
Williams and Colbert Consent Decrees
Vision, Programming, and Expectations
SEPTEMBER 26, 2022
1

Welcome and Introductions
Illinois Department of Healthcare and Family Services
Theresa Eagleson, Director
Kelly Cunningham, Administrator of Medical Programs
Key Staff
Medicaid Managed Care Organizations
Illinois Department of Human Services
Grace Hou, Secretary
Key Staff
Williams and Colbert Comprehensive Program Prime Agencies
2

Purpose
To share the State’s vision for meeting its obligations
under the Williams and Colbert Consent Decrees.
To highlight the roles and responsibilities of
Comprehensive Program Prime Agencies and
Medicaid Managed Care Organizations in helping
the State achieve its vision.
3
Shared Success Depends on Coordination and Collaboration

Basis of Williams and Colbert Consent Decrees
Americans with Disabilities Act (ADA)of 1990
Prohibits discrimination on the basis of disability.
Introduces integration mandate:
Public entities, including HFS, DHS, and their contractors, must administer
services, programs, and activities in the most integrated setting appropriate to
the needs of qualified individuals with disabilities.
Olmstead Supreme Court Decision of 1999
Unnecessary institutionalization of people with disabilities is discrimination
under the ADA.
Williams and Colbert Consent Decrees can be viewed online at
IDHS: Olmstead Consent Decrees (state.il.us)
4

Requirements of Williams and Colbert
The State is required to deliver opportunities and support for community
integration to individuals in institutional settings.
Williams Class is comprised of individuals with Serious Mental Illness
who reside or have resided in a Specialized Mental Health
Rehabilitation Facilities (SMHRFs).
Colbert Class is comprised of individuals with disabilities who reside or
have resided in a Cook County Nursing Facility.
The State’s performance in both decrees is overseen by a single Court-
appointed Monitor.
Compliance entails meeting requirements set forth in the Consent
Decrees and implementing the strategies and achieving the milestones
negotiated annually with Plaintiffs’ Counsel and the Court Monitor.
5

Shared State Vision
A tightly coordinated and seamless experience
for all Class Members, characterized by proactive
collaboration between Prime Agencies and
Medicaid MCOs to deliver high quality services
to achieve and maintain community integration
and compliance with Consent Decree
requirements.
6

Comprehensive Program
Operated by the Department of Human Services, the lead state agency
for implementing and coordinating on the requirements of the Williams and
Colbert Consent Decrees.
The Comprehensive Program is the primary vehicle for satisfying Class
Member-facing requirements of the Decrees.
7

