artery with
other forms of angina pectoris
I25.119
Atherosclerotic heart disease of native coronary artery with
unspecified angina pectoris
I25.5
Ischemic cardiomyopathy
I25.6
Silent myocardial ischemia
I25.700
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with unstable angina pectoris
I25.701
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with angina pectoris with documented spasm
I25.708
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with other forms of angina pectoris
I25.709
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with unspecified angina pectoris
I25.710
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with unstable angina pectoris
I25.711
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with angina pectoris with documented spasm
I25.718
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with other forms of angina pectoris
I25.719
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with unspecified angina pectoris
I25.720
Atherosclerosis of autologous artery coronary artery bypass
graft(s) with unstable angina pectoris
I25.721
Atherosclerosis of autologous artery coronary artery bypass
graft(s) with angina pectoris with documented spasm
I25.728
Atherosclerosis of autologous artery coronary artery bypass
graft(s) with other forms of angina pectoris
I25.729
Atherosclerosis of autologous artery coronary artery bypass
graft(s) with unspecified angina pectoris
I25.730
Atherosclerosis of nonautologous biological coronary artery
bypass graft(s) with unstable angina pectoris
I25.731
Atherosclerosis of nonautologous biological coronary artery
bypass graft(s) with angina pectoris with documented spasm
I25.738
Atherosclerosis of nonautologous biological coronary artery
bypass graft(s) with other forms of angina pectoris
I25.739
Atherosclerosis of nonautologous biological coronary artery
bypass graft(s) with unspecified angina pectoris
I25.750
Atherosclerosis of native coronary artery of transplanted
heart with unstable angina

I25.751
Atherosclerosis of native coronary artery of transplanted
heart with angina pectoris with documented spasm
I25.758
Atherosclerosis of native coronary artery of transplanted
heart with other forms of angina pectoris
I25.759
Atherosclerosis of native coronary artery of transplanted
heart with unspecified angina pectoris
I25.760
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with unstable angina
I25.761
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with angina pectoris with documented
spasm
I25.768
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with other forms of angina pectoris
I25.769
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with unspecified angina pectoris
I25.790
Atherosclerosis of other coronary artery bypass graft(s) with
unstable angina pectoris
I25.791
Atherosclerosis of other coronary artery bypass graft(s) with
angina pectoris with documented spasm
I25.798
Atherosclerosis of other coronary artery bypass graft(s) with
other forms of angina pectoris
I25.799
Atherosclerosis of other coronary artery bypass graft(s) with
unspecified angina pectoris
I25.810
Atherosclerosis of coronary artery bypass graft(s) without
angina pectoris
I25.811
Atherosclerosis of native coronary artery of transplanted
heart without angina pectoris
I25.812
Atherosclerosis of bypass graft of coronary artery of
transplanted heart without angina pectoris
I25.89
Other forms of chronic ischemic heart disease
I25.9
Chronic ischemic heart disease, unspecified
I34.0
Nonrheumatic mitral (valve) insufficiency
I34.1
Nonrheumatic mitral (valve) prolapse
I34.2
Nonrheumatic mitral (valve) stenosis
I34.8
Other nonrheumatic mitral valve disorders
I34.9
Nonrheumatic mitral valve disorder, unspecified
I35.0
Nonrheumatic aortic (valve) stenosis
I35.1
Nonrheumatic aortic (valve) insufficiency
I35.2
Nonrheumatic aortic (valve) stenosis with insufficiency
I35.8
Other nonrheumatic aortic valve disorders
I35.9
Nonrheumatic aortic valve disorder, unspecified
I36.0
Nonrheumatic tricuspid (valve) stenosis
I36.1
Nonrheumatic tricuspid (valve) insufficiency
I36.2
Nonrheumatic tricuspid (valve) stenosis with insufficiency
I36.8
Other nonrheumatic tricuspid valve disorders
I36.9
Nonrheumatic tricuspid valve disorder, unspecified
I37.0
Nonrheumatic pulmonary valve stenosis
I37.1
Nonrheumatic pulmonary valve insufficiency
I37.2
Nonrheumatic pulmonary valve stenosis with insufficiency
I37.8
Other nonrheumatic pulmonary valve disorders
I37.9
Nonrheumatic pulmonary valve disorder, unspecified
I38
Endocarditis, valve unspecified
I39
Endocarditis and heart valve disorders in diseases classified
elsewhere
I42.0
Dilated cardiomyopathy

I42.2
Other hypertrophic cardiomyopathy
I42.3
Endomyocardial (eosinophilic) disease
I42.4
Endocardial fibroelastosis
I42.5
Other restrictive cardiomyopathy
I42.6
Alcoholic cardiomyopathy
I42.7
Cardiomyopathy due to drug and external agent
I42.8
Other cardiomyopathies
I42.9
Cardiomyopathy, unspecified
I43
Cardiomyopathy in diseases classified elsewhere
I46.2
Cardiac arrest due to underlying cardiac condition
I46.8
Cardiac arrest due to other underlying condition
I46.9
Cardiac arrest, cause unspecified
I47.0
Re-entry ventricular arrhythmia
I47.1
Supraventricular tachycardia
I47.2
Ventricular tachycardia
I47.9
Paroxysmal tachycardia, unspecified
I48.0
Atrial fibrillation
I48.1
Atrial flutter
I49.01
Ventricular fibrillation
I49.02
Ventricular flutter
I49.1
Atrial premature depolarization
I49.2
Junctional premature depolarization
I49.3
Ventricular premature depolarization
I49.40
Unspecified premature depolarization
I49.49
Other premature depolarization
I49.5
Sick sinus syndrome
I49.8
Other specified cardiac arrhythmias
I49.9
Cardiac arrhythmia, unspecified
I50.1
Left ventricular failure
I50.20
Unspecified systolic (congestive) heart failure
I50.21
Acute systolic (congestive) heart failure
I50.22
Chronic systolic (congestive) heart failure
I50.23
Acute on chronic systolic (congestive) heart failure
I50.30
Unspecified diastolic (congestive) heart failure
I50.31
Acute diastolic (congestive) heart failure
I50.32
Chronic diastolic (congestive) heart failure
I50.33
Acute on chronic diastolic (congestive) heart failure
I50.40
Unspecified combined systolic (congestive) and diastolic
(congestive) heart failure
I50.41
Acute combined systolic (congestive) and diastolic
(congestive) heart failure
I50.42
Chronic combined systolic (congestive) and diastolic
(congestive) heart failure
I50.43
Acute on chronic combined systolic (congestive) and
diastolic (congestive) heart failure
I50.9
Heart failure, unspecified
I51.4
Myocarditis, unspecified
I51.9
Heart disease, unspecified
I52
Other heart disorders in diseases classified elsewhere
I97.0
Postcardiotomy syndrome
I97.110
Postprocedural cardiac insufficiency following cardiac
surgery
I97.111
Postprocedural cardiac insufficiency following other surgery
I97.120
Postprocedural cardiac arrest following cardiac surgery
I97.121
Postprocedural cardiac arrest following other surgery

I97.130
Postprocedural heart failure following cardiac surgery
I97.131
Postprocedural heart failure following other surgery
I97.190
Other postprocedural cardiac functional disturbances
following cardiac surgery
I97.191
Other postprocedural cardiac functional disturbances
following other surgery
I97.710
Intraoperative cardiac arrest during cardiac surgery
I97.711
Intraoperative cardiac arrest during other surgery
I97.790
Other intraoperative cardiac functional disturbances during
cardiac surgery
I97.791
Other intraoperative cardiac functional disturbances during
other surgery
I97.88
Other intraoperative complications of the circulatory system,
not elsewhere classified
I97.89
Other postprocedural complications and disorders of the
circulatory system, not elsewhere classified
M32.11
Endocarditis in systemic lupus erythematosus
O90.89
Other complications of the puerperium, not elsewhere
classified
Q20.0
Common arterial trunk
Q20.1
Double outlet right ventricle
Q20.2
Double outlet left ventricle
Q20.3
Discordant ventriculoarterial connection
Q20.4
Double inlet ventricle
Q20.5
Discordant atrioventricular connection
Q20.6
Isomerism of atrial appendages
Q20.8
Other congenital malformations of cardiac chambers and
connections
Q20.9
Congenital malformation of cardiac chambers and
connections, unspecified
Q21.0
Ventricular septal defect
Q21.1
Atrial septal defect
Q21.2
Atrioventricular septal defect
Q21.3
Tetralogy of Fallot
Q21.4
Aortopulmonary septal defect
Q21.8
Other congenital malformations of cardiac septa
Q21.9
Congenital malformation of cardiac septum, unspecified
Q22.0
Pulmonary valve atresia
Q22.1
Congenital pulmonary valve stenosis
Q22.2
Congenital pulmonary valve insufficiency
Q22.3
Other congenital malformations of pulmonary valve
Q22.4
Congenital tricuspid stenosis
Q22.5
Ebstein's anomaly
Q22.6
Hypoplastic right heart syndrome
Q22.8
Other congenital malformations of tricuspid valve
Q22.9
Congenital malformation of tricuspid valve, unspecified
Q23.0
Congenital stenosis of aortic valve
Q23.1
Congenital insufficiency of aortic valve
Q23.2
Congenital mitral stenosis
Q23.3
Congenital mitral insufficiency
Q23.4
Hypoplastic left heart syndrome
Q23.8
Other congenital malformations of aortic and mitral valves
Q23.9
Congenital malformation of aortic and mitral valves,
unspecified
Q24.0
Dextrocardia

Q24.1
Levocardia
Q24.2
Cor triatriatum
Q24.3
Pulmonary infundibular stenosis
Q24.4
Congenital subaortic stenosis
Q24.5
Malformation of coronary vessels
Q24.6
Congenital heart block
Q24.8
Other specified congenital malformations of heart
Q24.9
Congenital malformation of heart, unspecified
R00.1
Bradycardia, unspecified
R57.0
Cardiogenic shock
T82.221A
Breakdown (mechanical) of biological heart valve graft,
initial encounter
T82.222A
Displacement of biological heart valve graft, initial
encounter
T82.223A
Leakage of biological heart valve graft, initial encounter
T82.228A
Other mechanical complication of biological heart valve
graft, initial encounter
T82.512A
Breakdown (mechanical) of artificial heart, initial encounter
T82.514A
Breakdown (mechanical) of infusion catheter, initial
encounter
T82.518A
Breakdown (mechanical) of other cardiac and vascular
devices and implants, initial encounter
T82.519A
Breakdown (mechanical) of unspecified cardiac and vascular
devices and implants, initial encounter
T82.522A
Displacement of artificial heart, initial encounter
T82.524A
Displacement of infusion catheter, initial encounter
T82.528A
Displacement of other cardiac and vascular devices and
implants, initial encounter
T82.529A
Displacement of unspecified cardiac and vascular devices
and implants, initial encounter
T82.532A
Leakage of artificial heart, initial encounter
T82.534A
Leakage of infusion catheter, initial encounter
T82.538A
Leakage of other cardiac and vascular devices and implants,
initial encounter
T82.539A
Leakage of unspecified cardiac and vascular devices and
implants, initial encounter
T82.592A
Other mechanical complication of artificial heart, initial
encounter
T82.594A
Other mechanical complication of infusion catheter, initial
encounter
T82.598A
Other mechanical complication of other cardiac and vascular
devices and implants, initial encounter
T82.599A
Other mechanical complication of unspecified cardiac and
vascular devices and implants, initial encounter
T86.20
Unspecified complication of heart transplant
T86.21
Heart transplant rejection
T86.22
Heart transplant failure
T86.23
Heart transplant infection
T86.290
Cardiac allograft vasculopathy
T86.298
Other complications of heart transplant
T86.30
Unspecified complication of heart-lung transplant
T86.31
Heart-lung transplant rejection
T86.32
Heart-lung transplant failure
T86.33
Heart-lung transplant infection
T86.39
Other complications of heart-lung transplant

Z48.21
Encounter for aftercare following heart transplant
Z48.280
Encounter for aftercare following heart-lung transplant
Z94.1
Heart transplant status
Z94.3
Heart and lungs transplant status
Z95.9
Presence of cardiac and vascular implant and graft,
unspecified
Q24.0
Dextrocardia
Q24.1
Levocardia
Q24.2
Cor triatriatum
Q24.3
Pulmonary infundibular stenosis
Q24.4
Congenital subaortic stenosis
Q24.5
Malformation of coronary vessels
Q24.6
Congenital heart block
Q24.8
Other specified congenital malformations of heart
Q24.9
Congenital malformation of heart, unspecified
R00.1
Bradycardia, unspecified
R57.0
Cardiogenic shock
T82.221A
Breakdown (mechanical) of biological heart valve graft,
initial encounter
T82.222A
Displacement of biological heart valve graft, initial
encounter
T82.223A
Leakage of biological heart valve graft, initial encounter
T82.228A
Other mechanical complication of biological heart valve
graft, initial encounter
T82.512A
Breakdown (mechanical) of artificial heart, initial encounter
T82.514A
Breakdown (mechanical) of infusion catheter, initial
encounter
T82.518A
Breakdown (mechanical) of other cardiac and vascular
devices and implants, initial encounter
T82.519A
Breakdown (mechanical) of unspecified cardiac and vascular
devices and implants, initial encounter
T82.522A
Displacement of artificial heart, initial encounter
T82.524A
Displacement of infusion catheter, initial encounter
T82.528A
Displacement of other cardiac and vascular devices and
implants, initial encounter
T82.529A
Displacement of unspecified cardiac and vascular devices
and implants, initial encounter
T82.532A
Leakage of artificial heart, initial encounter
T82.534A
Leakage of infusion catheter, initial encounter
T82.538A
Leakage of other cardiac and vascular devices and implants,
initial encounter
T82.539A
Leakage of unspecified cardiac and vascular devices and
implants, initial encounter
T82.592A
Other mechanical complication of artificial heart, initial
encounter
T82.594A
Other mechanical complication of infusion catheter, initial
encounter
T82.598A
Other mechanical complication of other cardiac and vascular
devices and implants, initial encounter
T82.599A
Other mechanical complication of unspecified cardiac and
vascular devices and implants, initial encounter
T86.20
Unspecified complication of heart transplant
T86.21
Heart transplant rejection
T86.22
Heart transplant failure
T86.23
Heart transplant infection

T86.290
Cardiac allograft vasculopathy
T86.298
Other complications of heart transplant
T86.30
Unspecified complication of heart-lung transplant
T86.31
Heart-lung transplant rejection
T86.32
Heart-lung transplant failure
T86.33
Heart-lung transplant infection
T86.39
Other complications of heart-lung transplant
Z48.21
Encounter for aftercare following heart transplant
Z48.280
Encounter for aftercare following heart-lung transplant
Z94.1
Heart transplant status
Z94.3
Heart and lungs transplant status
Z95.9
Presence of cardiac and vascular implant and graft,
unspecified
ICD-10
Procedure
Code
Definition
Discharges
Effective
02RK0JZ
Replacement of Right Ventricle with Synthetic Substitute,
Open Approach
On or After
ICD-10
Implementation
02RL0JZ
Replacement of Left Ventricle with Synthetic Substitute,
Open Approach
02WA0JZ
Revision of Synthetic Substitute in Heart, Open Approach
NOTE: Total artificial heart is reported with a “cluster” of 2 codes for open replacement with
synthetic substitute of the right and left ventricles- 02RK0JZ + 02RL0JZ
320.3 – Ventricular Assist Devices (VADs)
(Rev.10837; Issued: 06-11-21; Effective: 12-01-20; Implementation: 07-27-21)
Medicare may cover a Ventricular Assist Device (VAD). A VAD is surgically attached to one
or both intact ventricles and is used to assist or augment the ability of a damaged or weakened
native heart to pump blood. Improvement in the performance of the native heart may allow
the device to be removed. Refer to the Internet Only Manual Publication 100-03, National
Coverage Determination (NCD) Manual, section 20.9.1, for coverage criteria.

320.3.1 – Post-cardiotomy
(Rev.10837; Issued: 06-11-21; Effective: 12-01-20; Implementation: 07-27-21)
Post-cardiotomy is the period following open-heart surgery. VADs used for support of blood
circulation post-cardiotomy are covered only if they have received approval from the Food
and Drug Administration (FDA) for that purpose, and the VADs are used according to the
FDA-approved labeling instructions.
320.3.2 – VADs for Short-term or Long-term Mechanical Circulatory
Support
(Rev.10837; Issued: 06-11-21; Effective: 12-01-20; Implementation: 07-27-21)
Effective for claims with dates of service on or after December 1, 2020, Left ventricular assist
devices (LVADs) are covered if they are FDA-approved for short-term (e.g., bridge-to-
recovery and bridge-to-transplant) or long-term (e.g., destination therapy) mechanical
circulatory support for heart failure patients who meet specific clinical criteria outlined in
NCD 20.9.1.
320.3.3 – Other
(Rev. 12396; Issued: 12-07-23; Effective: 01-09-24; Implementation: 01-09-24)
All other indications for the use of VADs not otherwise listed remain non-covered, except in
the context of Category B investigational device exemption clinical trials (42 CFR 405) or as
a routine cost in clinical trials defined under section 310.1 of the NCD Manual.
Claims Coding
Appropriate ICD-10 diagnosis and procedure codes are included below:
ICD-10
Diagnosis
Code
Definition
I09.81
Rheumatic heart failure
I11.0
Hypertensive heart disease with heart failure
I13.0
Hypertensive heart and chronic kidney disease with heart
failure and stage 1
through stage 4 chronic kidney disease,
or unspecified chronic kidney disease
I13.2
Hypertensive heart and chronic kidney disease with heart
failure and with stage 5 chronic kidney disease, or end
stage renal disease
I20.0
Unstable angina
I21.01
ST elevation (STEMI) myocardial infarction involving left
main coronary artery
ST elevation (STEMI) myocardial infarction involving left

I21.02
anterior descending coronary artery
I21.09
ST elevation (STEMI) myocardial infarction involving
other coronary artery of anterior wall
I21.11
ST elevation (STEMI) myocardial infarction involving
right coronary artery
I21.19
ST elevation (STEMI) myocardial infarction involving
other coronary artery of inferior wall
I21.21
ST elevation (STEMI) myocardial infarction involving left
circumflex coronary artery
I21.29
ST elevation (STEMI) myocardial infarction involving
other sites
I21.3
ST elevation (STEMI) myocardial infarction of
unspecified site
I21.4
Non-ST elevation (NSTEMI) myocardial infarction
I22.0
Subsequent ST elevation (STEMI) myocardial infarction
of anterior wall
I22.1
Subsequent ST elevation (STEMI) myocardial infarction
of inferior wall
I22.2
Subsequent non-ST elevation (NSTEMI) myocardial
infarction
I22.8
Subsequent ST elevation (STEMI) myocardial infarction
of other sites
I22.9
Subsequent ST elevation (STEMI) myocardial infarction of
unspecified site
I24.0
Acute coronary thrombosis not resulting in myocardial
infarction
I24.1
Dressler's syndrome
I24.81
Acute coronary microvascular dysfunction Effective 10/1/23
I24.89
Other forms of acute ischemic heart disease Effective
10/1/23
I24.9
Acute ischemic heart disease, unspecified
I25.10
Atherosclerotic heart disease of native coronary artery
without angina pectoris
Atherosclerotic heart disease of native coronary artery
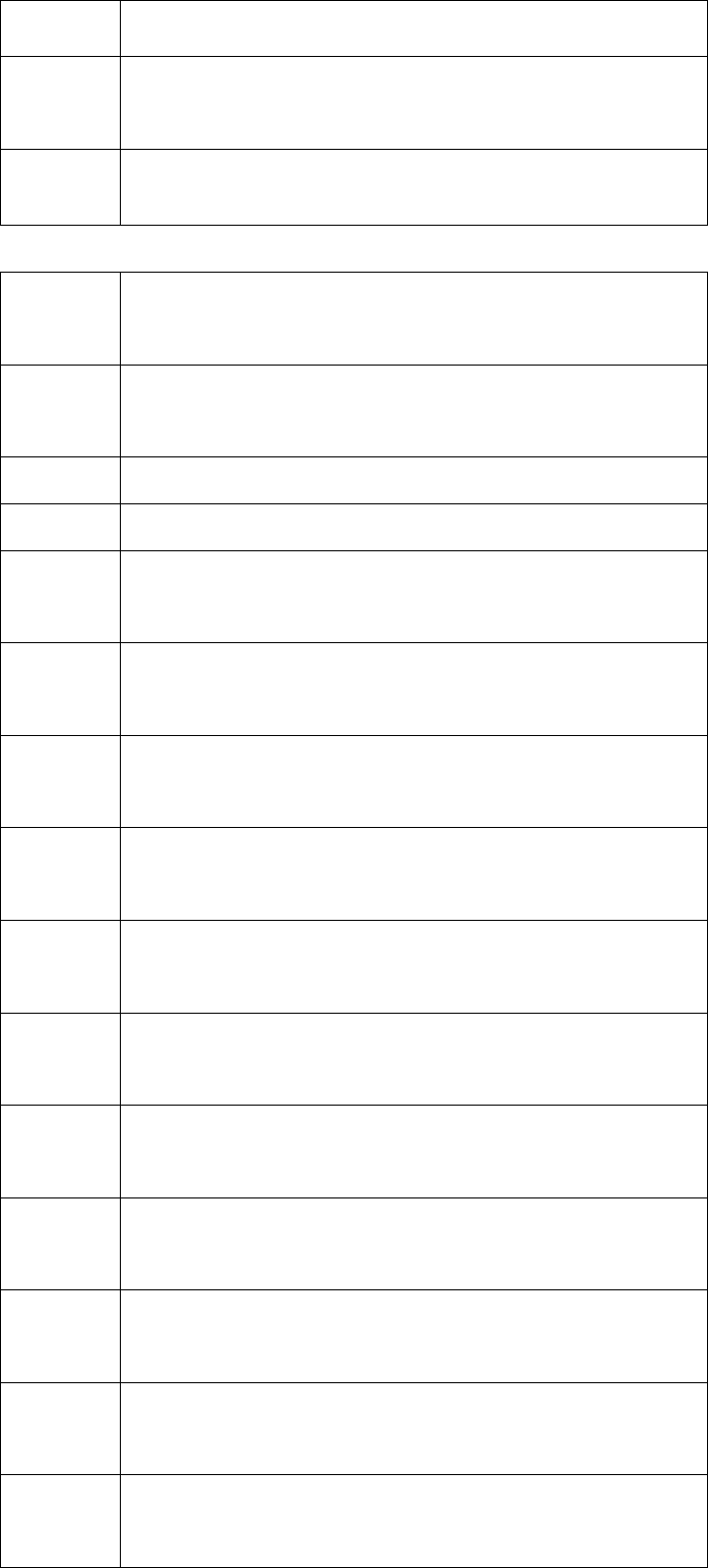
I25.110
with unstable angina pectoris
I25.111
Atherosclerotic heart disease of native coronary artery with
angina pectoris with documented
spasm
I25.112
Atherosclerotic heart disease of native coronary artery with
refractory angina pectoris
I25.118
Atherosclerotic heart disease of native coronary artery with
other forms of angina pectoris
I25.119
Atherosclerotic heart disease of native coronary artery
with unspecified angina pectoris
I25.5
Ischemic cardiomyopathy
I25.6
Silent myocardial ischemia
I25.700
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with unstable angina
pectoris
I25.701
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with angina pectoris with documented spasm
I25.708
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with other forms of angina pectoris
I25.709
Atherosclerosis of coronary artery bypass graft(s),
unspecified, with unspecified angina pectoris
I25.710
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with unstable angina pectoris
I25.711
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with angina pectoris with documented spasm
I25.718
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with other forms of angina pectoris
I25.719
Atherosclerosis of autologous vein coronary artery bypass
graft(s) with unspecified angina pectoris
I25.720
Atherosclerosis of autologous artery coronary artery
bypass graft(s) with unstable angina pectoris
I25.721
Atherosclerosis of autologous artery coronary artery
bypass graft(s) with angina pectoris with documented spasm
I25.728
Atherosclerosis of autologous artery coronary artery
bypass graft(s) with other forms of angina pectoris

I25.729
Atherosclerosis of autologous artery coronary artery
bypass graft(s) with unspecified angina pectoris
I25.730
Atherosclerosis of nonautologous biological coronary artery
bypass graft(s) with unstable angina pectoris
I25.731
Atherosclerosis of nonautologous biological coronary artery
bypass graft(s) with angina pectoris with
documented spasm
I25.738
Atherosclerosis of nonautologous biological coronary
artery bypass graft(s) with other forms of angina pectoris
I25.739
Atherosclerosis of nonautologous biological coronary
artery bypass graft(s) with unspecified angina pectoris
I25.750
Atherosclerosis of native coronary artery of transplanted
heart with unstable angina
I25.751
Atherosclerosis of native coronary artery of transplanted
heart with angina pectoris with documented spasm
I25.758
Atherosclerosis of native coronary artery of transplanted
heart with other forms of angina pectoris
I25.759
Atherosclerosis of native coronary artery of transplanted
heart with unspecified angina pectoris
I25.760
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with unstable angina
I25.761
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with angina
pectoris with documented
spasm
I25.768
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with other forms of angina pectoris
I25.769
Atherosclerosis of bypass graft of coronary artery of
transplanted heart with unspecified angina pectoris
I25.790
Atherosclerosis of other coronary artery bypass graft(s)
with unstable angina pectoris
I25.791
Atherosclerosis of other coronary artery bypass graft(s)
with angina pectoris with documented spasm
Atherosclerosis of other coronary artery bypass graft(s)

I25.798
with other forms of angina pectoris
I25.799
Atherosclerosis of other coronary artery bypass graft(s)
with unspecified angina pectoris
I25.810
Atherosclerosis of coronary artery bypass graft(s) without
angina pectoris
I25.811
Atherosclerosis of native coronary artery of transplanted
heart without angina pectoris
I25.812
Atherosclerosis of bypass graft of coronary artery of
transplanted heart without angina pectoris
I25.89
Other forms of chronic ischemic heart disease
I25.9
Chronic ischemic heart disease, unspecified
I34.0
Nonrheumatic mitral (valve) insufficiency
I34.1
Nonrheumatic mitral (valve) prolapse
I34.2
Nonrheumatic mitral (valve) stenosis
I34.8
Other nonrheumatic mitral valve disorders
I34.9
Nonrheumatic mitral valve disorder, unspecified
I35.0
Nonrheumatic aortic (valve) stenosis
I35.1
Nonrheumatic aortic (valve) insufficiency
I35.2
Nonrheumatic aortic (valve) stenosis with insufficiency
I35.8
Other nonrheumatic aortic valve disorders
I35.9
Nonrheumatic aortic valve disorder, unspecified
I36.0
Nonrheumatic tricuspid (valve) stenosis
I36.1
Nonrheumatic tricuspid (valve) insufficiency
I36.2
Nonrheumatic tricuspid (valve) stenosis with insufficiency
I36.8
Other nonrheumatic tricuspid valve disorders
I36.9
Nonrheumatic tricuspid valve disorder, unspecified
I37.0
Nonrheumatic pulmonary valve stenosis
I37.1
Nonrheumatic pulmonary valve insufficiency
I37.2
Nonrheumatic pulmonary valve stenosis with
insufficiency
I37.8
Other nonrheumatic pulmonary valve disorders
I37.9
Nonrheumatic pulmonary valve disorder, unspecified

I38
Endocarditis, valve unspecified
I39
Endocarditis and heart valve disorders in diseases
classified elsewhere
I42.0
Dilated cardiomyopathy
I42.2
Other hypertrophic cardiomyopathy
I42.3
Endomyocardial (eosinophilic) disease
I42.4
Endocardial fibroelastosis
I42.5
Other restrictive cardiomyopathy
I42.6
Alcoholic cardiomyopathy
I42.7
Cardiomyopathy due to drug and external agent
I42.8
Other cardiomyopathies
I42.9
Cardiomyopathy, unspecified
I43
Cardiomyopathy in diseases classified elsewhere
I46.2
Cardiac arrest due to underlying cardiac condition
I46.8
Cardiac arrest due to other underlying condition
I46.9
Cardiac arrest, cause unspecified
I47.0
Re-entry ventricular arrhythmia
I47.2
Ventricular tachycardia
I47.9
Paroxysmal tachycardia, unspecified
I47.10
Supraventricular tachycardia, unspecified Effective
10/1/23
I47.11
Inappropriate sinus tachycardia, so stated Effective
10/1/23
I47.19
Other supraventricular tachycardia Effective 10/1/23
I48.0
Atrial fibrillation
I48.11
Longstanding persistent atrial fibrillation
I48.19
Other persistent atrial fibrillation
I49.01
Ventricular fibrillation
I49.02
Ventricular flutter
I49.1
Atrial premature depolarization
I49.2
Junctional premature depolarization
I49.3
Ventricular premature depolarization
I49.40
Unspecified premature depolarization
I49.49
Other premature depolarization

I49.5
Sick sinus syndrome
I49.8
Other specified cardiac arrhythmias
I49.9
Cardiac arrhythmia, unspecified
I50.1
Left ventricular failure
I50.20
Unspecified systolic (congestive) heart failure
I50.21
Acute systolic (congestive) heart failure
I50.22
Chronic systolic (congestive) heart failure
I50.23
Acute on chronic systolic (congestive) heart failure
I50.30
Unspecified diastolic (congestive) heart failure
I50.31
Acute diastolic (congestive) heart failure
I50.32
Chronic diastolic (congestive) heart failure
I50.33
Acute on chronic diastolic (congestive) heart failure
I50.40
Unspecified combined systolic (congestive) and diastolic
(congestive) heart failure
I50.41
Acute combined systolic (congestive) and diastolic
(congestive) heart failure
I50.42
Chronic combined systolic (congestive) and diastolic
(congestive) heart failure
I50.43
Acute on chronic combined systolic (congestive) and
diastolic (congestive) heart failure
I50.84
End-stage heart failure
I50.9
Heart failure, unspecified
I51.4
Myocarditis, unspecified
I51.9
Heart disease, unspecified
I52
Other heart disorders in diseases classified elsewhere
I97.0
Postcardiotomy syndrome
I97.110
Postprocedural cardiac insufficiency following cardiac
surgery
I97.111
Postprocedural cardiac insufficiency following other
surgery
I97.120
Postprocedural cardiac arrest following cardiac surgery
I97.121
Postprocedural cardiac arrest following other surgery

