
February 2020 | Issue Brief
Medicaid Home and Community-Based Services
Enrollment and Spending
Molly O’Malley Watts, MaryBeth Musumeci, and Priya Chidambaram
Executive Summary
Medicaid fills in gaps in the overall health care system by serving as the primary source of coverage for
long-term services and supports (LTSS), including home and community-based services (HCBS), as
these services are typically unavailable and/or unaffordable through private insurance or Medicare.
HCBS help seniors and people with disabilities and chronic illnesses live independently outside
institutions by assisting with daily needs. This issue brief presents the latest (FY 2018) Medicaid HCBS
enrollment and spending data from KFF’s 18th annual 50-state survey. Appendix Tables contain detailed
state-level data. Key findings include the following:
Most HCBS enrollees receive services provided at state option. Over 2.5 million individuals
receive HCBS through an optional Section 1915 (c) or Section 1115 waiver, and nearly 1.2 million
receive optional personal care state plan services, while 600,000 receive home health state plan
services, the sole required benefit. Fewer individuals receive HCBS through the relatively newer state
plan options including Section 1915 (i) and Community First Choice.
Joint federal and state Medicaid HCBS spending totaled $92 billion in FY 2018, with nearly all
spending for optional services.
National per enrollee spending varies among the HCBS authorities, ranging from under $8,000
for Section 1915 (i) state plan services to nearly $30,000 for Section 1915 (c) waivers.
Per enrollee spending by Section 1915 (c) waiver target population is highest for people with
intellectual/developmental disabilities ($46,000). Per enrollee spending is relatively lower for
seniors/adults with physical disabilities ($16,000).
State Medicaid programs will face increased pressure to meet the health and LTSS needs of a growing
elderly population in the coming years, and their ability to do so could be affected by an economic
downturn that could leave states with limited resources and require reductions in services offered at state
option. In addition, if the ACA ultimately is struck down in Texas v. Azar, states would lose authority to
offer some HCBS as well as some flexibility to design benefit packages. The 2020 elections also could
have important implications for Medicaid and HCBS as policymakers may consider a range of proposals,
from those that could cap federal Medicaid financing program-wide as in the President’s FY 2020 budget
to proposals advocated by some Democrats to create a single, federal, universal health insurance
program known as Medicare-for-all.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
2
Introduction
Medicaid continues to be the primary source of coverage for long-term services and supports (LTSS),
financing over half of these services in 2018 (Figure 1). LTSS help seniors and people with disabilities
with self-care, such as bathing and dressing, and household activities, such as preparing meals and
managing medication. LTSS needs arise from a range of conditions, such as cognitive disabilities, like
dementia or Down syndrome; physical disabilities, like multiple sclerosis or spinal cord injury; mental
health disabilities, like depression or schizophrenia; and disabling chronic conditions, like cancer or
HIV/AIDS.
1
State Medicaid programs must cover LTSS in nursing homes, while most home and community-based
services (HCBS) are optional.
2
Spending on HCBS surpassed spending on institutional care for the first
time in 2013, and comprises 57% of total Medicaid LTSS spending as of 2016 (Figure 2). Factors
contributing to this trend include beneficiary preferences for HCBS, the fact that states are encouraging
HCBS as an alternative to typically more costly institutional care, and states’ community integration
obligations under the Americans with Disabilities Act and the Supreme Court’s Olmstead decision. In
Olmstead, the Supreme Court held that the unjustified institutionalization of people with disabilities is
illegal discrimination and violates the Americans with Disabilities Act.
NOTE: Total LTSS expenditures include spending on residential care facilities, nursing homes, home health services, and home and community-
based waiver services. Expenditures also include spending on ambulance providers and some post-acute care. This chart does not include Medicare
spending on post-acute care ($83.3 billion in 2018). All home and community-based waiver services are attributed to Medicaid.
SOURCE: KFF estimates based on 2018 National Health Expenditure Accounts data from CMS, Office of the Actuary.
Long-term services and supports (LTSS) spending, by payer,
2018.
Figure 1
Medicaid, 52%
Out-of-Pocket,
16%
Private Insurance,
11%
Other Public
and Private,
20%
Total National LTSS Spending = $379 billion
Medicaid LTSS Spending
= $196.9 billion

Medicaid Home and Community-Based Services Enrollment and Spending Growth
3
This issue brief presents the latest (FY 2018
3
) state-level Medicaid HCBS enrollment and spending data
from KFF’s 18th annual survey of all 50 states and DC. The survey tracks Medicaid HCBS across four
types of state plan benefits and two types of waivers, which are described in more detail in Table 1,
4
and
also presents enrollment and spending by target population where relevant. In general, state plan benefits
are provided to all Medicaid beneficiaries for whom they are medically necessary. Waivers allow states to
provide services to specific populations, set enrollment caps, and expand income and asset limits. State
plan HCBS include home health; personal care; Section 1915 (i), which authorizes HCBS targeted to a
particular population with functional needs that are less than an institutional level of care; and Community
First Choice (CFC) attendant services and supports. HCBS waivers include Section 1915 (c) and Section
1115,
5
both of which allow states to expand financial eligibility and offer HCBS to seniors and people with
disabilities who would otherwise qualify for an institutional level of care, while limiting enrollment.
6
The
Appendix Tables contain detailed state-level data. A related brief presents the latest data and highlights
themes in state HCBS policies.
SOURCE: Steve Eiken, Kate Sredl, Brian Burwell, and Angie Amos, Medicaid Expenditures for Long-Term Services and Supports in FY 2016 (IBM
Watson Health, May, 2018), https://www.medicaid.gov/medicaid/ltss/downloads/reports-and-evaluations/ltssexpenditures2016.pdf.
Medicaid long-term services and supports spending, by
institutional vs. community setting.
Figure 2
1995 2000 2005 2010 2012 2013 2014 2015 2016
Home and
Community-Based
LTSS
Institutional LTSS
$57
$76
$107
$139
$142
$146
$152
$159
$167
82%
63% 52%
51%
49%
73%
18%
27%
37%
48%
49% 51%
47%
53%
54%
46%
57%
43%
Annual Medicaid LTSS Spending, in billions:

Medicaid Home and Community-Based Services Enrollment and Spending Growth
4
Table 1: Medicaid Home and Community Based Services (HCBS) Authorities
State Plan Benefits
Home
Health
Services
Part-time or intermittent nursing services, home health aide services, and medical
supplies, equipment and appliances suitable for use in the home
At state option - physical therapy, occupational therapy, and speech pathology and
audiology services
Required
Personal
Care
Services
Assistance with self-care (e.g., bathing, dressing) and household activities (e.g.,
preparing meals)
Optional
Community
First
Choice
Attendant services and supports for beneficiaries who would otherwise require
institutional care
Income up to 150% FPL or eligible for benefit package that includes nursing home
services; state option to expand financial eligibility to those eligible for HCBS waiver
Optional
Section
1915 (i)
Case management, homemaker/home health aide/personal care services, adult day
health, habilitation, respite, day treatment/partial hospitalization, psychosocial
rehabilitation, chronic mental health clinic services, and/or other services approved
by the Secretary
Beneficiaries must be at risk of institutional care
Population targeting permitted
Optional
HCBS Waivers
Section
1915 (c)
Same services as available under Section 1915 (i)
Beneficiaries must otherwise require institutional care
Secretary can waive regular program income and asset limits
Cost neutrality required (average per enrollee cost of HCBS cannot exceed average
per enrollee cost of institutional care)
Enrollment caps permitted
Geographic limits permitted
Population targeting permitted
Optional
Section
1115
Secretary can waive certain Medicaid requirements and allow states to use Medicaid
funds in ways that are not otherwise allowable under federal rules for experimental,
pilot, or demonstration projects that are likely to assist in promoting program
objectives
Federal budget neutrality required
HCBS enrollment caps permitted
Optional

Medicaid Home and Community-Based Services Enrollment and Spending Growth
5
HCBS Enrollment and Spending by Authority
Nearly all HCBS are provided at state option. Home health state plan services are the only HCBS that
are required for states participating in Medicaid, covering 616,800 enrollees. Among the optional HCBS
authorities, waivers continue to be the most commonly used. While some states have taken up Section
1915 (i) and/or CFC, these relatively newer state plan options have not supplanted waivers as the primary
authority through which HCBS are provided. Personal care services are the most commonly used HCBS
state plan option, offered in 34 states (Figure 3 and Appendix Table 1).