Comprehensive Program
Goals:
To maximize continuity of services by partnering with providers who can work with Class
Members along the entire continuum of services. The continuum includes the four core
services required by both Consent Decrees (Outreach, Assessment, Service Planning, &
Transition), as well as an array of ancillary services that address various barriers to
transition, all managed through a Care Management approach.
Better integrate and align services for Colbert and Williams Class Members, ensuring that
all Class Members can access appropriate services regardless of current institutional
placement.
Identify opportunities to better align the Olmstead service system with the Medicaid
program, both in terms of covered services and the managed care service delivery
system. Because care coordination is an expectation of Medicaid MCOs, DHS will work
closely with HFS to identify and avoid or resolve any duplication of services.
8
Prime Agency Grant Agreements
Grant agreements contain multiple deliverables relevant to the Williams
and Colbert Consent Decrees and best practices for serving Class
Members.
Expenditure-based funding model with advance-and-reconcile payments
for FY23 and for future fiscal years when providers have adequate financial
management systems under GATA. Smaller outcome-based payments are
offered as a supplemental incentive for high performance.
9
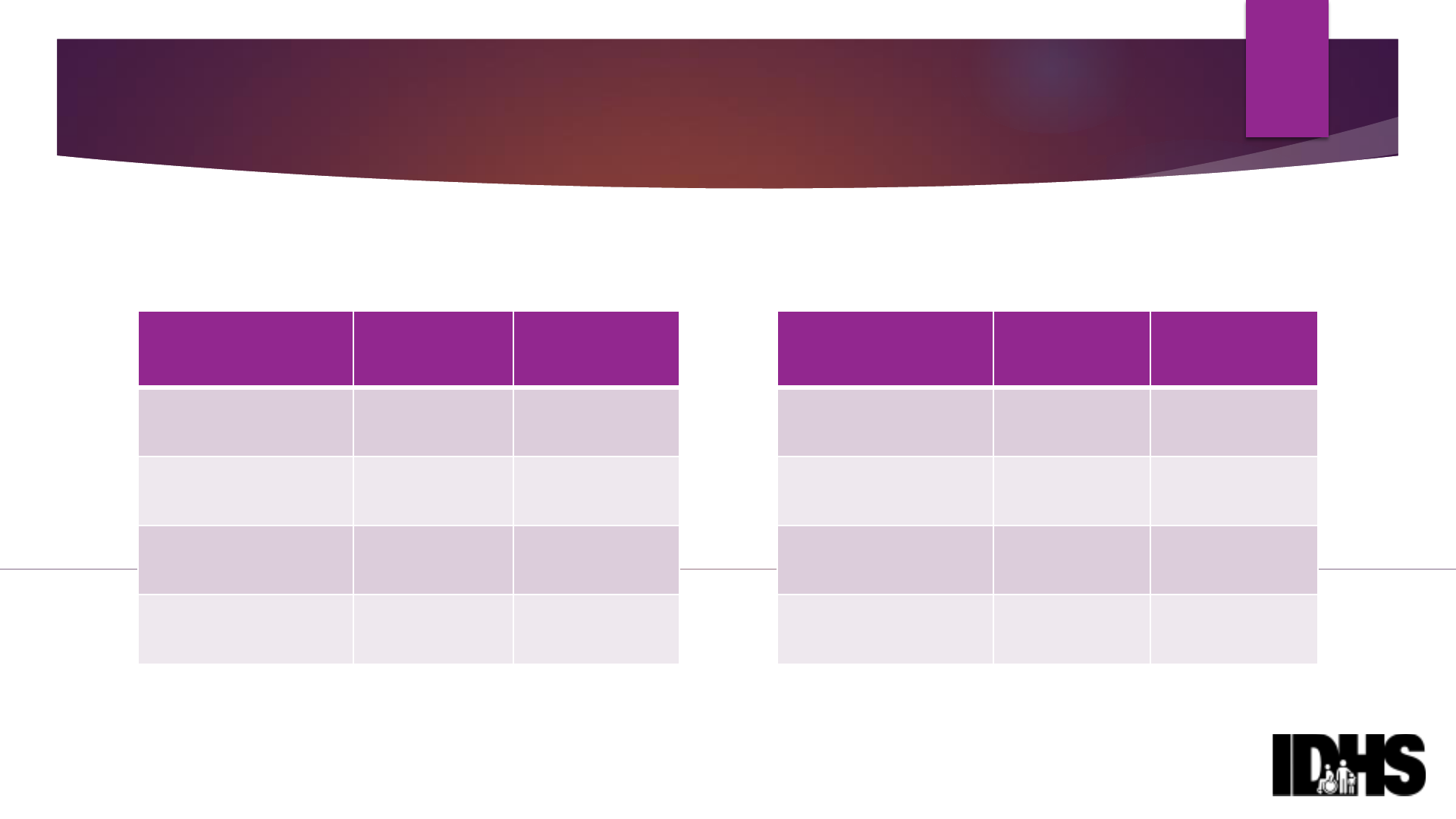
Comprehensive Program Historical
Transition Requirements & Performance
Fiscal Year
Williams
Required*
Williams
Achieved*
FY20
(starting March 2020)
109
32 (29%)
FY21
407
178 (36%)
FY22
407
352 (86%)
FY23
400
42**
10
Fiscal Year
Colbert
Required*
Colbert
Achieved*
FY20
(starting March 2020)
225
35 (16%)
FY21
901
227 (25%)
FY22
462
396 (86%)
FY23
450
61**
*Moves to community
**As of 9/19/22
*Moves to community
**As of 9/19/22

Services & Staffing – Outreach
11
Service
Staffing
Responsibility
Outreach
Outreach Workers
(Peers
preferred)
Offer assessment and
engagement in the program,
conduct Brief Screen, &
education on CM rights.
Address any transition
concerns expressed by CM.
Initial outreach within 60
-70
days of CM admission to
facility. Follow
-up outreach of
CMs not already in program,
annually or within 14 days of
request.