I97.130
Postprocedural heart failure following cardiac surgery
I97.131
Postprocedural heart failure following other surgery
I97.190
Other postprocedural cardiac functional disturbances
following cardiac surgery
I97.191
Other postprocedural cardiac functional disturbances
following other surgery
I97.710
Intraoperative cardiac arrest during cardiac surgery
I97.711
Intraoperative cardiac arrest during other surgery
I97.790
Other intraoperative cardiac functional disturbances
during cardiac surgery
I97.791
Other intraoperative cardiac functional disturbances
during other surgery
I97.88
Other intraoperative complications of the circulatory
system, not
elsewhere classified
I97.89
Other postprocedural complications and disorders of the
circulatory system, not elsewhere classified
M32.11
Endocarditis in systemic lupus erythematosus
R00.1
Bradycardia, unspecified
R57.0
Cardiogenic shock
T82.221A
Breakdown (mechanical) of biological heart valve graft,
initial encounter
T82.222A
Displacement of biological heart valve graft, initial
encounter
T82.223A
Leakage of biological heart valve graft, initial encounter

T82.228A
Other mechanical complication of biological heart valve
graft, initial encounter
T82.512A
Breakdown (mechanical) of artificial heart, initial
encounter
T82.514A
Breakdown (mechanical) of infusion catheter, initial
encounter
T82.518A
Breakdown (mechanical) of other cardiac and vascular
devices and implants, initial encounter
T82.522A
Displacement of artificial heart, initial encounter
T82.528A
Displacement of other cardiac and vascular devices and
implants, initial encounter
T82.529A
Displacement of unspecified cardiac and vascular devices
and implants, initial encounter
T82.532A
Leakage of artificial heart, initial encounter
T82.538A
Leakage of other cardiac and vascular devices and
implants, initial encounter
T82.592A
Other mechanical complication of artificial heart, initial
encounter
T82.598A
Other mechanical complication of other cardiac and
vascular devices and implants, initial encounter
T86.20
Unspecified complication of heart transplant
T86.21
Heart transplant rejection
T86.22
Heart transplant failure
T86.23
Heart transplant infection
T86.290
Cardiac allograft vasculopathy
T86.298
Other complications of heart transplant
T86.30
Unspecified complication of heart-lung transplant
T86.31
Heart-lung transplant rejection
T86.32
Heart-lung transplant failure
T86.33
Heart-lung transplant infection
T86.39
Other complications of heart-lung transplant
Z48.21
Encounter for aftercare following heart transplant
Z48.280
Encounter for aftercare following heart-lung transplant
Z94.1
Heart transplant status

Z94.3
Heart and lungs transplant status
This policy does not address coverage of VADs for right ventricular support, biventricular
support, use in beneficiaries under the age of 18, use in beneficiaries with complex congenital
heart disease, or use in beneficiaries with acute heart failure without a history of chronic heart
failure. Coverage under section 1862(a) (1) (A) of the Social Security Act for VADs in these
situations will be made by local Medicare Administrative Contractors (MACs) within their
respective jurisdictions.
320.3.4– Replacement Accessories and Supplies for External VADs or Any
VAD
(Rev.10837; Issued: 06-11-21; Effective: 12-01-20; Implementation: 07-27-21)
Effective April 1, 2013, claims for replacement of accessories and supplies for VADs
implanted in patients who were not eligible for coverage under Medicare Part A or had other
insurance that paid for the device and hospital stay at the time that the device was implanted,
but are now eligible for coverage of the replacement supplies and accessories under Part B,
should be submitted using HCPCS code Q0509. Those claims will be manually reviewed.
In rare instances it may be appropriate to pay for replacement of supplies and accessories for
external VADs used by patient who are discharged from the hospital. In addition, in some rare
instances, it may be necessary for a patient to have an emergency back-up controller for an
external VAD. Coverage of these items is at the discretion of the contractor. Claims for
replacement of supplies and accessories used with an external VAD that are furnished by
suppliers should be billed to the Part B MACs. Claims for replacement of supplies and
accessories used with an external VAD that are furnished by hospitals and other providers
should be billed to the Part AMACs. Effective April 1, 2013, these items should be billed
using code Q0507 so that the claims can be manually reviewed.
Claims for replacement supplies or accessories used with VADs that do not have specific
HCPCS codes and do not meet the criteria of codes Q0507 and Q0509 should be billed using
code Q0508.
Claims Coding
HCPCS Definition Effective
Date
Q0507 Miscellaneous Supply Or Accessory For Use With An
External Ventricular Assist Device
April 1,
2013
Q0508
Miscellaneous Supply or Accessory For Use With An
Implanted Ventricular Assist Device
April 1,
2013
Q0509
Miscellaneous Supply Or Accessory For Use With Any
Implanted Ventricular Assist Device For Which Payment
Was Not Made Under Medicare Part A
April 1,
2013
Q0480:Driver for use with pneumatic ventricular assist device, replacement only
Q0481:Microprocessor control unit for use with electric ventricular assist device, replacement only
Q0482:Microprocessor control unit for use with electric/pneumatic combination ventricular assist device, replacement
only
Q0483:Monitor/display module for use with electric ventricular assist device, replacement only
Q0484:Monitor/display module for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0485:Monitor control cable for use with electric ventricular assist device, replacement only
Q0486:Monitor control cable for use with electric/pneumatic ventricular assist device, replacement only
Q0487:Leads (pneumatic/electrical) for use with any type electric/pneumatic ventricular assist device, replacement only
Q0488:Power pack base for use with electric ventricular assist device, replacement only
Q0489:Power pack base for use with electric/pneumatic ventricular assist device, replacement only
Q0490:Emergency power source for use with electric ventricular assist device, replacement only
Q0491:Emergency power source for use with electric/pneumatic ventricular assist device, replacement only
Q0492:Emergency power supply cable for use with electric ventricular assist device, replacement only
Q0493:Emergency power supply cable for use with electric/pneumatic ventricular assist device, replacement only
Q0494:Emergency hand pump for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0495:Battery/power pack charger for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0496:Battery, other than lithium-ion, for use with electric or electric/pneumatic ventricular assist device, replacement
only
Q0497:Battery clips for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0498:Holster for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0499:Belt/vest/bag for use to carry external peripheral components of any type ventricular assist device, replacement
only
Q0500:Filters for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0501:Shower cover for use with electric or electric/pneumatic ventricular assist device, replacement only
Q0502:Mobility cart for pneumatic ventricular assist device, replacement only
Q0503:Battery for pneumatic ventricular assist device, replacement only, each
Q0504:Power adapter for pneumatic ventricular assist device, replacement only, vehicle type
Q0506:Battery, lithium-ion, for use with electric or electric/pneumatic ventricular assist device, replacement only
NOTE: When determined to be medically necessary, dressings used with VADs are covered under the prosthetic device
benefit as a supply necessary for the effective use of the VAD/prosthetic device. Claims for dressings necessary for the
effective use of a VAD should be billed using the appropriate miscellaneous VAD supply code, depending upon whether
the patient was eligible for coverage under Medicare Part A at the time that the VAD was implanted. The claims
processing jurisdiction for dressings used with VADs is identical to that of other VAD replacement supplies and
accessories and does not fall under Durable Medical Equipment MAC jurisdiction.
330 – Percutaneous Image-guided Lumbar Decompression (PILD) for Lumbar Spinal Stenosis
(LSS)
(Rev. 2959, Issued: 05-16-14, Effective: 01-09-14, Implementation: 10-06-14)
PILD is a posterior decompression of the lumbar spine performed under indirect image guidance without any direct
visualization of the surgical area. This is a procedure proposed as a treatment for symptomatic LSS unresponsive to
conservative therapy. This procedure is generally described as a non-invasive procedure using specially designed
instruments to percutaneously remove a portion of the lamina and debulk the ligamentum flavum. The procedure is
performed under x-ray guidance (e.g., fluoroscopic, CT) with the assistance of contrast media to identify and monitor the
compressed area via epiduragram. For complete Medical coverage guidelines, see National Coverage Determinations
(NCD) Manual (Pub 100-03) §150.13.
330.1 – Claims Processing Requirements for Percutaneous Image-guided Lumbar Decompression
(PILD) for Lumbar Spinal Stenosis (LSS) on Professional Claims
(Rev. 3811, Issued: 07-25-17, Effective: 12-07-16, Implementation: 06-27-17)
For claims with dates of service on or after January 9, 2014, PILD (procedure code 0275T) is a covered service when
billed as part of a clinical trial approved by CMS. The description for CPT 0275T is “Percutaneous
laminotomy/laminectomy (intralaminar approach) for decompression of neural elements, (with or without ligamentous
resection, discectomy, facetectomy and/or foraminotomy”, any method, under indirect image guidance (e.g.,
fluoroscopic, CT), with or without the use of an endoscope, single or multiple levels, unilateral or bilateral; lumbar”.
For claims with dates of service on or after January 1, 2015, PILD (procedure code G0276) is a covered service when
billed as part of a clinical trial approved by CMS. HCPCS G0276 is “Blinded procedure for lumbar stenosis,
percutaneous image-guided lumbar decompression (PILD), or placebo control, performed in an approved coverage with
evidence development (CED) clinical trial”.
Effective for dates of service on or after December 7, 2016, Medicare will cover PILD under CED for beneficiaries with
LSS who are enrolled in a CMS-approved prospective longitudinal study for PILD procedures using a FDA-
approved/cleared device that completed a CMS-approved randomized, controlled clinical trial (RCT) that met the criteria
listed in the January 2014 NCD (see CR 8757, transmittal # 2959, dated May 16, 2014).
The claim may only contain one of these procedure codes, not both. To use G0276, the procedure must be performed in
an approved CED clinical trial that is randomized, blinded, and contains a placebo control arm of the trial. CMS will
cover procedure code 0275T for PILD only when the procedure is performed within any other CED approved clinical
trial. Regardless of the type of CED approved clinical trial (e.g. G0276 vs 0275T), PILD is only covered when billed for
the ICD-9 diagnosis of 724.01-724.03 or the ICD-10 diagnosis of M48.05-M48.07, when billed in places of service 22
(Outpatient) or 24 (Ambulatory Surgical Center), when billed along with V70.7 (ICD-9) or Z00.6 (ICD-10) in either the
primary/secondary positions, and when billed with modifier Q0.
Additionally, per Transmittal 2805 (Change Request 8401), issued October 30, 2013, all claims for clinical trials must
contain the 8 digit clinical trial identifier number.
The following message(s) shall be used to notify providers of return situations that may occur:
Professional Claims 8-digit Clinical Trial Number
For PILD claims with procedure code 0275T with dates of service on or after January 9, 2014, or for claims with
procedure code G0276 with dates of service on or after January 1, 2015, contractors shall pay for PILD only when billed with
the numeric, 8-digit clinical trial identifier number preceded by the two alpha characters “CT” when placed in Field 19 of
paper Form CMS-1500, or when entered without the “CT” prefix in the electronic 837P in Loop 2300 REF02 (REF01=P4).
Claims for PILD which are billed without an 8-digit clinical trial identifier number shall be returned as unprocessable.
The following messages shall be used when Medicare contractors return PILD claims billed without an 8-digit clinical trial
identifier number as unprocessable:
Claims Adjustment Reason Code 16: “Claim/service lacks information or has submission/billing error(s) which is
needed for adjudication”.
Remittance Advice Remark Code N721: “This service is only covered when performed as part of a clinical trial.”
Remittance Advice Remark Code MA50: “Missing/incomplete/invalid Investigational Device Exemption number or
Clinical Trial number.”
Remittance Advice Remark Code N704: "Alert: You may not appeal this decision but can resubmit this claim/service
with corrected information if warranted."
Professional Claims Place of Service – 22 or 24
For PILD claims with procedure code 0275T with dates of service on or after January 9, 2014, or for claims with
procedure code G0276 with dates of service on or after January 1, 2015, contractors shall pay for PILD for LSS claims only
when billed in place of service 22 or 24. Claims for PILD which are billed in any other place of service shall be returned as
unprocessable.
The following messages shall be used when Medicare contractors return PILD claims not billed in place of service 22 or 24:
Claims Adjustment Reason Code 58: “Treatment was deemed by the payer to have been rendered in an inappropriate or
invalid place of service.”
Remittance Advice Remark Code N704: "Alert: You may not appeal this decision but can resubmit this claim/service
with corrected information if warranted."
Professional Claims Modifier – Q0
For PILD claims with procedure code 0275T with dates of service on or after January 9, 2014, or for claims with
procedure code G0276 with dates of service on or after January 1, 2015, contractors shall pay for PILD for LSS claims only
when billed with modifier Q0. Claims for PILD which are billed without modifier Q0 shall be returned as unprocessable.
The following messages shall be used when Medicare contractors return PILD claims billed without modifier Q0 as
unprocessable:
Claims Adjustment Reason Code 4: “The procedure code is inconsistent with the modifier used or a required modifier is
missing.”
Remittance Advice Remark Code N657: “This should be billed with the appropriate code for these services."
Remittance Advice Remark Code N704: "Alert: You may not appeal this decision but can resubmit this claim/service
with corrected information if warranted."
Non-covered Diagnosis
For PILD claims with procedure code 0275T with dates of service on or after January 9, 2014, or for claims with
procedure code G0276 with dates of service on or after January 1, 2015, contractors shall pay for PILD for LSS claims only
when billed with
the ICD-9 diagnosis of 724.01-724.03 or the ICD-10 diagnosis of M48.05-M48.07.
The following messages shall be used when Medicare contractors return PILD claims, billed without the covered diagnosis, as
unprocessable:
Claims Adjustment Reason Code B22: “This payment is adjusted based on the diagnosis.”
Remittance Advice Remark Code N704: "Alert: You may not appeal this decision but can resubmit this claim/service
with corrected information if warranted."
Clinical Trial Diagnosis
For PILD claims with procedure code 0275T with dates of service on or after January 9, 2014, or for claims with
procedure code G0276 with dates of service on or after January 1, 2015, contractors shall pay for PILD only when billed with
the ICD-9 diagnosis of V70.7 (ICD-9) or Z00.6 (ICD-10) in either the primary or secondary positions. The following
messages shall be used when Medicare contractors return PILD claims, billed without the clinical trial diagnosis, as
unprocessable:
Claims Adjustment Reason Code B22: “This payment is adjusted based on the diagnosis.”
Remittance Advice Remark Code N704: "Alert: You may not appeal this decision but can resubmit this claim/service
with corrected information if warranted."
330.2 - Claims Processing Requirements for PILD for Outpatient Facilities
(Rev. 3811, Issued: 07-25-17, Effective: 12-07-16, Implementation: 06-27-17)
Hospital Outpatient facilities shall bill for percutaneous image-guided lumbar decompression (PILD) procedure code
0275T effective on or after January 9, 2014, or procedure code G0276 effective on or after January 1, 2015, for lumbar
spinal stenosis (LSS) on a 13X or 85X TOB. Refer to Section 69 of this chapter for further guidance on billing under
CED.
Effective for dates of service on or after December 7, 2016, Medicare will cover PILD under CED for beneficiaries with
LSS who are enrolled in a CMS-approved prospective longitudinal study for PILD procedures using a FDA-
approved/cleared device that completed a CMS-approved randomized, controlled clinical trial (RCT) that met the criteria
listed in the January 2014 NCD (see CR 8757, transmittal # 2959, dated May 16, 2014).
Hospital outpatient procedures for PILD shall be covered when billed with:
• ICD-9 V70.7 (ICD-10 Z00.6) and Condition Code 30.
• Modifier Q0
• An 8-digit clinical trial identifier number listed on the CMS Coverage with Evidence Development website
Hospital outpatient procedures for PILD shall be rejected when billed without:
• ICD-9 V70.7 (ICD-10 Z00.6) and Condition Code 30.
• Modifier Q0

• An 8-digit clinical trial identifier number listed on the CMS Coverage with Evidence Development website
Claims billed by hospitals not participating in the trial /registry, shall be rejected with the following message:
CARC: 50 -These are non-covered services because this is not deemed a “medical necessity” by the payer.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a
copy of the NCD.
Group Code –Contractual Obligation (CO)
MSN 16.77 – This service/item was not covered because it was not provided as part of a qualifying trial/study. (Este
servicio/artículo no fue cubierto porque no estaba incluido como parte de un ensayo clínico/estudio calificado.)
340 – Transcatheter Edge-to-Edge Repair (TEER) for Mitral Valve Regurgitation
(Rev. 10985; Issued:09-08-21, Effective:01-19-21; Implementation:10-08-21)
Transcatheter Edge-to-Edge Repair (TEER) of the mitral valve (previously named Transcatheter Mitral Valve Repair
(TMVR)) is used in the treatment of mitral regurgitation (MR). TEER approximates the anterior and posterior mitral
valve leaflets by grasping them with a clipping device in an approach similar to a treatment developed in cardiac surgery
called the Alfieri stitch.
The most recent reconsideration of NCD 20.33 (TEER for Mitral Valve Regurgitation (previously named TMVR)) is
effective for claims with dates of service on and after January 19, 2021. It expands coverage of mitral valve TEER
procedures for the treatment of functional MR and maintains coverage of TEER for the treatment of degenerative MR,
through coverage with evidence development (CED) and with mandatory registry participation. It also makes changes
to the criteria for the heart team and hospital, and to the registry questions/criteria and the trial requirements and
outcomes. For more detailed information see Pub. 100-03, Medicare National Coverage Determinations (NCD) Manual,
Chapter 1, Section 20.33.
For services furnished between August 7, 2014 and January 19, 2021, the CMS covered TMVR for MR when furnished
under CED when the treatment was furnished for an FDA-approved indication with an FDA-approved device as follows:
(1) Treatment of significant, symptomatic, degenerative MR when furnished according to an FDA-approved indication
and all CMS coverage criteria are met, and, (2) TMVR for MR uses not expressly listed as FDA-approved indications
but only within the context of an FDA-approved, randomized clinical trial that meets all CMS coverage criteria. TMVR
was non-covered outside CED or for non-MR indications.
Historical Note: For claims processing instructions from August 7, 2014, through January 19, 2021, please see the
following links:
Change request (CR) 9002, Transmittal (TN) 178, issued December 5, 2014, informed Medicare Administrative
Contractors to pay for TMVR under CED and revised the NCD manual to add NCD 20.33:
https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R178NCD.pdf.
CR 9002, TR 3142, issued December 5, 2014, implemented the initial NCD for TMVR, effective August 7, 2014. TR
3241 rescinded and replaced TN 3142 on April 25, 2014: https://www.cms.gov/Regulations-and-
Guidance/Guidance/Transmittals/Downloads/R3241CP.pdf.
ICD-10 Coding Updates: https://www.cms.gov/Medicare/Coverage/CoverageGenInfo/ICD10
340.1 – Coding Requirements for Mitral Valve TEER Claims Furnished on or After August 7,
2014
(Rev. 10985; Issued:09-08-21, Effective:01-19-21; Implementation:10-08-21)
Current Procedural Terminology (CPT) Codes for Mitral Valve TEER Claims
CPT code 33418, Transcatheter mitral valve repair, percutaneous approach, including transseptal puncture when
performed; initial prosthesis, effective January 1, 2015.
CPT code 33419, Transcatheter mitral valve repair, percutaneous approach, including transseptal puncture when
performed; additional prosthesis (es) during same session, effective January 1, 2015. (List separately in addition to code
for primary procedure).
0345T - Transcatheter mitral valve repair percutaneous approach via the coronary sinus
ICD-10 Procedure Code for Mitral Valve TEER Claims
02UG3JZ – Supplement mitral valve with synthetic substitute, percutaneous approach
02UG3JH – Supplemental mitral valve with synthetic substitute, transapical, percutaneous approach
ICD-10 Diagnosis Codes for Mitral Valve TEER
I34.0 – Nonrheumatic mitral (valve) insufficiency, or,
I34.1 – Nonrheumatic mitral (valve) prolapse, and,
Z00.6 – Encounter for examination for normal comparison and control in clinical research program
340.2 – Claims Processing Requirements for Mitral Valve TEER Services on Professional Claims
(Rev. 10985; Issued:09-08-21, Effective:01-19-21; Implementation:10-08-21)
Professional Claims Place of Service (POS) Codes for Mitral Valve TEER Claims
Effective for claims with dates of service on and after August 7, 2014, place of service (POS) code 21 shall be used for
mitral valve TEER services. All other POS codes shall be denied.
The following messages shall be used when Medicare contractors deny mitral valve TEER claims for POS:
Claim Adjustment Reason Code (CARC) 58: “Treatment was deemed by the payer to have been rendered in an
inappropriate or invalid place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110
Service Payment Information REF), if present.”
Group Code: CO (Contractual Obligation) assigning financial liability to the provider (if a claim is received with a GZ
modifier indicating no signed ABN is on file.)
Medicare Summary Notice (MSN) 21.25: “This service was denied because Medicare only covers this service in certain
settings.”
Spanish Version: El servicio fue denegado porque Medicare solamente lo cubre en ciertas situaciones."
Professional Claims Modifiers for Mitral Valve TEER Claims
Effective for claims with dates of service on or after August 7, 2014, contractors shall pay claim lines for mitral valve
TEERs billed with the most recent CPT codes 33418, 33419, and 0345T in a clinical trial when billed with modifier -Q0.
Mitral valve TEER claim lines in a clinical trial billed without modifier -Q0 shall be returned as unprocessable.
The following messages shall be used when Medicare contractors return mitral valve TEER claim lines in a clinical trial
billed without modifier -Q0 as unprocessable:
CARC 4: “The procedure code is inconsistent with the modifier used or a required modifier is missing. Note: Refer to
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.”
N386: This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy of the
NCD.
Group Code: CO “(Contractual Obligation) assigning financial liability to the provider (if a claim is received with a GZ
modifier indicating no signed ABN is on file.)”
Professional Clinical Trial Diagnostic Coding for Mitral Valve TEER Claims
Effective for claims with dates of service on or after August 7, 2014 contractors shall pay claim lines for mitral valve
TEERs billed with the most recent CPT codes 33418, 33419 and 0345T in a clinical trial when billed with the most
recent ICD-10 diagnosis codes ICD-10 I34.0 or I34.1 and secondary ICD-10 diagnosis code Z00.6. Mitral valve TEER
claim lines in a clinical trial billed without ICD-10 diagnosis code I34.0 or I34.1 and secondary ICD-10 diagnosis code
Z00.6 shall be denied.
The following messages shall be used when Medicare contractors deny mitral valve TEER claim lines in a clinical trial
billed without secondary ICD-10 diagnosis code Z00.6:
CARC 50: These are non-covered services because this is not deemed a “medical necessity” by the payer.
RARC N386: This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a
copy of the NCD Group Code: CO (Contractual Obligation) assigning financial liability to the provider (if a claim is
received with a GZ modifier indicating no signed ABN is on file.)
MSN 15.20: The following policies [NCD 20.33]] were used when we made this decision
Spanish Version: MSN 15.20: Las siguientes políticas [NCD 20.33] fueron utilizadas cuando se tomó esta decisión.
Mandatory National Clinical Trial (NCT) Number for Mitral Valve TEER Claims
Effective for claims with dates of service on or after August 7, 2014, contractors shall pay mitral valve TEER claim lines
billed with the most recent CPT codes 33418, 33419, and 0345T in a clinical trial only when billed with an 8-digit
national clinical trial (NCT) number. Contractors shall accept the numeric, 8-digit NCT number preceded by the two
alpha characters of “CT” when placed in Field 19 of paper Form CMS-1500, or when entered WITHOUT the “CT”
prefix in the electronic 837P in Loop 2300 REF02 (REF01=P4). NOTE: The “CT” prefix is required on a paper claim,
but it is not required on an electronic claim. Mitral valve TEER claim lines in a clinical trial billed without an 8- digit
NCT number shall be returned as unprocessable.
The following messages shall be used when Medicare contractors return mitral valve TEER claim lines as unprocessable
when billed without an 8-digit NCT number:
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one Remark Code must be
provided (may be comprised of either NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an
ALERT.)”
RARC MA50: “Missing/incomplete/invalid Investigational Device Exemption number for FDA-approved clinical trial
services.”
Group Code: CO (Contractual Obligation) assigning financial liability to the provider (if a claim is received with a GZ
modifier indicating no signed ABN is on file.)
340.3 - Claims Processing Requirements for Mitral Valve TEER Services on Inpatient Hospital
Claims
(Rev. 10985; Issued:09-08-21, Effective:01-19-21; Implementation:10-08-21)
Inpatient hospitals shall bill for mitral valve TEER on an 11X type of bill (TOB) effective for discharges on or after
August 7, 2014. Refer to Section 69 of this chapter for further guidance on billing under CED.
In addition to the ICD-10 procedure and diagnosis codes mentioned above, inpatient hospital discharges for mitral valve
TEER shall be covered when billed with the following clinical trial coding:
• Secondary ICD-10 diagnosis code Z00.6
• Condition Code 30
• Value code D4 - Clinical Trial Number Assigned by NLM/NIH with an 8-digit clinicaltrials.gov identifier
number listed on the CMS website
Inpatient hospital discharges for mitral valve TEERs shall be denied when billed without the ICD-10 diagnosis,
procedure codes and clinical trial coding mentioned above. Claims that do not include these required codes shall be
rejected with the following messages:
CARC 50: These are non-covered services because this is not deemed a “medical necessity” by the payer.
RARC N386: This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a
copy of the NCD.
Group Code: CO (Contractual Obligation) assigning financial liability to the provider
MSN 15.20: The following policies [NCD 20.33] were used when we made this decision
Spanish Version: MSN 15.20 - Las siguientes políticas [NCD 20.33] fueron utilizadas cuando se tomó esta decisión.
340.4 - Claims Processing Requirements for Mitral Valve TEER Services for Medicare
Advantage (MA) Plan Participants
(Rev. 10985; Issued:09-08-21, Effective:01-19-21; Implementation:10-08-21)
MA plans are responsible for payment of mitral valve TEER services for MA plan participants. Medicare coverage for
mitral valve TEERs is not included under section 310.1 of the NCD Manual (Routine Costs in Clinical Trials).
350 - Emergency and Foreign Hospital Services
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
The conditions for payment for services furnished in a foreign country can be found in 42 CFR 424.120-127, Subpart H -
Special Conditions: Emergency Services Furnished In a Foreign Country. The payment exclusion for services furnished
outside the U.S. is located at 42 CFR 411.9 and 42 CFR 411.9(a)(2) describes the applicability of the payment exclusion
when services are furnished on board a ship.
350.1 - Services Rendered By Nonparticipating Providers
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
A. Services in Nonparticipating Domestic Hospital
Payment may be made for certain Part A inpatient and Part B outpatient hospital services provided in a nonparticipating
U.S. hospital where they are necessary to prevent the death or serious impairment of the health of the individual.
Because of the threat to the life or health of the individual, the use of the most accessible hospital equipped to furnish
such services is necessary. Items and services furnished in a domestic nonparticipating hospital may be reimbursed if
the following apply:
The hospital meets the definition of an emergency hospital. (See §350.3.)
The services meet the definition of emergency services. (See §350.2.)
The hospital is substantially more accessible from the site of the emergency than is the nearest participating
hospital. (See §350.4.)
B. Services Received by Medicare Beneficiaries outside the United States
Items and services furnished outside the United States and certain services rendered on board a ship are excluded from
coverage except for the following services:
Emergency inpatient hospital services where the emergency occurred:
o While the beneficiary was physically present in the United States; or
o In Canada while the beneficiary was traveling without reasonable delay and by the most direct route between
Alaska and another State.
Emergency or nonemergency inpatient hospital services furnished by a hospital located outside the United States,
if the hospital was closer to, or substantially more accessible from, the beneficiary’s United States residence than
the nearest participating United States hospital that was adequately equipped to deal with, and available to
provide treatment for the illness or injury.
Physician and ambulance services furnished in connection with a covered foreign hospitalization. Program
payment may not be made for any other Part B medical and other health services, including outpatient services
furnished outside the United States.
Services rendered on board a ship in a United States port, or within 6 hours of when the ship arrived at, or
departed from, a United States port, are considered to have been furnished in United States territorial waters.
Services not furnished in a United States port, or within 6 hours of when the ship arrived at, or departed from, a
United States port, are considered to have been furnished outside United States territorial waters, even if the ship
is of United States registry.
The term “United States” means the 50 States, the District of Columbia, the Commonwealth of Puerto Rico, the U.S.
Virgin Islands, Guam, the Northern Mariana Islands, American Samoa and, for purposes of services rendered on a ship,
includes the territorial waters adjoining the land areas of the United States.
A hospital that is not physically situated in one of the above jurisdictions is considered to be outside the United States,
even if it is owned or operated by the United States Government.
C. Ship Physician’s Office is in the United States.
When the physician’s office is inside of the United States, the contractor designated to process the shipboard claim is
determined by the beneficiary’s residence.
D. Ship Physician’s Office is Outside of the United States.
When the physician’s office is outside of the United States, the contractor designated to process the shipboard claim is
determined by the beneficiary’s residence.
MSN message 16.240 (English)
Services provided aboard a ship are covered only when the ship is in United States waters. In addition, the service must
be provided by a doctor licensed to practice in the United States.
MSN message 16.240 (Spanish)
Servicios proporcionados abordo de un barco son cubiertos solamente cuando el barco está en aguas territoriales de los
Estados Unidos. Además, el servicio debe ser proporcionado por un médico con licencia para practicar en los Estados
Unidos.
Payment may not be made for any item provided or delivered to the beneficiary outside the United States, even though
the beneficiary may have contracted to purchase the item while he or she was within the United States or purchased the
item from an American firm.
Under the Railroad Retirement Act, payment is made to qualified Railroad Retirement beneficiaries (QRRBs) by the
RRB for covered hospital services furnished in Canadian hospitals as well as in the U.S. Physician and ambulance
services are not covered by the Railroad Retirement Act; however, under an agreement between CMS and RRB, if the
QRRB claims payment for Part B services in connection with Canadian hospitalization, RRB processes the Part B claim.
In such cases the RRB determines:
Whether the requirements are met for the inpatient services; and
Whether the physician and/or ambulance services were furnished in connection with the services.
Services for an individual who has elected religious nonmedical health care status may be covered if the above
requirements are met but this revokes the religious nonmedical health care institution election.
350.2 - Establishing an Emergency
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Claims for emergency services must be accompanied by a physician's statement describing the nature of the emergency
and stating that the services were necessary to prevent the death, or the serious impairment of, the beneficiary. A

