ONC Data Brief ■ No. 16 ■ May 2014
Adoption of Electronic Health Record Systems among U.S. Non-federal Acute
Care Hospitals: 2008-2013
Dustin Charles, MPH; Meghan Gabriel, PhD; Michael F. Furukawa, PhD
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009
directed the Office of the National Coordinator for Health Information Technology (ONC) to
describes trends in adoption of EHR systems among non-federal acute care hospitals from 2008
to 2013.
Hospital adoption of EHR systems has increased more than five-fold since 2008.
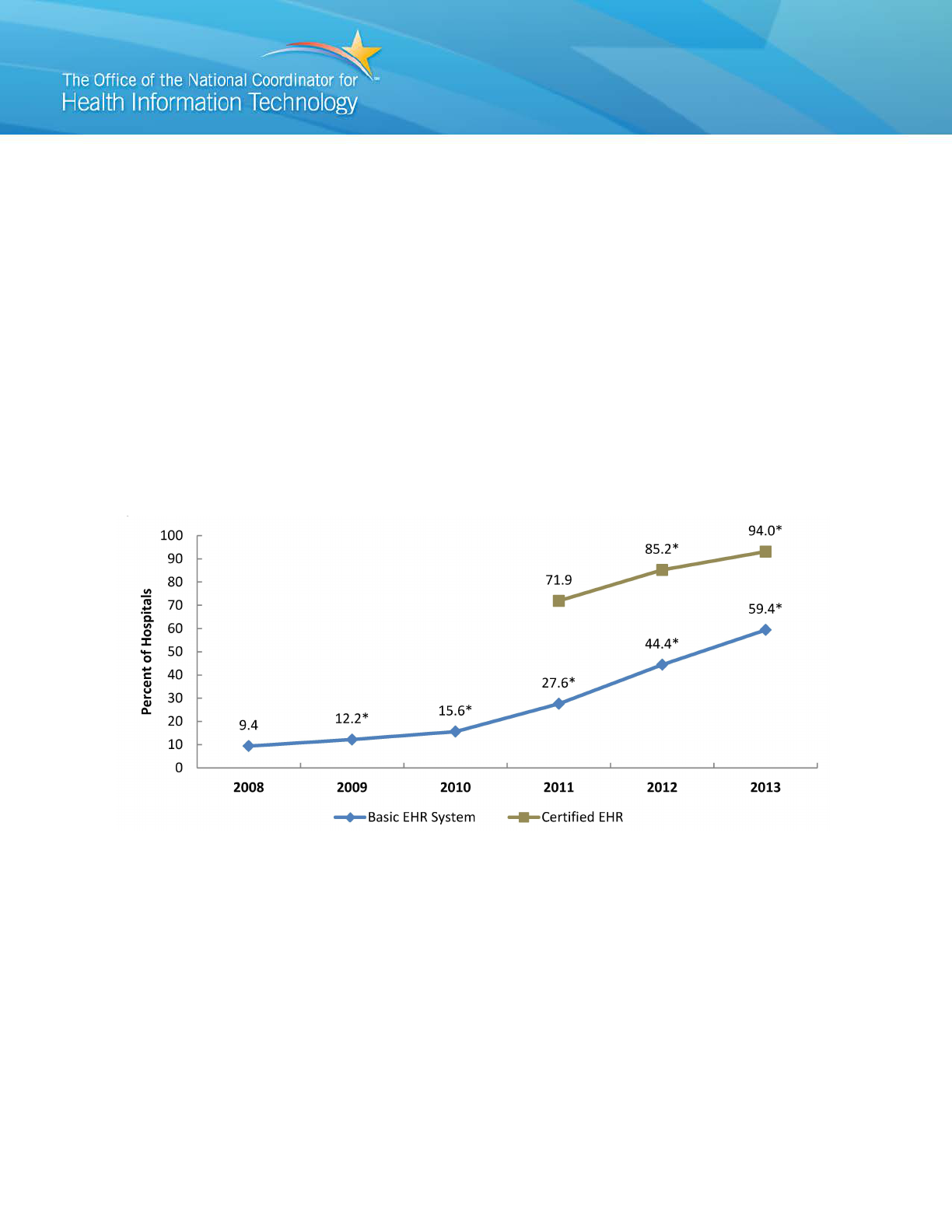
Figure 1: Percent of non-federal acute care hospitals with adoption of at least a Basic EHR
system and possession of a certified EHR: 2008-2013
NOTES: Basic EHR adoption requires the EHR system to have a set of EHR functions defined in Table 2. A certified
EHR is EHR technology that has been certified as meeting federal requirements for some or all of the hospital
objectives of the CMS EHR Incentive Program. Possession means that the hospital has a legal agreement with the
EHR vendor, but is not equivalent to adoption.
*Significantly different from previous year (p < 0.05).
SOURCE: ONC/American Hospital Association (AHA), AHA Annual Survey Information Technology Supplement
I
r
n 2013, nearly six in ten (59%) hospitals have adopted at least a Basic EHR system. This
epresents an increase of 34% from 2012 to 2013 and a five-fold increase since 2008
(Figure 1).
Over nine in ten (93%) hospitals possessed a certified EHR technology in 2013,
increasing by 29% since 2011.
1