Enrollment across the various HCBS authorities ranges from 81,000 individuals receiving Section
1915 (i) state plan services to 1.8 million individuals receiving Section 1915 (c) waiver services
(Figure 3 and Appendix Table 1). Most HCBS enrollees receive services provided through an optional
authority. Over 2.5 million individuals receive HCBS through a Section 1915 (c) or Section 1115 waiver,
and nearly 1.2 million individuals are served in the personal care state plan option, while about 600,000
individuals receive home health state plan services through the sole required HCBS benefit. Total home
health state plan enrollment omits some or all individuals in four states (AZ,
7
HI,
8
NE,
9
and TX
10
) and total
personal care state plan enrollment omits individuals in two states (KS
11
and NM
12
) that provide services
through capitated managed care and cannot separately report enrollment data. In addition, New York is
unable to report enrollment for CFC and Section 1115.
13
HCBS enrollment under a state plan authority is slightly less than enrollment under a waiver
authority (2.3 million vs. 2.5 million) (Figure 3). Total HCBS enrollment across all authorities is not
presented as individuals may receive services under more than one authority. For example, in some
states, an individual could receive some personal care hours through the state plan option and additional
personal care hours through a Section 1915 (c) waiver. States can choose to allow enrollees to self-direct
their personal care and/or home health services. Box 1 contains enrollment data for those services.
NOTES: Home health omits AZ and HI and includes only fee-for-service in NE and TX (omits capitated managed care). Personal care omits KS and
NM. CFC and Section 1115 omit NY. Section 1115 includes states with Section 1115 HCBS waivers without any accompanying Section 1915 (c)
waivers. SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.
Enrollment in Medicaid HCBS by program authority, FY 2018.
Figure 3
616,800
1,173,900
392,700
81,000
1,806,600
698,500
Home health services Personal care services Community First Choice Section 1915 (i) Section 1915 (c) Section 1115
Number of enrollees:
State plan services enrollment = 2,264,400
51 states
Waiver enrollment = 2,505,300
Mandatory
Optional
34 states
8 states
11 states
48 states
12 states

Medicaid Home and Community-Based Services Enrollment and Spending Growth
6
Box 1: Enrollment in Self-Directed Personal Care and
Home Health State Plan Services
Nearly 700,000 people are self-directing personal care state plan services in 15 (of 20) states
reporting this data.
14
Self-direction typically allows enrollees to select and dismiss their direct care
workers, determine worker schedules, set worker payment rates, and/or allocate their service
budgets.
15
The number of individuals self-directing services varies considerably from state to state.
California has the greatest number of individuals (over 516,000) self-directing personal care state
plan services, followed by Michigan (61,000) and Massachusetts (45,000). Self-direction of home
health state plan services is less common. Among the three states that allow self-direction for home
health state plan services, one state reports enrollment data (over 12,400 individuals in NJ).
16
Medicaid HCBS spending totaled $92 billion in FY 2018, with nearly all spending for services
provided at state option. Six percent of total HCBS spending is devoted to mandatory home health state
plan services (Figure 4 and Appendix Table 2). Additionally, over two-thirds of all Medicaid HCBS
spending is on services provided under a waiver authority compared to a state plan authority. Total
spending under a state plan authority is under $30 billion, or about one-third of total Medicaid HCBS
spending. Total home health state plan spending omits some or all spending in four states (AZ,
17
HI,
18
NE,
19
and TX
20
) and total personal care state plan spending omits two states (KS
21
and NM
22
) that provide
services through capitated managed care and cannot separately report spending data. In addition, New
York is unable to report spending for CFC and Section 1115,
23
and DC is unable to report spending for
Section 1915 (i).
NOTE: Home health omits AZ and HI and includes only fee-for-service in NE and TX (omits capitated managed care). Personal care omits KS and
NM. CFC and Section 1115 omit NY. Section 1915 (i) omits DC. Section 1115 includes Section 1115 HCBS waivers without an accompanying Section
1915 (c) waiver. SOURCE: KFF Medicaid FY 2018 HCBS program surveys.
Medicaid HCBS spending by program authority, FY 2018.
Figure 4
Home health state plan,
$5.5 billion,
6%
Personal care
state plan,
$15.1 billion,
17%
Community First
Choice, $8.7 billion,
9%
Section 1915 (i)
state plan,
$641 million,
1%
Section 1915 (c)
waiver, $53.5 billion,
58%
Section 1115
waiver,
$8.9 billion,
10%
Total Medicaid HCBS spending = $92 billion
Waiver spending =
$62.5 billion
State plan spending
= $29.5 billion

Medicaid Home and Community-Based Services Enrollment and Spending Growth
7
National per enrollee spending varies among the HCBS authorities, ranging from under $8,000 for
Section 1915 (i) state plan services to nearly $30,000 for Section 1915 (c) waivers (Figure 5 and
Appendix Table 3). This variation likely is due to the type and extent of services provided in the different
HCBS authorities. For example:
Lower per enrollee spending for Section 1915 (i) compared to other authorities may reflect that
Section 1915 (i) serves enrollees with functional needs that are less than an institutional level of
care. By contrast, Section 1915 (c) waivers generally require enrollees to meet an institutional
level of care and therefore are likely to serve individuals with more extensive and intensive – and
therefore generally costlier -- service needs.
Lower per enrollee spending on home health state plan services compared to other authorities
likely reflects shorter periods of service utilization. In contrast, Section 1915 (c) waiver enrollees
typically use services over an extended period of time, due to chronic long-term needs.
24
Lower per enrollee spending for Section 1115 waivers compared to Section 1915 (c) waivers may
reflect that most Section 1115 waiver states use this authority for seniors and adults with physical
disabilities but continue to serve people with intellectual or developmental disabilities (I/DD), the
costliest population, through Section 1915 (c).
Enrollment and spending increased in each HCBS authority from FY 2017 to FY 2018, except
home health state plan services (Table 2).
25
The two authorities with the largest percent increases in
total spending were CFC and personal care state plan services; spending increases in these authorities
appear to be driven by increased per enrollee costs rather than by increased enrollment. Notable state-
level changes from FY 2017 to FY 2018 include the following:
SOURCE: KFF Medicaid FY 2018 HCBS program surveys.
Medicaid HCBS spending per enrollee, by program authority,
FY 2018
Figure 5
$9,000
$12,800
$22,000
$7,900
$29,600
$12,800
Home health state plan Personal care state plan Community First Choice Section 1915 (i) state
plan
Section 1915 (c) waiver Section 1115 waiver
Spending Per Enrollee:
State plan spending per enrollee = $13,200 Waiver spending per enrollee = $24,900
Mandatory
Optional

Medicaid Home and Community-Based Services Enrollment and Spending Growth
8
Sizeable growth in CFC total spending and spending per enrollee is largely attributable to
substantially increased spending in California (76%). More modest growth in CFC enrollment
primarily reflects an increase from 61,000 to nearly 80,000 individuals in Washington.
Increased total spending and spending per enrollee for personal care state plan services reflects
notable spending growth in South Dakota, Colorado, and California. Although enrollment in
personal care state plan services increased slightly across all states electing this option, two
states (MD and MT) had enrollment declines in both FY 2017 and FY 2018, as individuals
transitioned to CFC services.
Growth in Section 1915 (c) waiver spending reflects notable increases in Nebraska (36%) and
Pennsylvania (19%). Specifically, spending in one I/DD waiver in Nebraska grew substantially
(87%), while spending in three Pennsylvania waivers serving seniors and adults with physical
disabilities and individuals with I/DD grew by more than 20 percent.
Growth in Section 1115 waiver enrollment was driven by an increase in New Jersey (19%).
Growth in Section 1915 (i) enrollment is largely due to an increase from 3,100 to 7,000 individuals
in Ohio.
Home health state plan services is the only authority with both enrollment and spending declines, which
could be attributable at least in part to increased enrollment in capitated managed care, and states’
inability to isolate home health enrollment and spending from other services included in the capitation
payment. States with substantial home health state plan enrollment declines as a result of such data
limitations include Texas (-55%) and Nebraska (-85%). Overall enrollment across all HCBS state plan
authorities also decreased from FY 2017 to FY 2018, likely driven by the home health decrease.