statement that an emergency existed is not sufficient. In addition, when inpatient services are involved, the statement
must include the date when, in the physicians' judgment, the emergency ceased.
The finding of whether the patient's condition required emergency diagnosis or treatment is ordinarily based upon the
physician's evaluation of the patient's condition immediately upon the beneficiary's arrival at the hospital.
However, the emergency nature of the situation may have been assessed by a physician who attended the patient where
the incident resulting in hospitalization occurred (for example, a heart attack or an automobile accident). In these cases,
the attending physician who ordered the hospitalization may substantiate the claim that emergency hospitalization was
necessary.
Most emergencies are of relatively short duration so that only one bill is submitted. Generally, only one physician's
statement is necessary. However, in the rare situation where an emergency continued over an extended period,
subsequent requests for payment must be accompanied by a physician's statement containing sufficient information to
indicate clearly that the emergency situation still existed. A statement that the emergency continued to exist is not
acceptable.
Additional information to support a finding that the services were emergency services from the physician, the hospital,
and others (e.g., the police department at the scene of an accident) may be requested.
Medical necessity can be documented by the physician on a CMS-l77l, Attending Physician's Statement and
Documentation of Medicare Emergency or by the beneficiary's medical records. The CMS-1771 can be obtained from:
Centers for Medicare & Medicaid Services
Forms Management Section
7500 Security Blvd.
Baltimore, MD 21244-1850
Or, the form can be downloaded from http://cms.hhs.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-List.html
350.3 - Qualifications of an Emergency Services Hospital
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
An emergency services hospital is a nonparticipating hospital that meets the requirements of the law's definition of a
"hospital" relating to full-time nursing services and licensure under State or applicable local law. (A federal hospital
need not be licensed under state or local licensing laws to meet this definition.) In addition, the hospital must be
primarily engaged in providing, under the supervision of doctors of medicine or osteopathy, services of the type
described in defining the term hospital.
The hospital must not be primarily engaged in providing skilled nursing care and related services for patients who
require medical or nursing care. Psychiatric hospitals can qualify as emergency hospitals.
350.4 - Coverage Requirements for Emergency Hospital Services Furnished Outside of the
United States
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
The following requirements must be met for payment to be made for emergency services received by Medicare
beneficiaries in foreign hospitals:
• The hospital must meet the definition of an emergency hospital and be licensed or approved by the appropriate
agency of the country in which it is located.
• The services meet the criteria of emergency services.
The foreign hospital must be closer to or substantially more accessible from the site of the emergency than the nearest
U.S. hospital that was adequately equipped and available to treat the illness or injury.
1. Emergency Occurred in the U.S. (See §350.1.B for definition of the U.S.)
If the individual was physically present in the U.S. at the time the emergency occurred, the individual's reason for
departure from the U.S. must have been specifically to obtain treatment at the foreign hospital. Services are not covered
where the person's departure from the U.S. is part of a trip abroad and the foreign hospital is more accessible simply
because the individual was in the process of travel. For example, the airplane on which the individual was traveling
could not readily return to permit the person's removal.
2. Emergency Occurred in Canada
If the emergency occurred in Canada, the beneficiary must have been traveling, without unreasonable delay, by the most
direct route between Alaska and another state. Benefits are not payable if the emergency occurred while a beneficiary
was vacationing. The requirement of travel without unreasonable delay by the most direct route will be considered met
if the emergency occurred while the beneficiary was enroute between Alaska and another state by the shortest
practicable route, or while making a necessary stopover in connection with such travel.
NOTE: An emergency occurring within the Canadian inland waterway between the States of Washington and Alaska is
considered to have occurred in Canada.
Ordinarily, the "shortest practicable route" is the one that results in the least amount of travel in Canada, consistent with
the mode of travel used between the point of entry into Canada and the intended point of departure. The amount of
travel in the U.S., prior to entering Canada is not pertinent. A route involving greater travel within Canada may be
considered the "shortest practicable route" if the additional travel resulted in a saving of time or was necessary because
of such factors as:
• Road or weather conditions;
• The age of the traveler;
• Health, or physical condition of the traveler;
• The need to make suitable travel arrangements; or
• The need to obtain acceptable accommodations.
However, the individual would be considered to have deviated from the "shortest practicable route" if the detour was
unrelated to the purpose of reaching their destination (e.g., for the principal purpose of sightseeing or vacationing).
The term "necessary stopover" means a routine stopover for rest, food, or servicing of the vehicle, and a non-routine
stopover (even though of significant duration) caused by such factors as unsuitable road or weather conditions, the
age, health, or physical condition of the traveler, the need to make suitable travel arrangements, or to obtain
acceptable accommodations.
350.5 - Services Furnished in a Foreign Hospital Nearest to Beneficiary's U.S. Residence
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Coverage is provided for inpatient hospital services furnished in a foreign hospital that is closer to, or substantially more
accessible from, the beneficiary's U.S. residence than the nearest available participating U.S. hospital that is adequately
equipped to deal with the illness or injury, whether or not an emergency existed and without regard to where the illness
or injury occurred.
"Residence" means the beneficiary's fixed and permanent home to which they intend to return whenever they are away
or a dwelling where the beneficiary periodically spends some time (e.g., a summer home).
The foreign hospital must meet accreditation requirements equivalent to Joint Commission standards. For example, the
Canadian Council on Hospital Accreditation (CCHA) has equivalent requirements. Thus, Canadian hospitals accredited
by the CCHA meet the qualifying requirements. In the case of Mexican hospitals, the Dallas or San Francisco RO
makes the determination, depending upon the hospital's location. Claims for services provided in countries other than
Canada or Mexico should be sent to the MAC that is responsible for the state or territory where the emergency arose. In
other words, the foreign claim would be processed similarly to how claims are processed in the state or territory where
the emergency arose.
See §350.11.4 below for discussion of accessibility criteria.
Some claims for services furnished in a foreign hospital nearest to the beneficiary's U.S. residence will not be
"emergency." In these nonemergency situations, it may be necessary to deny payment in whole or part, (even though it
has been approved with regard to accessibility) because the services are not medically reasonable and necessary or
involve custodial care (i.e., exclusions under §§1862(a)(1) and (9)). However, in the case of denials under the medical
necessity and custodial care exclusions, the MAC applies the limitation on liability considerations under §1879 of the
Act before issuing the denial notice.
The MAC examines claims involving medical necessity or custodial care denials to determine if there is any evidence
that the beneficiary (or the person acting on behalf of the beneficiary) was aware that the beneficiary did not require, or
no longer required, a covered level of care. The foreign hospital, since it is not participating, is not under any obligation
to furnish a written notice of noncoverage to a beneficiary in order to protect itself from being held liable under the
§1879 waiver of liability provision. However, there may be instances where the medical records of the denied foreign
claim show that the beneficiary was advised that the beneficiary did not require, or no longer required, Medicare covered
services, (e.g., written notice of noncoverage from the hospital's staff or a prior CMS denial notice). It will probably be
rare where a finding is made that the beneficiary had knowledge of noncoverage, so that, generally, payments are made
under the waiver of liability provision. The MAC uses appropriate Medicare Summary Notice (MSN) and Remittance
Advice denial messages for determinations involving the limitation on liability provision. For additional information
regarding the application of the §1879 liability provisions, see Pub 100-04, chapter 30.
350.6 – Coverage of Physician and Ambulance Services Furnished Outside U.S.
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Payment is made for necessary physician and ambulance services that meet the other coverage requirements of the
Medicare program, and are furnished in connection with a covered foreign hospitalization.
A. Coverage of Physician and Ambulance Services Furnished Outside the U.S.
Where inpatient services in a foreign hospital are covered, payment may also be made for:
Physicians’ services furnished to the beneficiary while he/she is an inpatient,
Physicians’ services furnished to the beneficiary outside the hospital on the day of his/her admission as an
inpatient, provided the services were for the same condition for which the beneficiary was hospitalized (including
the services of a physician who furnishes emergency services in Canadian waters on the day the patient is
admitted to a Canadian hospital for a covered emergency stay) and,
Ambulance services, where necessary, for the trip to the hospital in conjunction with the beneficiary’s admission
as an inpatient. Return trips from a foreign hospital are not covered.
In cases involving foreign ambulance services, the general requirements in chapter 15 are also applicable, subject to the
following special rules:
If the foreign hospitalization was determined to be covered on the basis of emergency services, the medical
necessity requirements outlined in chapter 15 are considered met.
The definition of “physician,” for purposes of coverage of services furnished outside the U.S., is expanded to
include a foreign practitioner, provided the practitioner is legally licensed to practice in the country in which the
services are furnished.
Only the beneficiary may file for Part B benefits. The assignment method may not be used. However, where the
beneficiary is deceased, the rule for settling Part B underpayments is applicable, i.e., payment may be made to
the foreign physician or ambulance company on the basis of an unpaid bill, provided the physician or ambulance
company accepts the MACs reasonable charge determination as the full charge.
The regular deductible and coinsurance requirements apply to physician and ambulance services.
350.7 - Claims for Services Furnished in Canada to Qualified Railroad Retirement Beneficiaries
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
All claims for hospital and/or related physician or ambulance services furnished in Canada to qualified railroad
retirement beneficiaries (QRRB’s) are forwarded first to the Railroad Retirement Board (RRB). Under the Railroad
Retirement Act, payment is made by the RRB to Qualified Railroad Retirement Beneficiaries (QRRB) for covered
hospital services furnished in Canadian hospitals as well as in the U.S. The Railroad Retirement Act does not cover
physician and ambulance services; however, under an agreement between CMS and RRB, if the QRRB claims payment
for Part B services in connection with Canadian hospitalization, RRB processes the Part B claim. In such cases the RRB
determines:
• Whether the requirements in §§350.1.B and 350.6 are met in regard to the inpatient services; and
• Whether the requirements in§350.6.A are met in regard to the physician and/or ambulance services were
furnished in connection with the services
If either is not met, RRB denies the claim and notifies the beneficiary. If met, RRB refers the claim to the RRB MAC,
Palmetto GBA, to determine if the coverage criteria for physician and/or ambulance services are met.
The hospital must forward all claims for services furnished QRRBs in Canada to:
Retirement Medicare Section
U.S. Railroad Retirement Board
844 North Rush Street
Chicago, IL 60611-2092
If a QRRB is a resident of Canada, Medicare payments are reduced by the amount of payment made for the same
services by the Canadian Provincial Health Insurance Plan.
B. Claims for services furnished in other foreign countries
The RRB does not pay for health care services furnished in Mexico or any foreign countries other than Canada.
All claims for inpatient hospital services and/or related physician or ambulance services furnished in Mexico to QRRB’s
should be forwarded directly to the Railroad Retirement Board. If the Railroad Retirement Board determines that the
requirements in §350.6.A are not met, the Railroad Retirement Board will deny the claim and send notice to the
beneficiary. If the requirements in §350.6.A or B are met, the Railroad Retirement Board will hold any potentially
allowable Part B claim until an MAC determination regarding the coverage of Part A services has been made. When
the information regarding Part A coverage is available, the Railroad Retirement Board will send the Part B claim,
together with pertinent information regarding the Part A determination, to Palmetto Government Benefits for
consideration of whether the other requirements for Part B coverage are met, and further processing.
350.8 - Claims from Hospital-Leased Laboratories Not Meeting Conditions of Participation
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Services furnished by a laboratory that does not meet the hospital laboratory conditions of participation and is operated
under a lease arrangement in a domestic emergency hospital are covered only if they are emergency inpatient services
reimbursable under Part A.
A MAC may send a claim from such a laboratory and identify it as an "Emergency Lead." The MAC checks its files to
see if a claim for emergency services was filed and, if so, determines whether the laboratory services were furnished
during the period of emergency. If the emergency claim was forwarded to the appropriate MAC for processing, it enters
the date received on the laboratory claim.
If no emergency claim was filed, or laboratory services were not furnished in the period covered by the emergency
claim, the MAC develops the claim as a possible emergency. It includes the laboratory claim with any subsequent
claim.
If no emergency is alleged, the MAC records on the claim that no emergency existed and disallows it.
350.9 - Nonemergency Part B Medical and Other Health Services
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
A. Coverage
Nonemergency services to Medicare beneficiaries may be paid for if the coverage requirements for the services are met,
and are not covered as Part A emergency inpatient services.
Program payment may be made for the following Part B medical and other health services furnished by a U.S.
nonparticipating hospital on a nonemergency basis:
• Diagnostic x-ray tests, diagnostic laboratory tests and other diagnostic tests. (The hospital must meet the
applicable conditions of participation for the services.)
• X-ray, radium, and radioactive isotope therapy, including materials and services of technicians. (The hospital
must meet the applicable conditions of participation for these services.)
• Services of residents and interns, nurses, therapists, etc., which are directly related to the provision of x-ray or
laboratory or other diagnostic tests, or the provisions of x-ray or radium therapy.
• Prosthetic devices (other than dental) which replace all or part of an internal body organ (including contiguous
tissue) or replace all or part of the functions of a permanently inoperative or malfunctioning internal body organ,
including replacement of such devices.
• Leg, arm, back, and neck braces, trusses and artificial legs, arms, and eyes, including replacement, if required,
because of a change in the patient's physical condition.
B. Distinction Between Emergency and Nonemergency Medical and Other Health Services
Emergency coverage, particularly Part B emergency outpatient coverage, is broader than the nonemergency Part B
Medical and Other Health Services coverage provisions. When the emergency requirements are met, program payment
may be made to the hospital for the full range of outpatient hospital services. In addition to the nonemergency coverage
list, emergency coverage includes hospital services (including drugs and biologicals - blood is a biological - which
cannot be self-administered), "incident to physicians' services rendered to outpatients," and outpatient physical therapy
and speech-language pathology. The latter two services are not covered under the nonemergency provisions. Payment
for "incident to" services can be only under the emergency rather than the nonemergency provisions.
Whether Part B payment is made under the emergency or nonemergency provisions, it may be made for diagnostic
laboratory tests furnished by an emergency hospital only if the hospital meets the conditions of participation relating to
hospital laboratories. It may be made only for radiology services furnished by an emergency hospital if the hospital
meets the conditions of participation relating to radiology departments. Part B payment may be made for diagnostic
laboratory tests furnished by a nonparticipating hospital which is not an emergency hospital only if the hospital
laboratory meets the conditions of coverage of independent laboratories and for radiology services furnished by it, only
if it meets the conditions of participation relating to radiology departments.
C. Claims Processing
The hospital enters the annotation "nonemergency-hospital accepts assignment" in Remarks of the Form CMS-1450. If
it is determined that some or all of the services are not covered under the nonemergency provisions, the claim is returned
to it (if hospital-filed) or to the beneficiary (if patient-filed) to determine whether the services might be covered as
emergency services.
350.10 - Elections to Bill for Services Rendered By Nonparticipating Hospitals
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
A. Nonparticipating U.S. Hospitals
As a nonparticipating U.S. hospital meeting emergency requirements, the hospital has the option to bill the program
during a calendar year by filing an election with its MAC. If it files an election, it should submit claims for the
following services furnished all Medicare beneficiaries throughout the year:
• Emergency inpatient services; and
• Emergency outpatient services.
In addition, the hospital may not bill any beneficiary beyond deductibles, coinsurance, and noncovered services in that
calendar year. It must agree to refund any monies incorrectly collected. It may not file an election for the calendar year
if it has already charged any beneficiary for covered services furnished in that year.
If the hospital does not file a billing election, the beneficiary can file a claim. The beneficiary may request information
from the hospital or the MAC as appropriate.
During November of each year, the MAC will send the non-participating hospital a letter (see §360.3.1). Also, during
November of each year, the MAC will send a letter to each domestic hospital, giving it an opportunity to elect to bill
Medicare if it has not been doing so (§360.3.2).
If during the year the hospital requests to bill the program, its MAC will send the model letter in §360.3.3.
B. Billing for Services Furnished Prior to Certification
The following rules apply if a bill is submitted for services rendered before and after a hospital's certification
(participation) date:
• PPS hospitals are paid the DRG, if the date of discharge is after the certification date.
• Other hospitals are paid for services rendered after the certification date. However, the hospital must include
services before certification date on its cost report.
It should annotate in the upper right hand corner of the claim "Emergency Conversion."
C. Foreign Hospitals
Foreign hospitals may submit a statement to the appropriate MAC stating that they will bill for all claims. If they do not,
the beneficiary may claim the payment. When the MAC is aware that a hospital is willing to bill the program for all
covered services, it solicits the hospital's agreement to:
• Bill for all covered services for the calendar year (except for deductible and coinsurance amounts);
• Not bill the beneficiary for any amounts other than for deductible and coinsurance and charges for noncovered
services; and
• Refund to the beneficiary any monies incorrectly collected.
A hospital may not file an election for a calendar year if it has charged any beneficiary for covered services during that
year.
D. Submitting Claims
The beneficiary or the hospital that has elected to bill the program may submit emergency claims for payment to the
appropriate MAC for evaluation of accessibility or emergency factors.
The hospital completes the claim (Form CMS-1450 or electronic equivalent) according to billing instructions in chapter
25. It enters "hospital filed emergency admission" in Item 94 "Remarks." It sends the completed bill and the necessary
emergency documentation (Form CMS-1771, Attending Physicians Statement and Documentation of Medicare
Emergency) or medical records to substantiate the emergency to the appropriate MAC.
NOTE: See §360.2, "Designated Contractors."
If the hospital submits a claim but has not filed an election to bill the program, the MAC will contact the hospital to
determine if it is qualified and wish to bill the program. If it declines, the claim will be denied. A claim will be solicited
from the beneficiary.
If the hospital has filed a billing election and the beneficiary files a claim, the beneficiary's claim is denied and the MAC
contacts the hospital regarding the claim.
350.11 - Processing Claims
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
All claims are subject to development to determine whether the Medicare secondary payer provisions apply. (See Pub.
100-05, Medicare Secondary Payer Manual.)
A. Nonparticipating Hospitals
The processing MAC is responsible for making accessibility and medical emergency determinations for physician and
ambulance services.
1. Claims Subject to Technical Denials
The following claims are subject to technical denial:
• Foreign nonemergency services claims if:
° The residence requirement is not met. (See §350.5.)
° The hospital rendering the service does not meet Joint Commission or equivalent accreditation
requirements set by a hospital approval program of the country in which it is located.
° The accessibility requirements are not met. (See §350.11.4.)
• Canadian travel claims when the requirements in §350.4 are not met.
• Emergency services claims for which the hospital does not meet the definition of an emergency hospital.
• Claims for which the query response shows the beneficiary is not entitled to benefits.
• Any foreign claim when Part A benefits are exhausted and Part B physician or ambulance claims are not
involved.
2. Either the Accessibility or Medical Emergency Requirements are Not Met
Claim is denied but retained in case of an appeal by the beneficiary.
NOTE: Even though Part A or Part B emergency services furnished by U.S. hospitals are denied, Part B payment may
be possible for Medical and Other Health Services specified in Pub. 100-02, Medicare Benefit Policy Manual, chapter 6.
Claim is retained in case of an appeal by the beneficiary.
3. Emergency Services Partially Denied
When the medical emergency is approved but not for the entire period, the claim is processed and payment made for the
covered period.
B. Foreign Part B Physician and Ambulance Claims
The hospital must attach any Part B claim for foreign physician and ambulance services to the corresponding Part A
claim and forward to the MAC.
If the MAC determines that the inpatient services were covered, it sends the physician and/or independent ambulance
claim to the designated MAC for processing and payment. (See §350.6.)
If the Part A claim is denied on the basis of accessibility of medical emergency, the MAC denies the Part B claim, and
sends a MSN to the beneficiary. It retains copies in case of an appeal by the beneficiary.
NOTE: Even though Part A benefits are totally or partially exhausted, payment may be made by the MAC for physician
and independent ambulance services furnished if all coverage requirements are met.
If a Part A claim was partially denied because the emergency terminated, the MAC makes a decision on the claim and
any provider-based ambulance claim. It sends copies to the appropriate MAC for processing.
350.11.1 - Contractors Designated to Process Foreign Claims
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Per contractor Statement of Work (SOW) all contractors are designated to process claims for physicians’ and ambulance
services furnished in connection with a covered foreign hospital stay for their beneficiaries who reside in the states/areas
for which they process claims.
All contractors are designated to determine whether the requirements in §350.6 are met for claims for inpatient services
based upon the geographic location of the foreign hospitals furnishing the services.
All contractors are designated to process these claims if there is evidence that the Part B services were furnished in
connection with covered foreign inpatient hospital services. If there is no evidence, the Contractor must send a front-end
rejection notice in accordance with §350.11.2.
350.11.2 - Contractor Processing Guidelines
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Per contractor Statement of Work (SOW) all contractors are responsible for processing foreign, emergency and
shipboard claims for their beneficiaries who reside in the states/areas for which they process claims.
The A/B MAC determines whether the requirements in §350.6.A are met. If these requirements are not met, the A/B
MAC denies the Part A claim and related Part B claim and notifies the beneficiary. Where the A/B MAC determines
that the requirements in §350.6.A are met, the A/B MAC determines whether other applicable Part A coverage
requirements are met. If the A/B MAC disallows the Part A claim, it denies the related Part B claim and notifies the
beneficiary. However, the A/B MAC will not be involved in the processing of foreign claims if, for any reason, the
related Part A claim is denied.
If the claim does not show that the beneficiary was hospitalized, the A/B MAC sends the beneficiary a front-end
rejection notice. In filling out the Notification of Medicare Determination, the A/B MACs should check “other” and
include the following explanation: “Foreign physician or ambulance services are not covered unless they were furnished
in connection with a covered inpatient stay.”
350.11.3 - Medicare Approved Charges for Services Rendered in Canada or Mexico
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
For Canadian services, the Medicare approved charge will be the lower of:
1. The allowed amount for the same service in the U.S. locality closest to where the service was furnished (as
determined by the designated MAC), or
2. The Canadian Provincial fee.
Therefore, the designated MAC must obtain the most recent schedule of fees published by the appropriate Canadian
Province. Most of the designated MACs deal with only one Provincial schedule.
For Mexican services, the maximum charge is the Medicare allowed amount for the same service in the locality closest
to where the service was furnished (as determined by the designated MAC).
350.11.4 - Accessibility Criteria
(Rev. 4111, Issued: 08-10-18, Effective: 9-11-18, Implementation: 9-11-18)
A. Emergency Claims
The MAC uses the same criteria in domestic and foreign emergency claims. This includes services in a foreign religious
non-medical health care institution and Canadian Travel claims. (See §350.4 and §350.9.)
Emergency determinations take into account such matters as relative distances of a participating hospital, and road
conditions. The MAC considers whether the nature of the emergency required immediate transportation to the nearest
available hospital (i.e., the nonparticipating hospital) or, without hazard to the patient, would have permitted the
additional transportation time to take the patient to a more distant participating hospital in the same general area.
The MAC does not consider in its determination such factors involving selection of a hospital which reflect the personal
preferences of the individual or physician, (e.g., physician does not have staff privileges at the participating hospital)
nearness to beneficiary's residence, presence of previous medical records at the nonparticipating hospital, cost, or type of
accommodations available.
The following sections discuss documentation of the accessibility requirement and provide guidelines for making a
determination where the participating hospital is:
• Closer to the site of the emergency than is the admitting nonparticipating hospital;
• Fifteen or fewer miles farther from the site of the emergency than is the nonparticipating hospital; or
• Sixteen or more miles farther from the site of the emergency than is the admitting nonparticipating hospital.
In urban and suburban areas, where both participating and nonparticipating hospitals are similarly available, it is
presumed, in the absence of clear and convincing evidence to the contrary, that the services could have been provided in
the participating hospital.
1. Participating Hospital Closer to Site of Emergency
If there is an adequately equipped participating hospital with available beds closer to the site of the emergency than the
nonparticipating hospital, accessibility is not met. Claim is denied unless extenuating circumstances were present that
necessitated admission to the nonparticipating hospital, e.g., because of road or traffic conditions additional travel time
would have been needed.
2. Participating Hospital 15 or Fewer Miles Farther From the Location of the Emergency Than the Admitting
Nonparticipating Hospital
In this situation the accessibility is provisionally not met. The claim is reviewed to determine if the nature of the
emergency required the immediate transportation to the nonparticipating hospital. If the review indicates that the nature
of the emergency would have allowed the additional transportation time needed to take the patient to the participating
hospital without undue hazard, the accessibility requirement is not met. The claim is denied.
3. Participating Hospital More than 15 Miles Farther From the Location of the Emergency Than the Admitting
Nonparticipating Hospital
The accessibility requirement is deemed met.
B. Foreign Nonemergency Claims
The following presumptions are applied to the relative accessibility of the nearest participating U.S. and foreign
hospitals.
1. Admitting Foreign Hospital is Closer to the Beneficiary's Residence Than the Nearest Participating U.S. Hospital
The accessibility requirement is met.
2. Admitting Foreign Hospital is Farther From the Beneficiary's Residence Than the Nearest Participating U.S. Hospital
The accessibility requirement is not met unless evidence establishes the practical necessity for the beneficiary's
admission. This requirement is met if the use of a closer participating U.S. hospital was impractical, e.g., non-
availability of beds, needed equipment or personnel, or transportation not available.
In determining whether a foreign hospital is more accessible than a participating hospital, the MAC does not consider
the personal preference of the beneficiary, physician, or others in the selection of a hospital, the type of accommodations
available, or the nonavailability of staff privileges to the attending physician.
350.11.5 - Medical Necessity
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
A. Emergency Services
Reimbursement for emergency inpatient hospital services is permitted only for those periods during which the patient's
state of injury or disease is such that a health or life-endangering emergency existed and continued to exist, requiring
immediate care that could be provided only in a hospital. The allegation that an emergency existed must be
substantiated by sufficient medical information from the physician or hospital. If the physician's statement does not
provide it, or is not supplemented by adequate clinical corroboration of this allegation, it does not constitute sufficient
evidence.
Death of the patient does not necessarily establish the existence of a medical emergency, since in some chronic, terminal
illnesses, time is available to plan admission to a participating hospital. The lack of adequate care at home or lack of
transportation to a participating hospital does not constitute a reason for emergency hospital admission, without an
immediate threat to the life and health of the patient. Since the existence of medical necessity for emergency services is
based upon the physician's assessment of the patient prior to admission, serious medical conditions developing after a
non-emergency admission are not "emergencies" under the emergency services provisions of the Act.
The emergency ceases when it becomes safe, from a medical standpoint, to move the individual to a participating
hospital, another institution, or to discharge the individual.
B. Criteria
Since the decision that a medical emergency existed can be a matter of subjective medical judgment involving the entire
gamut of disease and accident situations, it is impossible to provide arbitrary guidelines.
1. Diagnosis is Considered "Usually an Emergency"
An emergency condition is an unanticipated deterioration of a beneficiary's health which requires the immediate
provision of inpatient hospital services because the patient's chances of survival, or regaining prior health status, depends
upon the speed with which medical or surgical procedures are, or can be, applied. While many diagnoses (e.g.,
myocardial infarction, acute appendicitis) are normally considered emergencies, the hospital must check medical
documentation for internal consistencies (e.g., signs and symptoms upon admission, notations concerning changes in a
preexisting condition, results of diagnostic tests).
EXAMPLE: If the diagnosis is given as "coronary," the physician's statement is "coronary," without further explanatory
remarks, and the statement of services rendered gives no indication that an electrocardiogram was taken, or that the
patient required intensive care, etc., further information is required. On the other hand, if the diagnosis is one that
ordinarily indicates a medical and/or surgical emergency, and the treatment, diagnostic procedures, and period of
hospitalization are consistent with the diagnosis, further documentation may be unnecessary. An example is: admitting
diagnosis - appendicitis; discharge diagnosis - appendicitis; surgical procedures - appendectomy; period of inpatient stay
- 7 days.
2. Patient Dies During Hospitalization
If an emergency existed at the time of admission and the patient subsequently expires, the claim is allowed for
emergency services if the period of coverage is reasonable. However, death of the patient is not prima facie evidence
that an emergency existed; e.g., death can occur as a result of elective surgery or in the case of a chronically ill patient
who has a long terminal hospitalization. Such claims are denied.
3. Patient's Physician Does Not Have Staff Privileges at a Participating Hospital
The fact that the beneficiary's attending physician does not have staff privileges at a participating hospital has no bearing
on the emergency services determination. If the lack of staff privileges in an accessible participating hospital is the
governing factor in the decision to admit the beneficiary to an "emergency hospital," the claim is denied irrespective of
the seriousness of the medical situation.
4. Beneficiary Chooses to be Admitted to a Nonparticipating Hospital
The claim is denied if the beneficiary chooses to be admitted to a non-participating hospital as a personal preference
(e.g., participating hospital is on the other side of town) when a bed for the required service is available in an accessible,
participating hospital.
5. Beneficiary Cannot be Cared for Adequately at Home
The patient who cannot be cared for adequately at home does not necessarily require emergency services. The claim is
denied in the absence of an injury, the appearance of a disease or disorder, or an acute change in a pre-existing disease
state which poses an immediate threat to the life or health of the individual and which necessitates the use of the most
accessible hospital equipped to furnish emergency services.
6. Lack of Suitable Transportation to a Participating Hospital
Lack of transportation to a participating hospital does not, in and of itself, constitute a reason for emergency services.
The availability of suitable transportation can be considered only when the beneficiary's medical condition
contraindicates taking the time to arrange transportation to a participating hospital. The claim is denied if there is no
immediate threat to the life or health of the individual, and time could have been taken to arrange transportation to a
participating hospital.
7. "Emergency Condition" Develops Subsequent to a Non-emergency Admission to a Nonparticipating Hospital
Program payment cannot be made for emergency services furnished by a nonparticipating hospital when the emergency
condition arises after a non-emergency admission. An example: treatment of postoperative complications following an
elective surgical procedure or treatment of a myocardial infarction that occurred during a hospitalization for an elective
surgical procedure. The existence of medical necessity for emergency services is based upon the physician's initial
assessment of the apparent condition of the patient at the time of the patient's arrival at the hospital, i.e., prior to
admission.
8. Additional "Emergency Condition" Develops Subsequent to an Emergency Admission to a Nonparticipating Hospital
If the patient enters a nonparticipating hospital under an emergency situation and subsequently has other injuries,
diseases or disorders, or acute changes in preexisting disease conditions, related or unrelated to the condition for which
the patient entered, which pose an immediate threat to life or health, emergency services coverage continues.
Emergency services coverage ends when it becomes safe from a medical standpoint to move the patient to an available
bed in a participating institution or to discharge the patient, whichever occurs first.
C. Documenting Medical Necessity
1. Physician's Supporting Statement
Claims for emergency services by a non-participating hospital should be accompanied by an Attending Physician's
Statement and Documentation of Medicare Emergency, Form CMS-1771 or its equivalent. This form describes the
nature of the emergency, furnishing relevant clinical information about the patient, and certifying that the services
rendered were required as emergency services. However, a copy of the patient's hospital records may be submitted
instead. It should include history, physical, and admission notes, the medical record admission sheet, nurses' notes,
doctors' orders, discharge summary, and all progress notes. A statement that an emergency existed, or the listing of
diagnoses, without supporting information, is not sufficient. In addition, the statement must include the date, in the
physician's judgment, the emergency ceased. The physician who attended the patient at the hospital makes the statement
concerning emergency services. Only in exceptional situations, with appropriate justification, may another physician
having full knowledge of the case, make the certification.
2. Beneficiary's Statement in Canadian Travel Claims
In Canadian travel claims, the beneficiary's statement is considered in making a determination regarding medical
necessity for emergency services; i.e., whether an emergency occurred while a beneficiary was traveling between Alaska
and another State by the most direct route without unreasonable delay. (See §350.4.)
350.11.6 - Time Limitation on Emergency and Foreign Claims
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
The regular time limits apply to requests and claims for payment for emergency hospital services and hospital services
outside the U.S., for physician and ambulance services furnished in connection with foreign hospitalization, and for
nonemergency services furnished by a domestic nonparticipating hospital. See chapter 1 for a description of these
requirements.
A. Beneficiary Denial Notices
MACs shall send denial letters for non-covered foreign related claims.
Part B MACs will send an MSN for covered foreign emergency and shipboard claims related to a covered Part A foreign
claim. An MSN is also sent for shipboard services provided within US territories.
B. Termination of Emergency Services
No payment will be made for inpatient or outpatient emergency services rendered after a reasonable period of medical
care in relation to the emergency condition in question. Some services may be covered in a domestic nonparticipating
hospital as Part B Medical and Other Health Services. (See the Medicare Benefit Policy Manual, chapter 6.) If, based
upon all information, the total period claimed for emergency services coverage does not exceed the time required for a
reasonable period of emergency medical care, the entire inpatient stay is covered. The fact that a medical record or other
information states that the patient showed definite improvement several days prior to discharge is not necessarily an
indication that the need for emergency services ceased as of that date. The concept of a reasonable period of emergency
medical care is most easily applied when relatively short-term medical care is followed by the patient’s progressive
improvement. There are situations or conditions in which the determination of the end of covered emergency services
may be more difficult because the patient’s impairment is prolonged, there is no progressive improvement, or the
patient’s course may be progressively downhill, even though the condition is not critical. The stroke patient may be in
this category. In such cases the need for emergency medical care usually ceases before the need for medical care in an
institutional setting (i.e., hospital or SNF) ceases. Thus, the reasonable period of emergency care does not include the
entire hospital stay if the stay was prolonged beyond the point when major diagnostic evaluation and treatment were
carried out.
The MAC will make the determination based upon all information available. As a general rule, if the period claimed for
emergency services exceeds by more than 3 to 5 days the date on which the record definitely indicates that there was
substantial improvement in the patient’s condition so that the patient could possibly have been moved to a participating
facility or discharged without damage to health, the period beyond the 3 to 5 days is denied. If the total period claimed
for emergency services exceeds by no more than 3 to 5 days the date on which the record indicates substantial
improvement in the patient’s condition, the entire period is allowed.
This rule is intended to screen out short stay emergency hospitalization cases in which the patient was either discharged
or transferred to a participating provider within a reasonable time after the medical record definitely indicated substantial
improvement in the patient’s condition.
The reasonable period of emergency care is that period required to provide relief of acute symptoms or for initial
management of the condition while arrangements are made for definitive treatment. Two examples:
• Prostatic hypertrophy which results in acute urinary retention; and
• Mental illness with suicidal and/or homicidal tendencies.
In acute urinary retention, the reasonable period of emergency medical care includes the period required for
catheterization and stabilization of the patient. The patient could then be transferred to a participating hospital for
surgery or other required treatment. For the suicidal or homicidal patient, a reasonable period of emergency medical
care includes the time required for initial management of the case while arrangements are made for transfer (by
commitment or otherwise) to a participating hospital. A period of 24 to 48 hours of emergency care is usually sufficient
in both cases.
350.11.7 – Payment Denial for Medicare Services furnished to Alien Beneficiaries Who are Not
Lawfully Present in the United States
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Medicare payment may not be made for items and services furnished to an alien beneficiary who was not lawfully
present in the United States on the date of service.
The CWF must establish an auxiliary file based on enrollment data contained in the Enrollment Data Base maintained by
the Centers for Medicare & Medicaid Services in order to appropriately edit the claims specifically associated with alien
beneficiaries. The auxiliary file will be the basis for an edit that rejects claims for a beneficiary that was not lawfully
present in the U.S. on the date of service. MACs and DMACs must deny claims for items and services, rejected by
CWF on the basis that the beneficiary was not lawfully present in the U.S. on the date of service. MACs and DMACs
must refer to the CWF documentation on this subject for the error code MSN Message 5.7, assigned to this editing.
Upon receipt of an error code MSN Message 5.7, A/B MACs, DME MACs, and A/B MACs (HHH) must deny the claim
and use reason code (CARC) 177 – “Patient has not met the required eligibility requirements.” When CWF rejects a
claim, MACs and DMACs must use MSN message 5.7, “Medicare payment may not be made for the item or service
because, on the date of service, you were not lawfully present in the United States.” 5.7, Medicare no puede pagar por
este artículo o servicio porque, en la fecha en que lo recibió, usted no estaba legalmente en los Estados Unidos.
A party to a claim denied in whole or in part under this policy may appeal the initial determination on the basis that the
beneficiary was lawfully present in the United States on the date of service. In addition, this same information must be
published in your next regularly scheduled bulletin. If you have a listserv that targets the affected provider communities,
you must use it to notify subscribers that information “Medicare Services for Alien Beneficiaries Lawfully present the
United States” is available on your Web site.
NOTE: Section 401 of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA),
codified at 8 U.S.C. §1611, prohibits aliens who are not “qualified aliens” from receiving Federal public
benefits including Medicare.
However, Section 5561 of the Balanced Budget Act of 1997 (BBA) amended Section 401 of the PRWORA to create a
Medicare exemption to the prohibition on eligibility for non-qualified alien beneficiaries, who are lawfully present in the
United States and who meet certain other conditions. Specifically, payment may be made for services furnished to an
alien who is lawfully present in the United States (and provided that with respect to benefits payable under Part A of
Title XVIII of the Social Security Act [42 U.S.C. 1395c et seq.], who was authorized to be employed with respect to any
wages attributable to employment which are counted for purposes of eligibility for Medicare benefits). The definition
for “lawfully present in the United States” is found at 8 CFR 1.3.
350.12 - Appeals on Claims for Emergency and Foreign Services
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
When a MAC receives a beneficiary appeal of a claim submitted by the beneficiary for services provided by a non-
participating provider, the MAC will process the appeal in accordance with the guidelines in Pub. 100-04 chapter 29.
When a MAC receives an appeal from a non-participating provider of a claim that was submitted by, or on behalf of, a
beneficiary, the MAC shall dismiss the appeal request as the non-participating provider is not a proper party. The MAC
shall send a copy of the dismissal to the beneficiary. A non-participating provider does not have standing to file an
appeal for the individual claims for payment it submits on behalf of a beneficiary, or for claims the beneficiary submits
for services it has furnished. See, 42 CFR 405.906(a)(3) and 405.902 (for the definition of provider); Pub. 100-04,
chapter 29, §210 and the glossary in Pub. 100-04, chapter 29, §110 (for the definition of provider). Only a beneficiary
(or the beneficiary’s authorized representative, or an appointed representative on behalf of the beneficiary) can appeal
claim determinations for services furnished by a non-participating provider.
NOTE: Non-participating providers have appeal rights under the provider and supplier enrollment appeals process in 42
CFR Part 498 for MAC determinations related to the non-participating provider’s election to file claims (see §350.10).
NOTE: The RRB conducts Part B redeterminations under the Railroad Retirement Act for services rendered in Canada.
360 - Payment for Services Received By Nonparticipating Providers
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
The condition of payment regulations for emergency services received in Nonparticipating Providers can be found in the
42 CFR 424.100-109, Subpart G—Special Conditions: Emergency Services Furnished by a Nonparticipating Hospital.
The Form CMS-1450 or its electronic equivalent must be used.
A. Hospital Filed Claims
1. Inpatient Services
The payment rate for inpatient claims is 100 percent of the nonparticipating provider’s customary charges (see 42 C.F.R.
413.74(b) and 42 C.F.R. 424.104(a)(3)).
The cost of the services is adjusted by any applicable deductible and coinsurance amounts for which the beneficiary is
responsible.
Payment will be made to Federal hospitals that furnish emergency services, on an inpatient basis, to individuals entitled
to hospital benefits. Payment will be based on the lower of the actual charges from the hospital or rates published for
Federal hospitals in the “Federal Register” under Office of Management and Budget - Cost of Hospital and Medical Care
and Treatment Furnished by the United States; Certain Rates Regarding Recovery from Tortiously Liable Third Persons.
Medicare will not pay federal hospitals for emergency items or services furnished to veterans, retired military personnel
or eligible dependents. However, Medicare can pay for the inpatient deductible charged by VA hospitals, or credit that
amount to the Medicare Part A deductible, for emergency services furnished to veterans. If a Part A claim is denied, a
denial notice will be forwarded to the beneficiary from the MAC. The beneficiary can use this notice to forward to their
private insurer, if applicable.
The VA or Department Of Defense hospital must file a statement of election for each calendar year to receive direct
payment from Medicare for all claims filed that year.
2. Outpatient Services
The amount paid by Medicare for emergency outpatient claims is obtained as follows:
• Eighty-five percent of the total covered charges is the estimated cost figure. The applicable Part B deductible
is subtracted. Coinsurance is subtracted from the remainder.
• Subtracting the deductible from 85 percent of the total covered charges and applying the 20 percent
coinsurance rate to the remainder obtains the patient’s coinsurance amount. The hospital will be paid cost
(85 percent of covered charges) minus deductible and coinsurance.
3. Part B Medical and Other Health Services
Part B medical and other health services, including hospital-based ambulance services whether hospital or beneficiary
filed, may be covered and paid on a non-emergency basis. To calculate the amount paid by Medicare, the hospital
subtracts the Part B deductible from the total covered charges and applies the 80 percent payment rate.
4. Special Letters for Partially or Totally Denied (Hospital-Filed) Claims for Emergency Inpatient Services
The patient receives a notice from CMS covering the emergency payment of a partially denied claim. A denial letter and
a Part B explanation of benefits is sent to the patient. The MAC includes its address on this letter.
B. Beneficiary Filed Claim
1. Emergency Inpatient Claims
The payment computation follows:
• Any noncovered accommodation charge is subtracted from the total accommodation charges. The amount of
the inpatient deductible or coinsurance met on this bill is subtracted. Any remainder is multiplied by 60
percent.
• The total noncovered ancillary charge is subtracted from the total ancillary charge. Any inpatient deductible
or coinsurance that remains is subtracted. The remainder is multiplied by 80 percent.
• The benefit amounts obtained are added.
2. Emergency Outpatient Services
To calculate the amount paid by Medicare, the hospital must subtract any applicable Part B deductible from the total
covered charges and apply the 80 percent payment rate.
3. Part B Medical and Other Health Services
Part B medical and other health services furnished by nonparticipating hospitals, including hospital-based ambulance
services, may be covered and paid on a non-emergency basis.
To calculate the amount paid by Medicare, the hospital must subtract any applicable Part B deductible from the total
covered charges and apply an 80 percent payment rate.
4. Special Letters for Patient-Filed Claims for Emergency Inpatient Services
For emergency admissions to nonparticipating hospitals where direct payment is made to the patient, the MAC sends the
beneficiary one of the letters described below, as appropriate.
The letter explains the Part A payments made. Part B payments are made for ancillary services not covered by Part A
and are also explained in a letter. This letter also explains the beneficiary’s right of appeal.
The MAC retains a duplicate of all notices sent for documentation in any appeals process. It enters the date the notice is
released on both copies of all notices.
Sample paragraphs:
• “Enclosed is a check for $______, which is the amount Medicare can pay for inpatient hospital services you
received from (date of admission) to (date of discharge) in (hospital).”
• “Medicare is able to pay 60 percent of the charges for your room and board plus 80 percent of the charges for all
other covered services during the period (date emergency began) to (date payment ended).”
“Medicare is able to pay 60 percent of the charges for your room and board, 80 percent of the charges for other
separately identified charges, and 66 2/3 percent of the other charges which were not separately identified on the
hospital bill.”
• “Medicare does not pay (the first $ ____ of charges) (the first three pints of blood) ($ ____ a day after the 60th
day) in a benefit period. (Select one or more, if applicable.)”
• “If lifetime reserve days are used, add $ ___ a day from ________ to _________.”
• “If you believe your Medicare hospital insurance should have covered all or more of your expenses, you may get
in touch with us at the address shown on this letter.”
• “If you believe that the determination is not correct, you may request a reconsideration for hospital insurance (or
a review for medical insurance). You may make the request by mail to the address shown on this letter. If you
come in person, please bring this notice with you.”
• “This check includes a medical insurance payment for 80 percent of the charges for certain nonroutine hospital
services which you received from _______ through _______. These services are listed on the enclosed form.”
• “If a hospital bill is not itemized, Medicare can pay 66 2/3 percent of the total covered charges. Payment is being
made at this rate for charges from (date emergency began) to (date payment ended).”
• “We are enclosing a check for $ ______. This is your payment under Part B for 80 percent of the charges for the
services which you received from (admission date) through (discharge date) while in (name of hospital). These
services are listed on the enclosed form.”
When payment cannot be made under hospital insurance, medical insurance covers some, but not all, of the hospital
services. Room and board and certain other services are not covered by medical insurance.
360.1 - Payment for Services from Foreign Hospitals
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
The condition of payment regulations for emergency services received in Nonparticipating Providers can be found in the
42 CFR 424.100-109, Subpart G—Special Conditions: Emergency Services Furnished by a Nonparticipating Hospital
A. Hospital Filed Claim