Hospital adoption of EHR systems varied significantly by state.
system by U.S. state: 2013
State
Basic EHR, %
n (N)
State
Basic EHR, %
n (N)
United States
59.4
2655 (4472)
Missouri
53.1
111 (112)
Alabama
45.4
31 (90)
Montana
67.5
28 (54)
Alaska
55.3
6 (19)
Nebraska
41.0
§
49 (84)
Arizona
71.6†
39 (60)
Nevada
68.0
11 (29)
Arkansas
78.2†
38 (71)
New Hampshire
58.7
12 (26)
California
55.3
170 (328)
New Jersey
43.9
§
45 (64)
Colorado
76.3†
48 (71)
New Mexico
47.8
17 (31)
Connecticut
75.7†
17 (29)
New York
63.4
115 (171)
Delaware
50.1
4 (6)
North Carolina
74.7†
55 (108)
District of Columbia
67.9
6 (8)
North Dakota
78.7†
14 (42)
Florida
65.7
96 (184)
Ohio
57.9
106 (158)
Georgia
60.9
58 (134)
Oklahoma
47.3
§
57 (107)
Hawaii
83.4†
12 (20)
Oregon
51.6
27 (59)
Idaho
52.4
20 (38)
Pennsylvania
53.2
§
114 (154)
Illinois
66.8†
141 (178)
Rhode Island
61.3
8 (10)
Indiana
63.6
63 (107)
South Carolina
63.0
19 (58)
Iowa
61.4
75 (117)
South Dakota
82.2†
23 (50)
Kansas
36.1
§
97 (125)
Tennessee
52.9
48 (115)
Kentucky
50.8
§
63 (97)
Texas
53.7
§
199 (343)
Louisiana
49.2
44 (100)
Utah
26.2
§
22 (44)
Maine
45.2
§
22 (36)
Vermont
66.1
6 (14)
Maryland
73.0†
31 (45)
Virginia
65.2
42 (81)
Massachusetts
63.6
40 (62)
Washington
70.3
36 (88)
Michigan
67.5†
74 (128)
West Virginia
47.3
§
28 (49)
Minnesota
71.6†
127 (129)
Wisconsin
78.1†
93 (125)
Mississippi
56.1
§
33 (90)
Wyoming
80.9†
15 (24)
NOTES: Basic EHR adoption requires the EHR system to have a set of EHR functions defined in Table 2.
n = survey respondents; N = hospitals surveyed. All estimates met standards for reliability.
†Significantly higher than national average
§Significantly lower than national average (p < 0.05)
SOURCE: ONC/AHA, AHA Annual Survey Information Technology Supplement
State rates of hospital adoption of at least a Basic EHR system ranged from 26% to 83%
(Table 1).
Hawaii (83%), South Dakota (82%), and North Dakota (79%) had the highest percent of
hospitals with adoption of at least a Basic EHR system.
Utah (26%), Kansas (36%), and Nebraska (41%) had the lowest percent of hospitals with
adoption of at least a Basic EHR system.
2