Services & Staffing – Care Management
12
Service
Staffing
Responsibility
Care Management (incl.
Assessment & Service
Planning)
Care Managers
(Master’s
degree in counseling, social work,
psychology, or other highly related
field, supervised by an LPHA, RN, or
OT with oversight of the care
manager’s work)
A comprehensive, person
-
centered approach to working
with Class Members that
involves assessment,
collaboration with other
providers, working with social
supports, as well as
developing, implementing,
and evaluating a
comprehensive, Class
Member
-
focused service plan.
Care Management involves
intensive care coordination in
addition to this broader set of
tasks throughout the program.

Services & Staffing – Other Services
13
Service
Staffing
Responsibility
Housing Location/Transition
Coordination
Housing Locators/Transition
Coordinators
Locating & securing
housing; move into the
community
Integrated Healthcare
Licensed Registered Nurses
& Licensed Occupational
Therapists
Healthcare assessments &
care coordination
SSI/SSDI Outreach, Access,
and Recovery (SOAR)
SOAR Worker
(Bachelor’s degree
or certified as Certified Recovery
Support Specialist (CRSS) or Certified
Peer Recovery Specialist (CPRS).
Become SOAR trained (online) and
certified within 40 days from the date
of hire)
Completion & submission of
SOAR applications/appeals

Partnerships
Prime Agencies’ engagement and coordination with various IDHS partners
serves in the interest of facilitating safe and timely Class Member transitions.
UIC- College of Nursing
UIC- Jane Addams College of Social Work
UIC- Assistive Technology Unit
UIC- Department of Psychiatry
Subsidy Administrators – Catholic Charities & IACAA
IDHS-DRS Home Services Programs & IDoA Community Care Program
IDHS-FCS Medicaid & SNAP Applications
14
Coordination with MCOs
Prime Agencies’ engagement of Medicaid MCOs in planning and
problem-solving is essential to Class Members’ success and the State’s
compliance under the Decrees.
Prime Agencies are required to coordinate with MCOs for the purposes of
facilitating safe Class Member transitions
Notification and involvement in Service Planning (pre-discharge planning) &
discharge planning.
Coordination on the establishment of community-based services/supports
authorized and covered by the MCO
Notification and involvement in transition to the community
15

Comprehensive Program Barriers &
Solutions
Staffing shortages – Grant funding for competitive salaries, retention/hiring
bonuses; other DMH efforts
Securing affordable housing – Fair Market Rent overage waivers
Accessing & securing community-based Medicaid services, including
home and community-based waiver services – MCO contacts provided
and DHS/HFS support to resolve issues
Facility barriers – IDPH investigation process, DHS & DPH support and
intervention to resolve issues
16

Path Forward
In partnership with IDHS and other entities, we hope Primes will continue to
make every effort to meet transition requirements.
IDHS would like to continue to problem-solve with you on barriers/issues you
face in achieving safe and timely transitions.
It is through these collaborative efforts and shared dedication to Class
Members that we can achieve success!
17

Q&A Opportunity for MCOs
What information surprised you or is new to you about the work of Prime
Agencies?
What additional information would be helpful to know about the work of
Prime Agencies?
How can IDHS &/or the Primes be helpful to MCOs related to Class
Member transitions?
18

Medicaid Managed Care Organizations
Contracted by the Department of Healthcare and Family Services, a
Defendant in the Consent Decrees.
Responsible for providing Medicaid-covered services to ALL Class Member
enrolled in managed care.
Includes partnering effectively with Primes.
Community Transition Initiative
Incentive program operating parallel to the Comprehensive Program.
MCOs (rather than Prime agencies) initiate and provide all Decree-specified
services to which Class Members are entitled.
MCO performance partnering with Primes and achieving
independent success under CTI is closely monitored by Plaintiffs,
Court Monitor, and Governor’s Office.
19

Medicaid Managed Care Contracts
Contracts contain multiple provisions
relevant to compliance with the ADA, the
Olmstead Decision, and the Williams and
Colbert Consent Decrees.
20