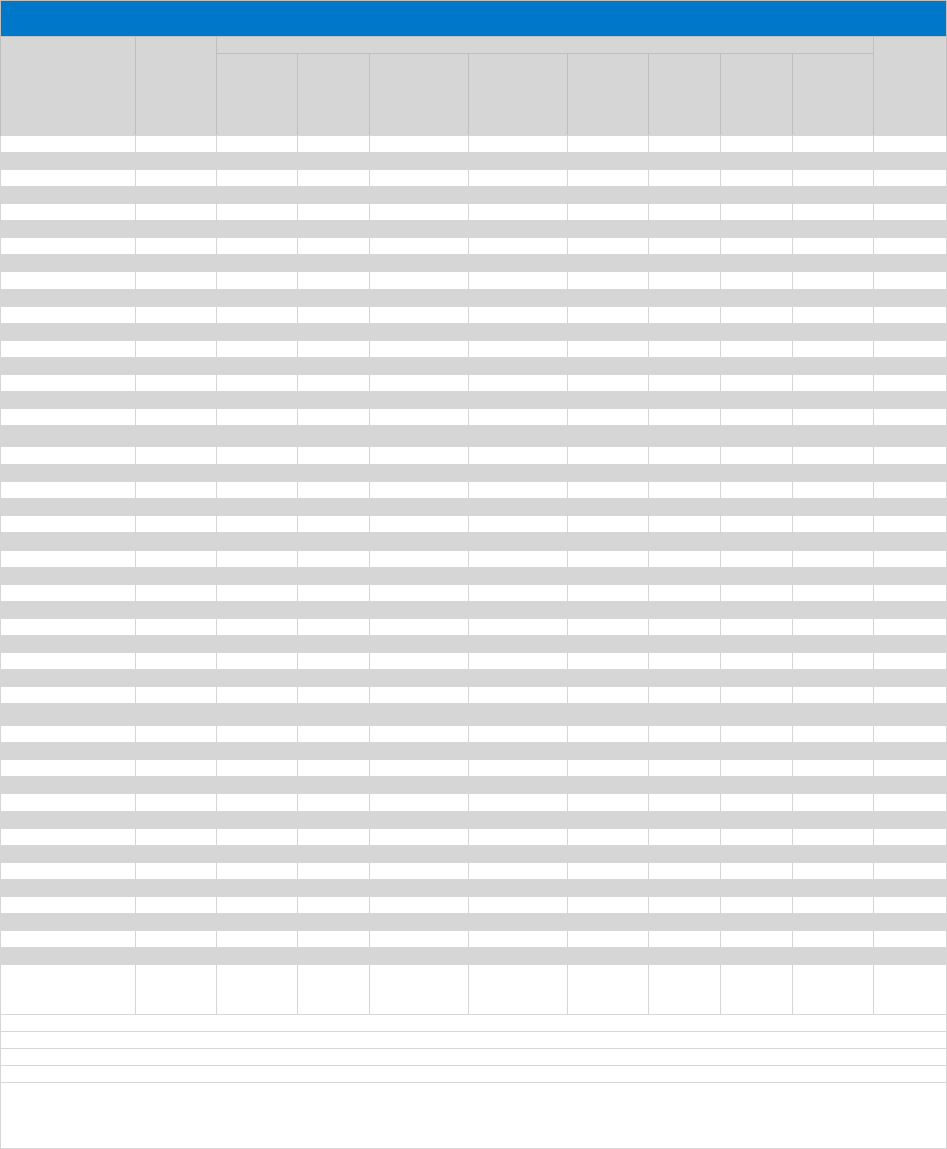
Year Home Health
Personal
Care
Community
First Choice
Section
1915 (i)
State Plan
Authority
Total
Section
1915 (c)
Section
1115
Waiver
Authority
Total
FY 2017 659,118 1,156,455 381,599 77,073 2,274,245 1,744,590 660,295 2,404,885
FY 2018 616,762 1,173,943 392,678 80,997 2,264,380 1,806,838 698,499 2,505,337
% Change -6% 2% 3% 5% -0.40% 4% 6% 4%
FY 2017 $6,021,542 $13,477,500 $5,951,319 $606,844 $26,057,205 $50,038,136 $8,636,374 $58,674,510
FY 2018 $5,530,014 $15,070,520 $8,650,291 $640,850 $29,891,675 $53,469,983 $8,944,964 $62,414,947
% Change -8% 12% 45% 6% 15% 7% 4% 6%
FY 2017 $9,136 $11,654 $15,596 $7,874 $11,458 $28,682 $13,080 $24,398
FY 2018 $8,966 $12,838 $22,029 $7,912 $13,201 $29,593 $12,806 $24,913
% Change -2% 10% 41% 0% 15% 3% -2% 2%
SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.
Table 2: Medicaid HCBS Enrollment and Spending, by Authority, FY 2017 and FY 2018
State Plan Services
Waiver Services
National Enrollment
National Average Spending (in thousands)
National Average Spending Per Enrollee

Medicaid Home and Community-Based Services Enrollment and Spending Growth
9
HCBS Enrollment and Spending by Target Population
Section 1915 (c) waivers
26
People with I/DD account for less than half of overall Section 1915 (c) waiver enrollment but more
than two-thirds of spending (Figure 6 and Appendix Tables 4 and 5).
27
Spending for this population is
disproportionate to their enrollment as a result of their generally more intensive needs. By contrast,
seniors and people with physical disabilities comprise over half of Section 1915 (c) waiver enrollment and
over a quarter of spending.
28
Other target populations, including people with mental health disabilities,
29
people with traumatic brain or spinal cord injuries (TBI/SCI),
30
children who are medically fragile or
technology dependent,
31
and people with HIV/AIDS,
32
together account for a small share of Section 1915
(c) waiver enrollment and spending.
NOTES: Percentages may not sum to 100% due to rounding. Other Populations include children who are medically fragile or technology dependent,
people with HIV/AIDS, people with mental health disabilities, and people with traumatic brain or spinal cord injuries.
SOURCE: KFF Medicaid FY 2018 HCBS program surveys.
Medicaid § 1915 (c) HCBS waiver enrollment and spending
by target population, FY 2018.
Figure 6
People with Intellectual/
Developmental
Disabilities,
786,000
43%
People with Intellectual/
Developmental
Disabilities,
$36 billion
68%
Seniors and People with
Physical Disabilities,
958,000
53%
Seniors and People with
Physical Disabilities,
$15.4 billion, 29%
Other Populations,
63,000
3%
Other Populations,
$1.7 billion
3%
Enrollees Expenditures
Total = $53.5 billionTotal = 1.8 million
NOTES: I/DD = intellectual and developmental disabilities. TBI/SCI = traumatic brain injuries/spinal cord injuries. Other states serve HCBS waiver
populations through Section 1115.
SOURCE: KFF Medicaid FY 2018 HCBS program surveys.
Section 1915 (c) waiver per enrollee spending, by target
population, FY 2018
Figure 7
$46,300
$16,000
$35,200
$11,100
$12,700
$43,700
I/DD Seniors &/or Adults with
Physical Disabilities
Medically Fragile/Tech.
Dep. Children
HIV/AIDS Mental Health TBI/SCI
Number of
states
serving
population:
11
21
48
42
18
5
Per enrollee spending by target population:

Medicaid Home and Community-Based Services Enrollment and Spending Growth
10
The fact that services for people with I/DD comprise over two-thirds of total Section 1915 (c)
waiver spending reflects high per enrollee costs for this population. There is substantial variation in
per enrollee spending among Section 1915 (c) waiver target populations, ranging from about $11,000 for
people with HIV/AIDS to over $46,000 for people with I/DD (Figure 7 and Appendix Table 6). Per enrollee
spending for people with I/DD is closely followed by the TBI/SCI population ($44,000) and medically
fragile children ($35,000). In addition to people with HIV/AIDS, per enrollee spending is relatively lower for
seniors and adults with physical disabilities ($16,000) and people with mental health disabilities
($13,000).
Section 1915 (i) state plan option
People with I/DD account for the vast majority of enrollment and spending in the Section 1915 (i)
state plan option, largely due to California’s program (Figure 8).
33
Unlike waivers which require an
institutional level of care, Section 1915 (i) state plan HCBS are provided to people with functional needs
that are less than an institutional level of care. The next largest Section 1915 (i) target population for both
enrollment and spending is people with mental health disabilities.
34
Nearly three-quarters of Section 1915
(i) enrollment for this population is in Iowa and Ohio, while Iowa’s program comprises most of the
spending ($94 million). Seniors and adults with physical disabilities account for a very small share of
Section 1915 (i) enrollment and spending.
35
Per enrollee spending is similar across Section 1915 (i) state plan HCBS target populations.