EHR adoption rates were significantly higher than the national average in fifteen
states.
system compared with the national average (59.4%): 2013
NOTES: Basic EHR adoption requires the EHR system to have at least a basic set of EHR functions, including
clinician notes, as defined in Table 2.
SOURCE: ONC/AHA, AHA Annual Survey Information Technology Supplement
Hospital adoption of at least a Basic EHR system was significantly higher than the
national average in fifteen states (Arizona, Arkansas, Colorado, Connecticut, Hawaii,
Illinois, Maryland, Massachusetts, Michigan, Minnesota, North Carolina, North Dakota,
South Dakota, Wisconsin, and Wyoming) (Figure 2).
Hospital adoption of at least a Basic EHR system was significantly lower than the
national average in eleven states (Kansas, Kentucky, Maine, Mississippi, Nebraska, New
Jersey, Oklahoma, Pennsylvania, Texas, Utah, and West Virginia).
Most of the states with adoption rates significantly higher than the national average were
located in the Midwest.
3

Trends in EHR adoption show increasing use of advanced functionality.
Figure 3: Percent of non-federal acute care hospitals with adoption of EHR systems by level of
functionality: 2008-2013
NOTES: Definitions of Basic EHR and Comprehensive EHR systems are reported in Table 2.
*Significantly different from previous year (p < 0.05).
A prior study reported estimates of hospital adoption based on at least Basic EHR with Clinician Notes (1).
Differences in the estimates in this brief from (1) are due to the inclusion of children’s and cancer hospitals and small
differences in the calculation of hospital-level weights.
SOURCE: ONC/AHA, AHA Annual Survey Information Technology Supplement
Hospital adoption of a Basic EHR without Clinician Notes has declined marginally while
the systems with more advanced functionality have increased significantly (Figure 3).
Hospital adoption of Comprehensive EHR systems has increased eight-fold since 2009,
rising to over a quarter (26%) of hospitals in 2013.
4

Summary
Adoption of EHR systems by non-federal acute care hospitals has steadily increased since
HITECH. In 2013, nearly six in ten (59%) non-federal acute care hospitals had adopted at least a
Basic EHR system with clinician notes. This represents a 34% increase from the previous year
and a more than five-fold increase in EHR adoption since 2008. In addition, a vast majority of
acute care hospitals (93%) possessed EHR technology certified as meeting federal requirements
for Meaningful Use objectives.
Hospital adoption of EHR systems varied across U.S. states. Rates of hospital adoption of at least
a Basic EHR system were significantly above the national average in fourteen states and
significantly below the national average in eleven other states. Hospitals in Hawaii, South
Dakota, and North Dakota had the highest rates of adoption. Hospitals in Utah, Kansas, and
Nebraska had the lowest adoption rates.
In addition to growth in EHR adoption overall, hospital adoption of advanced functionality has
increased significantly. Hospital adoption of comprehensive EHR systems has increased more
than eight-fold in the last four years.
5

Definitions
Non-federal acute care hospital: Includes acute care general medical and surgical, children’s
general, and cancer hospitals owned by private/not-for-profit, investor-owned/for-profit, or
state/local government and located within the 50 states and District of Columbia. The inclusion
of children’s general and cancer hospitals makes this definition different from previous peer-
reviewed research (2). However, it is more consistent with the population of hospitals eligible for
federal health IT adoption incentives.
Adoption of Basic EHR: Table 2 defines the electronic functions required for hospital adoption
of a Basic or Comprehensive EHR system, which a consensus expert panel established (3). The
panel disagreed on the need to include physician notes and nursing assessments to classify a
Basic system, so they developed two definitions of Basic EHR adoption (Basic EHR without
Notes and Basic EHR with Notes) (3). Since the first stage of the CMS EHR Incentive Program
did not require clinician notes, an earlier brief reported Basic EHR without Clinician Notes (4).
Since clinician notes are a requirement for the second stage (5), the definition of Basic EHR in
this brief includes clinician notes as a requirement for at least a Basic EHR system.
Possession of Certified EHR: A certified EHR is EHR technology that has been certified as
meeting federal requirements for some or all of the hospital objectives of the CMS EHR
Incentive Program. “Possession” of certified EHR technology is considered to be either the
physical possession of the medium on which a certified Complete EHR, or certified Modular
EHR resides, or a legally enforceable right by an eligible health care provider to access and use,
at its discretion, the capabilities of a certified Complete EHR or certified Modular EHR. An
eligible health care provider may determine the extent to which it will implement or use these
capabilities, which will not affect the provider’s “possession” of the certified Complete EHR or
certified EHR Module.
6
Table 2: Electronic Functions Required for Hospital Adoption of Basic or Comprehensive EHR
Systems
EHR Functions
Required
Clinician Notes
Basic EHR with
Clinician Notes
Comprehensive
EHR
Electronic Clinical
Information
Patient demographics
Physician notes
Nursing assessments
Problem lists
Medication lists
Discharge summaries
Advance directives
Computerized Provider
Order Entry
Lab reports
Radiology tests
Medications
Consultation requests
Nursing orders
Results Management
View lab reports
View radiology reports
View radiology images
View diagnostic test results
View diagnostic test images
View consultant report
Decision Support
Clinical guidelines
Clinical reminders
Drug allergy results
Drug-drug interactions
Drug-lab interactions
Drug dosing support
NOTES: Basic EHR adoption requires each function to be implemented in at least one clinical unit, and
Comprehensive EHR adoption requires each function to be implemented in all clinical units
7
blank
blank
blank
blank blank
blank blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank
blank blank