A foreign hospital that elects to bill the Medicare program receives 100 percent of its customary charges, subject to
applicable deductible and coinsurance amounts. The hospital establishes its customary charges for the services by
submitting an itemized bill with each claim. This eliminates the need to file a cost report.
Regardless of the billing form used, the MAC must:
• Recode the bill using revenue codes for the Form CMS-1450;
• Prepare an HUIP or HUOP input record for CWF; and
• Send a Medicare Summary Notice (MSN) to the beneficiary.
The nonparticipating hospital must file a statement of election for each calendar year to receive direct payment from
Medicare for all claims filed that year.
Payment is subject to the official exchange rate on the date the patient is discharged.
B. Beneficiary Filed Claim
To calculate the amount paid by Medicare for Part B Hospital-Based Ambulance Claims, the hospital must subtract any
unmet Part B deductible from the total covered charges and apply the 80 percent payment rate.
Payment to the beneficiary is subject to the official exchange rate on the date of discharge.
360.1.1 - Attending Physician’s Statement and Documentation of Medicare Emergency
(
Rev. 4111, Issued: 08-10-18, Effective: 9-11-18, Implementation: 9-11-18)
Form CMS-1771 - go to https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-List.html
360.2 - Designated Contractors
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
Per Contractor Statement of Work (SOW) all contractors are designated to process claims for physicians’ and ambulance
services furnished in connection with a covered hospital stay in Canada and Mexico for their beneficiaries who reside in
the states/areas for which they process claims.
360.3 - Model Letters, Nonparticipating Hospital and Emergency Claims
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
360.3.1 - Model Letter to Nonparticipating Hospital That Elected to Bill For Current Year
(Rev.3287, Issued: 6-30-15, Effective:04-21-15, Implementation: 04-21-15)
DEPARTMENT OF HEALTH AND HUMAN SERVICES
CENTERS FOR MEDICARE & MEDICAID SERVICES
REFER TO:
Identification Number:___________________
Dear _________________:
Your election to bill the Medicare program for emergency services furnished to Medicare beneficiaries will expire on
December 31. Payment for emergency services can be made to a nonparticipating hospital only if the hospital elects to
receive reimbursement from Medicare for all emergency services furnished to Medicare beneficiaries in a calendar year.
If you elect to bill the program, please return to us in the enclosed self-addressed envelope a statement signed by an
authorized official of your hospital stating that you elect to claim payment under the Medicare program. An election to
bill cannot be withdrawn during the year. If a statement is not received by December 31, we will assume that you do not
wish to continue to bill the program at this time. However, you still retain the right to elect to bill the program at any
time during the coming year if, when you make your election, you have not yet charged any Medicare beneficiary in that
year for emergency hospital services rendered to him.
Hospitals electing to bill the program for emergency services may obtain information on reimbursement by contacting
the MAC serving nonparticipating hospitals in your State. If you do not elect to bill, the beneficiary may apply for
reimbursement by submitting an itemized bill.
Please contact us if you need any further information. In addition, if at any time you decide to request full participation
as a provider of hospital services under the Medicare program, please contact your Medicare MAC for complete
particulars.
Sincerely,
360.3.2 - Model Letter to Nonparticipating Hospital That Did Not Elect to Bill for Current Year
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
DEPARTMENT OF HEALTH AND HUMAN SERVICES
CENTERS FOR MEDICARE & MEDICAID SERVICES
REFER TO:
Identification Number:______________________
Dear ___________________:
Under the Medicare program, hospital benefits ordinarily can be paid only for care furnished to patients of hospitals that
are participating in the program. However, the program can also pay for hospital services furnished to a beneficiary who
is admitted to a nonparticipating hospital in an emergency. To receive payments for emergency services, a
nonparticipating hospital must meet certain conditions specified in the law. We have determined that your hospital
meets these conditions.
Payment for emergency services can be made to a nonparticipating hospital only if the hospital elects to receive
reimbursement from Medicare for all emergency services furnished to Medicare beneficiaries in a calendar year.
Although your hospital did not elect to bill the program for the current calendar year, you may wish to bill for the
coming year. If you so choose, please have an authorized official of your hospital sign a statement to this effect and
return in the enclosed self-addressed envelope. Retain a copy for your records. An election to bill cannot be withdrawn
during the year.
If we have not received a statement from you by December 31, we will assume that you do not wish to bill the program
at this time. However, you still retain the right to elect to bill the program at any time during the coming year if, when
you make your election, you have not yet charged any Medicare beneficiary in that year for emergency hospital services
rendered to him.
Hospitals electing to bill the program for emergency services may obtain information on reimbursement by contacting
us. If a hospital does not elect to bill, the beneficiary may apply for reimbursement by submitting an itemized bill.
If at any time you decide to request full participation as a provider of hospital services under the Medicare program,
please contact your Medicare intermediary for complete particulars.
Sincerely,
360.3.3 - Model Letter to Nonparticipating Hospital That Requests to Bill the Program
(Rev. 3287, Issued: 06-30-15, Effective: 04-21-15, Implementation: 04-21-15)
DEPARTMENT OF HEALTH AND HUMAN SERVICES
CENTERS FOR MEDICARE & MEDICAID SERVICES
REFER TO:
Identification Number:______________________
Dear ____________________:
This refers to your inquiry concerning payment for emergency hospital services rendered to a Medicare beneficiary in a
hospital which is not participating in the Medicare program. Under the Medicare program, hospital benefits ordinarily
can be paid only for care furnished to patients of hospitals that are participating in the program. However, the program
can also pay for hospital services furnished to a beneficiary who is admitted to a nonparticipating hospital in an
emergency. To receive payments for emergency services, a nonparticipating hospital must meet certain conditions
specified in the law. We have determined that your hospital meets these conditions.
Payment for emergency services can be made to a nonparticipating hospital only if you elect to receive reimbursement
from Medicare for all emergency services furnished to Medicare beneficiaries in a calendar year. Your hospital may
now choose to bill the program for all emergency services furnished to Medicare beneficiaries during the current
calendar year, if you have not yet charged any Medicare beneficiary this year for emergency hospital services rendered
to him.
If you so choose, please have an authorized official of your hospital sign a statement to this effect and return in the
enclosed self-addressed envelope. Retain a copy for your records. An election to bill cannot be withdrawn during the
year.
Hospitals electing to bill the program for emergency services may obtain information on reimbursement by contacting
us. If you do not elect to bill, the beneficiary may apply for reimbursement by submitting an itemized bill.
If at any time you decide to request full participation as a provider of hospital services under the Medicare program,
please contact your Medicare intermediary for complete particulars.
Sincerely,
360.3.4 - Full Denial - Hospital-Filed or Beneficiary-Filed Emergency Claim
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare identification
number. For purposes of this manual, Medicare beneficiary identifier references both the Health Insurance Claim
Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition period and after
for certain business areas that will continue to use the HICN as part of their processes.
Contractors shall include beneficiary appeal rights language and include in the mailing a redetermination request
form where applicable.
MODEL DENIAL NOTICE A
(MAC'S NAME AND ADDRESS)
Date: ______________
Beneficiary: ____________________
Claim Number ________________
DETERMINATION ON EMERGENCY HOSPITAL SERVICES
We are sorry, but payment cannot be made for your stay from _______ through _______ at (hospital). This is because
the (hospital) does not participate in the Medicare program and it has been determined that your treatment there does not
qualify as emergency care.
Under the law, payment for services received in a nonparticipating hospital can be made only if you go, or are brought
to, the hospital to receive emergency care. Emergency care under Medicare is defined as:
a. Care which is necessary to prevent the death or serious impairment to the health of the individual; and
b. Which, because of threat to the life or health of the individual, requires the use of the nearest hospital (in miles or
travel time) that has a bed available and is equipped to handle the emergency.
The medical facts of your hospital admission and stay have been carefully reviewed. Based upon this review, we have
found that, although it was necessary for you to be hospitalized, a medical emergency did not exist. There would have
been time for you to have been admitted to a hospital participating in Medicare.
If you have questions about this notice, you may call 1-800-MEDICARE (1-800-633-4227) for additional information.
If you believe the determination is not correct, you may request a redetermination. You must file your request within
120 days from the date you receive this notice. A request for a redetermination must be filed either on Form CMS-
20027 or on a written request that includes all of the elements listed below.
• Beneficiary name
• Medicare beneficiary identifier
• Specific service and/or item(s) for which a redetermination is being requested
• Specific date(s) of service
• Signature of the beneficiary or the beneficiary’s authorized or appointed representative.
You may send the request to our address above. Please keep a copy of any written correspondence for your files.
Sincerely,
360.3.5 - Partial Denial - Hospital-Filed or Beneficiary-Filed Emergency Claim
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare identification
number. For purposes of this manual, Medicare beneficiary identifier references both the Health Insurance Claim
Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition period and after
for certain business areas that will continue to use the HICN as part of their processes.
MODEL DENIAL NOTICE A
(MAC'S NAME AND ADDRESS)
Date: ______________
Beneficiary: ____________________
Claim Number ________________
DETERMINATION ON EMERGENCY HOSPITAL SERVICES
This refers to your request for payment under Medicare for the services received while a patient at (hospital), from
_______ through _______.
Payment can be made under the hospital insurance part of Medicare only for the costs of your hospitalization from
_______ to _______.
The (hospital) does not participate in the Medicare program. Under the law, payment for services received in a
nonparticipating hospital can be made only if you go, or are brought to, the hospital to receive emergency care.
Emergency care under Medicare is defined as:
a. Care which is necessary to prevent the death or serious impairment to the health of the individual; and
b. Which, because of threat to the life or health of the individual, requires the use of the nearest hospital (in miles or
travel time) which has a bed available and is equipped to handle the emergency.
Payment for emergency services stops when the emergency ends and it is permissible, from a medical standpoint, either
to transfer the patient to a participating hospital or to discharge him.
The medical facts of your hospital admission and stay have been carefully reviewed. Based upon this review, we have
found that an emergency condition existed when you were admitted. However, the medical information indicates that
this emergency condition ended on ________. At that time, your condition had improved to the extent that you could
have been transferred to a hospital participating in the Medicare program.
If you have questions about this notice, you may call 1-800-MEDICARE (1-800-633-4227) for additional information.
If you believe the determination is not correct, you may request a redetermination. You must file your request within
120 days of the date you receive this notice. A request for a redetermination must be filed either on Form CMS-20027
or on a written request that includes all of the elements listed below.
• Beneficiary name
• Medicare beneficiary identifier
• Specific service and/or item(s) for which a redetermination is being requested
• Specific date(s) of service
• Signature of the beneficiary or the beneficiary’s authorized or appointed representative.
You may send the request to our address listed above. Please keep a copy of any written correspondence for your files.
Sincerely,
360.3.6 - Denial - Military Personnel/Eligible Dependents
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare identification
number. For purposes of this manual, Medicare beneficiary identifier references both the Health Insurance Claim
Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition period and after
for certain business areas that will continue to use the HICN as part of their processes.
MODEL DENIAL NOTICE A
(MAC'S NAME AND ADDRESS)
Date: ______________
Beneficiary: ____________________
Claim Number ________________
DETERMINATION ON EMERGENCY HOSPITAL SERVICES
We are sorry, but payment cannot be made for your stay from________ through________ at (hospital).
Under the law, medical services that have been furnished by a federal hospital to retired members of the armed services,
or their eligible dependents, are not covered under the Medicare program.
If you have questions about this notice, you may call 1-800-MEDICARE (1-800-633-4227) for additional information.
If you believe the determination is not correct, you may request a redetermination. You must file your request within
120 days from the date you receive this notice. A request for a redetermination must be filed either on Form CMS-20027
or on a written request that includes all of the elements listed below.
• Beneficiary name
• Medicare beneficiary identifier
• Specific service and/or item(s) for which a redetermination is being requested
• Specific date(s) of service
• Signature of the beneficiary or the beneficiary’s authorized or appointed representative.
You may send the request to our address listed above. Please keep a copy of any written correspondence for your files.
Sincerely,
360.3.7 - Full Denial - Shipboard Claim - Beneficiary Filed
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare identification
number. For purposes of this manual, Medicare beneficiary identifier references both the Health Insurance Claim
Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition period and after
for certain business areas that will continue to use the HICN as part of their processes.
MODEL DENIAL NOTICE
(MAC’S NAME AND ADDRESS)
Date: ____________________
Beneficiary: _________________________
Claim Number: __________________
DETERMINATION ON SHIPBOARD SERVICES
We are sorry, but medical services provided on the (vessel/ship's name) cruise ship are not covered. The Medicare
program can make payment for medically necessary shipboard services only if all of the following requirements are met:
1. The services are furnished while the ship is within the territorial waters of the United States (in a U.S. port, or
within 6 hours of departure or arrival at a U.S. port).
2. The services are furnished to an individual who is entitled to Part B benefits;
3. The services are furnished in connection with covered inpatient hospital services;
4. The services furnished on the ship are for the same condition that required inpatient admission;
5. The physician is legally authorized to practice in the country where he or she furnishes the services.
If you have a supplemental insurance policy, you should check with the company carrying that policy to see if they
cover these services and what procedures you should follow in submitting your claim.
If you have questions about this notice, you may call 1-800-MEDICARE (1-800-633-4227) for additional information.
If you believe the determination is not correct, you may request a redetermination. You must file your request within
120 days from the date you receive this notice. A request for a redetermination must be filed either on Form CMS-
20027 or on a written request that includes all of the elements listed below.
• Beneficiary name
• Medicare beneficiary identifier
• Specific service and/or item(s) for which a redetermination is being requested
• Specific date(s) of service
• Signature of the beneficiary or the beneficiary’s authorized or appointed representative.
You may send the request to our address listed above. Please keep a copy of any written correspondence for your files.
Sincerely,
360.3.8 - Full Denial - Foreign Claim - Beneficiary Filed
(Rev. 4203, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare identification
number. For purposes of this manual, Medicare beneficiary identifier references both the Health Insurance Claim
Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition period and after
for certain business areas that will continue to use the HICN as part of their processes.
MODEL DENIAL
NOTICE (MAC’S NAME AND ADDRESS)

Date:
Beneficiary:
Claim Number:
DETERMINATION ON FOREIGN HOSPITAL SERVICES
We are sorry, but payment cannot be made for your stay
from through
at (hospital) in (country).
Medicare law prohibits payment for items and services furnished outside the United States except in certain limited
circumstances. The term “outside the U.S.” means anywhere other than the 50 states of the U.S., the District of
Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands.
There are three situations when Medicare may pay for certain types of health care services rendered in a foreign
hospital (a hospital outside the U.S.):
1. You’re in the U.S. when you have a medical emergency and the foreign hospital is closer than the nearest
U.S. hospital that can treat your illness or injury.
2. You’re traveling through Canada without unreasonable delay by the most direct route between Alaska and
another state when a medical emergency occurs, and the Canadian hospital is closer than the nearest U.S.
hospital that can treat your illness or injury. Medicare determines what qualifies as “without unreasonable
delay” on a case-by-case basis.
3. You live in the U.S. and the foreign hospital is closer to your home than the nearest U.S. hospital that can
treat your medical condition, regardless of whether it’s an emergency.
In these situations, Medicare will pay only for the Medicare-covered services you get in a foreign hospital.
If you have a supplemental insurance policy, you should check with the company carrying that policy to see if they
cover these services and what procedures you should follow in submitting your claim.
If you have questions about this notice, you may call 1-800-MEDICARE (1-800-633-4227) for additional information.
If you believe the determination is not correct, you may request a redetermination. You must file your request within
120 days from the date you receive this notice. A request for a redetermination must be filed either on Form CMS-
20027 or on a written request that includes all of the elements listed below.
• Beneficiary name
• Medicare beneficiary identifier
• Specific service and/or item(s) for which a redetermination is being requested
• Specific date(s) of service
• Signature of the beneficiary or the beneficiary’s authorized or appointed representative.
You may send the request to our address listed above. Please keep a copy of any written correspondence for your files.
Sincerely,
370 – Microvolt T-wave Alternans (MTWA)
(Rev. 3265, Issued: 05-22-15, Effective: 01-13-15, Implementation: 06-23-15)

On March 21, 2006, the Centers for Medicare & Medicaid Services (CMS) began national coverage of microvolt T-
wave Alternans (MTWA) diagnostic testing when it was performed using only the spectral analysis (SA) method for the
evaluation of patients at risk for sudden cardiac death (SCD) from ventricular arrhythmias and patients who may be
candidates for Medicare coverage of the placement of an implantable cardiac defibrillator (ICD).
Effective for claims with dates of service on and after January 13, 2015, Medicare Administrative Contractors (MACs)
may determine coverage of MTWA diagnostic testing when it is performed using methods of analysis other than SA for
the evaluation of patients at risk for SCD from ventricular arrhythmias. Further information can be found at Publication
100-03, section 20.30, of the National Coverage Determinations Manual.
370.1 - Coding and Claims Processing for MTWA
(Rev. 12396; Issued: 12-07-23; Effective: 01-09-24; Implementation: 01-09-24)
Effective for claims with dates of service on and after March 21, 2006, MACs shall accept CPT
93025 (MTWA for assessment of ventricular arrhythmias) for MTWA diagnostic testing for the
evaluation of patients at risk for SCD with the SA method of analysis only. All other methods of
analysis for MTWA are non-covered.
Effective for claims with dates of service on and after January 13, 2015, MACs shall at their
discretion determine coverage for CPT 93025 for MTWA diagnostic testing for the evaluation of
patients at risk for SCD with methods of analysis other than SA. The –KX modifier shall be used as
an attestation by the practitioner and/or provider of the service that documentation is on file verifying
the MTWA was performed using a method of analysis other than SA for the evaluation of patients at
risk for SCD from ventricular arrhythmias and that all other NCD criteria was met.
NOTE: The –KX modifier is NOT required on MTWA claims for the evaluation of patients at
risk for SCD if the SA analysis method is used.
NOTE: This diagnosis code list/translation was approved by CMS/Coverage. It may or may not be a
complete list of covered indications/diagnosis codes that are covered but should serve as a finite
starting point.
As this policy indicates, individual A/B MACs within their respective jurisdictions have the discretion
to make coverage determinations they deem reasonable and necessary under section 1862(a)(1)(A) of
the Social Security Act. Therefore, A/B MACs may have additional covered diagnosis codes in their
individual policies where contractor discretion is appropriate.
ICD-10-Codes:
ICD-10 CM
ICD-10 DX Description
I21.01
ST elevation (STEMI) myocardial infarction involving left main coronary
artery
I21.02
ST elevation (STEMI) myocardial infarction involving left anterior
descending coronary artery
I21.09
ST elevation (STEMI) myocardial infarction involving other coronary artery
of anterior wall
I21.11
ST elevation (STEMI) myocardial infarction involving right coronary artery