Section 1915 (i) state plan HCBS per enrollee spending was nearly $10,000 (in 2 of 3 states reporting
36
)
for seniors and adults with physical disabilities, less than $9,000 for people with I/DD (in 4 states
37
), and
under $6,000 for people with mental health disabilities (in 4 states
38
). Lower per enrollee spending for
Section 1915 (i) state plan HCBS compared to Section 1915 (c) waivers could reflect a more limited
scope benefit package and/or the fact that Section 1915 (i) enrollees have fewer and/or less intensive
needs (less than an institutional level of care) that Section 1915 (c) waiver enrollees (who must meet an
institutional level of care).
NOTES: Percentages may not sum to 100% due to rounding. Seniors/physical disabilities omits spending data for DC.
SOURCE: KFF Medicaid FY 2018 HCBS program surveys.
Medicaid § 1915 (i) HCBS state plan option enrollment and
spending by target population, FY 2018.
Figure 8
People with
Intellectual/
Developmental
Disabilities,
61,000,
75%
People with
Intellectual/
Developmental
Disabilities,
$520 million,
81%
Mental Health,
19,000,
24%
Mental Health,
$113 million,
18%
Seniors/
Physical
Disabilities,
1,000,
1%
Seniors/
Physical
Disabilities,
$8 million,
1%
Enrollees Expenditures
Total = $641 millionTotal = 81,000

Medicaid Home and Community-Based Services Enrollment and Spending Growth
11
Looking Ahead
Medicaid HCBS enrollment ranges from 81,000 individuals receiving Section 1915 (i) state plan services
to 1.8 million individuals receiving Section 1915 (c) waiver services, with joint federal and state spending
across all HCBS authorities totaling $92 billion in FY 2018. Medicaid HCBS promote independence and
self-determination for seniors and people with disabilities and chronic conditions by enabling them to
receive assistance with self-care needs and household activities outside an institution. Medicaid provides
substantial federal funding to help states meet their community integration obligations under Olmstead
and the Americans with Disabilities Act.
Most HCBS enrollees receive services provided through an optional authority, and nearly all HCBS
spending is devoted to authorities provided at state option. Although home health state plan services are
the only HCBS that states participating in Medicaid must offer, all states elect at least one optional HCBS
authority. While nearly all Medicaid HCBS authorities are optional, Medicaid fills a gap by covering HCBS
that are typically not available through private insurance or Medicare, and not affordable for many paying
out-of-pocket, especially those with lower incomes. The optional nature of most HCBS results in
substantial variation across states in enrollment and spending, reflecting states’ different choices about
optional authorities, benefit package contents, and scope of covered services. States would lose some of
their existing optional HCBS authorities and flexibility if the entire ACA ultimately is struck down in Texas
v. Azar.
39
Specifically, the option to offer CFC services would cease to exist, as would provisions that
provide states with the flexibility to offer the current full scope of Section 1915 (i) services and to target
those services to specific populations.
40
The optional nature of most HCBS has implications for federal and state spending, especially during
economic recessions. States face increasing pressures from revenue shortfalls during times of economic
downturn. Optional Medicaid eligibility pathways and services, including HCBS, may be at risk for cuts as
states must make difficult choices to balance their budgets.
41
The 2020 elections also could have important implications for Medicaid and HCBS as policymakers may
consider a range of proposals that could affect these populations and services. At one end of the
spectrum, a Medicaid program-wide federal financing cap is proposed in President Trump’s FY 2020
budget, though efforts to repeal and replace the ACA and cap federal Medicaid funding through a block
grant or per capita cap were narrowly defeated in Congress in 2017.
42
In addition, Tennessee has
submitted a proposal to CMS that seeks capped federal Medicaid funding through a Section 1115 waiver
pursuant to state legislation that includes some seniors, nonelderly adults with physical disabilities, and
children and adults with I/DD receiving HCBS.
43
Depending on how they are structured, policies that
would cap federal Medicaid funding could affect coverage, services, provider payment rates, and access
to care for vulnerable populations.
At the other end of the policy spectrum, continued attention to Medicaid HCBS enrollment and spending
is important to understanding proposals from some Democrats to create a single, federal, universal health
insurance program known as Medicare-for-all. One of the most fundamental changes under Medicare-for-
Medicaid Home and Community-Based Services Enrollment and Spending Growth
12
all would be uniform coverage of community-based long-term care services for all Americans. The current
Medicare-for-all proposals would require and explicitly prioritize HCBS over institutional services,
eliminating the state variation in eligibility, benefits, and payment and delivery systems that exists today
under Medicaid, while also shifting responsibility for designing and implementing much of health policy
from states to the federal government.
44
While the economy, the litigation challenging the ACA, and the upcoming election all will have
implications for Medicaid and HCBS, changing demographics also will result in increased pressure for
states to meet the health and LTSS needs of a growing elderly population in the coming years. The
number of adults age 65 and older is expected to more than double in size between 2014 and 2060, with
the largest increase during this period (18 million) expected in this decade, from 2020 to 2030.
45
With the
aging of the baby boomers, one in five U.S. residents will be age 65 or older by 2030,
46
and for the first
time in U.S. history, older adults are projected to outnumber children by 2034.
47
All of these factors make
continued attention to Medicaid’s role in providing HCBS an important policy area to watch.
MaryBeth Musumeci and Priya Chidambaram are with KFF.
Molly O’Malley Watts is with Watts Health Policy Consulting.
Medicaid Home and Community-Based Services Enrollment and Spending Growth
13
Appendix Tables
Appendix Table 1: Medicaid HCBS Enrollment, by State and Authority, FY 2018
Appendix Table 2: Medicaid HCBS Spending, by State and Authority, FY 2018
Appendix Table 3: Medicaid HCBS Spending Per Enrollee, by State and Authority, FY 2018
Appendix Table 4: Medicaid Section 1915 (c) HCBS Waiver Enrollment, by Target Population and State,
FY 2018
Appendix Table 5: Medicaid Section 1915 (c) HCBS Waiver Spending, by Target Population and State,
FY 2018
Appendix Table 6: Medicaid Section 1915 (c) HCBS Waiver Spending Per Enrollee, by Target Population
and State, FY 2018

Medicaid Home and Community-Based Services Enrollment and Spending Growth
14
Appendix Table 1: Medicaid HCBS Enrollment, By State and Authority, FY 2018
State
State Plan Services
Waivers
Home health
Personal care
Community
First Choice
Section 1915 (i)
Section 1915 (c)
Section 1115
Alabama
5,900
15,100
Alaska
300
3,700
4,300
Arizona
included in 1115
52,400
Arkansas
5,000*
13,700
15,500*
California
37,500*
273,800
228,200
55,800
149,500
474,300*
Colorado
23,500
100
46,300*
Connecticut
30,700
3,200
600
28,300
Delaware
14,000
400
1,200
6,900
DC
8,600*
6,000*
200*
6,900*
Florida
20,800
3,200
102,500
Georgia
6,200
42,600
Hawaii
included in 1115
2,900
8,500
Idaho
1,900
8,500
4,000
20,200
Illinois
14,400
161,600*
Indiana
16,300
4,700
49,100
Iowa
12,400
7,100
30,400*
Kansas
3,300
included in 1115
28,700
Kentucky
15,400
24,300*
Louisiana
6,600
14,200
20,600
Maine
1,900
3,300
7,500
Maryland
4,000
1,000
13,500
25,800
Massachusetts
52,200
45,000
30,600*
Michigan
3,300
60,700
24,700
Minnesota
28,900
43,700
81,500
Mississippi
1,400
700
25,800
Missouri
4,100
65,600
33,900
Montana
600
500
3,400
5,700
Nebraska
200^
3,800
11,800
Nevada
1,300
10,300
200
5,700
New Hampshire
1,400*
100*
9,200
New Jersey
50,300
49,500
10,700*
25,000
New Mexico
4,000
included in 1115
5,100
28,000
New York
101,400*
116,200*
NR
98,000*
NR
North Carolina
9,900
44,700
25,300*
North Dakota
1,100
1,300
5,800*
Ohio
26,900
7,000
111,400
Oklahoma
3,600
3,800
26,200*
Oregon
300
3,100
36,500
64,200*
Pennsylvania
26,300
119,700
Rhode Island
8,800
400
5,500
South Carolina
500
35,200*
South Dakota
11,200
1,600
5,900*
Tennessee
11,200
7,800
17,500
Texas
11,600^
369,700
30,000
200
48,100
68,800
Utah
3,100
200
9,300
Vermont
3,700
1,400
10,600
Virginia
1,600
51,300*
Washington
4,600
1,200
77,900
64,500
1,000
West Virginia
8,100
5,700
10,900
Wisconsin
5,900
17,900
89,900
Wyoming
400
5,300*
U.S. TOTAL
(51 states):
616,800
(51 states)
1,173,900
(34 states)
392,700
(8 states)
81,000
(11 states)
1,806,600
(48 states)
698,500
(12 states)
NOTES: Totals may not sum due to rounding. NR indicates state did not report data. Included in 1115 indicates that state was unable to
report state plan services separately from Section 1115 waiver services. Blank cell indicates state does not elect option. Total HCBS
enrollment across all authorities is not presented as individuals may receive services under more than one authority. *Data from year
other than FY 2018, as noted in table endnotes. ^NE and TX home health data are fee-for-service only and exclude capitated managed
care.
SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
15
Appendix Table 2: Medicaid HCBS Spending, By State and Authority, FY 2018 ($, in thousands)
State
State Plan Services
Waivers
Total HCBS
Spending
Home health
Personal care
Community
First Choice
Section
1915 (i)
Section
1915 (c)
Section
1115
Alabama
30,700
437,500
468,200
Alaska
1,400
61,900
265,100
328,400
Arizona
included in
1115
1,544,700
1,544,700
Arkansas
11,800*
94,300
389,600*
495,700
California
153,900*
2,960,800
5,562,600
494,600
3,810,300
4,679,100*
17,661,300
Colorado
345,800
1,200
903,700*
1,250,700
Connecticut
203,700
85,300
6,100
1,358,600
1,653,700
Delaware
63,900
500
137,200
87,200
288,800
DC
229,500*
254,000*
NR
295,000*
778,500
Florida
413,100
63,200
2,103,500
2,579,800
Georgia
4,700
1,212,900
1,217,600
Hawaii
included in
1115
135,600
104,200
239,800
Idaho
5,500
58,600
17,500*
364,000
445,600
Illinois
73,400
1,285,500*
1,358,900
Indiana
115,800
10,600
1,083,500
1,209,900
Iowa
44,600
94,400
647,900
786,900
Kansas
7,300
Included in 1115
1,198,300
1,205,600
Kentucky
30,500
805,100*
835,600
Louisiana
30,200
170,500
571,300
772,000
Maine
3,200
31,400
441,300
475,900
Maryland
2,900
7,300
300,400
1,145,200
1,455,800
Massachusetts
513,600
794,600
1,563,900*
2,872,100
Michigan
3,900
328,200
789,200*
1,121,300
Minnesota
67,800
1,017,200
2,911,800
3,996,800
Mississippi
1,600
7,600
400,800
410,000
Missouri
4,800
741,700
1,024,900
1,771,400
Montana
600
900
45,500
161,000
208,000
Nebraska
100^
15,400
365,700
381,200
Nevada
23,800
111,200
2,000
133,200
270,200
New Hampshire
6,500*
4,300*
315,700*
326,500
New Jersey
61,400
557,900
605,000*
183,000
1,407,300
New Mexico
12,000
included in 1115
379,900
329,400
721,310
New York
2,306,700*
3,274,500*
NR
6,426,100*
NR
12,007,300
North Carolina
12,800
450,500
897,500*
1,360,800
North Dakota
9,800
37,000
206,800*
253,600
Ohio
216,700
3,200
2,871,200
3,091,100
Oklahoma
15,700
10,900
476,400*
503,000
Oregon
300
7,100
673,700
100,700*
781,800
Pennsylvania
30,200
6,023,100
6,053,300
Rhode Island
115,400
6,300
71,800
193,500
South Carolina
4,200
657,700*
661,900
South Dakota
15,500
7,400
145,300*
168,200
Tennessee
226,500
684,400
297,400
1,208,300
Texas
13,900^
3,637,700
550,300
4,400
1,946,400
1,245,100
7,397,800
Utah
21,000
800
357,600
379,400
Vermont
7,600
13,900
401,700
423,200
Virginia
1,900
1,684,800*
1,686,700
Washington
6,000
6,400
1,432,500
728,600
1,300
2,174,800
West Virginia
9,400
69,400
406,300
485,100
Wisconsin
46,000
273,700
2,451,600
2,771,300
Wyoming
2,300
163,500*
165,800
U.S. TOTAL:
5,530,000
(51 states)
15,070,500
(34 states)
8,650,300
(8 states)
640,900
(11
states)
53,470,000
(48 states)
8,945,000
(12 states)
92,306,600
NOTES: Totals may not sum due to rounding. NR indicates state did not report data. Included in 1115 indicates that state was unable to
report state plan services separately from Section 1115 waiver services. Blank cell indicates state did not elect option. *Data from year
other than FY 2018, as noted in table endnotes. ^NE and TX home health data are fee-for-service only and exclude capitated managed
care. SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
16
Appendix Table 3: Medicaid HCBS Spending Per Enrollee, By State and Authority, FY 2018 ($)
State
State Plan Services
Waivers
Home health
Personal care
Community
First Choice
Section 1915 (i)
Section 1915 (c)
Section 1115
Alabama
5,200
29,000
Alaska
4,500
16,900
61,100
Arizona
included in
1115
29,500
Arkansas
2,300*
6,900
25,200*
California
4,100*
5,400
24,400
8,900
25,500
9,900*
Colorado
14,700
11,100
19,500*
Connecticut
6,600
26,600
9,800
48,100
Delaware
4,600
1,200
119,200
12,700
DC
26,800*
42,000*
NR
42,500*
Florida
19,800
20,000
20,500
Georgia
800
28,500
Hawaii
included in
1115
47,400
12,200
Idaho
2,900
5,400
7,600*
18,000
Illinois
5,100
8,000*
Indiana
7,100
2,200
22,000
Iowa
3,600
13,200
21,300*
Kansas
2,200
included in 1115
41,700
Kentucky
2,000
33,100*
Louisiana
4,500
12,000
27,700
Maine
1,700
9,500
59,200
Maryland
700
7,500
22,300
44,400
Massachusetts
9,800
17,600
51,100*
Michigan
1,200
5,400
32,000*
Minnesota
2,300
23,300
35,700
Mississippi
1,100
10,500
15,500
Missouri
1,200
11,300
30,300
Montana
1,000
1,800
13,200
28,200
Nebraska
300
4,000
31,100
Nevada
18,100
10,800
10,600
23,200
New Hampshire
4,700*
35,200*
34,300*
New Jersey
1,200
11,300
56,500*
7,300
New Mexico
3,000
included in 1115
75,200
11,800
New York
22,700*
28,200*
NR
65,600*
NR
North Carolina
1,300
10,100
35,500*
North Dakota
8,900
29,200
35,800*
Ohio
8,100
500
25,800
Oklahoma
4,400
2,900
18,200*
Oregon
1,000
2,300
18,500
1,600*
Pennsylvania
1,200
50,300*
Rhode Island
13,100
15,200
13,000
South Carolina
7,900
18,700*
South Dakota
1,400
4,700
24,500*
Tennessee
20,200
87,400
17,000
Texas
1,200
9,800
18,300
27,500
40,500
18,100
Utah
6,900
5,200
38,600
Vermont
2,100
9,700
37,900
Virginia
1,200
32,800*
Washington
1,300
5,300
18,400
11,300
1,300
West Virginia
1,200
12,100
37,300
Wisconsin
7,800
15,300
27,300
Wyoming
5,900
30,900*
U.S. TOTAL:
9,000
(51 states)
12,800
(34 states)
22,000
(8 states)
7,900
(11 states)
29,600
(48 states)
12,800
(12 states)
NOTES: Totals may not sum due to rounding. NR indicates state did not report data. Included in 1115 indicates that state was unable to
report state plan services separately from Section 1115 waiver services. Blank cell indicates state did not elect option. *Data from year
other than FY 2018, as noted in table endnotes.
SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
17
Appendix Table 4: Medicaid Section 1915 (c) HCBS Waiver Enrollment, by Target Population and by State, FY 2018
State
Total No.
of
§ 1915 (c)
Waivers
Enrollment by Target Population
Total
I/DD
Seniors
Seniors &
Adults with
Physical
Disabilities
Adults
with
Physical
Disabilities
Med.
Fragile/
Tech
Dep.