Data Source and Methods
Data are from the American Hospital Association (AHA) Information Technology (IT)
Supplement to the AHA Annual Survey. Since 2008, ONC has partnered with the AHA to
measure the adoption and use of health IT in U.S. hospitals. ONC funded the 2013 AHA IT
Supplement to track hospital adoption and use of EHRs and the exchange of clinical data.
The chief executive officer of each U.S. hospital was invited to participate in the survey
regardless of AHA membership status. The person most knowledgeable about the hospital’s
health IT (typically the chief information officer) was requested to provide the information via a
mail survey or secure online site. Non-respondents received follow-up mailings and phone calls
to encourage response. The survey was fielded from November 2013 to the end of February
2014.
The response rate for non-federal acute care hospitals was 59%. A logistic regression model
was used to predict the propensity of survey response as a function of hospital characteristics,
including size, ownership, teaching status, system membership, availability of a cardiac
intensive care unit, urban status, and region. Hospital-level weights were derived by the inverse
of the predicted propensity.
Estimates considered unreliable had a relative standard error adjusted for finite populations
greater than 0.49. Responses with missing values were assigned zero values. Significant
differences were tested using p < 0.05 as the threshold.
References
1. Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, Shields A,
Rosenbaum S, Blumenthal D. Use of Electronic Health Records in U.S. Hospitals. New
England Journal of Medicine. 360(16): 1628-38; 2009.
2. DesRoches CM, Worzala C, Joshi MS, Kralovec PD, Jha AK. “Small, Nonteaching, and
Rural Hospitals Continue to be Slow in Adopting Electronic Health Record Systems.”
Health Affairs. 31(5): 1092-1099; 2012.
3. Blumenthal D, DesRoches CM, Donelan K, Ferris TG, Jha AK, Kaushal R, et al. Health
Information Technology in the United States: The Information Base for Progress.
Princeton, NJ: Robert Wood Johnson Foundation; 2006.
4. Charles D, Furukawa MF, Hufstader M. “Electronic Health Record Systems and Intent to
Attest to Meaningful Use among Non-federal Acute Care Hospitals in the United States:
2008-2011” ONC Data Brief, no 1. Washington, DC: Office of the National Coordinator
for Health Information Technology. February 2012.
5. Centers for Medicare & Medicaid Services. [Medicare and Medicaid] EHR Incentive
Programs. Available form: https://www.cms.gov/ehrincentiveprograms
.
8

About the Authors
The authors are with the Office of the National Coordinator for Health Information Technology,
Office of Economic Analysis, Evaluation and Modeling.
Acknowledgements
Peter Kralovec of the American Hospital Association contributed to the development of the
survey instrument and survey administration.
Suggested Citation
Charles D, Gabriel M, Furukawa MF. “Adoption of Electronic Health Record Systems among
U.S. Non-federal Acute Care Hospitals: 2008-2013,” ONC Data Brief, no. 16. Washington, DC:
9