Care Coordination
Deliberate organization of a member’s care activities is the
foundation of the state’s investment in the Medicaid managed
care service delivery system.
Ensures that members receive the appropriate care at the right
time and in the right setting.
Proactive care coordination aligned with ADA and Olmstead
standards is a minimal expectation for all MCOs working with Class
Members, whether the individual is paired with a Prime agency,
working with MCO under the CTI, or desiring to continue
receiving care in the institutional setting.
21

Care Coordination (continued)
Care management is explicitly required for:
All nursing facility residents and SMHRF residents.
All members receiving HCBS waiver services.
22

Network Adequacy Standards
Require that all MCO members, including Class Members who
transition to community settings, have adequate access and
proximity to primary care and behavioral health providers,
pharmacies, and other needed Medicaid-covered services.
HFS expects that health plans will work proactively with Primes
and other community providers to ensure that robust services
are available to support community integration.
Thoughtful creativity and innovation in this area is
encouraged to mediate staff shortages.
23

MCO Staffing
MCOs are well-staffed to support Class Members and to
coordinate with Prime Agencies on their behalf.
Key positions
Long Term Services and Supports Program Manager ensures that LTSS staff are
knowledgeable and adhere to the requirements of the Williams and Colbert
consent decrees.
Community Liaison develops and maintains relationships with community
entities and state agencies.
Quality Management Coordinator monitors and audits plan’s health care
delivery system to ensure success of efforts to improve health status and
health outcomes for members.
Compliance Officer ensures compliance with contract.
24

MCO Staffing (continued)
Designated Liaisons
Consumer advocate for enrollees who need behavioral health
services, responsible for internal advocacy for these enrollees’
interests, including ensuring input in policy development, planning,
decision-making, and oversight, as well as coordination of recovery
and resilience activities.
Consumer advocate for Dual-Eligible Adults, responsible for internal
advocacy for these enrollees’ interests, including ensuring input in
policy development, planning, decision-making, and oversight.
25

Services for Williams Class Members
MCO contracts require health plans to implement any Behavioral
Health service plan for a Williams Class Member developed by
DHS contractors (i.e., Prime agencies), unless both the managed
care member and the Prime agency agree to modify the plan.
MCO is responsible for payment of all Medicaid-covered services
in the service plan.
Utilization controls cannot be applied once the MCO has received
a copy of the service plan.
26

Catch-All Provision 9.1.40
Contractor shall consult and cooperate with the State in meeting
any obligations the State may have under any consent decree,
including the consent decrees entered in Colbert v. Quinn, No. 07
C 4735 (N.D. Ill.), and Williams v. Quinn, No. 05 C 4673 (N.D. Ill.).
Contractor shall modify its business practices, as required by the
State, in performing under the Contract in order for the State to
comply with such consent decrees and, if necessary, enter into
any amendments to the Contract.
If compliance with section 9.1.40 necessitates the expenditure of
additional material resources, then the Department will address
adjustments of the Capitation rates as set forth in section 7.7.
27

Community Transition Initiative
Introduced in late 2020 to incentivize MCOs to facilitate
community transitions of their members living in any NF or SMHRF.
Revised for 2022
Limits incentives to transitions of Williams and Colbert Class Members
only.
Minimum numeric transition requirements established with financial
penalties for failure to achieve targets.
HFS expects that MCOs and their staff and provider networks will
meet the highest clinical and care management standards,
deploying additional resources as needed to achieve and sustain
community integration on behalf of Class Members.
28

CTI Structure
Managed Care Program Policy 055 provides detailed guidance to
MCOs for operating the CTI and delivering all services to which
Class Members are entitled, including outreach, assessment,
service planning, transition support, and long-term monitoring and
reassessment.
HFS partners with University of Illinois College of Nursing (UIC-CON)
to administer CTI and support coordination with the
Comprehensive Program.
Clearinghouse function to ensure coordination for Class Members.
Clinical oversight to ensure thorough planning and safe transitions.
CTI website compiles all required forms and workflows.
29

CTI Contract Language
5.18.6.1
“Contractor’s efforts must comply with Department- issued written
policy, including but not limited to the nature, frequency, timing,
and substance of the following CTI activities: outreach,
assessment, transition planning, assistance with location of
appropriate housing for transition, subsidies to enable transition,
transition support, and follow-up.”
Class Members remain Class Members after community transition
and MCOs must continue to serve them as such.
30