Children
HIV/
AIDS
Mental
Health
TBI/
SCI
Alabama
6
5,500
8,900
600
15,100
Alaska
4
2,200
2,000
200
4,300
Arkansas
4
4,500*
11,000
15,500
California
7
129,100
10,500
4,600
3,800
300
1,200
149,500
Colorado
11
12,500*
27,400*
1,800*
4,000*
600*
46,300
Connecticut
11
10,200
15,300
1,100
300
800
600
28,300
Delaware
1
1,200
1,200
DC
2
3,300*
3,700*
6,900
Florida
4
31,800
70,800
< 50
102,500
Georgia
4
13,000
28,100
1,500
42,600
Hawaii
1
2,900
2,900
Idaho
4
8,800
11,500
20,200
Illinois
9
22,800*
84,700*
10,800*
36,100*
900*
1,500*
4,900*
161,600
Indiana
4
26,600
22,300
200
49,100
Iowa
7
12,600
12,600
2,800
< 50
1,000
1,400
30,400
Kansas
7
9,600
6,000
6,700
600
5,300
500
28,700
Kentucky
6
14,800
9,000*
< 50
500
24,300
Louisiana
7
12,100
5,900
2,600
20,600
Maine
5
5,300
1,900
200
7,500
Maryland
6
16,200
9,200
200
100
25,800
Massachusetts
10
15,600*
14,600*
500*
30,600
Michigan
4
8,700
15,300
700
24,700
Minnesota
5
19,900
30,300
29,400
600
1,300
81,500
Mississippi
5
2,600
20,000
2,400
800
25,800
Missouri
9
15,000
16,500
2,300
100
33,900
Montana
4
2,700
2,600
400
5,700
Nebraska
5
4,900
6,900
<50
11,800
Nevada
3
2,200
2,700
800
5,700
New Hampshire
4
5,100
3,900
300
9,200
New Jersey
1
10,700*
10,700
New Mexico
3
5,100
5,100
New York
9
85,400*
2,500*
600*
6,400
3,100*
98,000
North Carolina
3
12,500*
10,000
2,900
25,300
North Dakota
6
5,500*
300
< 50
< 50
5,800
Ohio
7
40,200
64,600
6,600
111,400
Oklahoma
6
5,400*
20,800
100*
26,200
Oregon
6
22,500*
41,400
300*
64,200
Pennsylvania
10
40,300
44,700
33,800
1,000
119,700
South Carolina
7
11,500
20,400*
100*
1,400
800*
1,100
35,200
South Dakota
4
3,700*
2,100
100*
5,900
Tennessee
3
7,800
7,800
Texas
6
39,600
6,200
2,300
48,100
Utah
8
5,500
600
2,300
100
700
100
9,300
Virginia
5
13,100
38,200*
51,300
Washington
8
19,400
43,600
1,600
64,500
West Virginia
3
4,600
6,200
100
10,900
Wisconsin
6
28,800
61,100
89,900
Wyoming
5
2,600
2,500*
100
200*
5,300
TOTAL
(48 states):
265
785,800
(48
states)
162,500
(8
states)
667,000
(37 states)
128,200
(16 states)
17,100
(18
states)
3,600
(5
states)
25,100
(11
states)
17,500
(21
states)
1,806,800
No Section 1915 (c) Waivers (3 states)
Arizona
Rhode Island
Vermont
NOTES: I/DD = intellectual and developmental disabilities. TBI = traumatic brain injury. SCI = spinal cord injury. Totals may not sum due to rounding.
States may offer more than one Section 1915 (c) waiver per target population category. Programs with enrollment under 50 individuals are noted as < 50.
Blank cell indicates state does not offer Section 1915 (c) waiver for that population. *Data from year other than FY 2018, as noted in table endnotes.
SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
18
Appendix Table 5: Medicaid Section 1915 (c) HCBS Waiver Spending, by Target Population and by State, FY 2018 ($, in thousands)
State
Total No.
of § 1915
(c)
Waivers
Spending by Target Population
Total
I/DD
Seniors
Seniors &
Adults with
Physical
Disabilities
Adults with
Physical
Disabilities
Med.
Fragile/
Tech Dep.
Children
HIV/
AIDS
Mental
Health
TBI/
SCI
Alabama
6
351,300
78,400
7,800
437,500
Alaska
4
186,900
69,000
9,100
265,100
Arkansas
4
240,100*
149,500
389,600
California
7
3,474,900
39,800
108,900
175,400
2,600
8,700
3,810,300
Colorado
11
462,200*
361,500*
18,100*
38,300*
23,500*
903,700
Connecticut
11
883,000
395,400
2,100
100
14,700
63,300
1,358,600
Delaware
1
137,200
137,200
DC
2
226,100*
68,900*
295,000
Florida
4
1,067,000
1,036,500
< 50
2,103,500
Georgia
4
639,200
493,300
80,400
1,212,900
Hawaii
1
135,600
135,600
Idaho
4
266,900
97,000
364,000
Illinois
9
71,600*
429,400*
127,800*
558,200*
1,900*
24,000*
72,600*
1,285,500
Indiana
4
812,100
266,700
4,700
1,083,500
Iowa
7
520,600*
60,500*
23,600*
300*
10,300
32,500
647,900
Kansas
7
523,400
210,900
304,300
55,900
79,000
24,900
1,198,300
Kentucky
6
670,900
86,100*
2,600
45,600
805,100
Louisiana
7
454,900
112,500
3,900
571,300
Maine
5
385,100
40,000
16,100
441,300
Maryland
6
994,900
135,400
2,700
12,200
1,145,200
Massachusetts
10
1,301,200*
211,900*
50,900*
1,563,900
Michigan
4
444,600*
339,900
4,700*
789,200
Minnesota
5
1,403,400
435,600
932,600
42,400
97,900
2,911,800
Mississippi
5
104,300
233,900
44,100
18,400
400,800
Missouri
9
924,200
63,300
35,000
2,400
1,024,900
Montana
4
113,600
42,000
5,400
161,000
Nebraska
5
252,700
112,400
700
365,700
Nevada
3
114,400
13,900
4,900
133,200
New Hampshire
4
243,700*
48,900
23,100
315,700
New Jersey
1
605,000*
605,000
New Mexico
3
379,900
379,900
New York
9
5,970,300*
158,500*
5,400*
97,300
194,600*
6,426,100
North Carolina
3
652,100*
196,000
49,500
897,500
North Dakota
6
199,500*
6,900
200
100
206,800
Ohio
7
1,968,100*
777,500
125,600
2,871,200
Oklahoma
6
305,900*
165,900
4,600*
476,400
Oregon
6
58,500*
41,600
600*
100,700
Pennsylvania
10
3,177,600
1,481,600
1,331,200
32,700
6,023,100
South Carolina
7
423,300
192,200*
1,800*
3,300
4,700*
32,600
657,700
South Dakota
4
121,000*
20,600
3,700*
145,300
Tennessee
3
684,400
684,400
Texas
6
1,545,300
390,400
10,712
1,946,400
Utah
8
275,400
7,200
50,900
2,600
14,900
6,600
357,600
Virginia
5
908,100
776,700*
1,684,800
Washington
8
650,100
24,700
53,800
728,600
West Virginia
3
305,400
99,400
1,500
406,300
Wisconsin
6
632,800
1,818,800
2,451,600
Wyoming
5
118,100
37,400*
< 50
7,900*
163,500
TOTAL
(48 states):
265
36,386,500
(48 states)
1,592,700
(8 states)
10,132,900
(37 states)
3,629,900
(16 states)
604,000
(18
states)
40,000
(5
states)
318,100
(11
states)
765,900
(21
states)
53,470,200
No Section 1915 (c) Waivers (3 states)
Arizona
Rhode Island
Vermont
NOTES: I/DD = intellectual and developmental disabilities. TBI = traumatic brain injury. SCI = spinal cord injury. Totals may not sum due to rounding. States may offer
more than one Section 1915 (c) waiver per target population category. Programs with enrollment under 50 individuals are noted as < 50. Blank cell indicates state does not
offer Section 1915 (c) waiver for that population. *Data from year other than FY 2018, as noted in table endnotes.
SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.
Medicaid Home and Community-Based Services Enrollment and Spending Growth
19
Appendix Table 6: Medicaid Section 1915 (c) HCBS Waiver Spending Per Enrollee, by Target Population and by State, FY 2018 ($)
State
Total
No. of
Waivers
Per Enrollee Spending by Target Population
Total
I/DD
Seniors
Seniors &
Adults with
Physical
Disabilities
Adults with
Physical
Disabilities
Med.
Fragile/
Tech
Dep.