I21.19
ST elevation (STEMI) myocardial infarction involving other coronary artery
of inferior wall
I21.21
ST elevation (STEMI) myocardial infarction involving left circumflex
coronary artery
I21.29
ST elevation (STEMI) myocardial infarction involving other sites
I21.3
ST elevation (STEMI) myocardial infarction of unspecified site
I21.4
Non-ST elevation (NSTEMI) myocardial infarction
I21.A1
Myocardial infarction type 2
I21.B
Myocardial infarction with coronary microvascular dysfunction
I22.0
Subsequent ST elevation (STEMI) myocardial infarction of anterior wall
I22.1
Subsequent ST elevation (STEMI) myocardial infarction of inferior wall
I22.2
Subsequent non-ST elevation (NSTEMI) myocardial infarction
I22.8
Subsequent ST elevation (STEMI) myocardial infarction of other sites
I22.9
Subsequent ST elevation (STEMI) myocardial infarction of unspecified site
I24.81
Acute coronary microvascular dysfunction
I24.89
Other forms of acute ischemic heart disease
I24.9
Acute ischemic heart disease, unspecified
I47.0
Re-entry ventricular arrhythmia
I47.2
Ventricular tachycardia
I49.01
Ventricular fibrillation
I49.02
Ventricular flutter
R55
Syncope and collapse
370.2 - Messaging for MTWA
(Rev. 3265, Issued: 05-22-15, Effective: 01-13-15, Implementation: 06-23-15)
Effective for claims with dates of service on and after January 13, 2015, MACs shall deny claims for MTWA CPT
93025 with methods of analysis other than SA without modifier -KX using the following messages:
CARC 4: “The procedure code is inconsistent with the modifier used or a required modifier is missing. Note: Refer to
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.”
RARC N657 – This should be billed with the appropriate code for these services.
Group Code: CO (Contractual Obligation) assigning financial liability to the provider
MSN 15.20 - The following policies [NCD 20.30] were used when we made this decision
Spanish Equivalent - 15.20 - Las siguientes políticas [NCD 20.30] fueron utilizadas cuando se tomó esta decisión.
380 - Leadless Pacemakers
(Rev. 3815, Issued: 07-28-17, Effective: 01-18-18, Implementation: 08-29-17 - for MAC local edits; January 2,
2018 - for MCS shared edits)
Effective for dates of service on or after January 18, 2017, contractors shall cover leadless pacemakers through Coverage
with Evidence Development (CED) when procedures are performed in CMS-approved CED studies. Please refer to the
National Coverage Determinations Manual (Publication 100-03, Section 20.8.4) for more information.
380.1 - Leadless Pacemaker Coding and Billing Requirements for Professional Claims
(Rev. 3815, Issued: 07-28-17, Effective: 01-18-18, Implementation: 08-29-17 - for MAC local edits; January 2,
2018 - for MCS shared edits)
Effective for dates of service on or after January 18, 2017, contractors shall allow the following procedure codes on
claims for leadless pacemakers:
0387T Transcatheter insertion or replacement of permanent leadless pacemaker, ventricular
0389T Programming device evaluation (in person) with iterative adjustment of the implantable device to test the
function of the device and select optimal permanent programmed values with analysis, review and report, leadless
pacemaker system.
0390T Peri-procedural device evaluation (in person) and programming of device system parameters before or after
surgery, procedure or test with analysis, review and report, leadless pacemaker system.
0391T Interrogation device evaluation (in person) with analysis, review and report, includes connection, recording and
disconnection per patient encounter, leadless pacemaker system.
Effective for dates of service on or after January 18, 2017, contractors shall allow the following ICD-10 diagnosis codes
on claims for leadless pacemakers:
Z00.6 – Encounter for examination for normal comparison and control in clinical research program.
380.1.1 - Leadless Pacemaker Place of Service Restrictions
(Rev. 3815, Issued: 07-28-17, Effective: 01-18-18, Implementation: 08-29-17 - for MAC local edits; January 2,
2018 - for MCS shared edits)
Effective for dates of service on or after January 18, 2017, contractors shall only pay claims for leadless pacemakers
when services are provided in one of the following places of service (POS):
POS 06 – Indian Health Service Provider Based Facility
POS 21 – Inpatient Hospital
POS 22 - On Campus-Outpatient Hospital
POS 26 – Military Treatment Facility
380.1.2 - Leadless Pacemaker Modifier
(Rev. 3815, Issued: 07-28-17, Effective: 01-18-18, Implementation: 08-29-17 - for MAC local edits; January 2,
2018 - for MCS shared edits)
Effective for claims with dates of service on or after January 18, 2017, modifier Q0 – Investigational clinical service
provided in a clinical research study that is an approved clinical research study, must also be included.
380.1.3 - Leadless Pacemaker Additional Claim Billing Information
(Rev. 3815, Issued: 07-28-17, Effective: 01-18-18, Implementation: 08-29-17 - for MAC local edits; January 2,
2018 - for MCS shared edits)
The professional claim must also contain the 8-digit clinical trial identifier in item 23 of the CMS-1500 form or the
electronic equivalent.
380.2 - Leadless Pacemaker Claim Adjustment Reason Codes (CARC), Remittance Advice
Remark Codes (RARC) and Medicare Summary Notice (MSN) Messages Applicable for
Professional Claims Only
(Rev. 3815, Issued: 07-28-17, Effective: 01-18-18, Implementation: 08-29-17 - for MAC local edits; January 2,
2018 - for MCS shared edits)
Effective for claims with dates of service on or after January 18, 2017, contractors shall deny professional claim lines for
leadless pacemakers that do not contain an appropriate POS code and use the following messages:
CARC 58: “Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service.
Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if
present.”
RARC N386: “This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
http://www.cms.hhs.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a
copy of the NCD.”
MSN 21.25: “This service was denied because Medicare only covers this service in certain settings.”
Spanish Version: El servicio fue denegado porque Medicare solamente lo cubre en ciertas situaciones."
Group Code –Contractual Obligation (CO).
- Effective for dates of service on or after January 18, 2017, contractors shall return claims with the procedure codes
listed in 380.2 billed without modifier Q0 and use the following messages:
CARC 4: “The procedure code is inconsistent with the modifier used or a required modifier is missing. Note: Refer
to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.”
RARC N572: This procedure not payable unless appropriate non-payable reporting.
Group Code – Contractual Obligation (CO).
- Effective for dates of service on or after January 18, 2017, contractors shall return claims as unprocessable with the
procedure codes listed in 10117-04.2 billed without ICD-10 Z00.6 and use the following messages:
CARC 16 - Claim/service lacks information or has submission/billing error(s) which is needed for adjudication. Do
not use this code for claims attachment(s)/other documentation. At least one Remark Code must be provided (may
be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an
ALERT.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information
REF), if present.
RARC M76 - Missing/incomplete/invalid diagnosis or condition.
- Effective for claims with dates of service on or after January 18, 2017, contractors shall return claims as
unprocessable that are billed with the Q0 modifier and do not contain the 8-digit clinical trial identifier in item 23 of
the CMS-1500 form or the electronic equivalent. Use the following messages:
CARC 16: “Claim/service lacks information which is needed for adjudication. At least one Remark Code must be
provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is
not an ALERT.)”
RARC MA50: Missing/incomplete/invalid Investigational Device Exemption number or Clinical Trial number.
Group Code – Contractual Obligation (CO).
390 - Supervised exercise therapy (SET) Symptomatic Peripheral Artery Disease
(Rev. 4049, Issued: 05- 11-18, Effective: 05-25-17, Implementation: 07-02-18)
Effective for claims with dates of service on or after May 25, 2017, the Centers for Medicare and Medicaid Services
(CMS) will cover supervised exercise therapy (SET) for beneficiaries with intermittent claudication (IC) for the
treatment of symptomatic peripheral artery disease (PAD). Up to 36 sessions over a 12 week period are covered if all of
the following components of a SET program are met:
The SET program must:
• consist of sessions lasting 30-60 minutes comprising a therapeutic exercise-training program for PAD in patients
with claudication;
• be conducted in a physician’s office;
• be delivered by qualified auxiliary personnel necessary to ensure benefits exceed harms, and who are trained in
exercise therapy for PAD; and
• be under the direct supervision of a physician (as defined in 1861(r)(1)) of the Social Security Act (the Act)),
physician assistant, or nurse practitioner/clinical nurse specialist (as identified in 1861(aa)(5)) of (the Act) who
must be trained in both basic and advanced life support techniques.
Beneficiaries must have a face-to-face visit with the physician responsible for PAD treatment to obtain the referral for
SET. At this visit, the beneficiary must receive information regarding cardiovascular disease and PAD risk factor
reduction, which could include education, counseling, behavioral interventions, and outcome assessments.
SET is non-covered for beneficiaries with absolute contraindications to exercise as determined by their primary
attending physician. .
Please refer to the National Coverage Determinations Manual (Publication 100-03, Section 20.35) for more information.
390.1 General Billing Requirements
(Rev. 4049, Issued: 05- 11-18, Effective: 05-25-17, Implementation: 07-02-18)
Effective for claims with date of services on or after May 25, 2017, contractors shall pay claims for SET for
beneficiaries with IC for the treatment of symptomatic PAD, with a referral from the physician responsible for PAD
treatment.
Medicare Administrative Contractors (MACs) have the discretion to cover SET beyond 36 sessions over 12 weeks and
may cover an additional 36 sessions over an extended period of time. Contractors shall accept the inclusion of the KX
modifier on the claim line(s) as an attestation by the provider of the services that documentation is on file verifying that
further treatment beyond the 36 sessions of SET over a 12 week period meets the requirements of the medical policy.
390.2 Coding Requirements for SET
(Rev. 4049, Issued: 05- 11-18, Effective: 05-25-17, Implementation: 07-02-18)
• CPT 93668 – Under
Peripheral Arterial Disease Rehabilitation
• ICD-10 Codes
I70.211 –right leg
I70.212 – left leg
I70.213 – bilateral legs
I70.218 – other extremity
I70.311 – right leg
I70.312 – left leg
I70.313 – bilateral legs
I70.318 – other extremity
I70.611 – right leg
I70.612 – left leg
I70.613 – bilateral legs
I70.618 – other extremity
I70.711 – right leg
I70.712 – left leg
I70.713 – bilateral legs
I70.718 – other extremity
390.3 Special Billing Requirements for Institutional Claims
(Rev.4049, Issued: 05- 11-18, Effective: 05-25-17, Implementation: 07-02-18)
Contractors shall pay claims for SET services containing CPT code 93668 on Types of Bill (TOBs) 13X under OPPS and 85X
based on reasonable cost.
Contractors shall pay claims for SET services containing CPT 93668 with revenue codes 096X, 097X, or 098X when billed
on TOB 85X Method II
based on 115% of the lesser of the fee schedule amount or the submitted charge.
390.4 Common Working File (CWF) Requirements
(Rev.4049, Issued: 05- 11-18, Effective: 05-25-17, Implementation: 07-02-18)
CWF shall create a new edit for CPT 93668 to reject claims when a beneficiary has reached 36 SET sessions within 84
days after the date of the first SET session and the KX modifier is not included on the claim or to reject any SET session
provided after 84 days from the date of the first session and the KX modifier is not included on the claim.
CWF shall determine the remaining SET sessions.
The CWF determination, to parallel claims processing, shall include all applicable factors including:
• Beneficiary entitlement status
• Beneficiary claims history
• Utilization rules
CWF shall update the determination when any changes occur to the beneficiary master data or claims data that would
result in a change to the calculation.
CWF shall display the remaining SET sessions on all CWF provider query screens.
The Multi-Carrier System Desktop Tool (MCSDT) shall display the remaining SET sessions in a format equivalent to
the CWF HIMR screen(s).
390.5 Applicable Medicare Summary Notice (MSN), Remittance Advice Remark Codes and
Claim Adjustment Reason Code Messaging
(Rev.4049, Issued: 05- 11-18, Effective: 05-25-17, Implementation: 07-02-18)
• Contractors shall deny claims for SET when services are provided on other than TOBs 13X and 85X using the
following messages:
MSN 15.20: “The following policies NCD 20.35 were used when we made this
decision.”
Spanish Version – “Las siguientes políticas NCD 20.35 fueron utilizadas cuando se tomó esta decisión.”
(Part A only) MSN 15.19: “Local Coverage Determinations (LCDs) help Medicare decide what is covered. An
LCD was used for your claim. You can compare your case to the LCD, and send information from your doctor if
you think it could change our decision. Call 1-800-MEDICARE (1-800-633-4227) for a copy of the LCD”.
Spanish Version - Las Determinaciones Locales de Cobertura (LCDs en inglés) le ayudan a decidir a Medicare lo
que está cubierto. Un LCD se usó para su reclamación. Usted puede comparar su caso con la determinación y
enviar información de su médico si piensa que puede cambiar nuestra decisión. Para obtener una copia del LCD,
llame al 1-800-MEDICARE (1800-633-4227).
Claim Adjustment Reason Code (CARC) 58:
“Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service.
NOTE: Refer to the 832 Healthcare Policy Identification Segment (loop 2110 Service payment Information
REF), if present.
Remittance advice remark code (RARC) N386: This decision was based on a National Coverage Determination
(NCD) 20.35. An NCD provides a coverage determination as to whether a particular item or service is covered.
A copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not have web access, you may
contact the contractor to request a copy of the NCD.
Contractors shall use Group Code CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
• Contractors deny/reject claim lines for CPT 93668 without one of the diagnosis codes listed in 390.2 and use the
following messages:
MSN 15.20: “The following policies NCD 20.35 were used when we made this
decision.”
Spanish Version – “Las siguientes políticas NCD 20.35 fueron utilizadas cuando se tomó esta decisión.”
(Part A only) MSN 15.19: “Local Coverage Determinations (LCDs) help Medicare decide what is covered. An
LCD was used for your claim. You can compare your case to the LCD, and send information from your doctor if
you think it could change our decision. Call 1-800-MEDICARE (1-800-633-4227) for a copy of the LCD”.
Spanish Version - Las Determinaciones Locales de Cobertura (LCDs en inglés) le ayudan a decidir a Medicare lo
que está cubierto. Un LCD se usó para su reclamación. Usted puede comparar su caso con la determinación y
enviar información de su médico si piensa que puede cambiar nuestra decisión. Para obtener una copia del LCD,
llame al 1-800-MEDICARE (1800-633-4227).
CARC 167 – This (these) diagnosis(es) is (are) not covered. Note: Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF), if present.
RARC N386 – “This decision was based on a National Coverage Determination (NCD). An NCD provides a
coverage determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy
of the NCD.”
Contractors shall use Group Code PR (Patient Responsibility) assigning financial liability to the beneficiary if a
claim is received with a GA modifier indicating a signed ABN is on file.
Contractors shall use Group CO (Contractual Obligation) assigning financial liability to the provider, if a claim is
received with a GZ modifier indicating no signed ABN is on file.
• Contractors shall reject claims with CPT 93668 which exceed 36 sessions within 84 days from the date of the
first session when the KX modifier is not included on the claim line OR any SET session provided after 84 days
from the date of the first session and the KX modifier is not included on the claim and use the following
messages:
96- Non-covered charge(s). At least one Remark Code must be provided (may be comprised of either the NCPDP Reject
Reason [sic] Code, or Remittance Advice Remark Code that is not an ALERT.)
Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if
present.
N640 Exceeds number/frequency approved/allowed within time period.
Group Code CO (Contractual Obligation) assigning financial liability to the provider (if a claim line-item is
received with a GZ modifier indicating no signed ABN is on file and occurrence code 32 is not present).
• Contractors shall deny/reject claim lines with CPT 93668 when sessions have reached 73 sessions using the
following messages:
MSN 15.20: “The following policies NCD 20.35 were used when we made this decision.”
Spanish Version – “Las siguientes políticas NCD 20.35 fueron utilizadas cuando se tomó esta decisión.”
(Part A only) MSN 15.19: “Local Coverage Determinations (LCDs) help Medicare decide what is covered. An
LCD was used for your claim. You can compare your case to the LCD, and send information from your doctor if
you think it could change our decision. Call 1-800-MEDICARE (1-800-633-4227) for a copy of the LCD”.
Spanish Version - Las Determinaciones Locales de Cobertura (LCDs en inglés) le ayudan a decidir a Medicare lo
que está cubierto. Un LCD se usó para su reclamación. Usted puede comparar su caso con la determinación y
enviar información de su médico si piensa que puede cambiar nuestra decisión. Para obtener una copia del LCD,
llame al 1-800-MEDICARE (1800-633-4227).
CARC 119: “Benefit maximum for this time period or occurrence has been reached.”
RARC N386: “This decision was based on a National Coverage Determination (NCD). An NCD provides a
coverage determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy
of the NCD.”
Group Code PR (Patient Responsibility) assigning financial responsibility to the beneficiary (if a claim is
received with occurrence code 32 with or without a GA modifier or a claim-line is received with a GA modifier
indicating a signed ABN is on file)
Group Code CO (Contractual Obligation) assigning financial liability to the provider (if a claim line-item is
received with a GZ modifier indicating no signed ABN is on file and occurrence code 32 is not present
• Contractors shall deny claim line-items for SET, CPT 93668, when sessions have reached 73 sessions with or
without the KX Modifier present using the following messages:
MSN 15.20: “The following policies NCD 20.35 were used when we made this decision.”
Spanish Version – “Las siguientes políticas NCD 20.35 fueron utilizadas cuando se tomó esta decisión.”
(Part A only) MSN 15.19: “Local Coverage Determinations (LCDs) help Medicare decide what is covered. An
LCD was used for your claim. You can compare your case to the LCD, and send information from your doctor if

you think it could change our decision. Call 1-800-MEDICARE (1-800-633-4227) for a copy of the LCD”.
Spanish Version - Las Determinaciones Locales de Cobertura (LCDs en inglés) le ayudan a decidir a Medicare lo
que está cubierto. Un LCD se usó para su reclamación. Usted puede comparar su caso con la determinación y
enviar información de su médico si piensa que puede cambiar nuestra decisión. Para obtener una copia del LCD,
llame al 1-800- MEDICARE (1800-633-4227).
CARC 119: “Benefit maximum for this time period or occurrence has been reached.”
RARC N386: “This decision was based on a National Coverage Determination (NCD). An NCD provides a
coverage determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy
of the NCD.”
Group Code PR (Patient Responsibility) assigning financial responsibility to the beneficiary (if a claim is
received with occurrence code 32 with or without a GA modifier or a claim-line is received with a GA modifier
indicating a signed ABN is on file)
Group Code CO (Contractual Obligation) assigning financial liability to the provider (if a claim line-item is
received with a GZ modifier indicating no signed ABN is on file and occurrence code 32 is not present).
400 - Chimeric Antigen Receptor (CAR) T-cell Therapy
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
T-cells employ a number of mechanisms to fight abnormal cells such as cancer. One type of therapy that leverages the
immune system, immunotherapy, is Chimeric Antigen Receptor (CAR) T-cell therapy. CAR T-cells have been
genetically altered in order to improve the ability of the T-cells to fight cancer.
400.1 - Coverage Requirements
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
Effective for services performed on or after August 7, 2019, the Centers for Medicare & Medicaid Services (CMS)
covers autologous treatment for cancer with T-cells expressing at least one CAR when administered at healthcare
facilities enrolled in the Food and Drug Administration (FDA) risk evaluation and mitigation strategies (REMS) and
used for a medically accepted indication as defined at Social Security Act (the Act) section 1861(t)(2), i.e., is used for
either an FDA-approved indication (according to the FDA-approved label for that product), or for other uses when the
product has been FDA-approved and the use is supported in one or more CMS-approved compendia. See Publication
100-03, National Coverage Determination (NCD) Manual 110.24 for complete coverage criteria. See the following
websites for specific REMS facility information:
Kymriah® https://www.us.kymriah.com/treatment-center-locator
Yescarta® https://www.yescarta.com/find-a-treatment-center
Tecartus™ https://www.tecartus.com/hcp/treatment-center-locator
Breyanzi® https://www.celltherapy360.com/locations
ABECMA® https://www.celltherapy360.com/locations
CARVYKTI™ https://www.carvyktihcp.com/treatment-centers
NOTE: The use of allogenic T-cells from healthy donors are not autologous CAR T-cell treatments and shall not be
billed as autologous CAR T-cell treatments.
400.2 - Billing Requirements
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
Effective for dates of service on or after August 7, 2019, contractors shall pay for line-item professional claims from
approved providers for the administration of autologous treatment for cancer with T-cells expressing at least one CAR
with Current Procedural Terminology (CPT) code 0540T.
Contractors shall not require the NCD 110.24 -KX modifier and diagnosis codes for clinical trials under NCD 310.1.
These claims shall be billed with the NCT number for the specific trial, the -Q0 clinical trial modifier, and the Z00.6
clinical trial diagnosis code on the 0540T claim line effective for dates of service on or after August 7, 2019.
For Part A Outpatient (OPPS) contractors shall not require NCD 110.24 REMS facility and diagnosis codes for CAR T-
cell therapy CPT code 0540T in clinical trials under NCD 310.1 billed with the NCT number for the specific trial, the -
Q0 clinical trial modifier, condition code 30, value code D4, and the Z00.6 clinical trial diagnosis code effective for
dates of service on or after August 7, 2019.
400.2.1 - A/B Medicare Administrative Contractor (MAC) (A) Bill Types
(Rev. 10891, Issued: 07-20-21, Effective: 08-07-19, Implementation: 09-20-21)
Valid type of bills (TOBs) for billing inpatient CAR T-cell therapy services may include (but are not necessarily limited
to):
011x – Inpatient Hospital
012x – Inpatient Ancillary Hospital
Valid TOBs for billing outpatient CAR T-cell therapy services may include (but are not necessarily limited to):
013x – Outpatient Hospital
085x – Critical Access Hospital
400.2.2 - A/B MAC (A) Revenue Code
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
The following Revenue Codes are used for billing inpatient and outpatient CAR T-cell therapy services:
0871 – Cell Collection w/CPT code 0537T
0872 – Specialized Biologic Processing and Storage – Prior to Transport w/CPT code 0538T
0873 – Storage and Processing after Receipt of Cells from Manufacturer w/CPT code 0539T
0874 – Infusion of Modified Cells w/CPT code 0540T
0891 – Special Processed Drugs – FDA Approved Cell Therapy w/ Healthcare Common Procedure Coding System
(HCPCS) codes Q2041, Q2042, C9073 (replaced with Q2053 April 1, 2021), C9076 (replaced with Q2054 October 1,
2021), C9081 (replaced with Q2055 January 1, 2022), C9098 (replaced with Q2056 October 1, 2022), or C9399
400.2.3 - A/B MAC Billing HCPCS Codes
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
The following HCPCS/CPT procedure codes are used for billing outpatient CAR T-cell therapy services:
HCPCS Code Q2041 for Axicabtagene Ciloleucel
HCPCS Code Q2042 for Tisagenlecleucel
HCPCS Code Q2053 for Brexucabtagene Autoleucel (effective April 1, 2021)
HCPCS Code Q2054 for Lisocabtagene Maraleucel (effective October 1, 2021)
HCPCS Code Q2055 for Idecabtagene Vicleucel (effective January 1, 2022)
HCPCS Code Q2056 for Ciltacabtagene Autoleucel (effective October 1, 2022)
HCPCS Code C9073 for Brexucabtagene Autoleucel (prior to April 1, 2021)
HCPCS Code C9076 for Lisocabtagene maraleucel (prior to October 1, 2021)
HCPCS Code C9081 for Idecabtagene Vicleucel (prior to January 1, 2022)
HCPCS Code C9098 for Ciltacabtagene Autoleucel (prior to October 1, 2022)
HCPCS Code C9399, J3490, J3590, or J9999 for unclassified drugs or biologicals when dose of CAR T-cell therapy
exceeds code descriptor or when other CAR T-cell therapy obtains FDA approval but has not yet received a specific
HCPCS code
CPT Code 0537T collection/handling*
CPT Code 0538T preparation for transport*
CPT Code 0539T receipt and preparation*
CPT Code 0540T the provider (physician/NPP) procedure to administer CAR T-cells
* Procedure represents the various steps required to collect and prepare the genetically modified T-cells, and these steps
are not paid separately under the Outpatient Prospective Payment System (OPPS)/Medicare Physician Fee Schedule
(MPFS).
400.2.3.1 – A/B MAC (B) Places of Service (POS)
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
The following places of service (POS) are covered for CAR T-cells product HCPCS codes (Q2041, Q2042, Q2053-
Q2056, J3490, J3590, and J9999):
11 (Office)
49 (Independent clinic)
Professional claims for the procedure to administer CAR T-cells (0540T) may include (but are not necessarily limited
to):
11 (Office)
19 (Off Campus-Outpatient Hospital)
21 (Inpatient Hospital)
22 (On Campus-Outpatient Hospital)
49 (Independent Clinic)
400.2.4 - A/B MAC Diagnosis and Procedure Code Requirements
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
Please see NCD spreadsheet for the applicable International Classification of Disease (ICD)-10-CM diagnosis codes for
CAR T-cell therapy coverage.
The following are the applicable ICD-10-PCS procedure codes for CAR T-cell therapy coverage for inpatient claims:
For dates of service on or after October 1, 2021:
CARVYKTI™ - XW033A7: Introduction of Ciltacabtagene Autoleucel into Peripheral Vein, Percutaneous Approach,
New Technology Group 7
CARVYKTI™ - XW043A7: Introduction of Ciltacabtagene Autoleucel into Central Vein, Percutaneous Approach, New
Technology Group 7
When other CAR T-cell therapy obtains FDA approval but has not yet received a specific PCS code, and for use in
clinical trials FDA-approved under NCD 310.1 – XW033C7: Introduction of Autologous Engineered Chimeric Antigen
Receptor T-cell Immunotherapy into Peripheral Vein, Percutaneous Approach, New Technology Group 7
When other CAR T-cell therapy obtains FDA approval but has not yet received a specific PCS code, and for use in
clinical trials FDA-approved under NCD 310.1 – XW043C7: Introduction of Autologous Engineered Chimeric Antigen
Receptor T-cell Immunotherapy into Central Vein, Percutaneous Approach, New Technology Group 7
Yescarta® - XW033H7: Introduction of Axicabtagene Ciloleucel Immunotherapy into Peripheral Vein, Percutaneous
Approach, New Technology Group 7
Yescarta® - XW043H7: Introduction of Axicabtagene Ciloleucel Immunotherapy into Central Vein, Percutaneous
Approach, New Technology Group 7
Kymriah® - XW033J7: Introduction of Tisagenlecleucel Immunotherapy into Peripheral Vein, Percutaneous Approach,
New Technology Group 7
Kymriah® - XW043J7: Introduction of Tisagenlecleucel Immunotherapy into Central Vein, Percutaneous Approach,
New Technology Group 7
ABECMA® - XW033K7: Introduction of Idecabtagene Vicleucel Immunotherapy into Peripheral Vein, Percutaneous
Approach, New Technology Group 7
ABECMA® - XW043K7: Introduction of Idecabtagene Vicleucel Immunotherapy into Central Vein, Percutaneous
Approach, New Technology Group 7
Tecartus™ - XW033M7: Introduction of Brexucabtagene Autoleucel Immunotherapy into Peripheral Vein,
Percutaneous Approach, New Technology Group 7
Tecartus™ - XW043M7: Introduction of Brexucabtagene Autoleucel Immunotherapy into Central Vein, Percutaneous
Approach, New Technology Group 7
Breyanzi® - XW033N7: Introduction of Lisocabtagene Maraleucel Immunotherapy into Peripheral Vein, Percutaneous
Approach, New Technology Group 7
Breyanzi® - XW043N7: Introduction of Lisocabtagene Maraleucel Immunotherapy into Central Vein, Percutaneous
Approach, New Technology Group 7
For dates of service prior to October 1, 2021:
Yescarta®, ABECMA®, Kymriah® - XW033C3: Introduction of Engineered Autologous Chimeric Antigen
Receptor T-cell Immunotherapy into Peripheral Vein, Percutaneous Approach, New Technology Group 3
Yescarta®, ABECMA®, Kymriah® - XW043C3: Introduction of Engineered Autologous Chimeric Antigen
Receptor T-cell Immunotherapy into Central Vein, Percutaneous Approach, New Technology Group 3
Tecartus™ - XW23346 - Transfusion of Brexucabtagene Autoleucel Immunotherapy into Peripheral Vein,
Percutaneous Approach, New Technology Group 6
Tecartus™ - XW24346 - Transfusion of Brexucabtagene Autoleucel Immunotherapy into Central Vein, Percutaneous
Approach, New Technology Group 6
Breyanzi® - XW23376 – Transfusion of lisocabtagene maraleucel immunotherapy into peripheral vein, percutaneous
approach, new technology group 6
Breyanzi®- XW24376 – Transfusion of lisocabtagene maraleucel immunotherapy into central vein, percutaneous
approach, new technology 6
NOTE: Since allogenic T-cells are by definition not autologous CAR T-cells, it is inappropriate to use any of the above
autologous CAR T-cell ICD-10 PCS procedure codes for allogenic T-cell treatments.
For Part A Inpatient contractors shall not require NCD 110.24 REMS facility and diagnosis codes for autologous CAR
T-cell therapy ICD-10-PCS codes XW033A7/XW043A7, XW033H7/XW043H7, XW033J7/XW043J7,
XW033K7/XW043K7, XW033M7/XW043M7, and XW033N7/XW043N7 in clinical trials under NCD 310.1 billed
with the NCT number for the specific trial, condition code 30, value code D4, and the Z00.6 clinical trial diagnosis code
effective for dates of service on or after August 7, 2019.
400.2.5 – Billing Information for Professional Claims
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
Professional claims for CAR T-cell therapy and related services are billed using the Form CMS-1500 or 837P following
instructions in chapter 12 of this manual (www.cms.hhs.gov/manuals/104_claims/clm104index.asp).
Contractors shall pay professional claims for CAR T-cell therapy when the service is administered at a healthcare
facility that is enrolled in the REMS program as a REMS participating site. Contractors shall use the CMS HCPCS
Website for current HCPCS codes, https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/HCPCS-Quarterly-
Update, and the individual REMS facility websites noted at section 400.1.
Contractors shall create an edit that only allows CAR T-cell therapy services to be submitted by, or performed in, an
FDA REMS approved facility when the line item has a -KX modifier appended. Note: When a provider submits a -KX
modifier on CAR T-cell therapy services, they are acknowledging that the service is being submitted by or performed in
an FDA REMS approved facility.
Contractors shall create an edit that only allows CAR T-cell therapy services when the line item has a -LU modifier
appended in addition to a -KX modifier. Note: When a provider submits an -LU modifier on a CAR T-cell claim, it
informs the MAC that the service is fractionated. The total units shall not exceed 1 unit.
Contractors shall set up their systems to allow fractionated units on multiple claims for CAR T-cell products on the same
DOS. These claims should suspend for proper adjudication of payment.
The total payment will be divided by 10 and the provider will need to bill in 0.1 unit fractions. The provider will need to
bill a total of 10 fractional units to reach the total Medicare allowed payment amount.
Example: CAR T-cell product allowed payment $445,000:
0.2 units = $89,000.06
0.2 units = $89,000.00
0.2 units = $88,999.99
0.2 units = $88,999.98