CTI Numeric Transition Requirements
HFS set modest minimum transition requirements for Health Choice
Illinois MCOs in CY 2022.
Failure to achieve targets will result in financial penalties.
Targets based on percentage of long-term care admissions in FY2020.
31
Colbert
Williams
Minimum transition requirement = 2% of
the number of enrollees admitted to
Cook County NFs in FY20.
Minimum transition requirement = 3% of
the number of enrollees admitted to
Illinois SMHRFs in
FY20.
Individual MCO targets range from three
to 19 transitions, totaling 70 transitions
across all HCI plans.
Individual MCO targets range from two
to seven transitions, totaling 23 transitions
across all HCI plans.

Process Performance to Date
Promising early indicators of leadership at the operational level –
HFS recognizes the CTI Leads:
Instrumental in working with MCO Care Coordinators and Case
Managers to facilitate Colbert Class Member transitions.
Productive partnering with HFS, UIC-CON, and other stakeholders on
process improvements.
Persistence in resolving barriers to Class Member transitions.
Evidence of improved clinical components: Assessment, Transition
Service Plan, and Post Transition Follow up and Monitoring.
Increasing efforts to enhance expertise in Housing and Behavioral
Health.
32

Factors Driving Successful CTI Transitions
Dedicated MCO staff who are experienced, detail-oriented, and
solution-focused.
Skillful navigation of provider network, especially arranging HCBS
waiver services and community-based mental health services.
Energetic and resourceful housing placement efforts.
Clinical expertise driving person-centered care planning, which in
turn informs transition and post-transition activities.
33

Outcome Performance to Date
Colbert
Williams
Modest progress towards
minimum targets.
Extremely poor performance
towards minimum targets
35 of 70 CY22 required transitions
achieved as of 08/31/2022
0 of 23 CY22 required transitions
achieved as of 08/31/2022
Performance varies by health
plan; one plan has already
achieved 106% of required
transitions compared to another
which has only achieved 22% of
required transitions to date.
No Williams Class Members have
transitioned under the CTI in CY22.
34
Barriers Addressed
HFS has responded with resources and technical assistance to barriers
identified by health plans in working with complex and challenging
cases of Class Members.
Contacts at each Prime agency.
Access to bridge housing subsidies
Access to transition assistance funds
Training on Olmstead
Training and technical assistance on housing supports and services
Access to HFS staff for help resolving critical issues.
35

Time to Pull Out All the Stops
Ensure ample resources and alignment of expectations across
leadership, care management staff, and provider network to reach
minimum transition targets in 2022 to avoid financial penalties.
Acknowledge and support good work underway in your MCO and
invest resources to enhance and expand what’s working well.
Leverage behavioral health expertise within and beyond your
organization to implement innovative strategies for serving Williams Class
Members.
Ensure highest degree of attentiveness and quality for Class Members
both during and following transition. (I.e., no shortcuts)
36

Coordination with Prime Agencies
Coordination with the Comprehensive Program and proactive problem
solving is nonnegotiable.
To maintain clear lines of accountability and minimize Class Member
confusion, MCOs must continue to confirm that any member they wish
to work with under the CTI is not already paired to a Prime, using the
UIC-CON clearinghouse process.
If for any reason a Class Member disengages from CTI, by choice or due
to disenrollment from the health plan, this must be reported to UIC-CON
to ensure the Class Member continues to receive the services to which
they are entitled.
37

Expectations and Opportunities
In remainder of CY 2022 and FY 2023
MCOs will ensure that ALL resources, infrastructure, and processes
required by the contract are deployed in support of the state’s vision
for ADA, Olmstead, and Consent Decree compliance.
MCOs will make concerted effort to meet CTI minimum transition
requirements for 2022 by 12/31/2022.
MCOs will demonstrate initiative in the CTI and prioritize
energetic and advanced collaboration with Prime Agencies to
ensure efficient, expeditious, and safe transitions for all Class
Members seeking community integration.
38
Q&A Opportunity for Primes
What information surprised you or is new to you about the work of MCOs?
What additional information would be helpful to know about the work of
MCOs?
How can HFS &/or the MCOs be helpful to Prime Agencies related to Class
Member transitions?
39