Children
HIV/
AIDS
Mental
Health
TBI/
SCI
Alabama
6
63,600
13,800
12,700
29,000
Alaska
4
86,400
35,100
42,900
61,100
Arkansas
4
53,500*
13,600
25,200
California
7
26,900
3,800
23,600
45,800
8,900
7,200
25,500
Colorado
11
37,000*
13,200*
9,900*
9,600*
41,300*
19,500
Connecticut
11
86,600
25,900
2,000
200
17,900
106,128
48,100
Delaware
1
119,200
119,200
DC
2
69,000*
18,800*
42,500
Florida
4
33,600
14,600
2,600
20,500
Georgia
4
49,000
17,600
53,700
28,500
Hawaii
1
47,400
47,400
Idaho
4
30,500
8,500
18,000
Illinois
9
3,100*
5,100*
11,900*
15,500*
2,300*
15,800*
14,800*
8,000
Indiana
4
30,500
12,000
24,700
22,000
Iowa
7
41,400*
4,800*
8,300*
9,600*
10,600
22,700
21,300
Kansas
7
54,500
35,200
45,400
93,200
14,900
46,400
41,700
Kentucky
6
45,300
9,600*
66,300
92,700
33,100
Louisiana
7
37,500
19,100
1.500
27,700
Maine
5
72,300
20,700
80,700
59,200
Maryland
6
61,200
14,700
12,600
126,800
44,900
Massachusetts
10
83,500*
14,600*
108,000*
51,100
Michigan
4
51,400*
22,200
6,400*
32,000
Minnesota
5
70,600
14,400
31,700
69,700
76,100
35,700
Mississippi
5
40,200
11,700
18,200
22,500
15,500
Missouri
9
61,800
3,800
15,100
31,300
30,300
Montana
4
41,400
16,100
15,000
28,200
Nebraska
5
51,800
16,400
33,400
31,100
Nevada
3
51,100
5,200
5,900
23,200
New Hampshire
4
47,900*
12,700
88,600
34,300
New Jersey
1
56,500*
56,500
New Mexico
3
75,200
75,200
New York
9
69,900*
63,000*
9,000*
15,300
62,100*
65,600
North Carolina
3
52,300*
19,700
17,100
35,500
North Dakota
6
36,500*
23,900
214,500
6,000
35,800
Ohio
7
48,900
12,000
19,100
25,800
Oklahoma
6
56,700*
8,000
52,100*
18,200
Oregon
6
3,800*
1,000
1,900*
1,600
Pennsylvania
10
78,900
33,200
39,400
33,900
50,300
South Carolina
7
36,900
9,400*
30,300*
2,300
5,900*
30,400
18,700
South Dakota
4
32,300*
9,900
34,500*
24,500
Tennessee
3
87,400
87,400
Texas
6
39,000
63,500
4,600
40,500
Utah
8
50,200
12,400
22,600
23,800
21,300
47,100
38,600
Virginia
5
69,300
20,300*
32,800
Washington
8
33,500
600
33,700
11,300
West Virginia
3
65,900
16,100
18,300
37,300
Wisconsin
6
22,000
29,800
27,300
Wyoming
5
46,000
15,200*
300
48,500*
30,900
TOTAL
(48 states):
265
46,300
(48
states)
9,800
(8
states)
15,200
(37 states)
28,300
(16 states)
35,200
(18
states)
11,100
(5
states)
12,700
(11
states)
43,700
(21
states)
29,600
No Section 1915 (c) Waivers (3 states)
Arizona
Rhode Island
Vermont
NOTES: I/DD = intellectual and developmental disabilities. TBI = traumatic brain injury. SCI = spinal cord injury. Totals may not sum due to rounding.
States may offer more than one Section 1915 (c) waiver per target population category Programs with enrollment under 50 individuals are noted as <
50. Blank cell indicates state does not offer Section 1915 (c) waiver for that population. *Data from year other than FY 2018, as noted in table
endnotes. SOURCE: KFF Medicaid HCBS Program Surveys, FY 2018.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
20
Table Notes
Arkansas: Home health data are from 2017. Wavier data are from 2015 (#936 I/DD).
California: Home health data are from 2016. Section 1115 waiver data are from 2015.
Colorado: Waiver data are from 2017 (#6 seniors/adults with physical disabilities, #7 I/DD, #268 mental health, #288
TBI/SCI, #293 I/DD, #305 I/DD, #450 children, #961 TBI/SCI, #4157 children, #4180 I/DD.)
District of Columbia: Home health, personal care, CFC, 1915 (i), and waiver data are from 2017.
Idaho: Section 1915 (i) spending and per enrollee spending data include only the adult DD program and exclude data
for the children’s DD program. The state reported 1,700 children with DD enrolled in 2017, but did not report
corresponding spending data.
Illinois: Waiver data are from 2015 (#143 seniors), 2016 (#278 children), and 2017 (#142 adults with physical
disabilities, #202 HIV/AIDS, #326 seniors/adults with physical disabilities, #329 TBI/SCI, #350 I/DD, #464 I/DD, #473
I/DD).
Iowa: Waiver enrollment data are from 2016 (#345 adults with physical disabilities, #4111 adults with physical
disabilities, #4155 seniors) and 2017 (#213 HIV/AIDS, #242 I/DD).
Kentucky: Waiver data are from 2017 (#144 seniors/adults with physical disabilities).
Massachusetts: Waiver data are from 2016 (#59 seniors/adults with physical disabilities) and 2017 (#359 TBI/SCI,
#826 I/DD, #827 I/DD, #828 I/DD, #1027 seniors/adults with physical disabilities, #1028 seniors/adults with physical
disabilities, #40207 I/DD, #40701 TBI/SCI, #40702 TBI/SCI).
Michigan: Waiver spending data are from 2016 (#167 I/DD, #438 mental health, #4119 I/DD).
New Hampshire: Home health and personal care data are from 2015. Waiver spending data are from 2016 (#397
I/DD).
New Jersey: Waiver data are from 2011 (#31 I/DD).
New York: Home health and personal care data are from 2017. Waiver data are from 2016 (#40176 children) and
2017 (#269 spending-only TBI/SCI, #444 spending-only seniors/adults with physical disabilities, #470 I/DD, and #471
children).
North Carolina: Waiver data are from 2016 (#432 I/DD).
North Dakota: Waiver data are from 2017 (#842 spending-only I/DD, #37 I/DD).
Oklahoma: Waiver data are from 2017 (#179 I/DD, #343 I/DD, #351 I/DD, #399 I/DD, #811 children).
Oregon: Waiver data are from 2017 (#117 I/DD, #375 I/DD, #565 children, #40193 children, #40194 I/DD).
South Carolina: Waiver data are from 2016 (#40181 adults with physical disabilities) and 2017 (#186 HIV/AIDS,
#405 seniors/adults with physical disabilities).
South Dakota: Waiver data are from 2016 (#44 I/DD, #264 TBI/SCI, #338 I/DD).
Virginia: Waiver data are from 2017 (#321 seniors/adults with physical disabilities).
Wyoming: Waiver data are from 2017 (#236 seniors/adults with physical disabilities, #370 TBI/SCI).

Medicaid Home and Community-Based Services Enrollment and Spending Growth
21
Endnotes
1
See, e.g., KFF, Medicaid Beneficiaries Who Need Home and Community-Based Services: Supporting Independent
Living and Community Integration (March 2014), http://kff.org/medicaid/report/medicaid-beneficiaries-who-need-
home-and-community-based-services-supporting-independent-living-and-community-integration/.
2
See generally KFF, Streamlining Medicaid Home and Community-Based Services: Key Policy Questions (March
2016), https://www.kff.org/medicaid/issue-brief/streamlining-medicaid-home-and-community-based-services-key-
policy-questions/; KFF, Medicaid Long-Term Services and Supports: An Overview of Funding Authorities (Sept.
2013), http://kff.org/medicaid/fact-sheet/medicaid-long-term-services-and-supports-an-overview-of-funding-
authorities/.
3
The Table Notes indicate where state-level data from a year prior to FY 2018 is used.
4
For additional background and current state policies relating to each of these authorities, see KFF, Key State Policy
Choices About Medicaid Home and Community-Based Services (Feb. 2020), https://www.kff.org/medicaid/issue-
brief/key-state-policy-choices-about-medicaid-home-and-community-based-services.
5
Enrollment and spending data for Section 1115 HCBS waivers includes those for which the state does not have an
accompanying Section 1915 (c) waiver.