0.2 units = $88,999.97
Note: Contractors shall only pay up to 1 unit, anything exceeding 1 unit must be denied.
For CAR T-cell products when the dose exceeds the code descriptor, use HCPCS code J3490, J3590, or J9999 for the
exceeded dosage. Include the CAR T-cell product name and the exceeded dosage in Block 19 of the 1500 claim form or
its electronic equivalent.
Example: CAR T-cell product with dose exceeded allowed payment $150,000:
0.5 units = $74,999.00
0.5 units = $75,001.00
For CAR T-cell products when the dose exceeds the code descriptor, the provider would bill a total of 1 unit of the Q
code plus a total of 1 unit of the J code.
For example, Q2041 Axicabtagene ciloleucel, up to 200 million autologous anti-CD19 CAR positive T- cells. If the
provider gives 300 million cells, they will bill:
Q2041 for 0.1 fraction $42,294.00 x10 for 200 million cells (total $422,940.00)
J9999 for 0.2 fractions $42,294.00 x5 for 100 million cells (total $211,470.00)
NOTE: The FDA labels for CAR T-cell products state the maximum number of cells that are to be infused. The HCPCS
code descriptors for Q2041, Q2042, Q2053, Q2054, Q2055, and Q2056 all align with the FDA label maximum number
of cells that are to be infused. If a provider exceeds the HCPCS code descriptor number of cells, this is off label use.
This should be extremely rare.
Contractors shall allow a -76 modifier (repeat procedure or service by same physician or other qualified healthcare
professional) on subsequent claims billed on the same date of service to assist with preventing duplicate denials.
400.3 - Payment Requirements
(Rev. 10891, Issued: 07-20-21, Effective: 08-07-19, Implementation: 09-20-21)
Inpatient
The A/ B MAC billing requirements will allow for CAR T-cell therapy when the services are submitted on the
following TOB: 11X. Type of facility and setting determines the basis of payment:
For services performed in inpatient hospitals, TOB 11X, under the Inpatient PPS is based on the Medicare
Severity-Diagnosis Related Group (MS-DRG).
For services performed in Critical Access Hospital (CAH) inpatient TOB 11X, payment is based on 101% of
reasonable cost.
Outpatient
The A/B MAC billing requirements will pay for CAR T-cell therapy when the services are submitted on the TOBs:
13X and 85x. Type of facility and setting determines the basis of payment:
For services performed in hospital outpatient departments (HOPDs), TOBs 13X, or inpatient ancillary TOB 12X,
payment is based on OPPS.
For services performed in CAH OPDs, TOB 85X, payment is based on reasonable cost.
For services performed in CAH Method II with revenue code 096X, 097X, and 098X, TOB 85X, payment is based
on the lesser of the actual charge or the Medicare Physician Fee Schedule (115% of the lesser of the fee schedule
amount and submitted charge).
HOPDs may report CPT codes 0537T, 0538T, and 0539T to allow tracking of these services when furnished in the
outpatient setting. Medicare will reject these lines as Medicare does not separately pay for these services under the
OPPS.
These following scenarios present further clarification on how to report items and services related to CAR-T in various
clinical scenarios.
Scenario 1: CAR-T Dosing and Preparation Services and Viable T-cells Administered in HOPDs:
In instances when you administer the CAR-T drug in the HOPD setting, report CPT code 0540T for the administration
and HCPCS Q2041, Q2042, Q2053 (effective April 1, 2021), C9073 (prior to April 1, 2021), C9076, or, if a more
specific code is unavailable, the most appropriate unclassified drug code (e.g., C9399 for unclassified drugs or
biologicals). NOTE: the drug codes will be denied as a Part A service even if billed with the administration.) For
specific instructions on billing unclassified drug codes, refer to Chapter 26, Section 10.4 of the “Medicare Claims
Processing Manual” on the CMS website at: Regulations-and-Guidance.Ch26. As discussed in the Calendar Year (CY)
2019 OPPS/Ambulatory Surgery Center final rule (83 FR 58904), the procedures described by CPT 0537T
(collection/handling), 0538T (preparation for transport), and 0539T (receipt and preparation) represent the various
steps required to collect and prepare the genetically modified T-cells, and these steps are not paid separately under the
OPPS. However, you may report the charges for these various steps to collect and prepare the CAR T-cells separately
and Medicare will reject them on the HOPD claim, or they may be included in the charge reported for the biological.
Note: When including the charges for collection and preparation of the CAR T-cells in the charge for the CAR-T
product, outpatient providers should code the CAR-T product service on the date that the CAR-T administration took
place and not on the date when the cells were collected.
Scenario 2: CAR-T Dosing and Preparation Services Administered in HOPD Setting, but Viable T-cells Not
Administered:
In instances when the CAR-T drug is not ultimately administered to the beneficiary, but the CAR-T preparation services
are initiated or performed in the HOPD facility, the hospital may not report the drug Q code (which only applies when
the T-cells are administered in the HOPD setting). HOPDs may report CPT 0537T, 0538T, and 0539T (as appropriate)
and the charges associated with each code under the appropriate revenue code on the HOPD claim. Medicare will reject
these codes.
Scenario 3: CAR-T Dosing and Preparation Services Administered in HOPD Setting, but Viable T-cells
Administered in the Hospital Inpatient Setting:
When CAR T-cell preparation services are initiated and furnished in the HOPD setting, but the CAR T-cells are
administered in the inpatient setting, the hospital may not report the drug Q code (which only applies when the T-cells
are administered in the HOPD setting). Report the charge associated with the various steps to collect and prepare the
CAR T-cells on the inpatient claim (TOB 11x) separately using revenue codes 0871, 0872, or 0873. Alternatively, the
hospital may include the charges for these various steps in the charge reported for the biological using revenue code
0891 – Special Processed Drugs – FDA (U.S. Food and Drug Administration) Approved Cell Therapy – Charges for
Modified cell therapy.
Note: When the cells are collected in the HOPD setting and the CAR-T is administered in the hospital inpatient
setting, inpatient providers should report the date that the CAR-T administration took place and not the date the cells
were collected.
Physician Office or Non-Hospital Clinic
The A/B MAC billing requirements will pay for CAR T-cell therapy when the services are submitted on the Form
CMS-1500 or electronic 837P.
Scenario 1: CAR-T Dosing and Preparation Services and Viable T-cells Administered in Physician Office or Non-
Hospital Clinic:
In instances when you administer the CAR-T drug in the physician office setting or other non-hospital clinic setting
that is enrolled in the REMS program as a REMS participating site, report CPT code 0540T for the administration and
HCPCS Q2041, Q2042, Q2053 (effective April 1, 2021), C9073 (prior to April 1, 2021), C9076, or, if a more specific
code is unavailable, the most appropriate unclassified drug code (e.g., J3590 for unclassified biologics). For specific
instructions on billing unclassified drug codes, refer to Chapter 26, Section 10.4 of the “Medicare Claims Processing
Manual” on the CMS website at: Regulations-and-Guidance.Ch26.
The procedures described by CPT 0537T (collection/handling), 0538T (preparation for transport), and 0539T (receipt
and preparation) represent the various steps required to collect and prepare the genetically modified T-cells, and these
steps are not paid separately under the MPFS. However, you may report them separately, and Medicare will reject
them on the professional claim.
Note: Practitioners should code the CAR-T product service on the date that the CAR-T administration took place and
not on the date when the cells were collected.
Scenario 2: CAR-T Dosing and Preparation Services Administered in Physician Office or Non-Hospital Clinic,
but Viable T-cells Not Administered:
In instances when the CAR-T drug is not ultimately administered to the beneficiary, but the CAR-T preparation services
are initiated or performed in the physician office or other non-hospital clinic facility, the practitioner may not report the
drug HCPCS code (which only applies when the T-cells are administered in the setting). The practitioner may report
CPT 0537T, 0538T, and 05(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
Inpatient
The A/ B MAC billing requirements will allow for CAR T-cell therapy when the services are submitted on the following
TOB: 11X. Type of facility and setting determines the basis of payment:
For services performed in inpatient hospitals, TOB 11X, under the Inpatient PPS is based on the Medicare Severity-
Diagnosis Related Group (MS-DRG).
For services performed in Critical Access Hospital (CAH) inpatient TOB 11X, payment is based on 101% of reasonable
cost.
Outpatient
The A/B MAC billing requirements will pay for CAR T-cell therapy when the services are submitted on the TOBs: 13X
and 85x. Type of facility and setting determines the basis of payment:
For services performed in hospital outpatient departments (HOPDs), TOBs 13X, or inpatient ancillary TOB 12X,
payment is based on OPPS.
For services performed in CAH OPDs, TOB 85X, payment is based on reasonable cost.
For services performed in CAH Method II with revenue code 096X, 097X, and 098X, TOB 85X, payment is based on
the lesser of the actual charge or the Medicare Physician Fee Schedule (115% of the lesser of the fee schedule amount
and submitted charge).
HOPDs may report CPT codes 0537T, 0538T, and 0539T to allow tracking of these services when furnished in the
outpatient setting. Medicare will reject these lines as Medicare does not separately pay for these services under the
OPPS.
These following scenarios present further clarification on how to report items and services related to CAR T-cells in
various clinical scenarios.
Scenario 1: CAR T-cell Dosing and Preparation Services and Viable T-cells Administered in HOPDs:
In instances when a physician or non-physician provider administers the CAR T-cell product in the HOPD setting, report
CPT code 0540T for the administration. The HOPD reports CAR T-cell product HCPCS code Q2041, Q2042, Q2053
(effective April 1, 2021), C9073 (prior to April 1, 2021), Q2054 (effective October 1, 2021), C9076 (prior to October 1,
2021), Q2055 (effective January 1, 2022), C9081 (prior to January 1, 2022), Q2056 (effective October 1, 2022), C9098
(prior to October 1, 2022), or, if a more specific code is unavailable, the most appropriate unclassified drug code (e.g.,
C9399 for unclassified drugs or biologicals). For specific instructions on billing unclassified drug codes, refer to Chapter
26, Section 10.4 of the “Medicare Claims Processing Manual” on the CMS website at: Regulations-and-Guidance.Ch26.
As discussed in the Calendar Year (CY) 2019 OPPS/Ambulatory Surgery Center final rule (83 FR 58904), the
procedures described by CPT codes 0537T (collection/handling), 0538T (preparation for transport), and 0539T (receipt
and preparation) represent the various steps required to collect and prepare the genetically modified T-cells, and these
steps are not paid separately under the OPPS. However, you may report the charges for these various steps to collect and
prepare the CAR T-cells separately and Medicare will reject them on the HOPD claim, or they may be included in the
charge reported for the biological.
Note: When including the charges for collection and preparation of the CAR T-cells in the charge for the CAR T-cell
product, outpatient providers should code the CAR T-cell product service on the date that the CAR T-cell administration
took place and not on the date when the cells were collected.
Scenario 2: CAR T-cell Dosing and Preparation Services in HOPD Setting, but Viable T-cells Not Administered:
In instances when the CAR T-cell product is not ultimately administered to the beneficiary, but the CAR T-cell
preparation services are initiated or performed in the HOPD facility, the hospital shall not report the CAR T-cell product
HCPCS code (which only applies when viable T-cells are administered). HOPDs may report CPT codes 0537T, 0538T,
and 0539T (as appropriate) and the charges associated with each code under the appropriate revenue code on the HOPD
claim. Medicare will reject these codes.
Scenario 3: CAR T-cell Dosing and Preparation Services in HOPD Setting, but Viable T-cells Administered in the
Hospital Inpatient Setting:
When CAR T-cell preparation services are initiated and furnished in the HOPD setting, but the CAR T-cells are
administered in the inpatient setting, the hospital shall not report the CAR T-cell product HCPCS code (which only
applies when viable T-cells are administered in the outpatient setting). Report the charge associated with the various
steps to collect and prepare the CAR T-cells on the inpatient claim (TOB 11x) separately using revenue codes 0871,

0872, or 0873. Alternatively, the hospital may include the charges for these various steps in the charge reported for the
biological using revenue code 0891 – Special Processed Drugs – FDA (U.S. Food and Drug Administration) Approved
Cell Therapy – Charges for Modified cell therapy.
Note: When the cells are collected in the HOPD setting and the CAR T-cell product is administered in the hospital
inpatient setting, inpatient providers shall report the date that the CAR T-cell administration took place and not the date
the cells were collected.
Physician Office or Non-Hospital Clinic
The A/B MAC billing requirements will pay for CAR T-cell therapy products when the services are submitted in places
of service 11 or 49. Proper adjudication of payment is based on fractionated units.
The A/B MAC billing requirements will pay for CAR T-cell therapy when the services are submitted on the Form CMS-
1500 or electronic 837P.
Scenario 1: CAR T-cell Dosing and Preparation Services and Viable T-cells Administered in Physician Office or
Non-Hospital Clinic:
In instances when a physician or non-physician provider administers the CAR T-cells product in the physician office
setting or other non-hospital clinic setting that is enrolled in the REMS program as a REMS participating site, report
CPT code 0540T for the administration and CAR T-cell product HCPCS code Q2041, Q2042, Q2053 (effective April 1,
2021), Q2054 (effective October 1, 2021), Q2055 (effective January 1, 2022), Q2056 (effective October 1, 2022), or, if a
more specific code is unavailable, the most appropriate unclassified drug code (e.g., J3590 for unclassified biologics).
For specific instructions on billing unclassified drug codes, refer to Chapter 26, Section 10.4 of the “Medicare Claims
Processing Manual” on the CMS website at: Regulations-and-Guidance.Ch26.
The procedures described by CPT codes 0537T (collection/handling), 0538T (preparation for transport), and 0539T
(receipt and preparation) represent the various steps required to collect and prepare the genetically modified T-cells, and
these steps are not paid separately under the MPFS. However, you may report them separately, and Medicare will deny
them on the professional claim as Medicare does not pay separately for this service.
Note: Practitioners shall code the CAR T-cell product service on the date that the CAR T-cells administration took place
and not on the date when the cells were collected.
Scenario 2: CAR T-cells Dosing and Preparation Services in Physician Office or Non-Hospital Clinic, but Viable
T-cells Not Administered:
In instances when the CAR T-cell product is not ultimately administered to the beneficiary, but the CAR T-cells
preparation services are initiated or performed in the physician office or other non-hospital clinic facility, the practitioner
shall not report the CAR T-cell product HCPCS code (which only applies when viable T-cells are administered). The
practitioner may report CPT codes 0537T, 0538T, and 0539T (as appropriate) on the professional claim. Medicare will
deny these codes as Medicare does not pay separately for this service.
Scenario 3: CAR T-cells Dosing and Preparation Services in Physician Office or Non-Hospital Clinic, but Viable
T-cells Administered in the Hospital Inpatient Setting:
When CAR T-cell preparation services are initiated and furnished in the physician office or other non-hospital clinic
setting, but the CAR T-cells are administered in the hospital inpatient setting, the practitioner shall not report the CAR
T-cells product HCPCS code (which only applies when viable T-cells are administered in the outpatient setting). The
hospital that administers the T-cells will report the charge associated with the various steps to collect and prepare the
CAR T-cells on the inpatient claim (TOB 11x) separately using revenue codes 0871, 0872, or 0873. Alternatively, the
hospital may include the charges for these various steps in the charge reported for the biological using revenue code
0891 – Special Processed Drugs – FDA (U.S. Food and Drug Administration) Approved Cell Therapy – Charges for
Modified cell therapy.
Note: When the cells are collected in the physician office setting and the CAR T-cell product is administered in the
hospital inpatient setting, inpatient providers shall report the date that the CAR T-cell administration took place and not
the date the cells were collected.
Scenario 4: CAR T-cells Dosing and Preparation Services in Physician Office or Non-Hospital Clinic, but Viable
T-cells Administered in the HOPD Setting:
When CAR T-cell preparation services are initiated and furnished in the physician office or other non-hospital clinic
setting, but the CAR T-cells are administered in the HOPD setting, the practitioner shall not report the CAR T-cell
product HCPCS code (which only applies when the viable T-cells are administered). The HOPD that administers the T-
cells may report CPT codes 0537T, 0538T, and 0539T (as appropriate) and the charges associated with each code under
the appropriate revenue code on the HOPD claim. Medicare will reject these codes.
Note: When the cells are collected in the physician office setting and the CAR T-cell product is administered in the
HOPD setting, HOPD providers shall report the date that the CAR T-cell administration took place and not the date the
cells were collected.
39T (as appropriate) on the professional claim. Medicare will reject these codes.
Scenario 3: CAR-T Dosing and Preparation Services Administered in Physician Office or Non-Hospital Clinic,
but Viable T-cells Administered in the Hospital Inpatient Setting:
When CAR T-cell preparation services are initiated and furnished in the physician office or other non-hospital clinic
setting, but the CAR T-cells are administered in the inpatient setting, the practitioner may not report the drug HCPCS
code (which only applies when the T-cells are administered in the setting). The hospital that administers the T-cells will
report the charge associated with the various steps to collect and prepare the CAR T-cells on the inpatient claim (TOB
11x) separately using revenue codes 0871, 0872, or 0873. Alternatively, the hospital may include the charges for these
various steps in the charge reported for the biological using revenue code 0891 – Special Processed Drugs – FDA (U.S.
Food and Drug Administration) Approved Cell Therapy – Charges for Modified cell therapy.
Note: When the cells are collected in the physician office setting and the CAR-T is administered in the hospital
inpatient setting, inpatient providers should report the date that the CAR-T administration took place and not the date
the cells were collected.
400.4 - Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes
(RARCs), Group Codes, and Medicare Summary Notice (MSN) Messages
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
Contractors shall continue to use the appropriate existing messages that they have in place when denying claims
submitted that do not meet the Medicare coverage criteria for CAR T-cell therapy.
--Contractors shall deny claims for CAR T-cell therapy when the service is not administered through healthcare
facilities that are enrolled in the FDA REMS requirements using the following messages:
CARC 58 Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service.
Usage: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if
present.
RARC N386 – This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy of the
NCD.
Group Code CO (Contractual Obligations).
MSN 16.2 – This service cannot be paid when provided in this location/facility.
Spanish Version – Este servicio no se puede pagar cuando es suministrado en esta sitio/facilidad.
In addition to the codes listed above, contractors shall afford appeal rights to all denied parties.
--When denying claims for covered CAR T-cell therapy procedures because the appropriate ICD-10 coding was
not used, use the following messages:
CARC 50 - These are non-covered services because this is not deemed a "medical necessity" by the payer. Usage: Refer
to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy of the
NCD.
Group Code CO or PR dependent upon liability.
MSN 15.20 - “The following polices were used when we made this decision: NCD 110.24.”
Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión: NCD 110.24.”
--When denying claims for covered CAR T-cell therapy procedures because they are not performed in POS 11 or
49, use the following messages:
CARC 58 Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service.
Usage: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if
present.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy of the
NCD.
Group Code CO or PR (Patient Responsibility) dependent upon liability. (Use PR when the GA modifier is appended to
the line item).
MSN 09.040 - This item or service was denied because information required to make payment
was incorrect.
MSN 15.20 - “The following polices were used when we made this decision: NCD 110.24.”

Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión: NCD 110.24.”
--When denying claims for covered CAR T-cell therapy procedures because they do not contain new modifier -
LU, use the following messages:
CARC 4 - The procedure code is inconsistent with the modifier used. Usage: Refer to the 835 Healthcare Policy
Identification Segment (loop 2110 Service Payment Information REF), if present.
RARC N386 - This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage
determination as to whether a particular item or service is covered. A copy of this policy is available at
www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy of the
NCD.
Group Code CO
MSN 15.20 - “The following polices were used when we made this decision: NCD 110.24.”
Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión: NCD 110.24.”
--When denying claims for covered CAR T-cell therapy procedures because the fractional units exceed 1 unit, use
the following messages:
CARC 151 - Payment adjusted because the payer deems the information submitted does not support this many/frequency
of services.
Group Code CO
MSN 15.060 - The information provided does not support the need for this many services or items within this period of
time.
Spanish Version - (La información proporcionada no confirma la necesidad de estos servicios o artículos en este periodo
de tiempo.)
-- Contractors shall reject claims for allogeneic CAR T-cell therapy ICD-10-PCS codes XW033G7 and XW043G7
and autologous CAR T-cell therapy ICD-10-PCS codes XW033C7 and XW043C7 when not billed for clinical
trials under NCD 310.1 with the NCT number for the specific trial, condition code 30, value code D4, and the
Z00.6 clinical trial diagnosis code effective for dates of service on or after October 1, 2021, using the following
messages:
CARC 55: Procedure/treatment/drug is deemed experimental/investigational by the payor.
Group Code: CO
MSN 16.77 – This service/item was not covered because it was not provided as part of a qualifying trial/study.
Spanish Version – (Este servicio/artículo no fue cubierto porque no estaba incluido como parte de un ensayo
clínico/estudio calificado.)
In addition to the codes listed above, contractors shall afford appeal rights to all denied parties.

400.5 - Claims Editing
(Rev. 11721; Issued: 11-28-22; Effective: 01-01-23; Implementation: 01-03-23)
A. Fee-For-Service Medicare
Medicare edits CAR T-cell therapy claims based on requirements found in NCD 110.24.
B. Beneficiaries enrolled in Medicare Advantage (MA) plans
Effective for clams with dates of service on and after August 7, 2019, CMS determined that the NCD requiring coverage
of CAR T-cell therapy for cancer is a significant cost under section 422.109(a)(2) of title 42 of the Code of Federal
Regulations. As a result, for CYs 2019 (beginning August 7, 2019) and 2020 only, original fee-for-service Medicare will
pay for CAR T-cell therapy for cancer obtained by beneficiaries enrolled in Medicare Advantage (MA) plans when the
coverage criteria outlined in the NCD are met. Plans should account for CAR T-cell therapy for cancer items and
services in their contract year 2021 bids.
Consistent with §1862 (t)(2) of the Act, MACs will pay for CAR T-cell therapy for cancer for Medicare beneficiaries
enrolled in MA plans in CYs 2019 (beginning August 7, 2019) and 2020.
410 – Acupuncture for Chronic Low Back Pain (cLBP)
(Rev. 10337, Issued: 08-027-20, Effective: 01-21-20, Implementation: 06-24 - 20 - A/B MACs; 10-05-20-SSM
Edits; 01- 04-21 - BR 13 CWF only)
Acupuncture is the selection and manipulation of specific acupuncture points through the insertion of needles or
“needling,” or other “non-needling” techniques focused on these points.
410.1 - Coverage Requirements
(Rev. 10337, Issued: 08-027-20, Effective: 01-21-20, Implementation: 06-24 - 20 - A/B MACs; 10-05-20-SSM
Edits; 01- 04-21 - BR 13 CWF only)
Effective for services on or after January 21, 2020, the Centers for Medicare & Medicaid Services (CMS) will cover
acupuncture for chronic low back pain (cLBP) under section 1862(a)(1)(A) of the Social Security Act. Up to 12 visits in
90 days are covered for Medicare beneficiaries under the following circumstances:
• For the purpose of this decision, cLBP is defined as:
o Lasting 12 weeks or longer;
o nonspecific, in that it has no identifiable systemic cause (i.e., not associated with metastatic, inflammatory,
infectious, etc. disease);
o not associated with surgery; and
o not associated with pregnancy.
• An additional 8 sessions will be covered for those patients demonstrating an improvement. No more than 20
acupuncture treatments may be administered annually. Example: If the 1st service is performed on March 21, 2020,
the next service beginning a new year cannot be performed until March 1, 2021. This means 11 full months must
pass from the date of the 1
st
service before eligibility begins again.
All types of acupuncture including dry needling for any condition other than cLBP are non-covered by Medicare.
410.2 – Claims Processing General Information
(Rev. 10337, Issued: 08-027-20, Effective: 01-21-20, Implementation: 06-24 - 20 - A/B MACs; 10-05-20-SSM
Edits; 01- 04-21 - BR 13 CWF only)
Effective for claims with dates of service (DOS) on or after January 21, 2020, contractors shall recognize acupuncture
for cLBP services reported with CPT codes 97810, 97811, 97813, 97814, 20560, and 20561 as covered services under
National Coverage Determination (NCD) 30.3.3 no more than 20 times per annum.
NOTE: If the 1st service is performed on March 21, 2020, the next service beginning a new year cannot be performed
until March 1, 2021, 11 full months following the 1
st
service.
The attached includes the International Classification of Diseases (ICD)-10 diagnosis codes are applicable and must be
reported for acupuncture for cLBP services:
Contractors shall accept and process acupuncture for cLBP claims with the -KX modifier for the 13th through 20th
service per annum.
NOTE: The 1st through 12th service over a 90-day period do not require the –KX modifier. There is a 20 service
maximum per annum for this benefit.
NOTE: By applying the -KX modifier to the claim, the therapy provider is confirming that the additional services are
medically necessary as justified by appropriate documentation in the medical record.
410.3 – Institutional Claims Bill Type and Revenue Coding Information
(Rev. 10337, Issued: 08-027-20, Effective: 01-21-20, Implementation: 06-24 - 20 - A/B MACs; 10-05-20-SSM
Edits; 01- 04-21 - BR 13 CWF only)
Effective for claims with DOS on or after January 21, 2020, contractors shall recognize acupuncture for cLBP services
reported on institutional claims on types of bill (TOBs) 12X, 13X, 71X, 77X, and 85X (and revenue codes not equal to
096X, 097X, and 098X for CAH Method I).
Effective for claims with DOS on or after January 21, 2020, contractors shall recognize acupuncture for cLBP services
reported with Revenue Code 0940 on institutional claims.
Effective for claims with DOS on or after January 21, 2020, contractors shall recognize acupuncture for cLBP services
reported on institutional claims on TOB 12X, 71X, 77X 85X CAH Method II with revenue codes 096X, 097X, and
098X.
410.4 – Messaging
(Rev. 10337, Issued: 08-027-20, Effective: 01-21-20, Implementation: 06-24 - 20 - A/B MACs; 10-05-20-SSM
Edits; 01- 04-21 - BR 13 CWF only)
Effective for claims with DOS on or after January 21, 2020, contractors shall reject/deny claims that do not contain the
appropriate diagnosis/procedure coding noted in section 410.2 and use these messages:
Claim Adjustment Reason Code (CARC) 50 - These are non-covered services because this is not deemed a 'medical
necessity' by the payer.
Remittance Advice Remark Code (RARC) M64 – Missing/incomplete/invalid other diagnosis.
Group Code CO (Contractual Obligations) or PR (Patient Responsibility) dependent on liability.
MSN 15.20 - “The following polices were used when we made this decision: NCD 30.3.3.”
Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión: NCD 30.3.3.”
NOTE: Due to system requirement, the Fiscal Intermediary Shared System (FISS) has combined messages 15.19 and
15.20 so that, when used for the same line item, both messages will appear on the same MSN.
In addition to the codes noted in section 410.2, contractors shall afford appeal rights to all denied parties.
Contractors shall return to provider/return as unprocessable claims for acupuncture for cLBP for services 13 through 20
per annum without the -KX modifier and use these messages:
CARC 4 - The procedure code is inconsistent with the modifier used or a required modifier is missing. Usage: Note:
Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
RARC N657 - This should be billed with the appropriate code for these services.
Group Code CO
Contractors shall reject/deny more than 20 claims per annum for acupuncture for cLBP and use the following messages:
CARC 96 - Non-covered charge(s). At least one Remark Code must be provided (may be comprised of either the
NCPDP Reject Reason [sic] Code, or Remittance Advice Remark Code that is not an ALERT.) Note: Refer to the 835
Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
RARC N640 - Exceeds number/frequency approved/allowed within time period.
Group Code - CO (Contractual Obligation)
MSN 15.20 - “The following polices were used when we made this decision: NCD 30.3.3.”
Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión: NCD 30.3.3.”
MSN 15.19: “We used a Local Coverage Determination (LCD) to decide coverage for your claim. To appeal, get a copy
of the LCD at www.cms.gov/medicare-coverage-database (use the MSN Billing Code for the CPT/HCPCS Code) and
send with information from your doctor."
Spanish Version - Usamos una Determinación de Cobertura Local (LCD) para decidir la cobertura de su reclamo. Para
apelar, obtenga una copia del LCD en www.cms.gov/medicare-coverage-database (use el código de facturación de MSN
para el código "CPT/HCPCS") y envíela con la información de su médico.
NOTE: Due to system requirements, the Fiscal Intermediary Shared System has combined messages 15.19 and 15.20 so
that, when used for the same line item, both messages will appear on the same MSN.
410.5 – Common Working File (CWF) FISS, and Multi-Carrier System (MCS) Editing
(Rev. 10337, Issued: 08-027-20, Effective: 01-21-20, Implementation: 06-24 - 20 - A/B MACs; 10-05-20-SSM
Edits; 01- 04-21 - BR 13 CWF only)
The Common Working File (CWF) shall create a new reject for claims with DOS on and after January 21, 2020, for
claims received on or after October 5, 2020, to not allow payment for more than 20 acupuncture for cLBP claims per
annum.
For acupuncture for cLBP claims CWF, FISS and the Multi-Carrier System (MCS) shall apply appropriate updates to the
Next Eligibility Date file for DOS on or after January 21, 2020.
NOTE: Appropriate updates include modifications to HUQA, and Extract Records on the Next Generation Desktop
(NGD) and the Medicare Beneficiary Database (MBD) for next eligible date and services remaining.
CWF shall count 11 full months starting with the month of a beneficiary’s 1
st
acupuncture for cLBP service. EX: If 1
st
date of service is October 15, 2020, the next eligible date beginning a new year would be October 1, 2021.
NOTE: A new cLBP auxiliary (AUX) file will be created and HIMR will be updated to post the previous acupuncture
for cLBP HCPCS 97810, 97811, 97813, 97814, 20560, or 20561.
For acupuncture for cLPB claims with DOS on and after January 21, 2020, the Multi-Carrier System Desktop Tool shall
display the acupuncture for cLBP visits in a format equivalent to the CWF HIMR screen.
Effective for claims with DOS on and after January 21, 2020, received on and after October 5, 2020, CWF shall post
acupuncture for cLBP HCPCS codes 97810, 97811, 97813, 97814, 20560, and 20561, reported on institutional claims,
TOBs 12X, 13X, 71X, 77X, and 85X (and revenue code not equal to 096X, 097X, 098X), as the technical component on
the new cLBP AUX file.
NOTE: 1 TECH and 1 PROF on same DOS represents 1 service.
NOTE: CWF shall post the Part B Professional claim line as TECH/PROF for the HCPCS if the modifier is blank.
CWF shall create a new reject for HCPCS 97810, 97811, 97813, 97814, 20560, and 20561 when a beneficiary has
reached 20 acupuncture for cLBP sessions and the -KX modifier is not included on the claim line for sessions 13 through
20 (the reject will apply for both PROF and TECH sessions).
CWF shall update the determination when any changes occur to the beneficiary master data or claims data that would
result in a change to the calculation
CWF shall create a new HICR function for the new cLBP AUX file.
411– Home Infusion Therapy Services
(Rev. 10269, Issued: 08-07-2020, Effective: 01-01-2021, Implementation: 01-04-2021)
411.1 – Policy
(Rev. 10269, Issued: 08-07-2020, Effective: 01-01-2021, Implementation: 01-04-2021)
Effective beginning on January 1, 2021, the Medicare home infusion therapy benefit covers the professional services,
including nursing services, furnished in accordance with the plan of care, patient training and education (not otherwise
covered under the durable medical equipment benefit), remote monitoring, and monitoring services for the provision of
home infusion therapy and home infusion drugs furnished by a qualified home infusion therapy supplier. Home infusion
therapy means the items and services furnished by a qualified home infusion therapy supplier, which are furnished in the
individual’s home. Payment is for an “infusion drug administration calendar day,” which means the day on which home
infusion therapy services are furnished by skilled professionals in the individual’s home on the day of infusion drug
administration. The skilled services provided on such day must be so inherently complex that they can only be safely and
effectively performed by, or under the supervision of, professional or technical personnel.

411.2 – Coverage Requirements
(Rev. 10269, Issued: 08-07-2020, Effective: 01-01-2021 Implementation: 01-04-2021)
Payment for an “infusion drug administration calendar day” is only made if a beneficiary is furnished certain drugs and
biologicals administered through an item of covered DME, and payable only to suppliers enrolled in Medicare as a
“qualified home infusion therapy supplier.” The beneficiary must be under the care of an applicable provider, defined as
a physician, nurse practitioner, or physician’s assistant, and must be under the care of a physician-established plan of
care that prescribes the type, amount, and duration of infusion therapy services. A “qualified home infusion therapy
supplier” is a pharmacy, physician, or other provider of services or supplier licensed by the state in which supplies or
services are furnished. Qualified home infusion therapy suppliers must furnish infusion therapy to individuals with acute
or chronic conditions requiring administration of home infusion drugs; ensure the safe and effective provision and
administration of home infusion therapy on a 7-day-a-week, 24-hour-a-day basis; and be accredited by an organization
designated by the Secretary. The supplier may subcontract with a pharmacy, physician, other qualified supplier or
provider of services in order to meet these requirements.
411.3 - Home Infusion Drugs: Healthcare Common Procedural Coding System (HCPCS) Drug
Codes
(Rev. 11430; Issued: 05-24-22; Effective: 07-01-22; Implementation: 07-05-22)
The home infusion therapy services payment is intended to cover the professional services needed for
the administration of certain home infusion drugs covered as supplies necessary for the effective use
of external infusion pumps. This payment separately and explicitly pays for the services related to the
administration of the drugs identified on the DME LCD for External Infusion Pumps, when such
services are furnished in the individual’s home. Section 1861(iii)(3)(C) of the Act defines “home
infusion drug” as a parenteral drug or biological administered intravenously, or subcutaneously for an
administration period of 15 minutes or more, in the home of an individual through a pump that is an
item of durable medical equipment (as defined in section 1861(n) of the Act). Such term does not
include insulin pump systems or self-administered drugs or biologicals on a self-administered drug
exclusion list.
Home infusion drugs are assigned to three payment categories, as determined by the HCPCS J-code.
Payment category 1 includes certain intravenous antifungals and antivirals, uninterrupted long-term
infusions, pain management, inotropic, chelation drugs. Payment category 2 includes subcutaneous
immunotherapy and other certain subcutaneous infusion drugs. Payment category 3 includes certain
chemotherapy drugs. CMS will continue to use the G-codes, established for the temporary
transitional payments in CYs 2019 and 2020, for the professional services furnished on an infusion
drug administration calendar day for each payment category. CMS has established a single payment
amount for each of the three categories for professional services furnished for each infusion drug
administration calendar day. Each payment category will be paid at amounts in accordance with
infusion codes and units for such codes under the physician fee schedule for each infusion drug
administration calendar day in the individual’s home for drugs assigned to such category. The
payment amounts are equal to 5 hours of infusion therapy in a physician’s office. Further policy
information can be found in Publication 100-02, Chapter 15, Section 320.
Category 1
J-Code
Description
J0133
Injection, acyclovir, 5 mg
J0285
Injection, amphotericin b, 50 mg
J0287
Injection, amphotericin b lipid complex, 10 mg

J0288
Injection, amphotericin b cholesteryl sulfate complex, 10 mg
J0289
Injection, amphotericin b liposome, 10 mg
J0895
Injection, deferoxamine mesylate, 500 mg
J1170
Injection, hydromorphone, up to 4 mg
J1250
Injection, dobutamine hydrochloride, per 250 mg
J1265
Injection, dopamine hcl, 40 mg

J1325
Injection, epoprostenol, 0.5 mg
J1455
Injection, foscarnet sodium, per 1000 mg
J1457
Injection, gallium nitrate, 1 mg
J1570
Injection, ganciclovir sodium, 500 mg
J2175
Injection, meperidine hydrochloride, per 100 mg
J2260
Injection, milrinone lactate, 5 mg
J2270
Injection, morphine sulfate, up to 10 mg
J3010
Injection, fentanyl citrate, 0.1 mg
J3285
Injection, treprostinil, 1 mg
Category 2
J-Code
Description
J1551 JB
Injection, immune globulin (cutaquig), 100mg
J1555 JB
Injection, immune globulin (cuvitru), 100 mg
J1558 JB
Injection, immune globulin (xembify), 100mg
J1559 JB
Injection, immune globulin (hizentra), 100mg
J1561 JB
Injection, immune globulin, (gamunex-c/gammaked), non-lyophilized (e.g. liquid), 500 mg
J1562 JB
Injection, immune globulin (vivaglobin), 100 mg
J1569 JB
Injection, immune globulin, (gammagard liquid), non-lyophilized, (e.g., liquid), 500 mg
J1575 JB
Injection, immune globulin/hyaluronidase, (hyqvia), 100 mg immune globulin
J7799 JB
This NOC code may be used to identify the subcutaneous immune globulin (cutaquig)
Category 3
J-Code
Description
J9000
Injection, doxorubicin hydrochloride, 10 mg
J9039
Injection, blinatumomab, 1 microgram
J9040
Injection, bleomycin sulfate, 15 units
J9065
Injection, cladribine, per 1 mg
J9100
Injection, cytarabine, 100 mg
J9190
Injection, fluorouracil, 500 mg
J9360
Injection, vinblastine sulfate, 1 mg
J9370
Injection, vincristine sulfate, 1 mg
It is important to note that this list is not static. The payment category may be determined by the
contractor for any new home infusion drug additions to the Local Coverage Determination (LCD)
for
External Infusion Pumps as identified by the following not-otherwise-classified (NOC) codes:
- J7799 - Not otherwise classified drugs, other than inhalation drugs, administered through
DME
- J7999 - Compounded drug, not otherwise classified.

Attachment A: Billing for Home Infusion Therapy Services on or After January 1, 2021
Table 1 shows the time increments providers should report visit length in 15-minute increments (15 minutes
= 1 unit). See the table below for the rounding of units:
Table 1: Time Increments
Unit
Time
1
<23 minutes
2
= 23 minutes to <38 minutes
3
= 38 minutes to <53 minutes
4
= 53 minutes to <68 minutes
5
= 68 minutes to <83 minutes
6
= 83 minutes to <98 minutes
7
= 98 minutes to <113 minutes
8
= 113 minutes to <128 minutes
9
= 128 minutes to <143 minutes
10
= 143 minutes to <158 minutes
Table 2 shows the use of the three G-codes established for the home infusion therapy benefit, and
reflects the therapy type and complexity of the drug administration.
Table 2: Payment Categories for Home Infusion Therapy Professional Services (G-Codes)
Category 1
Category 2
Category 3
Description
G-Code
Intravenous anti-infective,
pain management, chelation,
pulmonary hypertension,
inotropic, and other certain
intravenous infusion drugs
Subcutaneous
immunotherapy and
other certain
Subcutaneous infusion
drugs
Chemotherapy
and other certain
highly complex
intravenous drugs
Initial Visit
G0088
G0089
G0090
Subsequent Visit
G0068
G0069
G0070
Table 3 provides a list of J-codes associated with the home infusion drugs that fall within each category.
Table 3: Payment Categories for Home Infusion Drugs (J-Codes)
Category 1
J-Code
Description
J0133
Injection, acyclovir, 5 mg
J0285
Injection, amphotericin b, 50 mg
J0287
Injection, amphotericin b lipid complex, 10 mg
J0288
Injection, amphotericin b cholesteryl sulfate complex, 10 mg
J0289
Injection, amphotericin b liposome, 10 mg
J0895
Injection, deferoxamine mesylate, 500 mg
J1170
Injection, hydromorphone, up to 4 mg
J1250
Injection, dobutamine hydrochloride, per 250 mg
J1265
Injection, dopamine hcl, 40 mg
J1325
Injection, epoprostenol, 0.5 mg

J1455
Injection, foscarnet sodium, per 1000 mg
J1457
Injection, gallium nitrate, 1 mg
J1570
Injection, ganciclovir sodium, 500 mg
J2175
Injection, meperidine hydrochloride, per 100 mg
J2260
Injection, milrinone lactate, 5 mg
J2270
Injection, morphine sulfate, up to 10 mg
J3010
Injection, fentanyl citrate, 0.1 mg
J3285
Injection, treprostinil, 1 mg
Category 2
J-Code
Description
J1551 JB
Injection, immune globulin (cutaquig), 100mg
J1555 JB
Injection, immune globulin (cuvitru), 100 mg
J1558 JB
Injection, immune globulin (xembify), 100mg
J1559 JB
Injection, immune globulin (hizentra), 100mg
J1561 JB
Injection, immune globulin, (gamunex-c/gammaked), non-lyophilized (e.g. liquid), 500 m
J1562 JB
Injection, immune globulin (vivaglobin), 100 mg
J1569 JB
Injection, immune globulin, (gammagard liquid), non-lyophilized, (e.g., liquid), 500 mg
J1575 JB
Injection, immune globulin/hyaluronidase, (hyqvia), 100 mg immune globulin
J7799 JB
This NOC code may be used to identify the subcutaneous immune globulin (cutaquig)
Category 3
J-Code
Description
J9000
Injection, doxorubicin hydrochloride, 10 mg
J9039
Injection, blinatumomab, 1 microgram
J9040
Injection, bleomycin sulfate, 15 units
J9065
Injection, cladribine, per 1 mg
J9100
Injection, cytarabine, 100 mg
J9190
Injection, fluorouracil, 500 mg
J9360
Injection, vinblastine sulfate, 1 mg
J9370
Injection, vincristine sulfate, 1 mg
The payment category may be determined by the contractor for any
new home infusion drug additions to the Local Coverage Determination
(LCD)
for External Infusion Pumps as identified by the following not-
otherwise-classified (NOC) codes:
- J7799 - Not otherwise classified drugs, other than inhalation drugs, administered
through DME
- J7999 - Compounded drug, not otherwise classified
411.4 - Billing and Payment Requirements
(Rev. 10269, Issued: 08-07-2020, Effective: 01-01-2021, Implementation: 01-04-2021)
Contractors shall accept and pay for home infusion therapy services to eligible home infusion
therapy suppliers (new specialty D6)
effective for claim lines with dates of service on or
after January 1, 2021 using the one of the following ‘G’ codes and applicable ‘J’ codes
listed in section 411.3 of this chapter. Claims for the home infusion therapy service G-
codes are billed to the A/B MACs and are payable to home infusion therapy suppliers; this
service is no longer payable to DME suppliers. The applicable ‘J’ codes are billed to the
DME MACs by the DME supplier.
Contractors shall use Type of Service (TOS) Code 1 for all six G-codes. Contractors shall
pay only one of the G-codes per line item date of service when one of the drugs from the
applicable category is billed with the same line item date of service or a date of service
within 30 days prior to the G-code visit.
NOTE:
• The fees associated with the G-codes on the MPFSD fee file will be “a per day
rate;” therefore, the units on the line should not be multiplied by the rate.
The drug remains separately payable from the G-code line item
Home infusion therapy suppliers will report the following HCPCS G-codes associated with the
payment categories for the professional services furnished in the individual’s home and on an
infusion drug administration calendar day.
Because the home infusion therapy services are contingent upon a home infusion drug J-
code, home infusion therapy suppliers must ensure that the appropriate drug associated
with the visit is billed no more than 30 days prior to the visit. In the event that multiple
visits occur on the same date of service, or multiple drugs, which are not all assigned to the
same payment category, are administered on the same infusion drug administration
calendar day, a single payment would be made that is equal to the highest payment
category. Suppliers must only bill for one visit and should report the highest paying visit
with the applicable drug.
To differentiate the first visit from all subsequent visits, home infusion therapy suppliers
may only bill one of the “initial visit” G-codes to indicate an visit for a new patient who
had previously received their last home infusion therapy service visit more than 60 days
prior to the new initial home infusion therapy service visit.
Home infusion therapy suppliers should report visit length in 15-minute increments (15
minutes=1 unit). See the Table 1 below for the rounding of units.

Table 1: Time Increments
Unit
Time
1
<23 minutes
2
= 23 minutes to <38 minutes
3
= 38 minutes to <53 minutes
4
= 53 minutes to <68 minutes
5
= 68 minutes to <83 minutes
6
= 83 minutes to <98 minutes
7
= 98 minutes to <113 minutes
8
= 113 minutes to <128 minutes
9
= 128 minutes to <143 minutes
10
= 143 minutes to <158 minutes
Table 2 shows the use of the G-codes established for the home infusion therapy benefit,
and reflects the therapy type and complexity of the drug administration.
Table 2: Payment Categories for Home Infusion Therapy Professional Services (G-
Codes)
Category 1
Category 2
Category 3
Description
G-Code
Intravenous anti-infective,
pain management, chelation,
pulmonary hypertension,
inotropic, and other certain
intravenous infusion drugs
Subcutaneous
immunotherapy and
other certain
Subcutaneous infusion
drugs
Chemotherapy
and other certain
highly complex
intravenous drugs
Initial Visit
G0088
G0089
G0090
Subsequent Visit
G0068
G0069
G0070
• G0068: Professional services for the administration of anti-infective, pain
management, chelation, pulmonary hypertension, inotropic, or other intravenous
infusion drug or biological (excluding chemotherapy or other highly complex drug
or biological) for each infusion drug administration calendar day in the individual’s
home, each 15 minutes
Short Descriptor: Adm IV infusion drug in home
• G0069: Professional services for the administration of subcutaneous
immunotherapy or other subcutaneous infusion drug or biological for each infusion
drug administration calendar day in the individual's home, each 15 minutes
Short Descriptor: Adm SQ infusion drug in home
• G0070: Professional services for the administration of intravenous chemotherapy or
other intravenous highly complex drug or biological infusion for each infusion drug
administration calendar day in the individual's home, each 15 minutes.
Short Descriptor: Adm of IV chemo drug in home
• G0088: Professional services, initial visit, for the administration of anti-infective,
pain management, chelation, pulmonary hypertension, inotropic, or other
intravenous infusion drug or biological (excluding chemotherapy or other highly
complex drug or biological) for each infusion drug administration calendar day in
the individual’s home, each 15 minutes.
Short Descriptor: Adm IV drug 1
st
home visit
• G0089: Professional services, initial visit, for the administration of subcutaneous
immunotherapy or other subcutaneous infusion drug or biological for each infusion
drug administration calendar day in the individual's home, each 15 minutes.
Short Descriptor: Adm SubQ drug 1
st
home visit
• G0090: Professional services, initial visit, for the administration of intravenous
chemotherapy or other highly complex infusion drug or biological for each infusion
drug administration calendar day in the individual's home, each 15 minutes.
Short Descriptor: Adm IV chemo 1
st
home visit
411.5 – Claim Adjustment Reason Codes, Remittance Advice Remark
Codes, Group Codes, and Medicare Summary Notice Messages
(Rev. 10269, Issued: 08-07-2020, Effective: 01-01-2021, Implementation: 01-04-2021)
Contractors shall deny the CWF rejected claim if a new G-code is received for the same date of
service as a previous claim was paid for the same line item date of service.
NOTE: The provider should submit an adjustment to the original claim to receive the higher
payment.
Contractors shall use the following CARC/RARC codes when denying claims:
CARC 97 - The benefit for this service is included in the payment/allowance for
another service/procedure that has already been adjudicated. Usage: Refer to the
835 Healthcare Policy Identification Segment (loop 2110 Service Payment
Information REF), if present.
RARC N111 - No appeal right except duplicate claim/service issue. This service
was included in a claim that has been previously billed and adjudicated.
Claim Adjustment Group Code - CO (Contractual Obligation)
MSN message: 41.14: This service/item was billed incorrectly. 41.14- Este servicio
o artículo fue facturado incorrectamente.
Contractors shall deny the CWF rejected G-code line when the claim has recycled three
times without finding the associated drug J-code claim and use the following messages:
CARC 16 - Claim/service lacks information or has submission/billing error(s).
Usage: Do not use this code for claims attachment(s)/other documentation. At least
one Remark Code must be provided (may be comprised of either the NCPDP Reject
Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Refer to
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment
Information REF), if present.
RARC N657 - This should be billed with the appropriate code for these services.
Claim Adjustment Group Code - CO (Contractual Obligation)
MSN message: 41.14: This service/item was billed incorrectly. 41.14- Este servicio
o artículo fue facturado incorrectamente.
Contractors shall deny CWF rejected claims for more than one claim line service of G0088,
G0089, or G0090 within a 60 day period and use the following messages:
CARC 96 - Non-covered charge(s). At least one Remark Code must be provided
(may be comprised of either the NCPDP Reject Reason [sic] Code, or Remittance
Advice Remark Code that is not an ALERT.) Note: Refer to the 835 Healthcare
Policy Identification Segment (loop 2110 Service Payment Information REF), if
present.
RARC N640 - Exceeds number/frequency approved/allowed within time period.
Group Code - CO (Contractual Obligation)
411.6 – CWF and MCS Editing Requirements
(Rev. 10269, Issued: 08-07-2020, Effective: 01-01-2021, Implementation: 01-04-2021)
MCS shall create a new edit to identify when there is more than one of the following six
HCPCS ‘G0068’, ‘G0069’ ‘G0070’, ‘G0088’, ‘G0089’, or ‘G0090’ with Date of Service
on or after 1/1/2021 for the same Date of Service on the same Part B Professional claim.
CWF shall create a new reject for a Part B Professional claim with one of the following six
HCPCS codes ‘G0068’, ‘G0069’ ‘G0070’, ‘G0088’, ‘G0089’, or ‘G0090’ with Date of
Service on or after 1/1/2021 and there is no DME claim in history with one of the identified
J-codes within 30 days prior to the incoming Date of Service.
NOTE: This edit shall have override capability at the claim detail line
CWF and contractors shall recycle ‘G0068’, ‘G0069’ ‘G0070’, ‘G0088’, ‘G0089’, or
‘G0090’ claim up to three times for a total of 15 days until a claim containing an allowable
drug J-code from above is received with the same line item date of service or within 30
days prior to the line item date of service of the G-code.
CWF shall create a new reject for a Part B Professional claim with one of the following six
‘G0068’, ‘G0069’ ‘G0070’, ‘G0088’, ‘G0089’, or ‘G0090’ codes with a Date of Service on
or after 1/1/2021 when there is a Part B claim in history with one of the identified six
‘G0068’, ‘G0069’ ‘G0070’, ‘G0088’, ‘G0089’, or ‘G0090’ codes for the same Date of
Service.
NOTE: This edit shall have override capability at the claim detail line
CWF shall create a new reject for a Part B Professional claim with one of the new ‘G0088’,
‘G0089’, or ‘G0090’ codes and in history is an allowed DME or Part B Professional claim
with any of the six ‘G0068’, ‘G0069’ ‘G0070’, ‘G0088’, ‘G0089’, or ‘G0090’ codes and
the Dates of Service is within 60 days prior to the incoming claim’s Dates of Service. The
incoming claim has Dates of Service on or after 1/1/2021.
CWF should still subject an incoming Part B Professional claim to the edit if it is within 60
days of posted DME claim, and if the claim in history is DME and has one of the three
existing ‘G0068’, ‘G0069’ ‘G0070’ codes and has Dates of Service prior to 1/1/2021.
CWF shall create a new Informational Unsolicited Response (IUR) when a Part B
Professional claim or a DME claim with one of the six ‘G0068’, ‘G0069’ ‘G0070’,
‘G0088’, ‘G0089’, or ‘G0090’ codes is received and in history is a Part B Professional
claim with one of the three new ‘G0088’, ‘G0089’, or ‘G0090’ codes with Dates of Service
within 60 days after the incoming claim’s Dates of Service.
CWF shall ensure that all new edits and the IUR appear on the ORPN Report.
412 – Monoclonal Antibodies Directed Against Amyloid for the
Treatment of Alzheimer’s Disease (AD) Policy and Overview
(Rev. 12649; Issued: 05-23-2024; Effective: 04-07-22) Implementation: 06-24-24)
Effective April 7, 2022, CMS covers Food and Drug Administration (FDA)-approved
monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s Disease
(AD) when furnished in accordance with the coverage criteria below, under coverage with
evidence development (CED) for patients who have a clinical diagnosis of mild cognitive
impairment (MCI) due to AD or mild AD dementia, both with confirmed presence of
amyloid beta pathology consistent with AD. For further information related to coverage,
refer to Publication 100-03, National Coverage Determination (NCD) Section 200.3
412.1 - Coding Information
(Rev. 12649; Issued: 05-23-2024; Effective: 04-07-22) Implementation: 06-24-24)
- ICD-10 diagnosis code Z00.6, along with one of the following additional diagnosis
codes: G30.0, G30.1, G30.8, G30.9, G31.84, the Q0 or Q1 modifier, and condition code
30 (for institutional claims only).
- Procedure code HCPCS J0174, Injection, lecanemab-irmb, 1 mg, (Leqembi®), OR,
- Procedure code HCPCS J3490 or J3590 or C9399 (for an FDA-approved therapy that is
covered under NCD 200.3 that hasn’t received a dedicated HCPCS code), OR,
- Dedicated HCPCS code for any future FDA-approved therapies covered under NCD
200.3 (a subsequent instruction would follow),
- National Clinical Trial (NCT) number consisting of 8 digits, OR,
- Default NCT number 99999999.
412.2 - Claims Processing Instructions
(Rev. 12649; Issued: 05-23-2024; Effective: 04-07-22) Implementation: 06-24-24)
Effective for claims with dates of service on or after April 7, 2022, contractors shall accept
and pay for claims for monoclonal antibodies for the treatment of AD with an appropriate
HCPCS, along with one of the diagnosis codes listed in Section 412.1 and condition code
30 (institutional claims only).
The following bill types are applicable for claims for monoclonal antibodies for the
treatment of AD:
- 012X, 013X, or 085X.
412.3 - Messaging
(Rev. 12649; Issued: 05-23-2024; Effective: 04-07-22) Implementation: 06-
24-24)
--Contractors shall return to provider/return as unprocessable any monoclonal antibody
claims that do not include an NCT number as indicated in 412.1 and use the following
messages:
CARC 16 - Claim/service lacks information or has submission/billing error(s).
RARC MA50 – Missing/incomplete/invalid Investigational Device Exemption number or
Clinical Trial number
Group Code: CO
---Contractors shall deny any monoclonal antibody claims that do not have the specified
diagnosis codes listed in 412.1 and use the following messages:
MSN 15.20 - “The following polices were used when we made this decision: NCD 200.3.”
Spanish Version – “Las siguientes políticas fueron utilizadas cuando se tomó esta decisión:
NCD 200.3.”
NOTE: Due to system requirement, the Fiscal Intermediary Shared System (FISS) has
combined messages 15.19 and 15.20 so that, when used for the same line item, both
messages will appear on the same MSN.
CARC 96 – Non-covered charge(s). At least one Remark Code must be provided (May be
comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code
that is not an ALERT).
RARC N386 – This decision was based on a National Coverage Determination (NCD). An
NCD provides a coverage determination as to whether a particular item or service is
covered.
Group Code - CO or PR
---Contractors shall return to provider/return as unprocessable any monoclonal antibody
claims that do not have the specified modifiers listed in Section 412.1 and use the
following messages:
CARC 16 - Claim/service lacks information or has submission/billing error(s).
RARC N823 – Incomplete/invalid Procedure Modifier(s).
Group Code: CO
--Contractors shall deny claims from any bill type other than those listed 412.1 and use the
following messages:
MSN 9.4 - This item or service was denied because information required to make payment
was incorrect.
Spanish Version: Este servicio fue denegado debido a que la información requerida para
hacer el pago fue incorrecta.
CARC 16 - Claim/service lacks information or has submission/billing error(s).
RARC MA30 - Missing/incomplete/invalid type of bill.
Group Code: CO

Transmittals Issued for this Chapter
Rev #
Issue Date
Subject
Impl Date
CR#
R12683CP
06/13/2024
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 32, Section
150.3 for Coding Revisions to the National
Coverage Determinations (NCDs)--October
2024 Change Request (CR)13596
07/15/2024
13622
R12649CP
05/23/2024
National Coverage Determination (NCD) 200.3
- Monoclonal Antibodies Directed Against
Amyloid for the Treatment of Alzheimer’s
Disease (AD)
06/24/2024
13598
R12571CP
04/11/2024
National Coverage Determination (NCD) 20.7
Percutaneous Transluminal Angioplasty (PTA)
of the Carotid Artery Concurrent with Stenting
05/13/2024
13512
R12533CP
03/07/2024
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 32, Section
90 for Coding Revisions to the National
Coverage Determinations (NCDs)--July 2024
Change Request (CR) 13507.
04/08/2024
13545
R12497CP
02/08/2024
Pulmonary Rehabilitation, Cardiac
Rehabilitation and Intensive Cardiac
Rehabilitation (PR/CR/ICR) Expansion of
Supervising Practitioners
03/12/2024
13513
R12435CP
12/28/2023
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 18, Sections
20.2, 60.3 and Chapter 32, Sections 50.4.1,
200.2 for Coding Revisions to the National
Coverage Determinations (NCDs)--April 2024
Change Request (CR) 13391
01/29/2024
12435
R12396CP
12/07/2023
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 32 Sections
320.3.3 and 370.1 for Coding Revisions to the
National Coverage Determinations (NCDs)--
April 2024 Change Request (CR) 13390
01/09/2024
13438
R12109CP
06/29/2023
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 32 Sections
130.1, for International Classification of
Diseases, 10th Revision (ICD-10) and Other
Coding Revisions to National Coverage
Determinations (NCDs)--October 2023 Update
Change Request (CR) 13166
10/02/2023
13227

Rev #
Issue Date
Subject
Impl Date
CR#
R11902CP
03/16/2023
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 18 Sections
50.3-
50.4, and Chapter 32 Sections 130.1, 170.2
for Coding Revisions to National Coverage
Determinations (NCDs)--July 2023 Change
Request (CR) 13070
04/17/2023
13104
R11875CP
02/23/2023
National Coverage Determination (NCD) 50.3 -
Cochlear Implantation Manual Update
03/24/2023
13073
R11789CP
01/19/2023
Update to the Internet Only Manual (IOM) For
Alpha-Numerical Order in Publication (Pub.)
100-04, Chapter 32, Index, Sections 40.2.1 and
40.2.4
02/21/2023
13025
R11759CP
12/21/2022
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 18 Section
170.1 and Chapter 32 Section 270.2 due to the
National Coverage Determinations (NCDs)
April 2023 Change Request (CR) 12960
01/23/2023
12993
R11721CP
11/28/2022
National Coverage Determination (NCD
110.24): Chimeric Antigen Receptor (CAR) T-
cell Therapy
01/03/2023
12928
R11430CP
05/24/2022
Update to 'J' Drug Code List for Billing Home
Infusion Therapy (HIT) Services
07/05/2022
12667
R11426CP
05/20/2022
An Omnibus CR Covering: (1) Removal of Two
National Coverage Determination (NCDs), (2)
Updates to the Medical Nutrition Therapy
(MNT) Policy, and (3) Updates to the
Pulmonary Rehabilitation (PR), Cardiac
Rehabilitation (CR), and Intensive Cardiac
Rehabilitation (ICR) Conditions of Coverage-
Rescinded and replaced by transmittal 11426
07/05/2022
12613
R11272CP
02/18/2022
An Omnibus CR Covering: (1) Removal of Two
National Coverage Determination (NCDs), (2)
Updates to the Medical Nutrition Therapy
(MNT) Policy, and (3) Updates to the
Pulmonary Rehabilitation (PR), Cardiac
Rehabilitation (CR), and Intensive Cardiac
Rehabilitation (ICR) Conditions of Coverage
07/05/2022
12613
R11214CP
01/20/2022
National Coverage Determination (NCD)
270.3 Blood-Derived Products for Chronic,
01/03/2022
12403