6
Unlike HCBS waivers, state plan services must be provided to all beneficiaries for whom they are medically
necessary. However, states can manage enrollment for Section 1915 (i) state plan services by restricting functional
eligibility criteria for future beneficiaries if enrollment will exceed the state’s initial estimate.
7
AZ delivers home health state plan services through a Section 1115 capitated managed care waiver and is unable
to separately report unduplicated home health enrollment data. Instead, AZ’s home health state plan enrollment is
included in its Section 1115 waiver enrollment. In FY 2018, Arizona reported that all 52,400 of its Section 1115 waiver
enrollees received home health services.
8
HI delivers home health state plan services through a Section 1115 capitated managed care waiver and is unable to
separately report unduplicated home health enrollment data. Instead, HI’s home health state plan enrollment is
included in its Section 1115 waiver enrollment. In FY 2018, Hawaii reported that 2,500 of its 8,500 Section 1115
waiver enrollees received home health services.
9
NE reports home health state plan enrollment only for fee-for-service enrollees.
10
TX reports home health state plan enrollment only for fee-for-service enrollees.
11
KS delivers personal care state plan services through a Section 1115 capitated managed care waiver and is
unable to separately report unduplicated personal care enrollment data. Instead, KS’s personal care state plan
enrollment is included in its Section 1115 waiver enrollment.
12
NM delivers personal care state plan services through a Section 1115 capitated managed care waiver and is
unable to separately report unduplicated personal care enrollment data. Instead, NM’s personal care state plan
enrollment is included in its Section 1115 waiver enrollment.
13
NY is unable to report Section 1115 waiver managed LTSS enrollment by community vs. institutional setting. In
2015 (the most recent year for which NY data are available), 49,930 people received long-term institutional or HCBS
in NY’s Section 1115 waiver.
14
Among the 34 states offering the personal care state plan option, 20 allow self-direction. The 15 states reporting
self-directed enrollment data are AK, AR, CA, FL, ID, MA, MI, MO, MT, NJ, OK, TX, UT, VT and WA. The five states
that allow self-directed personal care state plan services but do not report enrollment are ME, MN, NV, NH and NY.
15
For additional information on states’ self-direction policies, see KFF, Key State Policy Choices About Medicaid
Home and Community-Based Services (Feb. 2020), https://www.kff.org/medicaid/issue-brief/key-state-policy-choices-
about-medicaid-home-and-community-based-services.
16
Three of 51 states allow individuals to self-direct home health state plan services. CA and NE allow self-direction
but are unable to report enrollment.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
22
17
AZ delivers home health state plan services through a Section 1115 capitated managed care waiver and is unable
to separately report home health spending data. Instead, AZ’s home health state plan spending is included in its
Section 1115 waiver spending. Total home health state plan spending was $70 million in AZ in FY 2018.
18
HI delivers home health state plan services through a Section 1115 capitated managed care waiver and is unable
to separately report home health spending data. Instead, HI’s home health state plan spending is included in its
Section 1115 waiver spending. Total home health state plan spending was $4 million in HI in FY 2018.
19
NE reports home health state plan spending only for fee-for-service enrollees.
20
TX reports home health state plan spending only for fee-for-service enrollees.
21
KS delivers personal care state plan services through a Section 1115 capitated managed care waiver and is
unable to separately report personal care spending data. Instead, KS’s personal care state plan spending is included
in its Section 1115 waiver spending.
22
NM delivers personal care state plan services through a Section 1115 capitated managed care waiver and is
unable to separately report personal care spending data. Instead, NM’s personal care state plan spending is included
in its Section 1115 waiver spending.
23
NY is unable to report Section 1115 waiver managed LTSS spending by community vs. institutional setting. In 2015
(the most recent year for which NY data is available), total institutional and HCBS Section 1115 waiver spending was
$146,589,000.
24
Section 1915 (c) waiver participants were enrolled about 300 days a year on average in 2016, the most recent year
data are available. KFF analysis based on CMS 372 reports for Section 1915 (c) waivers in 2016.
25
The FY 2018 survey asked states to update prior years’ (FY 2016 and FY 2017) spending and enrollment data if
necessary; therefore, all trend analyses reflected in this report includes the most recently reported FY 2017 data.
26
Section 1115 waiver enrollment is not presented by target population because, unlike Section 1915 (c) waivers,
Section 1115 waivers can include multiple populations, and states only report total Section 1115 waiver enrollment in
our survey.
27
48 states offer Section 1915 (c) waivers targeted to people with I/DD. The other three states (AZ, RI, and VT) serve
their entire I/DD waiver populations under Section 1115. In addition, two states (NY and TN) serve some people with
I/DD under Section 1115 and others under Section 1915 (c).
28
42 states offer Section 1915 (c) waivers targeted to seniors and/or adults with physical disabilities. The other nine
states (AZ, DE, HI, NJ, NM, RI, TN, TX, and VT) serve all senior and adult with physical disabilities waiver
populations under Section 1115. In addition, three states (CA, NY, and WA) serve some seniors and adults with
physical disabilities under Section 1115 and others under Section 1915 (c).
29
11 states offer Section 1915 (c) waivers targeted to people with mental health disabilities. Another two states (DE
and RI) serve people with mental health disabilities under Section 1115. In addition, WA serves some people with
mental health disabilities under Section 1115 and others under Section 1915 (c).
30
21 states offer Section 1915 (c) waivers targeted to people with TBI/SCI. Another four states (DE, RI, VT, and WA)
serve people with TBI/SCI under Section 1115.
31
18 states offer Section 1915 (c) waivers targeted to children who are medically fragile or technology dependent.
Another two states (HI and RI) serve children who are medically fragile or technology dependent under Section 1115.
32
Five states offer Section 1915 (c) waivers targeted to people with HIV/AIDS. Another three states (DE, HI, and RI)
serve people with HIV/AIDS under Section 1115.
33
Four states (CA, DE, ID, and MS) serve people with I/DD under Section 1915 (i).
34
Four states (IA, IN, OH and TX) serve people with mental health disabilities under Section 1915 (i).
35
Three states (CT, DC, and NV) serve seniors and/or people with physical disabilities under Section 1915 (i). DC did
not report spending data.
36
Reporting states include CT and NV; DC did not report.

Medicaid Home and Community-Based Services Enrollment and Spending Growth
23
37
CA, DE, ID, and MS. ID per enrollee spending includes only the program for adults with I/DD because the state
was unable to report spending data for the program for children with I/DD.
38
IA, IN, OH, and TX.
39
KFF, Explaining Texas v. U.S.: A Guide to the 5
th
Circuit Appeal in the Case Challenging the ACA (Jan. 2020),
https://www.kff.org/health-reform/issue-brief/explaining-texas-v-u-s-a-guide-to-the-case-challenging-the-aca/
40
KFF, Potential Impact of Texas v. U.S. Decision on Key Provisions of the Affordable Care Act (Jan. 2020),
https://www.kff.org/health-reform/fact-sheet/potential-impact-of-texas-v-u-s-decision-on-key-provisions-of-the-
affordable-care-act/.
41
See also KFF, State Variation in Medicaid Per Enrollee Spending for Seniors and People with Disabilities (May
2017), https://www.kff.org/medicaid/issue-brief/state-variation-in-medicaid-per-enrollee-spending-for-seniors-and-
people-with-disabilities/.
42
KFF, Medicaid Financing: The Basics (March 2019), https://www.kff.org/medicaid/issuebrief/medicaid-financing-
the-basics/.
43
KFF, Why It Matters: Tennessee’s Medicaid Waiver Block Grant Proposal (Dec. 2019),
https://www.kff.org/medicaid/issue-brief/why-it-matters-tennessees-medicaid-block-grant-waiver-proposal/.
44
KFF, How Will Medicare-for-all Proposals Affect Medicaid? (Sept. 2019), https://www.kff.org/medicaid/issue-
brief/how-will-medicare-for-all-proposals-affect-medicaid/.
45
U.S. Census Bureau, Projections of the Size and Composition of the U.S. Population: 2014 to 2060, Report
Number P25-1143, at 5 (March 2015), https://www.census.gov/library/publications/2015/demo/p25-1143.html.
46
U.S. Census Bureau, Older People Projected to Outnumber Children for First Time in U.S. History, Release
Number CB18-41 (March 13, 2018), https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-
projections.html.
47
Id.; U.S. Census Bureau, An Aging Nation: Projected Number of Children and Older Adults (last revised Oct. 9,
2019), https://www.census.gov/library/visualizations/2018/comm/historic-first.html.