Rev #
Issue Date
Subject
Impl Date
CR#
Non-Healing Wounds
R11171CP
01/12/2022
National Coverage Determination (NCD)
270.3 Blood-Derived Products for Chronic,
Non-Healing Wounds Rescinded and replaced
by transmittal 11214
01/03/2022
12403
R11119CP
11/13/2021
National Coverage Determination (NCD)
270.3 Blood-Derived Products for Chronic,
Non-Healing Wounds Rescinded and replaced
by transmittal 11171
01/03/2022
12403
R11035CP
10/13/2021
Revisions to Chapters 3, 18, and 32 to Update
Coding
10/13/2021
12377
R11021CP
10/01/2021
Revisions To Chapters 13, 18 And 32 To
Update Coding
10/29/2021
12376
R10981CP
09/10/2021
National Coverage Determination (NCD) 270.3
Blood-Derived Products for Chronic, Non-
Healing Wounds - Rescinded and replaced by
transmittal 11119
01/03/2022
12403
R10985CP
09/08/2021
Claims Processing Instructions for National
Coverage Determination 20.33 - Transcatheter
Edge-to-Edge Repair [TEER] for Mitral Valve
Regurgitation
10/08/2021
12361
R10881CP
08/06/2021
REVISIONS TO CHAPTERS 13 AND 32 TO
UPDATE CODING
09/07/2021
12069
R10891CP
07/20/2021
National Coverage Determination (NCD
110.24): Chimeric Antigen Receptor (CAR) T-
cell Therapy - This CR Rescinds and Fully
Replaces CR 11783.
230.2222
09/20/2021
12177
R10796CP
National Coverage Determination (NCD
110.24): Chimeric Antigen Receptor (CAR) T-
cell Therapy - This CR Rescinds and Fully
Replaces CR 11783-
Rescinded and replaced by
transmittal 10891
07/23/2021
12177
R10837CP
06/11/2021
National Coverage Determination (NCD) 20.9.1
Ventricular Assist Devices (VADs)
07/27/2021
12290
R10796CP
05/20/2021
National Coverage Determination (NCD
110.24): Chimeric Antigen Receptor (CAR) T-
cell Therapy - This CR Rescinds and Fully
Replaces CR 11783. - Rescinded and replaced
by transmittal 10891
07/23/2021
12177

Rev #
Issue Date
Subject
Impl Date
CR#
R10573CP
03/24/2021
Update to Pulmonary Rehabilitation (PR),
Cardiac Rehabilitation (CR) and Intensive
Cardiac Rehabilitation (ICR) Program Manual
Sections
04/26/2021
12115
R10547CP
12/31/2020
Billing for Home Infusion Therapy Services On
or After January 1, 2021
01/04/2021
11880
R10463CP
11/13/2020
Billing for Home Infusion Therapy Services On
or After January 1, 2021
01/04/2021
11880
R10343CP
09/04/2020
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-04, Chapter 32, Section
40.2.1 and 40.2.4
10/06/2020
11950
R10337CP
08/27/2020
National Coverage Determination (NCD30.3.3):
Acupuncture for Chronic Low Back Pain
(cLBP)
01/04/2021
11755
R10269CP
08/07/2020
Billing for Home Infusion Therapy Services On
or After January 1, 2021- Rescinded and
replaced by transmittal 10463
01/04/2021
11880
R10229CP
07/21/2020
Modify Edits in the Fee for Service (FFS)
System When a Beneficiary has a Medicare
Advantage (MA) Plan
10/05/2020
11580
R10179CP
06/10/2020
NCD (20.32) Transcatheter Aortic Valve
Replacement (TAVR)
06/12/2020
11660
R10128CP
05/08/2020
National Coverage Determination (NCD30.3.3):
Acupuncture for Chronic Low Back Pain
(cLBP) Rescinded and replaced by transmittal
10337
01/04/2021
11755
R10071CP
05/01/2020
Modify Edits in the Fee for Service (FFS)
System When a Beneficiary has a Medicare
Advantage (MA) Plan Rescinded and replaced
by transmittal 10229
10/05/2020
11580
R4546CP
03/13/2020
NCD (20.32) Transcatheter Aortic Valve
Replacement (TAVR) Rescinded and replaced
by transmittal 10179
06/12/2020
11660
R4237CP
02/08/2019
Update to the Internet-Only-Manual (IOM)
Publication (Pub.) 100-04, Chapter 32, Section
12.1
03/12/2019
11127
R4222CP
02/01/2019
Update to Intensive Cardiac Rehabilitation
(ICR) Programs
03/19/2019
11117

Rev #
Issue Date
Subject
Impl Date
CR#
R4203CP
01/18/2019
Update to Pub. 100-04 Chapter 32 to Provide
Language-Only Changes for the New Medicare
Card Project
02/19/2019
11118
R4111CP
08/10/2018
Revisions to Medicare Claims Processing
Manual for Foreign, Emergency and Shipboard
Claims
09/11/2018
10856
R4049CP
05/11/2018
Supervised Exercise Therapy (SET) for
Symptomatic Peripheral Artery Disease (PAD)
07/02/2018
10295
R4016CP
04/03/2018
Supervised Exercise Therapy (SET) for
Symptomatic Peripheral Artery Disease (PAD)
07/02/2018
10295
R4013CP
03/30/2018
Institutional Billing for No Cost Items
06/29/2018
10521
R3969CP
02/02/2018
Supervised Exercise Therapy (SET) for
Symptomatic Peripheral Artery Disease (PAD)
04/03/2018
10295
R203NCD
11/17/2017
Hyperbaric Oxygen (HBO) Therapy (Section C,
Topical Application of Oxygen)
12/18/2017
10220
R3898CP
10/27/2017
Correction to Prevent Payment on Inpatient
Information Only Claims for Beneficiaries
Enrolled in Medicare Advantage Plans
04/02/2018
10238
R3871CP
09/29/2017
Revisions to Medicare Claims Processing
Manual for Foreign, Emergency and Shipboard
Claims
10/30/2017
10287
R3848CP
08/25/2017
Updates to Pub. 100-04, Chapter 18 Preventive
and Screening Services and Chapter 32 Billing
Requirements for Special Services and
Publication 100-03, Chapter 1 Coverage
Determinations Part 4
09/26/2017
10199
R3815CP
07/28/2017
National Coverage Determination (NCD20.8.4):
Leadless Pacemakers
08/29/2017
10117
R3811CP
07/25/2017
Percutaneous Image-guided Lumbar
Decompression (PILD) for Lumbar Spinal
Stenosis (LSS)
06/27/2017
10089
R3805CP
07/11/2017
Percutaneous Image-guided Lumbar
Decompression (PILD) for Lumbar Spinal
Stenosis (LSS) – Rescinded and replaced by
transmittal 3811
08/11/2017
10089
R3787CP
05/26/2017
Percutaneous Image-guided Lumbar
Decompression (PILD) for Lumbar Spinal
Stenosis (LSS) – Rescinded and replaced by
06/27/2017
10089

Rev #
Issue Date
Subject
Impl Date
CR#
transmittal 3805
R3556CP
07/01/2016
Stem Cell Transplantation for Multiple
Myeloma, Myelofibrosis, Sickle Cell Disease,
and Myelodysplastic Syndromes
10/03/2016
9620
R3509CP
04/29/2016
Stem Cell Transplantation for Multiple
Myeloma, Myelofibrosis, Sickle Cell Disease,
and Myelodysplastic Syndromes - Rescinded
and replaced by Transmittal 3556
10/03/2016
9620
R3384CP
10/26/2015
National Coverage Determination (NCD) for
Single Chamber and Dual Chamber Permanent
Cardiac Pacemakers - This CR rescinds and
fully replaces CR 8525
07/06/2015
9078
R3287CP
06/30/2015
Revisions to Medicare Claims Processing
Manual for Foreign, Emergency and Shipboard
Claims
04/21/2015
8940
R3265CP
05/22/2015
NCD20.30 Microvolt T-wave Alternans
(MTWA)
06/23/2015
9162
R3241CP
04/24/2015
Transcatheter Mitral Valve Repair (TMVR)-
National Coverage Determination (NCD)
04/06/2014
9002
R3199CP
02/20/2015
Revisions to Medicare Claims Processing
Manual for Foreign, Emergency and Shipboard
Claims – Rescinded and replaced by
Transmittal 3287
04/21/2015
8940
R3204CP
02/20/2015
National Coverage Determination (NCD) for
Single Chamber and Dual Chamber Permanent
Cardiac Pacemakers - This CR rescinds and
fully replaces CR 8525 - Rescinded and
replaced by Transmittal 3384
07/06/2015
9078
R3181CP
01/30/2015
Implementation of New NUBC Condition Code
“53” “Initial placement of a medical device
provided as part of a clinical trial or a free
sample”
07/06/2015
8961
R3175CP
01/30/2015
Percutaneous Image-guided Lumbar
Decompression (PILD) for Lumbar Spinal
Stenosis (LSS)-Blinded Clinical Trial – Follow-
Up CR to Implement a Second Claims
Processing Procedure Code
03/02/2015
8954
R3142CP
12/05/2014
Transcatheter Mitral Valve Repair (TMVR)-
National Coverage Determination (NCD) –
Rescinded and replaced by Transmittal 3241
04/06/2014
9002
Rev #
Issue Date
Subject
Impl Date
CR#
R3105CP
11/06/2014
Medicare Coverage of Items and Services in
Category A and B Investigational Device
Exemption (IDE) Studies
01/05/2015
8921
R3084CP
10/03/2014
Intensive Cardiac Rehabilitation Program -
Benson-Henry Institute Cardiac Wellness
Program
11/04/2014
8894
R3058CP
08/29/2014
Cardiac Rehabilitation Programs for Chronic
Heart Failure
08/18/2014
8758
R3054CP
08/29/2014
Ventricular Assist Devices for Bridge-to-
Transplant and Destination Therapy
09/30/2014
8803
R3050CP
08/22/2014
Extracorporeal Photopheresis
09/23/2014
8808
R2998CP
07/25/2014
Update to Pub. 100-04, Chapter 32 to Provide
Language-Only Changes for Updating ICD-10
and ASC X12
08/25/2014
8693
R2989CP
07/18/2014
Cardiac Rehabilitation Programs for Chronic
Heart Failure Failure – Rescinded and replaced
by Transmittal 3058
08/18/2014
8758
R2959CP
05/16/2014
Percutaneous Image-guided Lumbar
Decompression (PILD) for Lumbar Spinal
Stenosis (LSS)
10/06/2014
8757
R2955CP
05/14/2014
Mandatory Reporting of an 8-Digit Clinical
Trial Number on Claims
01/06/2014
8401
R2872CP
02/06/2014
National Coverage Determination (NCD) for
Single Chamber and Dual Chamber Permanent
Cardiac Pacemakers – Rescinded and replaced
by Transmittal 2986
07/07/2014
8525
R2841CP
12/23/2013
Bariatric Surgery for Treatment of Co-Morbid
Conditions Related to Morbid Obesity
12/17/2013
8484
R2827CP
11/29/2013
Transcatheter aortic valve replacement (TAVR)
- Implementation of Permanent CPT Code
01/06/2013
8537
R2816CP
11/15/2013
Bariatric Surgery for Treatment of Co-Morbid
Conditions Related to Morbid Obesity –
Rescinded and replaced by Transmittal 2841
12/17/2013
8484
R2805CP
10/30/2013
Mandatory Reporting of an 8-Digit Clinical
Trial Number on Claims – Rescinded and
replaced by Transmittal 2955
01/06/2014
8401
R2783CP
09/10/2013
Corrections to the Medicare Claims Processing
Manual
09/17/2013
8343

Rev #
Issue Date
Subject
Impl Date
CR#
R2758CP
08/09/2013
Mandatory Reporting of an 8-Digit Clinical
Trial Number on Claims – Rescinded and
replaced by Transmittal 2805
01/06/2014
8401
R2743CP
07/25/2013
Coding Changes to Ultrasound Diagnostic
Procedures for Transesophageal Doppler
Monitoring
08/26/2013
8330
R2737CP
07/11/2013
National Coverage Determination (NCD) for
Transcatheter Aortic Valve Replacement
(TAVR) – Implementation of Mandatory
Reporting of Clinical Trial Number
10/07/2013
8255
R2728CP
06/14/2013
Ocular Photodynamic Therapy (OPT) with
Verteporfin for Macular Degeneration
07/16/2013
8292
R2725CP
06/14/2013
Corrections to the Medicare Claims Processing
Manual – Rescinded and replaced by
Transmittal 2783
09/17/2013
8343
R2720CP
06/10/2013
Autologous Platelet-Rich Plasma (PRP) for
Chronic Non-Healing Wounds
07/01/2013
8213
R2710CP
05/21/2013
Autologous Platelet-Rich Plasma (PRP) for
Chronic Non-Healing Wounds – Rescinded and
replaced by Transmittal 2720
07/01/2013
8213
R2689CP
05/03/2013
National Coverage Determination (NCD) for
Transcatheter Aortic Valve Replacement
(TAVR) – Implementation of Mandatory
Reporting of Clinical Trial Number –
Rescinded
and replaced by Transmittal 2737
10/07/2013
8255
R2666CP
03/08/2013
Autologous Platelet-Rich Plasma (PRP) for
Chronic Non-Healing Wounds – Rescinded and
replaced by Transmittal 2710
07/01/2013
8213
R2641CP
01/29/2013
Bariatric Surgery for the Treatment of Morbid
Obesity National Coverage Determination,
Addition of Laparoscopic Sleeve Gastrectomy
(LSG)
02/28/2013
8028
R2628CP
01/07/2013
NCD: Transcatheter Aortic Valve Replacement
(TAVR) Coding Update/Policy Clarification
04/01/2013
8168
R2590CP
11/09/2012
Bariatric Surgery for the Treatment of Morbid
Obesity National Coverage Determination,
Addition of Laparoscopic Sleeve Gastrectomy
(LSG) – Rescinded and replaced by Transmittal
2641
12/10/2012
8028
R2252CP
09/24/2012
National Coverage Determination (NCD) FOR
Transcatheter Aortic Valve Replacement
01/07/2013
7897

Rev #
Issue Date
Subject
Impl Date
CR#
R2551CP
09/24/2012
Extracorporeal Photopheresis (ICD-10) –
Rescinded and replaced by Transmittal 2551
10/01/2012
7806
R2544CP
09/13/2012
Contractor and Common Working File (CWF)
Additional Instructions Related to Change
Request (CR) 7633-Screening and Behavioral
Counseling Interventions in Primary Care to
Reduce Alcohol Misuse
10/01/2012
7791
R2543CP
09/07/2012
Extracorporeal Photopheresis (ICD-10) –
Rescinded and replaced by Transmittal 2551
10/01/2012
7806
R2512CP
08/03/2012
National Coverage Determination (NCD) FOR
Transcatheter Aortic Valve Replacement –
rescinded and Replaced by Transmittal 2552
01/07/2013
7897
R2506CP
08/03/2012
Extracorporeal Photopheresis (ICD-10) –
Rescinded and replaced by Transmittal 2543
10/01/2012
7806
R2494CP
07/10/2012
Extracorporeal Photopheresis (ICD-10) –
Rescinded and replaced by Transmittal 2506
10/01/2012
7806
R2488CP
06/21/2012
Contractor and Common Working File (CWF)
Additional Instructions Related to Change
Request (CR) 7633-Screening and Behavioral
Counseling Interventions in Primary Care to
Reduce Alcohol Misuse – Rescinded and
replaced by Transmittal 2544
10/01/2012
7791
R2473CP
05/18/2012
Extracorporeal Photopheresis (ICD-10)
10/01/2012
7806
R2454CP
04/26/2012
Contractor and Common Working File (CWF)
Additional Instructions Related to Change
Request (CR) 7633-Screening and Behavioral
Counseling Interventions in Primary Care to
Reduce Alcohol Misuse – Rescinded and
replaced by Transmittal 2488
10/01/2012
7791
R2394CP
01/25/2012
CWF Editing for Autologuous Cellular
Immunotherapy Treatment of Metastatic
Prostate Cancer (PROVENGE®)
07/02/2012
7659
R2380CP
01/06/2012
Autologous Cellular Immunotherapy Treatment
of Metastatic Prostate Cancer
08/08/2011
7431
R2339CP
11/02/2011
Autologous Cellular Immunotherapy Treatment
of Metastatic Prostate Cancer - Rescinded and
replaced by Transmittal 2380
08/08/2011
7431
R2254CP
07/08/2011
Autologous Cellular Immunotherapy Treatment
of Metastatic Prostate Cancer – Rescinded and
replaced by Transmittal 2339
08/08/2011
7431

Rev #
Issue Date
Subject
Impl Date
CR#
R2113CP
12/10/2010
Payment for 510k Post-Approval Extension
Studies Using 501k-
Cleared Embolic Protection
Devices During Carotid Artery Stenting (CAS)
Procedures
01/12/2011
7249
R2105CP
11/24/2010
Dermal Injections for Treatment of Facial
Lipodystrophy Syndrome (LDS)
07/06/2010
6953
R2062CP
10/08/2010
Allogeneic Hematopoietic Stem Cell
Transplantation (HSCT) for Myelodysplastic
Syndrome (MDS)
11/10/2010
7137
R2052CP
09/17/2010
Billing and Processing for Healthy Control
Group Volunteers in a Qualified Clinical Trial
07/06/2010
6776
R2005CP
07/23/2010
Billing and Claims Processing for Automatic
Implantable Cardiac Defibrillator (ICD)
Services
08/31/2010
7015
R1994CP
07/02/2010
Billing and Claims Processing for Automatic
Implantable Cardiac Defibrillator (ICD)
Services - Rescinded and replaced by
Transmittal 2005
08/31/2010
7015
R1978CP
06/04/2010
Dermal Injections for Treatment of Facial
Lipodystrophy Syndrome (LDS) – Rescinded
and replaced by Transmittal 2105
07/06/2010
6953
R1974CP
05/21/2010
Cardiac Rehabilitation and Intensive Cardiac
Rehabilitation
10/04/2010
6850
R1966CP
05/07/2010
Pulmonary Rehabilitation (PR) Services
10/04/2010
6823
R1925CP
03/05/2010
Percutaneous Transluminal Angioplasty (PTA)
of the Carotid Artery Concurrent with Stenting
04/05/2010
6839
R1924CP
02/26/2010
April 2010 Update of the Hospital Outpatient
Prospective Payment System (OPPS)
04/05/2010
6857
R1901CP
01/29/2010
Billing and Processing for Healthy Control
Group Volunteers in a Qualified Clinical Trial –
Rescinded and replaced by Transmittal 2052
07/06/2010
6776
R1889CP
01/08/2010
Pharmacogenomic Testing for Warfarin
Response
04/05/2010
6715
R1882CP
12/21/2009
January 2010 Update of the Hospital Outpatient
Prospective Payment System (OPPS)
01/04/2010
6751
R1871CP
12/11/2009
January 2010 Update of the Hospital Outpatient
Prospective Payment System (OPPS) -
Rescinded and replaced by Transmittal 1882
01/04/2010
6751
R1877CP
12/18/2009
Instructions Regarding Processing Claims
Rejecting for Gender/Procedure Conflict
04/05/2010
6638

Rev #
Issue Date
Subject
Impl Date
CR#
R1876CP
12/18/2009
Coverage of Kidney Disease Patient Education
Services
04/05/2010
6557
R1839CP
10/28/2009
Instructions Regarding Processing Claims
Rejecting for Gender/Procedure Conflict -
Rescinded and replaced by Transmittal 1877
04/05/2010
6638
R1816CP
09/17/2009
Fiscal Year (FY) 2010 Inpatient Prospective
Payment System (IPPS), Long Term Care
Hospital (LTCH) PPS, and Inpatient Psychiatric
Facility (IPF) PPS Changes
10/05/2009
6634
R1815CP
09/09/2009
Fiscal Year (FY) 2010 Inpatient Prospective
Payment System (IPPS), Long Term Care
Hospital (LTCH) PPS, and Inpatient Psychiatric
Facility (IPF) PPS Changes - Rescinded and
replaced by Transmittal 1816
10/05/2009
6634
R1778CP
07/24/2009
Wrong Surgical or Other Invasive Procedure
Performed on a Patient; Surgical or Other
Invasive Procedure Performed on the Wrong
Body Part; Surgical or Other Invasive
Procedure Performed on the Wrong Patient
07/06/2009
6405
R1764CP
07/02/2009
Wrong Surgical or Other Invasive Procedure
Performed on a Patient; Surgical or Other
Invasive Procedure Performed on the Wrong
Body Part; Surgical or Other Invasive
Procedure Performed on the Wrong Patient –
Rescinded and replaced by Transmittal 1778
07/06/2009
6405
R1761CP
06/26/2009
Billing Routine Cost of Clinical Trials
09/28/2009
6431
R1755CP
06/12/2009
Wrong Surgical or Other Invasive Procedure
Performed on a Patient; Surgical or Other
Invasive Procedure Performed on the Wrong
Body Part; Surgical or Other Invasive
Procedure Performed on the Wrong Patient –
Rescinded and replaced by Transmittal 1764
07/06/2009
6405
R1743CP
05/22/2009
Billing Routine Cost of Clinical Trials -
Rescinded and replaced by Transmittal 1761
07/10/2009
6431
R1742CP
05/22/2009
Clarification of CMS Publication 100-04,
Chapter 32, Section 80.8 Billing of Routine
Foot Care When Payment Ceases for Loss of
Protective Sensation Evaluation and
Management
06/08/2009
6456
R1731CP
05/08/2009
Clarification of CMS Publication 100-04,
Chapter 32, Section 80.8 Billing of Routine
06/08/2009
6456

Rev #
Issue Date
Subject
Impl Date
CR#
Foot Care When Payment Ceases for Loss of
Protective Sensation Evaluation and
Management - Rescinded and replaced by
Transmittal 1742
R1728CP
05/01/2009
Surgery for Diabetes
05/18/2009
6419
R1723CP
05/01/2009
Ensuring Only Clinical Trial Services Receive
Fee-For-Service Payment on Claims Billed for
Managed Care Beneficiaries
10/05/2009
6455
R1721CP
04/29/2009
Billing Routine Cost of Clinical Trials -
Rescinded and replaced by Transmittal 1743
07/10/2009
6431
R1711CP
04/17/2009
Surgery for Diabetes – Rescinded and replaced
by Transmittal 1728
05/18/2009
6419
R1710CP
04/10/2009
Billing Routine Cost of Clinical Trials -
Rescinded and replaced by Transmittal 1721
07/10/2009
6431
R1663CP
01/08/2009
Correction to Prothrombin Time (PT/INR)
Monitoring for Home Anticoagulation
Management
02/09/2009
6313
R1657CP
12/31/2008
January 2009 Update of the Hospital Outpatient
Prospective Payment System (OPPS)
01/05/2009
6320
R1646CP
12/09/2008
Thermal Intradiscal Procedures (TIPs)
01/05/2009
6291
R1593CP
09/12/2008
Smoking and Tobacco Use Cessation
Counseling Billing Update for Comprehensive
Outpatient Rehabilitation Facilities (CORFs)
and Outpatient Physical Therapy Providers
(OPTs)
12/12/2008
6163
R1592CP
09/10/2008
Artificial Hearts
12/01/2008
6185
R1583CP
08/29/2008
Artificial Hearts - Replaced by Transmittal
1592
10/06/2008
6185
R1562CP
07/25/2008
Prothrombin Time (PT/INR) Monitoring for
Home Anticoagulation Management -
Rescinded and replaced by CR 6313
08/25/2008
6138
R1509CP
05/16/2008
Adjusting Inpatient Prospective Payment
System (IPPS) Reimbursement for Replaced
Devices Offered Without Cost or With a Credit
10/06/2008
5860
R1498CP
05/02/2008
Adjusting Inpatient Prospective Payment
System (IPPS) Reimbursement for Replaced
Devices Offered Without Cost or With a Credit
– Replaced by Transmittal 1509
10/06/2008
5860
R1472CP
03/06/2008
Update of Institutional Claims References
04/07/2008
5893

Rev #
Issue Date
Subject
Impl Date
CR#
R1433CP
02/01/2008
Smoking and Tobacco Use Cessation
Counseling Billing Code Update
07/07/2008
5878
R1430CP
02/01/2008
Use of HCPCS V2787 When Billing Approved
Astigmatism-Correcting Intraocular Lens (A-
CIOLs) in Ambulatory Surgery Centers (ASCs),
Physician Offices, and Hospital Outpatient
Departments (HOPDs)
03/03/2008
5853
R1421CP
01/25/2008
Update of Institutional Claims References -
Rescinded and Replaced by Transmittal 1472
04/07/2008
5893
R1418CP
01/18/2008
New HCPCS Modifiers When Billing for
Patient Care in Clinical Research Studies
04/07/2008
5805
R1340CP
09/21/2007
Lumbar Artificial Disc Replacement (LADR)
10/01/2007
5727
R1315CP
08/10/2007
Clarification of Percutaneous Transluminal
Angioplasty (PTA) Billing Requirements Issued
in CR 3811
10/01/2007
5667
R1271CP
06/22/2007
Vagus Nerve Stimulation (VNS) for Resistant
Depression
07/23/2007
5612
R1233CP
04/27/2007
Clarification of Bariatric Surgery Billing
Requirements Issued in CR 5013
05/29/2007
5477
R1228CP
04/27/2007
Instructions for Implementation of CMS 1536-
R; Astigmatism-Correcting Intraocular Lens (A-
C IOLs)
05/29/2007
5527
R1206CP
03/16/2007
Extracorporeal Photopheresis
04/02/2007
5464
R1192CP
03/02/2007
Payment and Billing for Islet Isolation Add-On
in National Institutes of Health (NIH) Clinical
Trial
04/02/2007
5505
R1164CP
01/26/2007
Coding Change for Lumbar Artificial Disc
Replacement (LADR)
03/13/2007
5462
R1147CP
01/05/2007
Intracranial Percutaneous Transluminal
Angioplasty (PTA) with Stenting
02/05/2007
5432
R1111CP
11/09/2006
Clarification on Billing for Cryosurgery of the
Prostate Gland
04/02/2007
5376
R1042CP
08/25/2006
Clarification on Billing Requirements for
Percutaneous Transluminal Angioplasty (PTA)
Concurrent With the Placement of an
Investigational or FDA-Approved Carotid Stent
10/02/2006
5022
R1000CP
07/19/2006
Common Working File (CWF) to the Medicare
Beneficiary Database (MDB) Data Exchange
Changes
10/02/2006
4300

Rev #
Issue Date
Subject
Impl Date
CR#
R992CP
06/23/2006
Lumbar Artificial Disc Replacement (LADR)
07/17/2006
5057
R986CP
06/16/2006
Payment for Islet Cell Transplantation in NIH-
Sponsored Clinical Trials
07/31/2006
5140
R951CP
05/12/2006
Payment for Carotid Artery Stenting (CAS)
Post-Approval Extension Studies
06/12/2006
5088
R931CP
04/28/2006
Billing Requirements for Bariatric Surgery for
Treatment of Morbid Obesity
05/30/2006
5013
R911CP
04/21/2006
Clarification on Billing Requirements for
Percutaneous Transluminal Angioplasty (PTA)
Concurrent With the Placement of an
Investigational or FDA-Approved Carotid Stent
10/02/2006
5022
R909CP
04/21/2006
Cardiac Rehabilitation Programs
06/21/2006
4401
R908CP
04/21/2006
Common Working File (CWF) to the Medicare
Beneficiary Database (MBD) Data Exchange
Changes
10/02/2006
4300
R898CP
03/31/2006
External Counterpulsation (ECP) Therapy
N/A
4350
R816CP
01/20/2006
Coverage and Billing for Ultrasound
Stimulation for Nonunion Fracture Healing
04/03/2006
4085
R801CP
12/30/2005
Instructions for Reporting New HCPCS Code
V2788 for Presbyopia-Correcting Intraocular
Lenses (P-C IOLs)
01/03/2006
4184
R795CP
12/30/2005
Redefined Type of Bill (TOB) 14X for Non-
Patient Laboratory Specimens-CR 3835
Manualization
04/03/2006
4208
R766CP
12/02/2005
Stem Cell Transportation
01/03/2006
4173
R726CP
10/21/2005
Smoking and Tobacco-Use Cessation
Counseling Services: Common Working File
(CWF) Inquiry for Providers
01/24/2006
4104
R671CP
09/09/2005
Updated Manual Instructions for the Medicare
Claims Processing Manual, Regarding Smoking
and Tobacco-Use Cessation Counseling
Services
10/03/2005
4045
R605CP
07/15/2005
Frequency Instructions for Smoking and
Tobacco-Use Cessation Counseling Services
10/03/2005
3929
R601CP
07/01/2005
Cochlear Implantation
07/25/2005
3796
R597CP
06/24/2005
Coverage and Billing for Ultrasound
Stimulation for Nonunion Fracture Healing
08/01/2005
3836
R589CP
06/24/2005
Cochlear Implantation
07/05/2005
3796

Rev #
Issue Date
Subject
Impl Date
CR#
R562CP
05/20/2005
Smoking and Tobacco-Use Cessation
Counseling Services
07/05/2005
3834
R526CP
04/15/2005
Updated Requirements for Autologous Stem
Cell Transplantation (AuSCT)
05/16/2005
3797
R498CP
03/11/2005
Billing of the Diagnosis and Treatment of
Peripheral Neuropathy with Loss of Protective
Sensation in People with Diabetes
N/A
3580
R487CP
03/04/2005
Manualization of Claims Processing
Instructions for Medicare Qualifying Clinical
Trials
N/A
3625
R486CP
03/04/2005
Manualization of Carrier Claims Processing
Instructions for Stem Cell Transplantation
N/A
3684
R371CP
11/19/2004
Updated Billing Instructions for Rural Health
Clinics (RHCs) and Federally Qualified Health
Centers (FQHCs)
04/04/2005
3487
R261CP
07/30/2004
Billing Requirements for Islet Cell
Transplantation for Beneficiaries in a National
Institutes of Health Sponsored Clinical Trial
10/04/2004
3385
R216CP
06/25/2004
Manualization of Instructions for of INR
Monitoring
N/A
2323
R187CP
05/28/2004
Manualization of Instructions for Billing for
Hyberbaric Oxygen Therapy for the Treatment
of Wounds of the Lower Extremities
06/28/2004
3172
R130aCP
03/26/2004
Manualization of Instructions for INR
Monitoring
N/A
2323
R128CP
03/26/2004
Manualization of Instructions for Deep Brain
Stimulation
N/A
2553
R125CP
03/26/2004
Manualization of Instructions for Sacral Nerve
Stimulation
N/A
2532
R124CP
03/19/2004
Policy and Claims Processing Instructions for
Electrical Stimulation And Electromagnetic
Therapy
07/06/2004
3149
R109CP
02/27/2004
Updated Policy and Claims Processing
Instructions for Ambulatory Blood Pressure
Monitoring (AMPM)
04/05/2004
2726
Back to top of chapter
